Back to Journals » Open Access Rheumatology: Research and Reviews » Volume 12
Functional Disability and Its Determinants in Ecuadorian Patients with Rheumatoid Arthritis
Authors Intriago M, Maldonado G , Guerrero R , Moreno M, Moreno L, Rios C
Received 28 February 2020
Accepted for publication 30 April 2020
Published 10 June 2020 Volume 2020:12 Pages 97—104
DOI https://doi.org/10.2147/OARRR.S251725
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Chuan-Ju Liu
Maria Intriago, Genessis Maldonado, Roberto Guerrero, Mario Moreno, Letty Moreno, Carlos Rios
Rheumatology Department, Universidad Espiritu Santo, Guayaquil, Ecuador
Correspondence: Genessis Maldonado Email [email protected]
Introduction: Disability in RA is associated with loss of workdays, greater use of health resources and a higher prevalence of depression. The purpose of this study was to determine the prevalence of functional disability and the factors associated with it.
Methods: A cross-sectional study was carried out during January–June 2019 at a rheumatology clinic in the city of Guayaquil. Patients with pre-established RA were included. Functional disability was measured using the HAQ-DI. Data were analyzed using the statistical program SPSS v22. We compared characteristics between patients with and without disability using Student’s t-test and chi-square. A multiple logistic regression model for functional disability was made.
Results: We included 395 patients, 87.8% female and 12.2% male with a mean age of 51.4± 12 years and mean duration of disease 13.8± 7 years. Most patients had extra-articular manifestations (80.8%) and comorbidities (81.3%). The mean HAQ-DI was 0.8± 0.9, with a prevalence of disability of 26.6%. We found a statistically significant relationship between disability and female sex (p=0.018), age (p=0.020), presence of extra-articular manifestations (p=0.008), myalgia (p< 0.001) and fatigue (p< 0.001). In addition, patients with disabilities had a lower employment rate (26.7%) compared to those without disability (45.5%, p=0.001). In the multivariate logistic analysis, only depression (p=0.029), diabetes (p=0.003), SJC (p=0.001) and VAS of pain (p=0.004) were significantly related to functional disability.
Conclusion: Disability affects a quarter of patients with RA. Among the determinants of disability, we found female sex, older age, grade of pain, inflammatory markers and the level of disease activity.
Keywords: rheumatoid arthritis, disability, Ecuador
Introduction
Rheumatoid arthritis (RA) is an autoimmune disease with a prevalence that ranges from 0.5% to 1.0%.1 This disease is the result of a chronic inflammatory state that progresses and in advanced stages causes severe limitation of the patient. Although there have been many advances in the treatment of RA, functional disability remains a serious problem for these patients. Sokka et al2 established that patients with RA have a risk of disability seven times greater than the general population. Factors that are related to a higher disability rate in patients with RA include advanced age, female sex, higher disease activity indices and higher inflammatory markers.3
Disability leads to several repercussions such as loss of workdays and greater use of health resources. It has been shown that up to 70% of patients with RA develop impairment at work after 10 years of disease progression.4 Huscher et al5 estimated that the annual direct medical costs for patients with RA with disabilities are three times higher than those for patients without disability; also, annual indirect costs that include days lost at work and disability pensions are significantly higher in patients with disability. Likewise, disability affects personal relationships and lifestyles of patients and their families and is one of the most important predictors of depression and quality of life. Ji et al6 demonstrated a significant association between functional disability in RA and depression. Another study showed that functional disability and limitations in daily activities in RA have a negative impact on quality of life.7
Several authors have studied the prevalence of disability in RA and its determinants, among them, Krause et al8 in the United States, Sokka et al2 in Finland and Öken et al9 in Turkey. Regarding Latin America, Cordeiro et al10 described the prevalence of disability in RA and associated factors in Brazil while Schneeberger et al3 in Argentina and Durán et al11 in Chile. Studies in Ecuador regarding AR are limited and there are no studies having a disability as the main outcome or describing its determinants in Ecuadorian patients.
Due to the regional differences in the severity of rheumatic diseases and the available treatments, and the impact of disability in patients with RA, the aim of this study was to study the prevalence of disability and its determinants in Ecuadorian population. By doing this, physicians might be able to recognize disability and its determinants in the clinical practice and intervene in them early to reduce the burden of the disease on functional capacity.
Materials and Methods
A cross-sectional study was carried out to determine the prevalence of disability and its determinants in RA during a period of 6 months: January 2019–June 2019. The study was carried out at a Rheumatology Center in the city of Guayaquil, Ecuador.
This study was in accordance with the Declaration of Helsinki. The patients signed a written informed consent, which reflects the approval of the clinical study according to article 361 of the Political Constitution of the Republic of Ecuador, article 7 of the Organic Health Law, and article 15–16 of the Code of Medical Ethics of Ecuador. The study was approved by the Ethics and Teaching Committee of the Centro de Reumatología y Rehabilitación (CERER) with a registration number: No.005/2019; Folio 01: Book of Acts No.1. Patient anonymity of data was respected throughout the entire investigative process, and it was explained to the participants that the data collected would be used solely for the study.
The population consisted of patients with a pre-established diagnosis of RA according to the criteria of the American College of Rheumatology (ACR) 1987 which includes morning stiffness for at least 1 hour, arthritis of three or more joints, arthritis of hand joints, symmetric distribution of the disease, rheumatoid nodules, being seropositive for rheumatoid factor and radiographic changes compatible with RA such as erosions and periarticular osteopenia.12 Patients with RA that showed to the clinic either for a first consult or a follow-up were considered for the study, which represents a convenience sampling as patients were selected from the center due to its easy accessibility. Only those that had at least four ACR criteria out of the seven possible for more than 6 weeks were 18 years or older and gave written consent to participate in the study, were included. Also, as the surveys were in Spanish, only Spanish speakers were included. Patients with other connective tissue diseases or autoimmune diseases were excluded, as well as patients with mental disabilities or physical limitations that prevented them from understanding, communicating or completing the questionnaires. Patients were asked for their authorization prior to their enrollment after an adequate explanation of the study, its purpose and their roles as participants.
Data collection was based on surveys and questionnaires. Functional disability was measured using the validated Spanish version of the Health assessment questionnaire disability index (HAQ-DI).13 This questionnaire has proved to be a good predictor of mortality, joint replacement, work disability and economic losses, in addition to being sensitive to changes in the patient’s condition over time.14 All the questionnaires were in the official language of the patient (Spanish) to facilitate understanding. On the day the patient was seen in the consult, the following five activities were carried out: filling out the basic information survey, filling out the HAQ-DI questionnaire, assessment by the rheumatologist, checking the laboratories in the medical record and calculation of the disease activity score DAS-28:
- The basic information survey was filled out by a previously trained investigator and included:
- Demographics: age, sex, race, marital status, work, smoking.
- Characteristics of the disease: years with the disease, type of articular involvement, visual analogue scale (VAS) of pain (0–10) and presence of extra-articular symptoms (Raynaud’s phenomenon, fever, fatigue, myalgia, weight loss, xerophthalmia, xerostomia).
- Comorbidities: hypertension, diabetes mellitus, dyslipidemia, thyroid disease, depression, gastrointestinal disease. This was determined by asking the patient if he/she had been previously diagnosed or receives treatment for any of these diseases.
- Current treatment: non-steroidal anti-inflammatory drugs, corticosteroids, hydroxychloroquine, methotrexate, sulfasalazine, leflunomide, anti-TNF drugs and other biologics.
- The HAQ-DI questionnaire was filled out by the patient after an explanation of it. In this case, a researcher did not participate in order to avoid bias. Disability was defined as a HAQ-DI score greater than 1.25.
- A rheumatologist assessed the patients to determine the number of swollen joints (SJC) and the number of tender joints (TJC) according to the 28 joint count for arthritis.
- Medical records were accessed to obtain the most recent values for erythrocyte sedimentation rate (ESR), C-reactive protein (CRP) and rheumatoid factor (RF).
- Using the information about tender joint count, swollen joint count, ESR and patient global health, the DAS28-ESR was calculated online at: https://www.rheumakit.com/en/calculators/das28. The patient was considered in remission if the score was less than 2.6, with a mild activity if it was 2.6 to 3.2, moderate activity 3.2 to 5.1 and high activity if greater than 5.1.
Data were analyzed using the statistical program SPSS v22. Categorical variables were described with percentages. Continuous variables were described with mean and standard deviation. The Kolmogorov–Smirnov test was used to examine for normality of distribution of continuous variables. We compared characteristics between patients with and without disability using Student’s t-test (independent samples, two-tailed) for continuous variables and chi-square for categorical variables. With the variables that were significant predictors of disability in the univariate analysis, we conducted a multiple logistic regression model for functional disability. The a-priori level used was 0.05 for all analyses.
Results
We included 395 patients, 87.8% female and 12.2% male with a mean age of 51.4±12 years. The mean duration of the disease was 13.8±7 years and 72.4% had a positive rheumatoid factor. Table 1 shows the demographics and clinical characteristics of the population.
 |
Table 1 Characteristics of the Population |
The mean DAS-28 score was 3.4±1.5; 33.7% of patients were in remission, 17.0% had low activity, 34.1% moderate activity and 15.2% high activity. The mean for TJC was 5±6 and for SJC 4±5 joints, with a mean VAS of pain of 4±3. The mean ESR was 31.9±8.9 mm/h and CRP 18.2±8.1 mg/L. The mean HAQ-DI was 0.8±0.9, with a prevalence of disability of 26.6%. The disability rate in women was 28.5% and in men 12.5%. When stratifying patients according to their age, the disability rate in those <65 years of age was 26% and in those ≥65 years of age 30.4%.
Table 2 shows the comparison between patients with and without disabilities. We found a statistically significant relationship between disability and female sex (p=0.018), age (p=0.020), presence of extra-articular manifestations (p=0.008), myalgias (p<0.001), xerostomia (p=0.023), fever (p<0.001), fatigue (p<0.001), presence of comorbidities (p<0.001), number of comorbidities (p<0.001), depression (p<0.001), hypertension (p=0.001), diabetes (p=0.030) and gastric disease (p<0.001). As for markers of disease activity, functional disability was associated with ESR (p<0.001), CRP (p<0.001), TJC (p<0.001), SJC (p<0.001), VAS of pain (p<0.001) and DAS-28 (p<0.001). In addition, patients with disability had a lower employment rate (26.7%) compared to those without disability (45.5%, p=0.001). Likewise, patients with disability reported greater sexual impairment (19%) compared to patients without disability (10.3%, p=0.022). No statistically significant associations were found between disability and duration of the disease (p=0.058), RF positivity (p=0.441), smoking (p=0.463), Raynaud phenomenon (p=0.728), xerophthalmia (p=0.069), weight loss (p=0.149), hypothyroidism (p=0.827), dyslipidemia (p=0.355) or any treatment.
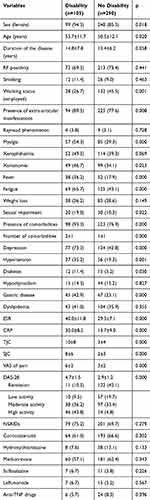 |
Table 2 Comparison Between Patients with and Without Disability |
In the multivariate logistic regression analysis, seen in Table 3, only depression (p=0.029), diabetes (p=0.003), SJC (p=0.001) and VAS of pain (p=0.004) were significantly related to functional disability. Using the Hosmer–Lemeshow test, this model had a good fit (χ2 = 11.160, P = 0.193). The Nagelkerke’s R2 suggested that the model explained 56% of the variation in the outcome.
 |
Table 3 Multivariate Logistic Regression Analyses Predictive of Disability |
Discussion
We found a prevalence of disability of 26.6%, similar to that found in other studies by Krause et al8 (28%) and Myasoedova et al15 (26%).
Among the predictors of disability, female gender and age have been described in many studies,16 which is consistent with our findings. This may be because women usually have a more aggressive disease and higher disease activity.17 In addition, aging is related to many anatomical and functional changes that can contribute to disability.
We did not find an association between disability and duration of the disease; however, in a study by Wolfe,18 it was seen that the HAQ-DI score increased at a rate of 0.020 units per year and that in 53% of patients, the grade of disability worsened with time, which can be related to the progression of the disease. In this aspect, we need to consider the effect of treatment in controlling the disease and limiting disability. Ward et al19 showed that the rate of progression of disability in patients treated regularly was 0.008 disability index units per year compared to 0.020 disability index units per year in those treated intermittently. Nowadays, biologics have shown to decrease the rate of disability by 1–3% per year, according to a study by Krishnan et al.20 Other studies have also found that treatment with biologic agents increases employability rates and decreases sick leaves.21,22 This is related to the control of the inflammation and joint damage that is achieved with biologic DMARDs. In this study, there was no significant difference in the rate of biological therapy between patients with and without disability, which could be related to the low overall use of biologics. In our study, only 9.1% of the patients used biologics which is significantly lower than the rate of biological therapy for RA in the United States (26%) described by Yazici et al.23
In this study, patients with disabilities had higher painful joints count and greater VAS of pain. Wolfe18 showed that a change of 0.5 units in the level of pain is associated with changes of 0.25 units in the HAQ-DI. One possible explanation for this relationship is that chronic pain can interfere with daily activities. Also, another study24 found that pain is not only related to disability but also to greater depression and fatigue which in turn can contribute to disability. In addition, Jeong et al25 found a greater impact on functional capacity in patients who have a compromise of the joints of the foot or ankle, which can produce changes in gait and the need for orthotic devices.
The presence of comorbidities was another determinant of disability. Patients with disabilities had a greater number of comorbidities compared to those without a disability. Similar results were found in other studies.26,27 Likewise, Radner et al26 reported a lower HAQ-DI in patients without comorbidities, which increased according to the number of comorbidities. In the study by Michaud et al,27 the comorbidities with the greatest influence on HAQ-DI were cardiac, pulmonary and psychiatric diseases. In this study, depression was significantly related to disability, as well as hypertension, diabetes and gastric disease but the only one that showed significance in the logistic regression analysis was depression; thus, highlighting the importance of addressing depression in patients with RA.
The prevalence of depression in our study was high (51%), consistent with other studies that have shown depression rates of 40%28 and 43%.29 The impact that depression has on the disease is important since it is related to greater disability, worse quality of life and higher mortality.29,30 Even in one study, it was found that patients with depression despite being in clinical remission, had scores of quality of life and disability similar to patients with high disease activity.31 This relationship between depression and disability in RA has been shown to be bidirectional. A study found that a 10% reduction in the ability to perform activities that an individual considers important, such as visiting the family or going on vacation, is followed by a sevenfold increase in depression.32 On the other hand, changes of two to three units in the depression questionnaires generate significant changes in the HAQ-DI.18 This association could be due to the fact that depression affects the threshold and the way of coping with pain and pain is also a determinant of disability.
This study also showed that patients with disabilities had a higher DAS-28, SJC, ESR and CRP. Regarding the association between disability and disease activity scores, Karpouzas et al16 found that patients with high disease activity had significantly higher HAQ-DI scores than those with low disease activity. In the study by Hakkinen et al,33 it was shown that the number of swollen joints in the lower extremities was related to the sub-dimensions of the HAQ-DI that involved walking and common activities of daily living that need weight support, while the number of swollen joints of the upper extremities influenced the sub-dimensions that require reach or grip. Also, Wolfe18 established that changes in the ESR generate significant changes in the HAQ-DI score.
Other factors that have been associated with disability are global patient evaluation, morning stiffness, grip strength and seropositivity of the rheumatoid factor.34 None of these findings were seen in this study.
The main limitation of this study is that it is cross-sectional so no causal relationships can be established between disability and its determinants. Also, we did not address radiographic damage or joint mobility which are related to disability. Another factor to consider is that sampling was done by convenience and not randomly, which means that our sample could differ from the whole population of patients with RA in Ecuador. This is important as there might be differences in the HAQ-DI score based on the mean age and the access to treatment of the patients included. However, when comparing our findings with a study by Ríos et al35 about the clinical and serological characteristics of Ecuadorian patients with RA, the description of the samples are similar. Moreover, one of the strengths of the study is that it was done with a large number of patients which might mean that the results can be generalized to the Ecuadorian population.
Conclusion
Disability affects a quarter of patients with RA. Older patients and women are more affected. Pain is one of the main determinants of disability, as well as inflammatory markers and the level of disease activity. Patients with extra-articular manifestations and comorbidities also had worse functional capacity. For this reason, the diagnosis and implementation of an early treatment in patients with RA is essential to reduce the impact of the disease on functional capacity. It should also be emphasized that depression is an important comorbidity that contributes to disability and worsens the quality of life of patients with RA, so interventions aimed at it could be an alternative to improve functional capacity and quality of life in patients with RA.
Acknowledgment
The abstract of this paper was presented at the 22nd PANLAR Congress, as a poster presentation with interim findings. The poster’s abstract was published in “Poster Abstracts” in the Journal of Clinical Rheumatology, DOI:10.1097/RHU.0000000000001389.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Helmick CG, Felson DT, Lawrence RC, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part I. Arthritis Rheum. 2008;58(1):15–25. doi:10.1002/art.23177
2. Sokka T, Krishnan E, Häkkinen A, Hannonen P. Functional disability in rheumatoid arthritis patients compared with a community population in Finland. Arthritis Rheum. 2003;48(1):59–63. doi:10.1002/art.10731
3. Schneeberger EE, Citera G, Maldonado Cocco JA, et al. Factors associated with disability in patients with rheumatoid arthritis. J Clin Rheumatol. 2010;16(5):215–218. doi:10.1097/RHU.0b013e3181e92d25
4. Burton W, Morrison A, Maclean R, Ruderman E. Systematic review of studies of productivity loss due to rheumatoid arthritis. Occup Med (Lond). 2006;56(1):18–27. doi:10.1093/occmed/kqi171
5. Huscher D, Mittendorf T, von Hinüber U, et al. Evolution of cost structures in rheumatoid arthritis over the past decade. Ann Rheum Dis. 2015;74(4):738–745. doi:10.1136/annrheumdis-2013-204311
6. Ji J, Zhang L, Zhang Q, et al. Functional disability associated with disease and quality-of-life parameters in Chinese patients with rheumatoid arthritis. Health Qual Life Outcomes. 2017;15(1):89. doi:10.1186/s12955-017-0659-z
7. Salaffi F, Carotti M, Gasparini S, Intorcia M, Grassi W. The health-related quality of life in rheumatoid arthritis, ankylosing spondylitis, and psoriatic arthritis: a comparison with a selected sample of healthy people. Health Qual Life Outcomes. 2009;7(1):25. doi:10.1186/1477-7525-7-25
8. Krause ML, Crowson CS, Bongartz T, et al. Determinants of disability in rheumatoid arthritis: a community-based cohort study. Open Rheumatol J. 2015;9(1):88–93. doi:10.2174/1874312901409010088
9. Oken O, Batur G, Gündüz R, Yorgancioğlu RZ. Factors associated with functional disability in patients with rheumatoid arthritis. Rheumatol Int. 2008;29(2):163–166. doi:10.1007/s00296-008-0661-1
10. Cordeiro K, Silva M, Galvão T, Pereira M. Functional disability of adults in Brazil: prevalence and associated factors. Rev Saúde Pública. 2015;49:89.
11. Durán J, Domínguez A, Espinoza M. Evaluation of the health assessment questionnaire disability index in Chilean patients with rheumatoid arthritis. Rev Méd Chile. 2019;147(5):612–617.
12. Arnett FC, Edworthy SM, Bloch DA, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. 1. Arthritis Rheum. 1988;31(3):315–324. doi:10.1002/art.1780310302
13. Cardiel MH, Abello-Banfi M, Ruiz-Mercado R, Alarcon-Segovia D. How to measure health status in rheumatoid arthritis in non-English speaking patients: validation of a Spanish version of the Health Assessment Questionnaire Disability Index (Spanish HAQ-DI). Clin Exp Rheumatol. 1993;11(2):117–121.
14. Wolfe F. The determination and measurement of functional disability in rheumatoid arthritis. Arthritis Res. 2002;4(Suppl 2):S11–5. doi:10.1186/ar547
15. Myasoedova E, Davis JM
16. Karpouzas GA, Dolatabadi S, Moran R, Li N, Nicassio PM, Weisman MH. Correlates and predictors of disability in vulnerable US Hispanics with rheumatoid arthritis. Arthritis Care Res. 2012;64:1274–1281.
17. Intriago M, Maldonado G, Cárdenas J, Ríos C. Clinical characteristics in patients with rheumatoid arthritis: differences between genders. Sci World J. 2019;2019:6. doi:10.1155/2019/8103812
18. Wolfe F. A reappraisal of HAQ disability in rheumatoid arthritis. Arthritis Rheum. 2000;43(12):2751–2756. doi:10.1002/1529-0131(200012)43:12<2751::AID-ANR15>3.0.CO;2-6
19. Ward MM, Leigh JP, Fries JF. Progression of functional disability in patients with rheumatoid arthritis. Associations with rheumatology subspecialty care. Arch Intern Med. 1993;153(19):2229–2237. doi:10.1001/archinte.1993.00410190069009
20. Krishnan E, Lingala B, Bruce B, Fries JF. Disability in rheumatoid arthritis in the era of biological treatments. Ann Rheum Dis. 2012;71(2):213–218. doi:10.1136/annrheumdis-2011-200354
21. Halpern MT, Cifaldi MA, Kvien TK. Impact of adalimumab on work participation in rheumatoid arthritis: comparison of an open-label extension study and a registry-based control group. Ann Rheum Dis. 2009;68(6):930–937. doi:10.1136/ard.2008.092734
22. Olofsson T, Englund M, Saxne T, et al. Decrease in sick leave among patients with rheumatoid arthritis in the first 12 months after start of treatment with tumour necrosis factor antagonists: a population-based controlled cohort study. Ann Rheum Dis. 2010;69(12):2131–2136. doi:10.1136/ard.2009.127852
23. Yazici Y, Shi N, John A. Utilization of biologic agents in rheumatoid arthritis in the United States: analysis of prescribing patterns in 16,752 newly diagnosed patients and patients new to biologic therapy. Bulletin NYU Hosp Joint Dis. 2008;66:77–85.
24. Pollard LC, Ibrahim F, Choy EH, Scott DL. Pain thresholds in rheumatoid arthritis: the effect of tender point counts and disease duration. J Rheumatol. 2012;39(1):28–31. doi:10.3899/jrheum.110668
25. Jeong H-J, Sohn IW, Kim D, et al. Impact of midfoot and Hindfoot involvement on functional disability in Korean patients with rheumatoid arthritis. BMC Musculoskelet Disord. 2017;18:365. doi:10.1186/s12891-017-1726-7
26. Radner H, Smolen JS, Aletaha D. Impact of comorbidity on physical function in patients with rheumatoid arthritis. Ann Rheum Dis. 2009;69(3):536–541. doi:10.1136/ard.2009.118430
27. Michaud K, Qallenstein G, Wolfe F. Treatment and non-treatment predictors of health assessment questionnaire disability progression in RA: a longitudinal study of 18,485 patients. Arthritis Care Res (Hoboken). 2011;63(3):366–372. doi:10.1002/acr.20405
28. Margaretten M, Yelin E, Imboden J, et al. Predictors of depression in a multiethnic cohort of patients with rheumatoid arthritis. Arthritis Rheum. 2009;61(11):1586–1591. doi:10.1002/art.24822
29. Intriago M, Maldonado G, Cardenas J, Rios C. Quality of life in Ecuadorian patients with established rheumatoid arthritis. Open Access Rheumatol. 2019;11:199–205. doi:10.2147/OARRR.S216975
30. Ang DC, Choi H, Kroenke K, Wolfe F. Comorbid depression is an independent risk factor for mortality in patients with rheumatoid arthritis. J Rheumatol. 2005;32(6):1013–1019.
31. Isnardi C, Capelusnik D, Schneeberger E, et al. La depresión es un determinante mayor de la capacidad funcional en pacientes con artritis reumatoidea, independientemente de la actividad de la enfermedad. Revista Argentina de Reumatología. 2019;30(2):5–10.
32. Katz PP, Yelin EH. The development of depressive symptoms among women with rheumatoid arthritis. Arthritis Rheum. 1995;38(1):49–56. doi:10.1002/art.1780380108
33. Häkkinen A, Kautiainen H, Hannonen P, Ylinen J, Arkela-Kautiainen M, Sokka T. Pain and joint mobility explain individual subdimensions of the health assessment questionnaire (HAQ) disability index in patients with rheumatoid arthritis. Ann Rheum Dis. 2005;64(1):59–63. doi:10.1136/ard.2003.019935
34. van Zeben D, Hazes JM, Breedveld FC, Zwinderman AH, Vandenbroucke JP, Breedveld FC. Factors predicting outcome of rheumatoid arthritis: results of a follow-up study. J Rheumatol. 1993;20(8):1288–1296.
35. Ríos C, Maldonado G, Paredes C, et al. Clinical and serological characteristics of Ecuadorian patients with rheumatoid arthritis. Open Access Rheumatol. 2017;9:117–122. doi:10.2147/OARRR.S130217
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
