Back to Journals » Clinical and Experimental Gastroenterology » Volume 14
Gas Leak and Mucosal Injury During Endoscopic Esophageal Myotomy After Previous Myotomy: A Single-Center Experience
Authors Samo S , Hamo F, Jain AS, Shah RH, Patel V, Calderon LF, Xie M, Mekaroonkamol P, Keilin SA, Cai Q
Received 18 December 2020
Accepted for publication 10 May 2021
Published 20 May 2021 Volume 2021:14 Pages 173—179
DOI https://doi.org/10.2147/CEG.S297338
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Andreas M. Kaiser
Salih Samo,1,2 Falak Hamo,2 Anand S Jain,1 Rushikesh H Shah,1 Vaishali Patel,1 Lucie F Calderon,1 Mengdan Xie,1 Parit Mekaroonkamol,1 Steven A Keilin,1 Qiang Cai1
1Division of Digestive Diseases-Department of Medicine, Emory University School of Medicine, Atlanta, GA, USA; 2Division of Gastroenterology, Hepatology and Motility-Department of Medicine, The University of Kansas School of Medicine, Kansas City, KS, USA
Correspondence: Qiang Cai
Emory University School of Medicine, 1365 Clifton Road, B1262, Atlanta, GA, 30322, USA
Tel +1 404-778-2714
Fax +1 404-778-2578
Email [email protected]
Purpose: Peroral endoscopic myotomy (POEM) after prior myotomy (PM-POEM) can be technically challenging with possible increased adverse events. We aimed to assess gas leak and mucosal injury incidence during PM-POEM, compared to an index POEM (iPOEM), and post-procedure extubation time.
Patients and Methods: A retrospective study comparing PM-POEM to iPOEM from March 2016 to August 2018.
Results: There were 21 subjects in the PM-POEM and 56 subjects in the iPOEM. The PM-POEM group was younger (average age 44.33 vs 57.57 years, p=0.0082). Gas leak incidence did not differ between groups (28.6% in PM-POEM vs 14.3% in iPOEM, p=0.148). For cases with imaging available postoperatively, there was a trend towards higher incidence of gas leak in the PM-POEM, but it was not statistically significant (60% vs 42.1%, p=0.359). The post-procedure extubation time was not different between PM-POEM and iPOEM (11.38 vs 9.46 minutes, p=0.93), but it was longer when gas leak occurred (15.92 vs 8.67 minutes, p=0.027). The odds of mucosal injury were four-fold higher (OR, 4.31; 95% CI, 1.32– 14.08), and more clips were used to close mucosal injuries (0.62 vs 0.14 clips, p=0.0053) in the PM-POEM group. More procedures were deemed difficult or challenging in the PM-POEM (33.3% vs 7.1%, p=0.007). The number of clips used to close the mucosotomy was not different between groups (4.05 vs 3.84 clips, p=0.498). Although the myotomy was shorter in PM-POEM, it was not statistically significant (6.38 vs 7.14 cm, p=0.074). However, the procedure was longer in PM-POEM (61.28 vs 45.39 minutes, p=0.0017). There was no intervention or ICU admission required pertinent to the procedure.
Conclusion: Performing PM-POEM can be more difficult with more mucosal injuries. Gas leak was associated with a slightly longer post-procedure extubation time, but clinical relevance is unclear given incidence of gas leak was unknown at time of extubation.
Keywords: peroral endoscopic myotomy, Heller’s myotomy, achalasia, gas leak, mucosal injury
Introduction
Peroral endoscopic myotomy (POEM) was initially introduced in 2010 as a novel treatment modality for achalasia.1 Subsequently, multiple studies have confirmed POEM to be both an effective and safe treatment for achalasia in short- and mid-term studies.2,3 POEM has also been used as a secondary or salvage treatment after failure of other modalities (eg, pneumatic dilation and Heller myotomy [HM])2,4–11 and has been shown to be safe and effective after a failed POEM.12
Progressive tunneling is performed in the submucosal space distally within the esophageal wall during a POEM procedure.1 Therefore, occurrence of gas leak through muscle fibers can occur.13 In fact, gas leak is the most reported insufflation-related event. The incidence of gas leak has been reported to be as high as 86%.14,15 Data from previous experience suggest that gas leak-related events during POEM do not have major clinical consequences.13 It is unknown, however, whether the occurrence of gas leak impacts time to extubation post-procedurally (as a result of presence of capnomediastinum or capnoperitoneum). Mucosal injury is another intra-procedural event that can occur during POEM with an incidence of 4–5%.7,13 Other events that can occur during or after POEM that are procedure-related include bleeding and abdominal and/or chest pain.
Performing surgical myotomy after a previous initial myotomy is complex.16 The same applies to POEM and the procedure is likely to be more technically challenging.6,8 Submucosal fibrosis from a previous myotomy can make the procedure more difficult and increase the risk of adverse events (AEs).17 The aim of our study was to assess the peri-procedural incidence of gas leak and mucosal injury occurring during or after POEM in a group with prior myotomy (whether HM or POEM), the post-myotomy POEM (PM-POEM) group, as compared to an index POEM (iPOEM). We hypothesized that the rate of gas leak and mucosal injury is higher in PM-POEM, and that occurrence of gas leak may be associated with a delay in extubation post procedure. We also hypothesized that tunnel creation may be more difficult in PM-POEM likely due to fibrosis from prior intervention; hence, more clips may be needed to close the mucosotomy site. The primary outcomes we aimed to study were the rate of and predictors of gas leak and mucosal injury. The secondary outcomes assessed were comparison of time to extubation post-procedure including when gas leak occurred, length of myotomy, procedure time, and length of hospital stay (LOS) between groups.
Patients and Methods
Subjects and Data Collection
We performed a retrospective study comparing procedural aspects of PM-POEM to iPOEM. POEM procedures performed at a tertiary referral center from March 2016 to August 2018 were included. All included cases had mucosotomy and myotomy completed. POEM procedures were performed for the indication of achalasia, except for one case of esophagogastric junction outflow obstruction (EGJOO). Carbon dioxide (CO2) was used for insufflation in all procedures. The detailed procedure was described in our previous study.17 The PM-POEM procedure was performed following the same steps as the iPOEM. The following data were collected: age at POEM, gender, position of myotomy, length of myotomy, procedure time (the time from endoscope insertion to endoscope withdrawal, in minutes), occurrence of mucosal injury, number of clips used to close mucosal injuries, number of clips used to close the mucosotomy site (as a surrogate for difficulty creating the tunnel), incidence of gas leak, extubation time from the end of the procedure (as recorded in anesthesia procedure sheet), and LOS in days including the day of the procedure and the day of discharge. Gas leak was defined by the presence of subcutaneous emphysema, capnomediastinum, capnoperitoneum, and/or capnothorax documented by physical exam and/or imaging. These included gas leak that was found incidentally as well as on imaging that was performed for symptoms. Difficult procedures were determined by the endoscopist’s impression of the procedure being challenging, often based on the degree of difficulty in creating the submucosal tunnel and/or difficulty performing myotomy. An institutional review board (IRB) approval was obtained for the current study (IRB00089650; June 21, 2016 and renewed each year). All POEM procedures were performed by S.K. and Q.C. with experience in performing > 100 POEMs each at the time of study.
Upper Endoscopy and POEM Protocol
Patients were instructed to stay on clear liquids for 2 days before the procedure and to be nil per os (NPO) after midnight on the day of the procedure. All POEM cases were performed under general anesthesia in supine position. A clear cap was attached to the tip of the endoscope and complete upper endoscopy was performed for every case. The POEM procedure was performed as has been described previously.18 First, a submucosal injection of a solution of 1 mL methylene blue and 1 mL epinephrine mixed with 500 mL of 0.9% normal saline was used to lift the mucosa at the site of the initial mucosotomy. The initial mucosal incision was made longitudinally starting at approximately 10 cm above the squamocolumnar junction using an I-Type Hybrid Knife (ERBE, Marietta, GA, USA). Next, the endoscope with a clear cap was used to enter into the submucosal tunnel, which was further created by continued submucosal injection and dissection. The submucosal tunnel was extended into the cardia by 2 cm. The myotomy was started distally from the cardia using an I-Type Hybrid Knife to perform a circular myotomy and extended proximally in retrograde fashion. The length of the myotomy was determined by the type of achalasia. Intra-procedure bleeding was controlled with electrocautery for small vessels and Coagrasper (FD-411 QR, Olympus, Japan) for larger vessel in the submucosal tunnel in the soft coagulation mode (ERBE, Germany). The mucosal entrance to the submucosal tunnel was closed using endoscopic clips. Mucosal injuries were closed with clips. Patients were administered 4.5 g of piperacillin/tazobactam or 500 mg of levofloxacin (if allergic to penicillin) intravenously prior to mucosotomy incision and were continued for a total of 5 days of antibiotics in IV/PO form. All patients were admitted for overnight observation with NPO status (6 patients in the iPOEM group were already admitted as inpatient and therefore stayed longer. The procedure was performed as inpatient after our team was consulted). A gastrografin esophagram study was routinely performed the next morning after POEM cases before allowing oral intake to rule out a leak per the endoscopist discretion until end of 2017. However, due to lack of significance and absence of clinical correlation of findings on swallow study, we halted this practice after 2017. Therefore, not every case had imaging routinely available post-procedure after that date unless clinically indicated.
Statistical Analysis
IBM®SPSS® version 25 (Armonk, NY) was used for statistical analysis. Mann–Whitney U-test was used to compare continuous outcomes and results are reported as means ± standard deviation (SD). Chi-square analysis with Fisher exact test was used to compare binary categorical outcomes with results reported as percentage (%) and odds ratio (OR) with 95% confidence interval (CI). Analyses assumed a two-tailed p valued of < 0.05 for statistical significance.
Results
Subjects
Table 1 shows study subjects’ characteristics. There were 21 subjects (52.4% male) in the PM-POEM group and 56 (39.3% male) in the iPOEM group who met inclusion criteria. The PM-POEM group was younger with an average age of 44.33 vs 57.57 (41.2–74) years, p=0.0082. The first myotomy in the PM-POEM group was HM in 8/21 (38.1%) and POEM in 13/21 (61.9). The studied POEM was the 3rd myotomy in three cases in the PM-POEM group: one case had 2 prior HMs and two cases had previous HM and POEM. Table 2 shows the indication and position for myotomy in each group. All cases underwent posterior myotomy in the iPOEM except for only 1 case, in which a lateral myotomy at 3 O’clock was performed as adequate submucosal lift could not be achieved posteriorly. In the PM-POEM group, posterior myotomy was performed in 11 cases (including 1 case that had previous anterior HM and posterior POEM), lateral myotomy in 7 cases (1 case with prior Heller myotomies anteriorly and posteriorly, 1 case with prior POEMs anteriorly and posteriorly, 5 cases with prior posterior POEM), anterior myotomy in 2 cases, and not specified in 1 case. The posterior myotomy orientation despite previous posterior myotomy and lateral orientation of myotomy after only a prior posterior myotomy were decided by the endoscopist intra-operatively and no further details are available as to why the myotomy position was selected given the retrospective nature of the study.
 |
Table 1 Characteristics and Data of Study Subjects+ |
 |
Table 2 Indication and Position of POEM in Both Groups |
Gas Leak
The incidence of gas leak was higher in the PM-POEM group, but it did not reach statistical significance (28.6% vs 14.3%; OR, 2.40, 95% CI, 0.72–8.02, p=0.148). We separately compared the incidence of gas leak between groups for cases with an imaging modality available after the procedure. Radiologic comparison was available in 29 patients who had imaging performed for post-procedural respiratory distress (n=3), abdominal pain (n=3), neck crepitus (n=1), chest pain (n=1), weight loss (n=1), and routine gastrografin swallow on the next day following POEM (n=20). Again, there was a trend towards a higher rate of gas leak with PM-POEM, but the difference was not statistically significant (60% vs 42.1%, OR, 2.06, 95% CI, 0.43–9.80, p=0.359).
Mucosal Injury
Mucosal injury occurred in 38.1% (8/21) in the PM-POEM group compared to 12.5% (7/56) in the iPOEM. The mucosal injuries were all full thickness whether thermal or traumatic and all were closed with clips in both groups, except for one case in the iPOEM group (bleeding at GE junction that stopped spontaneously). The odds of mucosal injury were four-fold higher in the PM-POEM group (OR, 4.31; 95% CI, 1.32–14.08, p=0.012), and more clips were used in the PM-POEM to close mucosal injuries (0.62 vs 0.14 clips, p=0.0053).
Post-Procedure Time to Extubation
The time to extubation after the procedure was not different between PM-POEM and iPOEM (11.38 vs 9.46 minutes, p=0.93). However, the time to extubation was longer when gas leak occurred (15.92 vs 8.67 minutes, p=0.027), Figure 1. Gas leak occurred in 14/77 (18.2%) of the cases in the entire cohort (Table 3).
 |
Table 3 Extubation Time When Gas Leak Occurred |
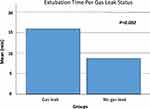 |
Figure 1 Extubation time based on gas leak status. |
Other Variables
More procedures were deemed to be difficult or challenging in the PM-POEM (33.3% vs 7.1%; OR 6.5, 95% CI, 1.7–25.4, p=0.007). However, difficulty of the procedure was not associated with incidence of either gas leak (OR 1.87; 95% CI, 0.43–8.21, p=0.410) or mucosal injury (OR 1.04; 95% CI, 0.25–4.28, p=1.000). Presence of symptoms did not predict incidence of gas leak (OR 4.87, 95% CI, 0.78-3-0.29, p=0.109). Regarding the esophageal anatomy, 5 cases (23.8%) in the PM-POEM group had a sigmoid esophagus with one case of gas leak detected, whereas 3 cases (5.3%) in the iPOEM group had sigmoid esophagus with one case of gas leak. Sigmoid configuration was not associated with gas leak occurrence (p=0.597). All sigmoid shaped cases were sigmoid-type S1. No case required intervention for gas leak decompression. No endoscopy was required after any case and there was no intensive care unit (ICU) admission pertinent to the procedure.
The length of myotomy was not statistically different between groups (6.38 cm in PM-POEM group vs 7.14 cm in iPOEM, p=0.074). Short myotomy (≤5 cm) was performed in 5 (23.8%) cases in the PM-POEM group and 5 (8.9%) cases in the iPOEM. In the PM-POEM group, one case had only a 3 cm long myotomy performed due to difficulty creating a long tunnel, altered muscle plane/lower esophageal sphincter anatomy in the setting of inflammation and tortuosity. The procedural time was longer in the PM-POEM (61.3 vs 45.4 minutes, p=0.001). When adjusted for time per myotomy length (min/cm), the time was still longer in the PM-POEM group (10.14 vs 6.66 min/cm, p=0.0005). Although the procedure was deemed overall to be more difficult and challenging in the PM-POEM group, the number of clips used to close the mucosotomy defect (as a surrogate for difficulty creating the tunnel) was not different (4.05 vs 3.84 clips, p=0.498). The average LOS was not different between groups (2.4 in the PM-POEM vs 3.14 in the iPOEM, p=0.57).
Discussion
In this retrospective study comparing PM-POEM to iPOEM, we found that performing POEM after a prior myotomy was associated with more mucosal injuries (and more clips used to close them), was more technically challenging, and had longer procedural time.
Although there was a trend toward higher incidence of gas leak in the PM-POEM group, it did not reach statistical significance, perhaps due to a smaller sample size in the PM-POEM group. However, due to high efficacy of POEM and HM procedure for achalasia, PM-POEM is not commonly performed and to obtain a higher number of cases a multicenter study would have to be performed. The incidence of gas leak seen in our study, whether in iPOEM or PM-POEM, is likely an underestimate of the true incidence had routine post-procedure imaging been obtained in all cases. Pannu et al has reported an incidence of 86% in a study of 84 consecutive POEM undergoing CT esophagram.14 Additionally, using air instead of CO2 insufflation and using medium to high flow CO2 will likely lead to more gas-related AEs. It has been shown that longitudinal mucosal incision, smaller tunnel width (≤3 cm), and sigmoid-shaped esophagus are independent predictors of gas-related AEs.19 We commonly perform longitudinal mucosal incision during POEM procedures at our institution. Sigmoid-shaped esophagus was not associated with gas leak in our cohort; however, the number of these cases was very small.
Mucosal injuries were encountered more in the PM-POEM group. This is likely from inflammation with subsequent submucosal fibrosis from prior myotomy, which has been shown to make the procedure more challenging.7,17 It is thought by some that mucosal injuries occur less frequently with a posterior approach.13 About 48% of the PM-POEM cases in our study had a non-posterior approach (Table 2), which may additionally explain the higher incidence of mucosal injuries in this group. In a study by Zhang et al, the rate of mucosal injury was not different between PM-POEM (after prior HM) and iPOEM (28.3% vs 30.5%).8 The mucosal injuries in our PM-POEM cohort were higher (38.1%). This may be explained by a smaller sample size, which can in turn exaggerate the numbers in this group. The mucosal injury rate was much lower in our iPOEM cohort (12.5%). Moreover, posterior myotomy orientation despite previous posterior myotomy in 6 cases and lateral orientation of myotomy after only a prior posterior myotomy in 5 cases were decided by the endoscopist intra-operatively and no further details are available as to why the myotomy position was selected given the retrospective nature of the study. This may have led to making the procedure difficult and therefore increase the risk of mucosal injury.
The time to extubation did not differ between groups; however, it was longer in cases when gas leak occurred. The occurrence of gas leak in these cases was discovered on imaging performed after the procedure when the patients were already extubated. Therefore, we are unable to make any assumption whether incidence of gas leak led to a longer extubation time given the event was unknown at time of extubation. It is possible that incidence of gas leak led to some hemodynamics and/or lung mechanic changes that led to delay in extubation post-procedure. However, this delay was short and did not prevent extubation. No cases required any additional intervention or ICU admission in the study. Although our anesthesia providers follow a similar pattern of practice at the institution where the study was performed, the extubation time is multifactorial and operator and non-operator variables play a role. Our investigation showed that there might be a signal, and this may warrant further prospective clinical investigation to assess any link between gas leak and delay in extubation.
Whether the duration of PM-POEM procedure is longer compared to an iPOEM is debatable and currently available data are conflicting.7,10,20 In our study, the procedure time, from the scope insertion to the time the scope was withdrawn from the esophagus, was longer in the PM-POEM group, 63.1 vs 45.4 minutes (p=0.0017). Although recent studies showed no difference in procedure times between PM-POEM and iPOEM, the overall procedure time in our study was considerably shorter compared to these studies.7,21 Likewise, studies’ results differ in regard to the length of myotomy between PM-POEM and iPOEM, with recent studies showing no difference7,8,21 while another study showed shorter myotomy in cases of prior HM.10 The myotomy length was shorter in the PM-POEM group in our study, but the difference did not reach statistical significance. While myotomy length can differ per operator’s discretion altered muscle plane from prior myotomy may limit the ability as to how much the endoscopist may opt to cut during the procedure.
The current study has some limitations. In addition to what mentioned earlier, this is a retrospective study relying on documentation in electronic medical records and documentation deficiency is a limitation in this type of studies. However, the focus of this study was on the peri-procedural period and the documentation is probably not affected given the real-time documentation by endoscopists and anesthesia staff. Lack of imaging after each case did impact determining the estimate of the actual incidence of gas leak during or after each procedure. Therefore, larger prospective studies with documented imaging during or soon after each procedure will be required for more accurate estimates.
Conclusion
Performing POEM after a prior myotomy can be more difficult, takes longer time to complete the procedure, and is associated with more mucosal injuries. Gas leak may be associated with a slightly longer post-procedure extubation time, but clinical relevance is unclear given incidence of gas leak was unknown at time of extubation in this study. Additionally, gas leak does not appear to affect the overall procedural outcomes or prolong hospitalization.
Ethics
The study was approved by the Emory University Institutional Review Board. Consent was waived given the study was retrospective in nature without any personal identification data. The study complied with the Declaration of Helsinki.
Acknowledgment
An abstract of these data was presented as a poster at the American College of Gastroenterology annual meeting in 2019 in San Antonio, Texas. https://journals.lww.com/ajg/Abstract/2019/10001/439_Risk_of_Air_Leak_and_Mucosal_Injury_in.439.aspx
Disclosure
None of the authors has conflict of interest or financial ties to disclose.
References
1. Inoue H, Minami H, Kobayashi Y, et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42(4):265–271. doi:10.1055/s-0029-1244080
2. Haito-Chavez Y, Inoue H, Beard KW, et al. Comprehensive analysis of adverse events associated with per oral endoscopic myotomy in 1826 patients: an international multicenter study. Am J Gastroenterol. 2017;112(8):1267–1276. doi:10.1038/ajg.2017.139
3. Shiwaku H, Inoue H, Sato H, et al. Peroral endoscopic myotomy for achalasia: a prospective multicenter study in Japan. Gastrointest Endosc. 2020;91(5):1037–1044.e2. doi:10.1016/j.gie.2019.11.020
4. Onimaru M, Inoue H, Ikeda H, et al. Peroral endoscopic myotomy is a viable option for failed surgical esophagocardiomyotomy instead of redo surgical Heller myotomy: a single center prospective study. J Am Coll Surg. 2013;217(4):598–605. doi:10.1016/j.jamcollsurg.2013.05.025
5. Vigneswaran Y, Yetasook AK, Zhao JC, Denham W, Linn JG, Ujiki MB. Peroral endoscopic myotomy (POEM): feasible as reoperation following Heller myotomy. J Gastrointest Surg. 2014;18(6):1071–1076. doi:10.1007/s11605-014-2496-2
6. Zhou PH, Li QL, Yao LQ, et al. Peroral endoscopic remyotomy for failed Heller myotomy: a prospective single-center study. Endoscopy. 2013;45(3):161–166. doi:10.1055/s-0032-1326203
7. Ngamruengphong S, Inoue H, Ujiki MB, et al. Efficacy and safety of peroral endoscopic myotomy for treatment of achalasia after failed Heller myotomy. Clin Gastroenterol Hepatol. 2017;15(10):1531–1537. doi:10.1016/j.cgh.2017.01.031
8. Zhang X, Modayil RJ, Friedel D, et al. Per-oral endoscopic myotomy in patients with or without prior Heller’s myotomy: comparing long-term outcomes in a large U.S. single-center cohort (with videos). Gastrointest Endosc. 2018;87(4):972–985. doi:10.1016/j.gie.2017.10.039
9. Fumagalli U, Rosati R, De Pascale S, et al. Repeated surgical or endoscopic myotomy for recurrent dysphagia in patients after previous myotomy for achalasia. J Gastrointest Surg. 2016;20(3):494–499. doi:10.1007/s11605-015-3031-9
10. Kristensen HO, Kirkegard J, Kjaer DW, Mortensen FV, Kunda R, Bjerregaard NC. Long-term outcome of peroral endoscopic myotomy for esophageal achalasia in patients with previous Heller myotomy. Surg Endosc. 2017;31(6):2596–2601. doi:10.1007/s00464-016-5267-1
11. Huang Z, Cui Y, Li Y, Chen M, Xing X. Peroral endoscopic myotomy for achalasia patients with prior Heller myotomy: a systematic review and meta-analysis. Gastrointest Endosc. 2020. doi:10.1016/j.gie.2020.05.056
12. Tyberg A, Seewald S, Sharaiha RZ, et al. A multicenter international registry of redo per-oral endoscopic myotomy (POEM) after failed POEM. Gastrointest Endosc. 2017;85(6):1208–1211. doi:10.1016/j.gie.2016.10.015
13. Nabi Z, Reddy DN, Ramchandani M. Adverse events during and after per-oral endoscopic myotomy: prevention, diagnosis, and management. Gastrointest Endosc. 2018;87(1):4–17. doi:10.1016/j.gie.2017.09.029
14. Pannu D, Yang D, Abbitt PL, Draganov PV. Prospective evaluation of CT esophagram findings after peroral endoscopic myotomy. Gastrointest Endosc. 2016;84(3):408–415. doi:10.1016/j.gie.2016.02.022
15. Yang S, Zeng MS, Zhang ZY, Zhang HL, Liang L, Zhang XW. Pneumomediastinum and pneumoperitoneum on computed tomography after peroral endoscopic myotomy (POEM): postoperative changes or complications? Acta Radiol. 2015;56(10):1216–1221. doi:10.1177/0284185114551399
16. Wang L, Li YM. Recurrent achalasia treated with Heller myotomy: a review of the literature. World J Gastroenterol. 2008;14(46):7122–7126. doi:10.3748/wjg.14.7122
17. Wu QN, Xu XY, Zhang XC, et al. Submucosal fibrosis in achalasia patients is a rare cause of aborted peroral endoscopic myotomy procedures. Endoscopy. 2017;49(8):736–744. doi:10.1055/s-0043-113440
18. Dacha S, Wang L, Li X, et al. Outcomes and quality of life assessment after per oral endoscopic myotomy (POEM) performed in the endoscopy unit with trainees. Surg Endosc. 2018;32(7):3046–3054. doi:10.1007/s00464-017-6015-x
19. Wang X, Tan Y, Zhang J, Liu D. Risk factors for gas-related complications of peroral endoscopic myotomy in achalasia. Neth J Med. 2015;73(2):76–81.
20. Louie BE, Schneider AM, Schembre DB, Aye RW. Impact of prior interventions on outcomes during per oral endoscopic myotomy. Surg Endosc. 2017;31(4):1841–1848. doi:10.1007/s00464-016-5182-5
21. Yeniova AO, Yoo IK, Jeong E, Cho JY. Comparison of peroral endoscopic myotomy between de-novo achalasia and achalasia with prior treatment. Surg Endosc. 2020. doi:10.1007/s00464-020-07380-3
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
