Back to Journals » Patient Preference and Adherence » Volume 16
Gender Bias in Urology: How Do Patients Really Choose Their Urologist?
Authors Tamalunas A , Lenau P, Stadelmeier LF, Mumm JN, Vilsmaier T, Höhn H, Mumm ML, Waidelich R, Casuscelli J, Magistro G, Buchner A , Kolben T , Stief C, Hennenberg M
Received 5 August 2022
Accepted for publication 18 October 2022
Published 3 November 2022 Volume 2022:16 Pages 3001—3013
DOI https://doi.org/10.2147/PPA.S384967
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Alexander Tamalunas,1 Philipp Lenau,1 Leo Federico Stadelmeier,1 Jan-Niclas Mumm,1 Theresa Vilsmaier,2 Henrik Höhn,2 Maja-Lena Mumm,3 Raphaela Waidelich,1 Jozefina Casuscelli,1 Giuseppe Magistro,1 Alexander Buchner,1 Thomas Kolben,2 Christian Stief,1 Martin Hennenberg1
1Department of Urology, University Hospital, LMU Munich, Munich, Germany; 2Department of Obstetrics and Gynecology, University Hospital, LMU Munich, Munich, Germany; 3Department of Political and Social Sciences, Institute for Media and Communication Studies, Freie Universität Berlin, Berlin, Germany
Correspondence: Alexander Tamalunas, Department of Urology, University Hospital, LMU Munich, Marchioninistr. 15, Munich, 81377, Germany, Tel +49 89 4400 – 0, Email [email protected]
Purpose: The present study aimed to investigate the influence of patients’ and urologists’ gender when choosing a urologist. With rising population diversity through immigration and generational differences, patient-centered healthcare has recently moved to the focus of European healthcare systems. As healthcare in urology often concentrates on sensitive topics, and often involves gender-specific diseases, research on the influence of gender on decision-making processes is of high importance. Understanding influence of gender on patients’ choices in real life would provide patients, and physicians alike, with the means to provide better resources to achieve greater satisfaction from visits to a urologist.
Patients and Methods: A questionnaire was prepared, and patients at our tertiary referral center were given the opportunity to voluntarily participate in our survey. We collected questionnaires from 1012 patients during their visits from June 2021 to October 2021.
Results: Patients were divided into groups according to their gender: male (n=763), female (n=246), and non-binary (n=3). Our patient cohort consisted of more men than women (75% vs 24%), with only three patients identifying as non-binary. Irrespective of the patients’ own gender, patients preferred a male urologist when problems were considered embarrassing, limiting daily activities, or when worrisome. When problems were considered painful, all patients preferred a female urologist. When patients had had a previous positive experience with a female or male urologist, they preferred to be treated by a female or male urologist, respectively. Overall, 65% of patients stated a gender preference for at least one given situation, or consultation scenario.
Conclusion: As the majority of our patients stated a gender preference, urological departments should be considerate of potential patients’ preferences for urologist gender that may be based on the individual patient’s history, taking a comprehensive approach to fulfill the patients’ need for same gender urologists in educational hospitals and health care services.
Keywords: gender, sex, urologist, health economics, health services research, medical research, patient-centered care, person-centered medicine, public health, decision making
Introduction
With rising population diversity through immigration and generational differences, patient-centered healthcare has recently moved to the focus in European healthcare systems. With healthcare services becoming increasingly more available throughout the population, a more patient-friendly approach is warranted in the effort to offer personalized medicine. While in the past, research on doctor-patient interaction has often focused on the decision-making abilities of physicians, it rarely centered around the question of what factors are important to patients when finding their respective practitioners.1,2 Slowly, the modern healthcare system has started to accept patients as clients, who are consumers of healthcare services.3 With healthcare professionals acknowledging that treatment satisfaction and adherence is essential to provide high quality health care, personalized medicine has become the ultimate goal.4 Thus, there is an increasing interest in the patients’ views and expectations of their doctors. The first step in this process is the selection of a physician by the patient, whenever possible.4,5 As satisfied patients usually establish a long-term treatment relationship with their doctor, they can also significantly alter other patients’ choice in care provider by recommendation. Therefore, patient satisfaction may not only result in increased treatment adherence and medication compliance but may also result in substantial financial profits.6,7 Patients may place high importance on the doctor’s professional skill, or recommendation by close relatives and friends, or even using doctor-rating websites. However, in urology healthcare, patients often present with far more intimate problems compared to other disciplines, taking the doctor-patient relationship to a high personal level.5,8,9 Urologic problems involve highly sensitive issues, including incontinence, genital infections, sexually transmitted diseases (STD), and erectile dysfunction (ED). Many of them address gender-specific ailments and are often considered embarrassing by the patient, and delayed care seeking may even result in adverse outcomes. Although research has begun to increasingly focus on patient satisfaction, there is only limited knowledge on how patients choose their urologist and on the impact of gender.4,5,9–12
Patients in the German healthcare system provide an ideal study cohort, as Germany has one of the most restriction-free and consumer-oriented healthcare systems. Compared to other healthcare systems, in which insurance networks may greatly influence patients’ choice of a urologist according to a particular healthcare plan or healthcare provider, as is often the case in the US, the German healthcare system allows patients to seek nearly any type of care they wish, and whenever they want it.13,14 When health insurance coverage was expanded from the majority of the population to everyone in 2009, it became compulsory for the whole population.15 Because of the consumer-oriented and compulsory health insurance in Germany, this largest-to-date survey poses a rare opportunity to determine the influence of both the patients’ and the doctors’ gender in urology healthcare. While research on fundamental decision processes is of high importance, understanding the factors that influence patients’ choices in real life decision making would potentially provide patients, and physicians alike, with the means to provide better resources to diminish barriers in seeking optimal urology healthcare.
We aimed to anonymously gather information on patients’ gender preference when choosing a urologist, and to the best of our knowledge, there is currently no such survey interviewing more than 1000 patients.
Materials and Methods
Patient Population
In our tertiary referral center, patients were given the opportunity to voluntarily participate in our survey. From June to October 2021 questionnaires were available to all patients presenting at our outpatient clinic.
Study Design
Random sampling was conducted at our institution’s outpatient clinic on multiple occasions from June to October 2021. Patients were handed the paper questionnaire with their documents and patient information at the beginning of their visit. The questionnaire was accompanied by a cover sheet explaining the survey. As participation was completely optional, patients were instructed to deposit the filled-out questionnaire in a sealed container at any given time, or return the blank questionnaire with their other documents. All data were collected anonymously and cannot be linked to any individual participant in our survey.
Study Tool
To collect data from a large patient cohort on how patients choose a urologist, we developed a questionnaire containing 17 different items of interest specifically for this patient survey (Supplementary File 1).16 Items were designed as closed questions with pre-coded multiple-choice response options. The detailed questionnaire focused on the participant’s own characteristics (gender, age, educational status, sociocultural background, and insurance modality), reason for consultation, and subsequent questions were related to the patient’s previous experiences with a urologist. Additionally, the questionnaire focused on the urologist’s personal features, including gender, academic position, and perceived ability to relate to the patient’s problems. For evaluating gender preference, 14 pertinent questions regarding gender-specific situations and the urologist’s perceived ability to relate to the patient’s problems were created (see Supplementary File 1, questions 8 and 9). To minimize bias and reduce the influence of the physician’s presence, the questions were phrased in a straightforward manner and simple written instructions accompanied every single question in the questionnaire. A clinical judgment discrimination process was crucial for determining all possible items and to identify the pertinent questions relevant to patient determinants. The initial version was evaluated, and questions deemed non-relevant or duplicated were rejected in the final version. Piloting was conducted in 50 patients. Following our previous experience, the pilot revealed no issues with understanding the questions, and patients found it easy to proceed while waiting for their appointment.5 Participants were provided with a cover letter designed to encourage the respondent to participate in this study, including information on the organization conducting the survey and contact details of the responsible researcher. However, and to reduce investigator bias, the patients were not given any oral instructions by healthcare personnel.
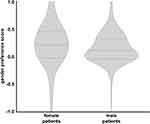
Statistical Analysis
Statistical analysis was performed using SPSS V28.0 software (IBM SPSS Statistics, Armonk, NY). For evaluating gender preference, answers were coded as follows: “-1.0” represented preferring a female urologist, “+1.0” represented preferring a male urologist, and “0.0” represented no preference. For evaluating same-gender preference, answers were coded as follows: “-1.0” represented preferring an opposite-gender urologist, “+1.0” represented preferring a same-gender urologist, and “0.0” represented no preference. The result was added up and divided by 14. Thus, a gender preference score could be developed for each patient with values ranking from −1.0 to +1.0. Results are given as percentages for categorial variables. Fisher’s exact test and χ2 test were performed for categorial variables, t-test, and Mann–Whitney U-test for continuous variables. Potential confounders for gender preference (yes vs no) in different scenarios were analyzed using multivariable logistic regression models. All reported p-values were two-sided and considered statistically significant if p<0.05.
Results
In total, we analyzed 1012 questionnaires. We report a response rate of 88% (1012/1150). No questionnaire had to be discarded due to a low rate of answered questions, which was defined as a participant answering to less than half of the questions.
Sample Characteristics
To obtain an overview we have listed a breakdown of our sample characteristics in Table 1. In the following, we will only present an overview of our data. We found our sample to be quite heterogeneous. Patients were of different age groups and genders, experienced different educational backgrounds, and had a variety of insurance modalities. With 75.4% the majority of our study cohort were male, while 24.3% were female, and 0.3% identified as non-binary. The highest percentage of patients was >60 years (63.8%), while the other age brackets contained far fewer participants (age <20, 20–40, and 41–60, with 0.3%, 11.2%, and 24.6%, respectively; Table 1).
 |
Table 1 Patient Characteristics |
Questions regarding patients’ socioeconomic background revealed, that most patients had statutory health insurance (87.6%), and the remaining patients chose private health insurance (12.4%). Most of our participants were retired (58.2%), while 27.3% and 7.8% were working full-time or part-time, respectively, and 6.1% were employed but currently on sick leave. The majority of patients were in a relationship (68.4%), and 13.6% were single.
Questions on the educational background revealed that the majority of patients had graduated with A-levels (57.3%). To investigate a possible sociocultural bias, we asked patients their nationality, country of birth, and religious beliefs. Interestingly, the overwhelming majority of patients were either born in Germany (92.6%), and/or held a German passport (95.6%). Also, the majority of patients identified as Christians (68.6%), followed by non-believers (22.1%), and patients who did not want to give an answer (6.9%).
In-House Visits
Patients presented with a variety of problems and reasons for their in-house visits (Table 2). Reasons for visiting the outpatient clinic included follow-up examinations after surgery (41.3%), examinations before a scheduled surgery (25.9%), acute complaints (20.6%), and preventive medical check-ups (4.2%). Problems involved the prostate (47.2%), bladder (40.7%), lower urinary tract symptoms (29.3%), kidneys (20.5%), erectile dysfunction (7.6%), and sexually transmitted diseases (1.6%). The problems with which patients presented were considered as worrisome (74.1%), limiting daily activities (67.1%), painful (30.5%), and embarrassing (20.4%).
 |
Table 2 Complaints and Previous Experience |
Gender Preference
Preference of the urologists’ gender was assessed using multiple questions (Table 3, supplementary File 1, questions 8 and 9). With 65% of patients, the majority of our study cohort expressed a gender preference for their treating urologist, either in a hypothetical albeit specific situation, or by the urologist’s perceived ability to relate to the patient’s problems. Only 35% consistently indicated that they had no preference for the urologist’s gender (Figure 1). In multivariable analysis, several significant confounders for gender preference were identified that varied between different scenarios (only consultation, examination etc.; Table 4). Interestingly, we could show that women and men preferred same-gender urologists, respectively (p<0.001). Irrespective of the patients’ own gender, they preferred a male urologist when problems were considered embarrassing (p=0.031), limited daily activities (p<0.001), or when worrisome (p=0.026). However, when problems were considered painful, all patients preferred a female urologist (p=0.001). When patients had had a previous positive experience with a female or male urologist, they preferred to be treated by a female or male urologist, respectively (p<0.001). When patients were asked in which situation they preferred which gender of urologist, we observed an interesting shift: for consultation only, 34.8% had a preference, which was fairly balanced at 40:60 for the preference of a female and male urologist, respectively (Figure 2). However, when asked which urologist should perform an operation, that ratio shifted to about 20:80 in favor of a male urologist. Interestingly, these observations were irrespective of the patients’ own gender. We stratified patients according to their own gender and observed a significant correlation (Figure 3). Of all patients, who selected a gender preference, female patients were more likely to choose a same-gender urologist for a urologic examination, while this shifted the more impersonal the reason for consultation got, with only 20.7% preferring a same-gender urologist for an operation under general anesthesia. However, male patients decidedly chose a male urologist, irrespective of the reason for consultation. When patients were asked what personal characteristics, they attributed to the urologist, women answered that female urologists understood their body better, that it was easier talking about their urologic problems with a female urologist, and that female urologists were more empathic. Correspondingly, men also answered that male urologists understood their body better and that it was easier talking about their problems to a male urologist, but then they also attributed better practical abilities to a male urologist.
 |
Table 3 Factors for Preference of Urologist |
 |
Table 4 Multivariable Analysis (Logistic Regression) of Potential Confounders for Gender Preference (Yes vs No) |
Discussion
The German health insurance system is one of the most consumer-oriented health care systems in the world. While our data may not be generalizable to other populations and health care systems, our study offers unique insight into the decision-making processes of patients seeking urological care, who are not bound by a particular health care plan or health care provider, as is often the case in the US.13,14 With more than 1000 participants, this is the largest-to-date study focusing on the influence of gender in urological health care. Although research has begun to increasingly focus on patient satisfaction, there is only limited knowledge on how patients choose their urologist and for gender preference.4,5,9–12
Recently, we could show that patients chose their urologist based on fairly rational grounds, focusing on certain core variables, such as professional skill and academic criteria of the urologist, or being attended by the same urologist at every visit, or by personal referral.5 These findings were later corroborated with the European Association of Urology Section of Outpatient and Office Urology (ESUO) questionnaire by Zachariou, et al.4 Those studies included board certification as surrogate for professional skill, and academic degree as visible external factor for professional accomplishment. While practicability, like location/convenience, or affordability may play an important role – or in case of the latter – greatly bias the patients’ decision, few studies have focused on the impact of gender in male-dominated medical disciplines.17 However, in 2005 Tempest et al were among the earliest investigators into the possibility of gender preference in urological practice.9 They asked the simple and straight-forward question, if patients had any preference for the examining urologist’s gender (ie “male”, “female”, or “no preference”), concluding that around 80% of patients indicated no preferred gender of the treating urologist. However, when a gender preference was expressed, 98% of patients preferred the same gender urologist. These results are in accordance with our previous survey, in which only around 25% of patients expressively wanted to be treated by a urologist of the same gender, which increased with age and became more obvious in older male patients (>60 years).5
There is data from other studies, using a more differentiated approach, resulting in slightly different conclusions. Placing patients in an endoscopic setting, Lahat et al report that the physician’s gender may be important for up to 35% of patients in endoscopy.18 Amir et al specifically aimed to identify, if male patients preferred a urologist of the same gender.8 Compared to the study by Lahat et al, they interviewed a small group of 119 male patients and found a slightly increased rate of 43% of patients preferring a same-gender urologist. However, taking into consideration a relatively high religious fraction of responders, as the research was conducted exclusively with male Israeli patients in Tel Aviv, Israel. They stratified patients according to the supposed intimacy of the procedure (physical examination versus consultation only) but evaluated a cohort, which may have had another cultural background as patients in our study.8 On the other hand, Kim et al phrased three questions associated to situations in which patients might prefer a same gender urologist. To cite specific pertinent results, 53% of patients stated preference for a same-gender urologist, and 62% of women preferred a female urologist, peaking up to 77% for urologic surgery in the same cohort.12
Still, many of these studies have in common that they only ask a generalized question, if patients, theoretically, had a gender preference, or do not further differentiate as to what the reason for consultation might have been, or in what circumstances patients may have had a preference.5,8,9,12,18 To minimize this bias, we differentiated this specific question into 14 items related to a possible gender preference for the treating urologist. Our patient cohort was distributed in a male to female ratio of 4: 1, which corresponded with other studies investigating factors when choosing a urologist.5,9,19 In total, only 35% of patients continuously stated no preference for the urologist’s gender. Corresponding to other studies, we found that preference for same gender urologist was most pronounced in the setting of a physical examination.8,12 However, and contrary to Kim et al, we found that women were predominantly indifferent when considering urologic surgery.12 Additionally, there seem to be certain confounding factors, such as education levels and insurance status. Private insurance status is dependent on income, and therefore may correlate with higher education levels, generating these results. However, privately insured patients in Germany are even more used to freely choosing their practitioner, whether for consultation or even for surgery.15 Thus, privately insured patients may present with a lower threshold in expressing their preference, even extending to the urologist’s gender.
While other studies have revealed that feelings of embarrassment among patients hindered them in communicating effectively with their urologist, we found that our patient cohort overall preferred a male urologist when problems were considered embarrassing, limiting daily activities, or when worrisome. However, when problems were considered painful, patients preferred a female urologist, who they deemed more empathic. Also, when patients had had a previous positive experience with a female or male urologist, they preferred to be treated by a future urologist of that same gender.
This corresponds well to an increasing demand for female urologists, attributing care, warmth, patience, and empathy to their practice style.11,20 Corresponding to our results, some women find female surgeons more desirable for sensitive procedures, and a study in 2019 showed most of the women with pelvic floor disorders had a preference for the same gender uro-gynecologists.11,21 Thus, when our patients were asked what personal characteristics they attributed to the same gender urologist, women and men alike, answered that they understood their body better, and that it was easier talking about their urologic problems with a urologist of the same gender. However, as men attributed better practical abilities to a male urologist, this may be due to a certain bias in male-dominated medical disciplines, such as urology.17
Nonetheless, there are studies not only attributing the availability of same gender physicians to greater patient satisfaction but demonstrating that patient and urologist gender similarity may even be associated with health outcomes.9,22 While the quality of patient-urologists relationship and the level of patient satisfaction in a medical encounter may also greatly influence health care outcomes, lacking presence of same gender urologists in clinical settings may even prove a barrier to timely care.23–25 Studies in which patients’ religious environments prompted female patients to refuse male urologists even in emergency situations, and male specialists even in non-sensitive procedures when female specialists were not available, have been reported.25–27 Unfortunately, our data did not yield a sufficient amount of religious and ethnic diversity in order to evaluate religious or socio-cultural bias on patients’ decisions and gender preferences. However, delayed care seeking in the absence of a same gender specialist may be associated with adverse health outcomes.11
However, many studies have already emphasized institutional obstacles such as gender inequality, and hostile work structure for female surgeons due to lacking family-friendly working conditions and missing flexibility in working shifts.28 Thus, with rising population diversity through immigration and generational differences, healthcare systems need to acknowledge cultural differences, values, religious, and also sociocultural norms in order to provide sufficient healthcare to all patients.8,9,11,25–27
There are certain limitations to this study. Even though being a tertiary referral center provides us with the advantage of a high coverage of diverse urological conditions, there may be a selection bias as our patient cohort may differ from outpatient consultations. Also, we were not able to establish sociocultural factors, that may have had an impact on patient preference for urologist gender, as our patient population did not yield the required diversity to perform a sufficiently powered analysis. Finally, our findings reflect the situation in the German health care system. Attributed to national variations in medical systems and country-specific conditions, our findings may not be generalized without limitations. Nevertheless, and to the best of our knowledge, this is the largest-to-date survey of gender preferences in the field of urology.
Conclusion
Patients may state a preference for urologist gender out of a multitude of very personal reasons, and in different situations. With rising population diversity through immigration and generational differences, healthcare systems need to be aware of cultural differences, values, religious, and also sociocultural norms in order to provide sufficient healthcare to all patients. As the absence of a same gender urologist may delay adequate treatment and, ultimately, result in adverse health outcomes, urological departments should be considerate of patient preference for urologist gender that may be based on the individual patient’s history, taking a comprehensive approach to fulfill the patients’ need for same gender urologists in educational hospitals and health care services.
Statement of Ethics
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required and was waived by the institutional review board (University of Munich), as the research presents no more than minimal risk of harm to subjects and involves no procedures for which written consent is normally required outside the research context. Additionally, the signature on the informed consent document would be the only record linking the subject to the research and the principal risk of harm to the subject would be a breach of confidentiality. All data were collected and analyzed anonymously.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
Thomas Kolben holds stock of Roche AG, Biontech, Valneva and a relative is employed at Roche AG. The other authors have no conflicts of interest to declare.
References
1. Detmer DE, Fryback DG, Gassner K. Heuristics and biases in medical decision-making. J Med Educ. 1978;53(8):682–683. doi:10.1097/00001888-197808000-00012
2. Dawson NV, Arkes HR. Systematic errors in medical decision making: judgment limitations. J Gen Intern Med. 1987;2(3):183–187. doi:10.1007/BF02596149
3. Kupfer JM, Bond EU. Patient satisfaction and patient-centered care: necessary but not equal. JAMA. 2012;308(2):139–140. doi:10.1001/jama.2012.7381
4. Zachariou A, Dimitriadis F, Papadimitriou V, et al. What factors determine the patients’ choice in finding their office urologist? Patient Prefer Adherence. 2021;15:2837–2843. doi:10.2147/PPA.S342624
5. Tamalunas A, Buchner A, Hennenberg M, et al. Choosing a Specialist: an Explanatory Study of Factors Influencing Patients in Choosing a Urologist. Urol Int. 2021;1081–8.
6. Preble S, Wachs WW. The new face of growth. Healthc Financ Manage. 2014;68(3):70–75.
7. Lucas JA. The satisfaction survey that matters. Am J Obstet Gynecol. 2012;206(6):518–522. doi:10.1016/j.ajog.2012.01.043
8. Amir H, Beri A, Yechiely R, et al. Do urology male patients prefer same-gender urologist? Am J Mens Health. 2018;12(5):1379–1383. doi:10.1177/1557988316650886
9. Tempest HV, Vowler S, Simpson A. Patients’ preference for gender of urologist. Int J Clin Pract. 2005;59(5):526–528. doi:10.1111/j.1368-5031.2005.00465.x
10. Wynn J, Johns Putra L. Patient preference for urologist gender. Int J Urol. 2021;28(2):170–175. doi:10.1111/iju.14418
11. Tabatabai S, Simforoosh N. Preference for patient -urologist gender similarity and its implications for urology departments: a systematic narrative review and thematic analysis. Urol J. 2020;17(6):568–577. doi:10.22037/uj.v0i0.5779
12. Kim SO, Kang TW, Kwon D. Gender preferences for urologists: women prefer female urologists. Urol J. 2017;14(2):3018–3022.
13. Lubalin JS, Harris-Kojetin LD. What do consumers want and need to know in making health care choices? Med Care Res Rev. 1999;56(Suppl 1):67–102. doi:10.1177/1077558799056001S04
14. Gibbs DA, Sangl JA, Burrus B. Consumer perspectives on information needs for health plan choice. Health Care Financ Rev. 1996;18(1):55–73.
15. Busse R, Knieps F, Bärnighausen T, et al. Statutory health insurance in Germany: a health system shaped by 135 years of solidarity, self-governance, and competition. Lancet. 2017;390(10097):882–897. doi:10.1016/S0140-6736(17)31280-1
16. Kelley K, Clark B, Brown V, et al. Good practice in the conduct and reporting of survey research. Int J Qual Health Care. 2003;15(3):261–266. doi:10.1093/intqhc/mzg031
17. Cox A, Siemens DR. Continued gender disparity in urology? Only time will tell. Can Urol Assoc J. 2020;14(4):79–80. doi:10.5489/cuaj.6519
18. Lahat A, Assouline-Dayan Y, Katz LH, et al. The preference for an endoscopist specific sex: a link between ethnic origin, religious belief, socioeconomic status, and procedure type. Patient Prefer Adherence. 2013;7:897–903. doi:10.2147/PPA.S48468
19. Berger GK, Medairos R, Regala P, et al. Factors influencing patient selection of urologists. Urology. 2020;137:19–25. doi:10.1016/j.urology.2019.08.066
20. Albury C, Pope C, Shaw S, et al. Gender in the consolidated criteria for reporting qualitative research (COREQ) checklist. Int J Qual Health Care. 2021;33(4). doi:10.1093/intqhc/mzab123.
21. Groutz A, Gordon D, Shimonov M, et al. Do women with pelvic floor disorders prefer to be treated by female urogynecologists? Health Care Women Int. 2020;41(5):543–552. doi:10.1080/07399332.2019.1623798
22. Oberlin DT, Vo AX, Bachrach L, et al. The gender divide: the impact of surgeon gender on surgical practice patterns in urology. J Urol. 2016;196(5):1522–1526. doi:10.1016/j.juro.2016.05.030
23. Kerssens JJ, Bensing JM, Andela MG. Patient preference for genders of health professionals. Soc Sci Med. 1997;44(10):1531–1540. doi:10.1016/S0277-9536(96)00272-9
24. Shin DW, Roter DL, Roh YK, et al. Physician gender and patient centered communication: the moderating effect of psychosocial and biomedical case characteristics. Patient Educ Couns. 2015;98(1):55–60. doi:10.1016/j.pec.2014.10.008
25. Alqufly AE, Alharbi B, Alhatlany K, et al. Muslim female gender preference in delaying the medical care at emergency department in Qassim Region, Saudi Arabia. J Family Med Prim Care. 2019;8(5):1658–1663. doi:10.4103/jfmpc.jfmpc_141_19
26. Ahmad WI, Kernohan EE, Baker MR. Patients’ choice of general practitioner: influence of patients’ fluency in English and the ethnicity and sex of the doctor. J R Coll Gen Pract. 1989;39(321):153–155.
27. Vu M, Azmat A, Radejko T, et al. Predictors of delayed healthcare seeking among American Muslim Women. J Womens Health. 2016;25(6):586–593. doi:10.1089/jwh.2015.5517
28. Cochran A, Hauschild T, Elder WB, et al. Perceived gender-based barriers to careers in academic surgery. Am J Surg. 2013;206(2):263–268. doi:10.1016/j.amjsurg.2012.07.044
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.