Back to Journals » International Journal of General Medicine » Volume 14
Functional Health Literacy in Patients with Cardiovascular Diseases: Cross-Sectional Study in Ethiopia
Authors Tilahun D , Gezahegn A, Tegenu K, Fenta B
Received 27 January 2021
Accepted for publication 25 March 2021
Published 19 May 2021 Volume 2021:14 Pages 1967—1974
DOI https://doi.org/10.2147/IJGM.S304007
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Desalew Tilahun,1 Adanech Gezahegn,2 Kenenisa Tegenu,1 Belete Fenta3
1Nursing School, Faculty of Health Science, Institute of Health, Jimma University, Addis Ababa, Ethiopia; 2Health Information, Jimma Medical Center, Addis Ababa, Ethiopia; 3Midwifery School, Faculty of Health Science, Institute of Health, Jimma University, Addis Ababa, Ethiopia
Correspondence: Desalew Tilahun Email [email protected]
Objective: This study assessed functional health literacy and associated factors among adult patients with cardiovascular diseases (CVDs) in Ethiopia.
Methods: A cross-sectional study was conducted on 410 respondents from May 1 to July 1, 2020, using a functional health literacy questionnaire consisting of 14 items that covers three conceptually distinct functional health literacy domains: having sufficient information to manage my health, ability to find good health information and understand health information well enough to know what to do. Data were analyzed using the Statistical Package for Social Sciences (SPSS) Version 23. Data were collected by exit face-to-face interview using an interviewer administered and pre-tested questionnaire. Statistical significance of associated variables had been declared based on the adjusted odds ratio (AOR) with its 95% CI and p-value < 0.05.
Results: Adequate functional health literacy was determined in 55.4% of CVD patients understanding health information whereas inadequate functional health literacy was determined in 53.9% participants for finding health information and in 50.5% of them having sufficient information to manage my health. Educational status was found to have a statistically significant association across the three domains.
Conclusion: The functional health literacy level of CVD patients varied by domain. Educational status of the participant is significantly associated with the three domains of functional health literacy whereas household monthly income and number of information sources are significantly associated with having sufficient information and the ability to find good health information. The findings indicate the need to streamline medical communication that improves the functional health literacy of CVD patients.
Keywords: health literacy, cardiovascular diseases, adults, Ethiopia
Introduction
Cardiovascular diseases (CVDs) result in millions of deaths around the world annually, most of which are avoidable if identified early.1 In Ethiopia, non-communicable diseases (NCDs) cause 42% of deaths, of which 27% are premature deaths, that is, before 70 years of age.2 Of these, CVD accounts for 24% of deaths.3 Preventive healthcare takes a prominent role in the fight against CVD.1 Health literacy (HL) is an effective means of preventing primary and secondary CVD,4 through generating and understanding effective prevention mechanisms for the management of CVD as a lifelong process.5 It does so by addressing cardiac rehabilitation components such as patient assessment, education and self-management strategies to promote behaviour change, exercise, psychosocial support and medical follow-up.6 Furthermore, HL plays a crucial role in prevention, adherence to treatment, self-care, and better use of health care.7
Health literacy represents cognitive and social skills that involve understanding access to and use of information in the way it promotes and maintains good health.8 On the other hand, HL also refers to the use of health information to follow medical instructions and communication with healthcare providers on the journey of receiving healthcare services.9–12 Functional health literacy (FHL) is one component of HL denoting sufficient basic reading and writing skills to function effectively in everyday circumstances.13 FHL encompasses three of the nine HL domains identified in Health Literacy (HLQ): Understanding health information, having sufficient information and finding useful health information.9
The functional health literacy level (FHLL) of patients with CVD is linked with patients' knowledge about their diseases, which can further affect patients’ health status, disease complications and14 disease outcomes.14,15 For example, CVD patients with inadequate FHLL experience a higher frequency of hospitalization,16 an increased risk of mortality,17,18 lower receipt of preventive services, a poorer ability to interpret labels and health messages, a higher rate of medication errors have poorer overall health status.19 They are also challenging to counsel, less likely to comprehend the benefits and risks of medication adherence,20 have little capacity for self-care, are unlikely to modify risky lifestyles, more frequently develop CNCD complications21 and have diminished self-management and decision-making skills.22 Lower FHL in CVD patients is associated with impaired comprehension of the disease and medical instructions and an inability to question healthcare professionals.23
Overall, HL is the sum of many factors, including where the person lives. For example, a study conducted in Slovakia with medical students revealed high FHLL relating to finding useful health information (70%) and understanding health information (75.6%).24 In contrast, a study in Nepal found high FHLL on functional health literacy domains such as having sufficient information (23.5%), finding useful health information (24.8%) and understanding health information (25.2%).25
Several studies7,26–30 have suggested that differences of FHLL across the globe in relation to health literacy domains are associated with socio-demographic and socio-economic characteristics (including age, sex, residence, marital status, education status, occupational status and income) and disease-related factors. However, there is a paucity of information about functional health literacy and associated factors among patients with CVD in Ethiopia. Thus, this study aimed to identify personal and socio-demographic factors associated with functional health literacy in CVD patients in Ethiopia.
Materials and Methods
Study Design and Setting
A cross-sectional study was conducted from May 1 to July 1, 2020, at a chronic illness clinic follow-up in JMC, Ethiopia. JMC is one of the oldest public hospitals that provides inpatient, outpatient, emergency, and chronic clinic follow-up services for an estimated 15 million people in soutwest Ethiopia. Per year, a total of 16,000 patients with chronic non-communicable diseases receive follow-up at the medical center, among which 1200 were identified as having CVD during data collection.
Study Population
The study included all adult patients aged 18 years and above receiving follow-up care at JMC for CVD and excluded those patients who had a hearing impairment or were seriously ill and required urgent care at the time of data collection. A total of 422 study participants were identified using a single population proportional sample size calculation formula based on a 50% health literacy estimate since there is no prevalence data in the context of Ethiopia. We used a 95% confidence interval; Zα/2 =1.96, margin of error=0.05 and non-response rate = 1
Ahead of the actual data collection, details of patients who attended the clinic over the period of two months were obtained from the patient registration logbook. In two months, there were 1200 patients with CVD. We used a simple random sampling technique to select individual study participants whereby each patient's card was given a unique code and then patients’ cards were randomly selected online using https://www.calculatorsoup.com/calculators/statistics/random-number-generator.php.
Data Collection Procedure, Method and Instrument
We confirm that the institutional review board (IRB) of Jimma University approved both the study and the consent process. Then the letter of permission was given to Jimma University medical center administrative body and this study was conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from literate patients and oral consent from illiterate patients. Data collectors explained the objectives and their right to refuse and discontinue the data collection process.
The functional health literacy (FHL) measurement tool was adopted from the comprehensive Health Literacy Questionnaire (HLQ), which was initially developed using a grounded, validity-driven approach9 and has been validated. Bayesian confirmatory factor analysis has deep-rooted high composite reliability in all nine HLQ scales (Cronbach’s alpha ≥0.8).31 The HLQ has been validated and translated into many languages and used to examine health literacy across many different populations, cultures and settings,11,32–38 including Australia.35,39–43 The FHL scale consists of 14 items that cover three conceptually distinct domains of health literacy representing scale 2.8 and 9 in HLQ: HLQ2 – having sufficient information (4 items), HLQ8 –finding health information (5 items) and HLQ9 – understanding health information (5 items).9 For HLQ1, four-point ordinal response options were used, and participants were asked to rate their level of agreement on HLQ statements as 1 = strongly disagree, 2 = disagree, 3 = agree and 4 = strongly agree; for HLQ2 and HLQ3, the five-point ordinal responses were: 1 = cannot do, 2 = very difficult, 3 = quite difficult, 4 = quite easy and 5 = very easy.44
The scoring algorithm of HLQ produces independent scores for each of the three domains of the FHL. The scorings for each domain were calculated by adding each item’s score for a domain, then multiplying it by the total number of items in the domain and, finally, dividing it by the maximum possible score of that domain. Thus, HLQ does not yield one overall summative score.9 High scores for each domain reflect high HLL within the domain and vice versa. The logic behind the use of HLQ is that it measures conceptually distinct scores in each domain that indicate a person’s strengths and weaknesses in relation to their health literacy.9
Data were also collected on patients' socio-demographic and socio-economic characteristics (age, residence, monthly household income, sex and marital, occupational and educational status), disease-related factors (complications and co-morbidity). The instrument was translated to Afaan Oromo and Amharic versions by experts who were fluent in both languages and translated back to English to check its consistency. Then Afaan Oromo and Amharic versions of the HLQ were used for data collection. Data was collected using a pretested translated version of the instrument through face-to-face interviews at a chronic illness clinic by two trained and experienced BSC nurses. It took 15–20 minutes to complete. The hospital COVID-19 prevention strategies were used, including using masks and hand sanitizers and maintaining a minimum 1.5-meter distance between interviewers and interviewees in an open room.
Data Quality Handing, Process and Analysis
Data quality was ensured during data collection, coding, double-data entry and analysis. One day's training was given to a supervisor and data collectors on data collection tools and procedures to prevent any confusion and ensure a common understanding of the study. A pre-test was done with 5%21 of the sample participants prior to actual data collection to assess the clarity and reliability of the data collection tool. Data from the pre-test was not included in the actual data. The scale reliability was assessed using the internal consistency of the reliability test. By far, all constructs of FHL reported excellent reliability, with an overall alpha value of 0.95 and more than 0.8 for each domain. Close supervision of the data collection process was carried out, and the completeness and consistency of questionnaires were checked on a daily basis. The data entry and cleaning processes were also closely monitored.
Data was coded, processed, entered into Epidata V3.1 and then exported to SPSS V23 for analysis. Before the actual data analysis, data was explored for completeness, outliers and missing values and then cleaned. We found no missing data. Next, descriptive (frequency, percentage) measures of central tendency (means) and dispersion (standard deviation, range) were computed. Multicollinearity was checked before the data analysis, and collinearity statistics showed that independent variables were uncorrelated given that variance of inflation factor (VIF) <10 and tolerance test is less than one for all independent variables. All independent variables with a p-value of 0.25 (to include important variables in multivariate analysis) after running for bivariate logistic regression were candidates for multivariate analysis using backward LR logistic regression. In the final model, variables with a p-value of less than 0.05 were regarded as significantly associated with functional health literacy domains.
Inter-quartile ranges were calculated for all included FHL domains separately, where the upper quartile cut-offs were used to define “high FHLL” and the lower two quartiles as “low health literacy level”. This applied to categorization of all three FHL domains as there was no standard cut-off.25
Results
Patient Characteristics
Out of 422 participants, 410 gave their responses, giving a response rate of 97.2%. The age of study participants ranged from 18–88, with a mean age of 48 years (SD = 14.9). More than half, 211 (51.7%), of study participants were male. Over half, 219 (53.9%), were rural residents. Just under three-quarters, 301 (73.8%), were married. The majority (83.6%) of study participants had one co-morbidity and close to three-quarters (73.3%) had complications from CVD (Table 1).
 |
Table 1 Sample Characteristics |
Functional Health Literacy Level (FHLL)
Table 2 illustrates the functional health literacy level of study participants. Patients with CVD had low FHLL except for in the understanding health information domain; here, more than half of the participants had high FHL. Mostly low FHL was the case for the finding health information domain.
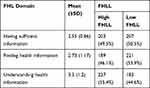 |
Table 2 Functional Health Literacy Level |
Factors Associated with FHL Domains
Table 3 summarizes factors associated with FHL domains. Those study subjects with a monthly income of more than 1000 birr are 2.93 times more likely to get sufficient health information, as are participants with an educational level of college and above (2.92 times more likely). Female patients with CVD are 35% less likely to have sufficient health information than their male counterparts. In relation to finding useful healthcare information, participants who attended college and above are 8 times, those who completed grades 9–12 are almost 3.3 times, those who completed grades 1–8 are 2.6 times, study subjects with a household monthly income of more than 1000 birr are 2 times and those with 500–1000 birr are 1.6 times more likely to do so. In contrast, study subjects who had complications from the disease are 15% less likely to find useful health information.
 |
Table 3 Multivariate Logistic Regression Analysis of Factors Associated with FHL Domains |
Those study participants with CVD who attended college and above are 4.5 times, those who completed grades 9–12 are 3.8 times, those with a monthly household income higher than 1000 birr are 3.3 times, those who completed grades 1–8 are 3 times and those with a household monthly income of 500–1000 birr are 2.9 times more likely to understanding health information.
Discussion
To the best of our knowledge, this is the first study of its kind in the context of Ethiopia. The overall findings show that just under half of patients with CVD had low FHLL for understanding health information, more than one out of two patients for finding health information and one out of two for having sufficient information. Though it varies from domain to domain, the low FHLL in domains indicates that the majority of patients with CVD on follow-up at Jimma Medical Center, Ethiopia, ack the cognitive and social skills that promote and maintain good health,8 are unable to follow necessary medical instructions29 or have inadequate communication with healthcare providers on the journey of receiving healthcare services.9–12
The findings of the current study on FHL domains reveal that the participants were less able to find useful health information and understand health information than the Slovakian medical students questioned in a previous study.24 This discrepancy could be due to variations in the study population and socio-demographic characteristics. For example, the study carried out in Slovakia involved medical students who can search for, read and understand health-related information, so that they can stay up to date, which in turn is positively linked with high FHLL and, ultimately, improved overall health status. In contrast, in this study more than one-third of respondents were in the age range 50–65 years and had not received formal education. Cognitive abilities decline with age, making reading about and comprehending one's disease more difficult and resulting in less attention being paid to prevention.
However, the results found in this study were higher than those identified in Nepal in relation to the FHL domains of: having sufficient information, finding useful health information and understanding health information.25 This could be due to variations in socio-demographic characteristics and the number of chronic diseases experienced by study participants. For example, of the study participants in Nepal, close to three-quarters had two or more co-morbidities, which challenges them to self-manage as most guidelines are available for a single disease. This indicates that having two or more chronic diseases is likely to make managing daily treatment regimens more difficult. Dealing with complex disease management can lead to low FHL and eventually poor health outcomes. It may also be challenging to navigate the health care system and comprehend and appraise information relating to two diseases at the same time. In addition, 70 out of 100 study respondents were also uneducated, which means they were unable to read and comprehend medical information provided by healthcare providers, which in turn led to their having less knowledge about their disease, then to paying less attention to prevention and, ultimately, low FHLL.
There are several factors affecting individual FHL.7,26–30 In our study and others, educational status was shown to be significant because educated people are more likely to have sufficient information to manage their health and better judge health-related information.26 Educated individuals may be aware about their diseases so they may participate in preventive services for early diagnosis, which in turn prevents disease complications and comorbidities, which enables them to prevent disease burden. Moreover, educated individuals possess knowledge about their disease,7 are proactive and confident enough to communicate with healthcare providers and gain information about their health,27 can make sound decisions when navigating the healthcare system and their improved HL ultimately improves their treatment outcomes.26 On top of this, being educated enables people to get better jobs, earn a good income and hence gain timely access to health services, which in turn may lead to the better health actions required for managing chronic health conditions.
In this study, monthly household income was significantly associated with three FHL domains: having sufficient information, finding useful health information and understanding health information. This association indicates that patients with high socio-economic status can access timely healthcare services as they can afford them. This finding is also supported by studies in Mashhad, Iran, Myanmar and Catalan,29,30,45 indicating that those patients with high socio-economic status can afford to get high-quality healthcare services.
In relation to finding health information, of those respondents who had complications from their disease, 15% were less likely to have high FHLL than those who had no complications. This indicates that a significant number of patients with CVD are at risk of developing poor health outcomes. This contrasts with the findings of another study,24 in which participants without chronic diseases had a low health literacy level. Summarizing the discussion, using three FHL domains of the HLQ as a tool to measure the health literacy of patients with CVD was found to be feasible and practicable. Each individual scale provided a detailed and action-oriented picture of health literacy competencies and limitations among patients with CVD.
This study has many strengths and limitations. All CVD patients receiving follow-up at the hospital had an equal chance of being included in the study. The study highlights areas of strength and weakness of patients with CVD, which is a good insight and highly relevant for organizations or practitioners seeking to intervene. The major limitations of this study are that the tool was utilized only in Ethiopia, which questions its external validity; clinical data and socio-demographic and economic status were self-reported by patients, which imposes a bias; and because it uses a cross-sectional design, the relationships identified should be interpreted as associations rather than cause and effect.
In conclusion, the study identifies that the level of functional health literacy in patients with CVD varies by domain. The current study highlights that high FHLL was seen in one of three and low FHLL in two of three FHL domains. Educational status and household monthly income were found to be significantly associated with three of the FHL domains. Complications from CVD was an independent factor in relation to finding good health information.
The findings indicate the need to design a strategy that improves the functional health literacy in CVD patients. For example, in addition to routine care, healthcare providers, especially nurses and doctors, should encourage patients to understand health information FHL domains and give due attention to providing up-to-date, reliable and applicable health information for two of three FHL domains to enhance HLL. They should also use the teach-back method and empower patients to have high FHLL so that patients can manage their CVD over their lifetime.
Abbreviations
CNCD, Chronic non-communicable diseases; SPSS, Statistical Package for Social Sciences; COR, Crude odds ratios; AOR, Adjusted odds ratio; HL, Health literacy; FHLL, Functional health literacy level; JMC, Jimma Medical Center; CVD, Cardiovascular diseases; HLQ, Health literacy questionnaire; VIF, Variance of inflation factor; LR, Likelihood ratio; SD, Standard deviation.
Data Sharing Statement
Due to no consent from the study participants to disclose raw data, this data could not be made available in order to protect the participants’ identity.
Consent for Publication
Not applicable.
Acknowledgment
We are grateful to Jimma University, Faculty of Health Science, JMC administrative body, school of nursing, nurses, and data collectors. Last but not least, we would like to thank the study participants for their wholehearted effort to provide information.
Author Contributions
All authors (DT, AG, KT and BF) made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
This work was supported by Jimma University. This funding organization hadn’t involved or hadn’t any role in the design of the study, collection, analysis, interpretation of data, and in writing the manuscript.
Disclosure
The authors reported no conflicts of interest for this work.
References
1. Karunathilake SP, Ganegoda GU. Secondary prevention of cardiovascular diseases and application of technology for early diagnosis. BioMed Res Int. 2018;2018:9. doi:10.1155/2018/5767864
2. Shiferaw F, Letebo M, Misganaw A, Feleke Y, Gelibo T. Original article Non-communicable Diseases in Ethiopia: disease burden, gaps in health care delivery and strategic directions. BMC Public Health. 2018;32(3):1–12.
3. Misganaw A, Mariam DH, Ali A, Araya T. Epidemiology of major non-communicable diseases in ethiopia: a systematic review search strategy. J Health, Popul, Nutr. 2014;32(1):1–13.
4. Dickson VV. Health literacy and cardiovascular. Circulation. 2018;138:e48–e74. doi:10.1161/CIR.0000000000000579
5. Report I WHO global coordination mechanism on the prevention and control of noncommunicable diseases using health literacy to impact on NCDs in the SDG-era. 2020;1–16.
6. Network CH. Cardiovascular rehabilitation and secondary prevention pathway principles for Western Australia. 2014;26.
7. Shrestha A, Singh SB, Camp G, Khanal V, Bhattarai S. Health literacy and knowledge of chronic diseases in nepal health literacy and knowledge of chronic diseases in Nepal. HLRP. 2018;2(4):e230. doi:10.3928/24748307-20181025-01
8. Nutbeam D, Kickbusch I. Health promotion glossary. Health Promot Int. 1998;13(4):349–364. doi:10.1093/heapro/13.4.349
9. Osborne RH, Batterham RW, Elsworth GR, Hawkins M, Buchbinder R. The grounded psychometric development and initial validation of the Health Literacy Questionnaire (HLQ). BMC Public Health. 2013;13(658):7.
10. Huang Y, Ruan T, Yi Q, Wang T, Guo Z. The health literacy questionnaire among the aged in Changsha, China: confirmatory factor analysis. Huang Al BMC Public Heal. 2019;19(1220):1–12.
11. Morris RL, Soh S, Hill KD, et al. Measurement properties of the Health Literacy Questionnaire (HLQ) among older adults who present to the emergency department after a fall: a Rasch analysis. BMC Health Serv Res. 2017;17(605):1–11. doi:10.1186/s12913-017-2520-9
12. Guzys D, Kenny A, Dickson-swift V, Threlkeld G. A critical review of population health literacy assessment. BMC Public Health. 2015;1–7.
13. Commission A, Care H. Health literacy: taking action to improve safety and quality. Australian Commission Safety And Quality In Health Care. 2014;1–94.
14. Aildasani K, Sharma N, Kaore NM. Relationship of functional health literacy to patients ’ knowledge of their own chronic diseases- an Indian perspective. The Journal of Community Health Management. 2019;6(2):59–63.
15. Sedighi M, Eghbali T, Hassan S. Health literacy among Iranian patients with type 2 diabetes: a systematic review and meta-analysis Diabetes & Metabolic Syndrome: clinical Research & Reviews Health literacy among Iranian patients with type 2 diabetes: a systematic review and meta-anal. Diabetes Metab Syndr Clin Res Rev. 2019;13(2):1341–1345. doi:10.1016/j.dsx.2019.02.020
16. Wu J, Holmes GM, Dewalt DA, et al. Low literacy is associated with increased risk of hospitalization and death among individuals with heart failure. Journal of General Internal Medicine. 2011;28(9):1174–1180.
17. Roumie CL. Health literacy and mortality: a cohort study of patients hospitalized for acute heart failure. Journal of the American Heart Association. 2015;4(e001799):1–9.
18. Peterson PN, Shetterly SM, Clarke CL, et al. Patients with heart failure. JAMA. 2011;305(16):1695–1701. doi:10.1001/jama.2011.512
19. Literacy LH, Review S. Annals of internal medicine review low health literacy and health outcomes: an updated. Ann Intern Med. 2011;155(2):19.
20. Choudhry FR, Ming LC, Munawar K. Health literacy studies conducted in australia: a scoping review. International Journal of Environmental Research and Public Health. 2019;1–32.
21. Dennis S, Williams A, Taggart J, et al. Which providers can bridge the health literacy gap in lifestyle risk factor modification education: a systematic review and narrative synthesis. BMC Fam Pract. 2012;13(1):1.
22. Taylor DM, Fraser SDS, Bradley JA, et al. Article A systematic review of the prevalence and associations of limited health literacy in CKD. Clin J Am Soc Nephrol. 2017;12:1070–1084. doi:10.2215/CJN.12921216
23. Antonio J, Neto C, Costa LA, et al. Functional Health Literacy in chronic cardiovascular patients. Cien Saude Colet. 2019;24(3):1121–1132. doi:10.1590/1413-81232018243.02212017
24. Gabriela Š, Č E, Kolar P, Madarasová A, If TD, If TD. ScienceDirect The level of health literacy of students at medical faculties. Elsevier. 2018;20(2018):e 363– e 369.
25. Narayan U, Id Y, Id JL, et al. Levels and determinants of health literacy and patient activation among multi-morbid COPD people in rural Nepal:Findings from a cross- sectional study. PLoS One. 2020;15(5):1–16.
26. Shahzad F, Saleem F, Iqbal Q, et al. A cross-sectional assessment of health literacy among hypertensive community of Quetta City, Pakistan. Biomedical Journal of Scientific and Technical Research. 2018;5(4):8685–8693.
27. Rheault H, Coyer F, Jones L, Bonner A. Health literacy in Indigenous people with chronic disease living in remote Australia. BMC Health Services Research. 2019;19(523):1–10.
28. Haghdoost AA, Karamouzian M, Jamshidi E, et al. Health Literacy among Iranian adults: findings from a nationwide population- Health literacy among Iranian adults: findings from a nationwide population-based survey in 2015. East Mediterr Health J. 2019;25(10):828–836. doi:10.26719/emhj.19.017
29. In SEJ, In P, Amirchaghmaghi M. Health literacy and its determinants in adult patients referred to dental clinics: a cross sectional study in Mashhad, Iran. Shiraze-Medical Journal.2019;11:7.
30. Oo WM, Soe PP, Lwin KT. Status and determinants of health literacy: a study among adult population in selected areas of Myanmar. International Journal of Community Medicine and Public Health. 2015;2(3):318–322.
31. Elsworth GR, Beauchamp A, Osborne RH. Measuring health literacy in community agencies: a Bayesian study of the factor structure and measurement invariance of the health literacy questionnaire (HLQ). BMC Health Serv Res. 2016;1–14.
32. Zhang NJ, Terry A, Mchorney CA. Impact of Health Literacy on Medication Adherence: a Systematic Review and meta-analysis . Ann Pharmacother. 2014;48(6):741–751. doi:10.1177/1060028014526562
33. Beauchamp A, Buchbinder R, Dodson S, et al. Distribution of health literacy strengths and weaknesses across socio-demographic groups: a cross-sectional survey using the Health Literacy Questionnaire (HLQ). BMC Public Health. 2015;15(678):13.
34. Cepova E, Cicvakova M, Kolarcik P, Markovska N, Geckova AM. Associations of multidimensional health literacy with reported oral health promoting behaviour among Slovak adults: a cross-sectional study. BMC Oral Health. 2018;18(44):1–9.
35. Hawkins M, Gill SD, Batterham R, Elsworth GR, Osborne RH. The Health Literacy Questionnaire (HLQ) at the patient-clinician interface: a qualitative study of what patients and clinicians mean by their HLQ scores. BMC Health Services Research. 2017;1–15.
36. Manhanzva R, Marara P, Duxbury T, et al. Gender and leadership for health literacy to combat the epidemic rise of non-communicable diseases. Health Care Women Int. 2017;9332(May).
37. Mullan J, Burns P, Weston K, et al. Education sciences health literacy amongst health professional university students: a study using the health literacy questionnaire. Educ Sci. 2017;7(54):11. doi:10.3390/educsci7020054
38. Nolte S, Osborne RH, Dwinger S, et al. German translation, cultural adaptation, and validation of the Health Literacy Questionnaire (HLQ). PLOS ONE. 2017;12:1–12.
39. Hosking SM, Brennan-olsen SL, Beauchamp A, Buchbinder R, Williams LJ, Pasco JA. Health literacy in a population-based sample of Australian women: a cross-sectional profile of the Geelong Osteoporosis Study. BMC Public Health. 2018;18(876):14. doi:10.1186/s12889-018-5751-8
40. Jessup RL, Osborne RH, Beauchamp A, Bourne A, Buchbinder R. Differences in health literacy profiles of patients admitted to a public and a private hospital in Melbourne, Australia. BMC Health Services Research. 2018;18(134):1–10.
41. Smith CA, Chang E, Brownhill S, Barr K. Complementary medicine health literacy among a population of older australians living in retirement villages: a mixed methods study. Shiraze-Medical Journal. 2016;2016(Cm).
42. Hosking SM, Brennan-olsen SL, Beauchamp A, Buchbinder R, Williams LJ, Pasco JA. Research in Social and Administrative Pharmacy Health literacy and uptake of anti-fracture medications in a population- based sample of Australian women. Res Soc Adm Pharm. 2018;14(9):846–850. doi:10.1016/j.sapharm.2018.05.002
43. Goodwin BC, March S, Zajdlewicz L, Osborne RH, Chambers SK. Health literacy and the health status of men with prostate cancer. Psycho-Oncol. 2018;27(June):2374–2381. doi:10.1002/pon.4834
44. Maindal HT, Kayser L, Norgaard O, Bo A, Elsworth GR, Osborne RH. Cultural adaptation and validation of the Health Literacy Questionnaire (HLQ): robust nine ‑ dimension Danish language confirmatory factor model. Springerplus. 2016;5(1232):1–16. doi:10.1186/s40064-016-2887-9
45. Garcia-codina O, Juvinyà-canal D, Amil-bujan P, et al. Determinants of health literacy in the general population: results of the Catalan health survey. Garcia-Codina Al BMC Public Heal. 2019;19(1122):1–12.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
