Back to Journals » Drug Design, Development and Therapy » Volume 9
The very-rapid and the ultra-rapid virologic response to two treatment options in patients with chronic hepatitis C: an interim report of a prospective randomized comparative effectiveness study
Authors Yakoot M , Abdo A, Yousry A, Helmy S
Received 31 August 2015
Accepted for publication 7 October 2015
Published 11 November 2015 Volume 2015:9 Pages 6027—6033
DOI https://doi.org/10.2147/DDDT.S95499
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Wei Duan
Video abstract presented by Mostafa Yakoot and Alaa M Abdo.
Views: 430
Mostafa Yakoot,1,2 Alaa M Abdo,3 Ahmed Yousry,4,5 Sherine Helmy6
1Green Clinic and Research Center, 2Abbas Helmy Clinics, 3Tropical Medicine and Hepatology Department, Alexandria Faculty of Medicine, Alexandria University, 4Microbiology Department, High Institute of Public Health, Alexandria University, 5Mabarat El Asafra Labs, 6Pharco Corporation, Alexandria, Egypt
Background: We aimed in this interim report to compare two registered generic sofosbuvir products for the degree and speed of virologic response to a dual antiviral treatment protocol within the first 2 weeks of treatment.
Methods: Data collected during the period of this interim report from the first 25 patients randomized to either one of two generic sofosbuvir products (Grateziano or Gratisovir) at a daily dose of one 400 mg tablet plus a weight-based ribavirin dose were analyzed for both the degree and speed of virus load reduction at the end of 1 and 2 weeks from starting treatment.
Results: The baseline Log10 transformed virus load (Log polymerase chain reaction) showed a fairly similar marked and significant reduction in both groups by more than 4 and 5 Logs at the end of week 1 and 2 of starting treatment, respectively. The differences between the two treatment groups at both analysis points were not statistically significant (P>0.05) by repeated measures factorial analysis of variance test. The differences in proportions of patients with ultra-rapid virologic response at the end of week 1 and very-rapid virologic response at the end of week 2 in both groups were also not statistically significant (P>0.05).
Conclusion: We can conclude from this interim report that the two generic products Gratisovir and Grateziano are almost equally fast and efficacious in reducing the hepatitis C virus load in our study setting.
Keywords: chronic hepatitis C, dual antiviral therapy, ultra-rapid virologic response, very-rapid virologic response, direct acting antiviral agents
Introduction
The very fast moving process of drug discovery in the area of directly acting antiviral drugs for the treatment of chronic hepatitis C (HCV), we are witnessing now, necessitates that clinicians should find fast-track methods for clinical trials especially suitable to support fast decision-making in certain urgent situations such as the comparative effectiveness research designed to smartly decide for the choice of the most cost-effective treatment protocol for funding among many available registered alternatives in a limited-resource setting.
Although American and European guidelines for management of chronic HCV are being more frequently updated to cope with the faster development of drugs in the field, yet every community should have the chance to test and adapt these guidelines for its local peculiar situation, population characteristics, economical, logistical, and other local settings.
In a country like Egypt, where ~15% of the over 90 million population is suffering from chronic HCV and facing a lot of economic and political challenges after two revolutions within a span of 3 years, governmental efforts alone would not be enough to manage this high-burden, high-cost problem.1,2
A lot of charity-based nongovernmental organizations (NGOs) are now volunteering to share in funding treatment for poor patients. The Egyptian Cure Bank and Abbas Helmy charity establishments are just two examples.
It has been shown that the speed of virologic response to treatment is linked to the ultimate rate of sustained virologic response (SVR) and hence cure.3 The faster the response to therapy, the higher the probability for cure.3,4
Both the early and the rapid virologic response (RVR) were established as predictive indicators for cure in the response-guided therapy protocols.5
Early virologic response is defined as an undetectable serum HCV RNA or a 2 log10 or greater drop in the HCV RNA at 12 weeks of therapy.6 RVR is defined as an undetectable HCV RNA at week 4 and remains one of the strongest predictors of SVR in patients on peginterferon and ribavirin, with up to 88% of those with RVR going on to SVR.7
Now, in the new era of directly acting antiviral drugs treatment for chronic HCV, with faster actions and shorter durations of therapy, the very-rapid virologic response (vRVR) and the ultra-rapid virologic response (uRVR) to therapy can be applied as the new interim outcome measures for urgent conclusions in comparative efficacy studies. The vRVR is defined as undetectable HCV RNA levels at the end of week 2 of therapy.8
The uRVR is a new endpoint that we defined as an undetectable serum HCV RNA or a 4 log10 or greater drop in HCV RNA at the end of 1 week of therapy.
We designed this comparative effectiveness study as a quick economic model to support making an urgent choice for a cost-effective dual antiviral treatment protocol for chronic HCV in a limited-resource charity setting.
Two, generic products of sofosbuvir, Gratisovir and Grateziano, produced by Pharco and European Egyptian Pharmaceutical Industries (EEPI), Alexandria, Egypt, respectively, that had been proven to be bioequivalent to the brand Sovaldi and already registered in Egypt, were tested for comparative efficacy in the dual sofosbuvir + ribavirin protocol.
The nongovernmental organization that sponsored the study had a time limit of 1 month to take a decision for sharing and funding a charity treatment campaign. So they needed to be assured within short time about the pharmacodynamics and clinical efficacy of these generic drugs as they had been assured about the pharmacokinetics and Bioequivalence tests for these drugs done during the process of registration by regulatory authority.
We used the vRVR and the uRVR as two interim endpoints to conclude our study’s primary objective. The study is planned to be continued to compare the 4 versus 6 months treatment duration in those who achieved vRVR.
Objectives
- To compare the degree and the speed of effect of two generic sofosbuvir products, Gratisovir (Pharco) versus Grateziano (EEPI), on virus kinetics in a dual antiviral treatment protocol, each given with a generic ribavirin product (Hepaverin), in patients with chronic HCV genotype 4.
- To compare the mean Log10 reduction of virus load at week 1 and 2 after starting treatment, as well as the proportion of patients achieving uRVR and vRVR in both groups.
- To evaluate the positive and negative predictive accuracy and the utility of both vRVR and uRVR as surrogate markers for comparative efficacy or the rationalization of a truncated response-guided therapy.
- To compare the truncated 4 months versus the recommended 6 months duration of therapy in those who achieved vRVR in our final study report.
Patients and methods
Study design and setting
The study was conducted in an outpatient setting according to a randomized, open-label, comparative effectiveness study design.
Group sample sizes of 12 and 12 achieve 80% power to detect a difference of 1.2 between the null hypothesis that both group Log10 transformed means are equal with estimated group standard deviations of 1.0 and with a significance level (alpha) of 0.05 using a two-sided two-sample t-test.
Twenty-five eligible patients with documented chronic HCV, genotype 4 had been included in the study during the period of this interim report according to the following criteria:
Inclusion criteria
- Chronic HCV infection genotype 4 with polymerase chain reaction (PCR) positive test and a virus load ≥104± elevated liver enzymes.
- Males or females between 18 and 70 years old.
- Interferon naive (not previously treated with interferon-based therapy).
- Relapsers (patients with a transient virologic response to previous therapy) or nonresponders to interferon or combined therapy were eligible if they stopped the antiviral drugs at least 3 months before inclusion.
Exclusion criteria
- Pregnant females.
- Patients with other causes of hepatitis, concurrent human immunodeficiency virus (HIV) infection, or active schistosomiasis.
- Critically ill, complicated patients with severe hepatic, cardiac or kidney failure (creatinine clearance <50 mL/min), malignancy, anemia, or multiorgan failure.
The study protocol was reviewed and approved by the Green Clinic and Research Center IRB (IRB00008268), the study was conducted according to the Declaration of Helsinki. All subjects gave written informed consent before any treatment interventions were performed.
Study protocol
Consecutive patients presenting to outpatient clinics of Green CRC and Abbas Helmy Clinics starting from June 1, 2015 were assessed for eligibility through full clinical examination and the following laboratory investigations done at Mabarat El Asafra Labs.
- Detection of HCV RNA by PCR quantitative measurements by COBAS Amplicor 2.0, Roche Molecular Diagnostics, Pleasanton, CA, USA (lower limit of detection of 10 IU/mL).
- Screening test for Hepatitis B surface antigen (HBsAg), autoimmune hepatitis, anti-HIV, schistosoma Ag.
- Liver and kidney functions tests, urine analysis, stool analysis, complete blood count, blood glucose, and pregnancy test.
- Upper abdominal and liver ultrasonography was also done at the clinics.
Patients fulfilling the inclusion/exclusion criteria were included and randomly divided into two treatment groups: - Group 1 who started treatment with Gratisovir 400 mg tablets (Pharco), one tablet daily after the main meal plus weight-based dosing of Hepaverin capsules (ribavirin) 1,200 mg if body weight was ≥75 kg and 1,000 mg if body weight was <75 kg bid orally for a duration of 6 or 4 months according to further randomization for those achieving vRVR.
- Group 2 who started treatment with Grateziano 400 mg tablets (EEPI), one tablet daily after the main meal plus weight-based dosing of Hepaverin capsules (ribavirin) 1,200 mg if body weight was ≥75 kg and 1,000 mg if body weight was <75 kg bid orally for a duration of 6 or 4 months according to further randomization for those achieving vRVR.
Randomization was done using software-generated balanced block randomization technique.
All included patients were handed their assigned drugs and were asked to revisit the clinic every week for follow-up and collection of clinical and laboratory efficacy and safety data. Blood samples were weekly taken for HCV RNA quantitative PCR test, complete blood count, alanine transaminase, aspartate aminotransferase, serum creatinine as routine tests. Other nonroutine lab or imaging tests were done, according to each patient’s condition, whenever deemed necessary. Asking patients about the occurrence of any adverse event and counting the remaining tablets and capsules during each visit as a measure for compliance were also performed weekly. All patients were subjected to full psychological support and assurance as routinely done in our practice for every patient with a chronic illness in order to raise the morale and the mood of the patient that might help his immune system.
End points
The following endpoints were evaluated and compared in this interim report:
- The mean reduction of Log10 virus load in both groups after 1 and 2 weeks of starting therapy.
- Incidence of uRVR following 1 week of treatment.
- Incidence of vRVR following 2 weeks of treatment.
- Proportion of subjects with an on-treatment serious adverse event.
The following endpoints are planned to be evaluated and compared in the next final report: - Incidence of RVR following 4 weeks of treatment.
- Incidence of end of treatment response at the end of 24 versus 16 weeks course of treatment in those patients randomized after achieving vRVR. Those who will not achieve vRVR will have to complete the full 24 weeks duration of therapy as recommended in the American Association for the Study of Liver Diseases guidelines.9
- Incidence of SVR measured after 12 weeks following completion of treatment (SVR12) for each drug combination and treatment duration.
- Percent of patients with vRVR and uRVR who will achieve SVR12 in each group and treatment duration.
- The positive and negative predictive accuracy and the utility of both vRVR and uRVR as surrogate markers for comparative efficacy or as guides for the rationalization of a truncated response-guided therapy.
- Different baseline variables as well as on-study (on-treatment) measures (vRVR and uRVR) will be tested by a multiple logistic regression model for determinant factors for SVR12, relapse or null response.
Statistical analysis
Data were analyzed using the computer software package IBM SPSS Statistics for Windows, Version 21.0, IBM Corporation, Armonk, NY, USA. Comparisons of means of reduction in Log10 transformed virus load between the treatment groups were done using Student’s t-test for independent samples and repeated measures analysis of variance split-plot. Exact tests are used for comparison of proportions of categorical variables as well as testing our on-study predictors (vRVR and uRVR) for their predictive accuracy, sensitivity, specificity, and the posttest positive likelihood ratio for SVR12 at the end of the study.
Multiple logistic regression model including important baseline and on-study variables and covariates will be applied to test for determinants for SVR12, relapse or null response.
Results
Here we report the results of interim analysis of the first 25 patients who were included and completed the first 2 weeks period of treatment and follow-up. They had been randomized to either Grateziano group (13 patients) or Gratisovir group (12 patients). There have been no dropouts during the first 2-week period of the follow-up of these patients and all of them were assessable and included in our interim analysis (Figure 1).
  | Figure 1 Patient flowchart. |
The baseline characteristics of both groups were found almost comparable (Table 1).
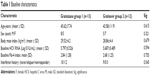  | Table 1 Baseline characteristics |
Here we report the results after week 1 and 2 treatments in both treatment groups.
Results at the end of week 1
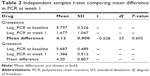
The baseline Log10 transformed virus load (Log PCR) in both groups showed markedly significant reduction at the end of week 1 of treatment by more than 4 Logs (−4.12 in Grateziano group and −4.3 in Gratisovir group). The difference between the two treatment groups was not statistically significant by both Student’s t-test and repeated measures factorial analysis of variance test (P=0.6), (Tables 2–4 and Figure 2).
  | Figure 2 Split-plot showing no significant difference in the mean reduction of Log10 PCR between the two drugs at week 1. |
The difference in proportion of patients with uRVR in both groups was also not statistically significant, 7/13 versus 6/12 (Table 4) by exact test (P=0.95).
Results at the end of week 2
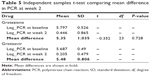
The baseline Log10 transformed virus load (Log PCR) in both groups showed markedly significant reduction at the end of week 2 of treatment by more than 5 Logs (−5.35 in Grateziano group and −5.48 in Gratisovir group). The difference between the two treatment groups was not statistically significant by both Student’s t-test and repeated measures factorial analysis of variance test (P=0.728) (Tables 5–7 and Figure 3).
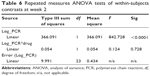  | Table 6 Repeated measures ANOVA tests of within-subjects contrasts at week 2 |
  | Figure 3 Split-plot showing no significant difference in the mean reduction of Log10 PCR between the two drugs at the end of week 2. |
The difference in the proportion of patients with vRVR in both groups was also not statistically significant, 10/13 versus 10/12 (Table 7) by exact test (P=0.863).
No serious adverse events were reported during the period of the interim report in both groups. Similar rates of treatment-emergent adverse events were reported in both groups, all were mild in severity. Headache was reported in three patients in each group (Grateziano and Gratisovir), fatigue (four and three), abdominal pain (three and two), and diarrhea (two and one), respectively. Anemia with grade 2 reduction of hemoglobin (between 8 and <10 g/dL) was reported in one patient in Grateziano group at week 2 and grade 1 reduction of hemoglobin (<lowest level of normal [LLN] – 10 g/dL) was reported in two other patients in each group. We reduced the dose of ribavirin only for the case of grade 2 reduction of hemoglobin; otherwise, no changes were made in the drug doses for all other patients.
Discussion
This study design and interim report could exemplify a fast model for comparative studies where both the speed and the degree of early response to therapy are incorporated in the comparison to support rapid provisional information needed instead of waiting for the usual lengthy efficacy studies to finish.
Early virologic response and RVR had been in use as decision support parameters for whether to stop or complete the long 48 weeks course of treatment before the new era of DDAs.
We proposed our logic that a decision can now be made more rapidly and accurately as the actions of new drugs become faster and the treatment durations got shorter. Our viewpoint is that, the decision for comparative effectiveness based on administration of the recommended dose and course of therapy and measuring the therapeutic effect gained over a suitably economic short time period could provide not only a complementary but also a more cost-effective comparative effectiveness information than the single-dose bioequivalence studies required for registration of generic products that provides only comparative pharmacokinetics data.
We acknowledge the fact that the sensitivity and specificity of both the vRVR and the uRVR as markers for efficacy have not been evaluated before, but it can be strongly extrapolated from the evidence of both early virologic response and the more accurate and rapid predictor RVR, that our suggested faster predictors could be more or, at least, as accurate as the RVR.
Conclusion
We can conclude from this interim report that the two generic products Gratisovir and Grateziano are almost equally effective and equally fast in reducing the HCV virus load in our study setting. No significant superiority was found in the mean reduction of virus load between both groups, as well as in the proportions of patients attaining uRVR or vRVR at the end of 1 or 2 weeks of therapy.
Disclosure
Sherine Helmy is working for Pharco Corporation. The authors report no other conflicts of interest in this work.
References
Sievert W, Altraif I, Razavi HA, et al. Systematic review of hepatitis C virus epidemiology in Asia, Australia and Egypt. Liver Int. 2011;31(2):61–80. | ||
Shawkat H, Yakoot M, Shawkat T, Helmy S. Efficacy and safety of a herbal mixture (Viron® tablets) in the treatment of patients with chronic hepatitis C virus infection: a prospective, randomized, open-label, proof-of-concept study. Drug Des Devel Ther. 2015;9:799–804. | ||
Yu ML, Dai CY, Huang JF, et al. A randomised study of peginterferon and ribavirin for 16 versus 24 weeks in patients with genotype 2 chronic hepatitis C. Gut. 2007;56(4):553–559. | ||
Bayram M, Koksal AR, Alkim H, et al. First week HCV RNA level under the pegylated interferon and ribavirin treatment predicts sustained virological response. Am J Ther. Epub 2015 Apr 30. | ||
Di Martino V, Richou C, Cervoni JP, et al. Response-guided peg-interferon plus ribavirin treatment duration in chronic hepatitis C: meta-analyses of randomized, controlled trials and implications for the future. Hepatology. 2011;54(3):789–800. | ||
Davis GL, Wong JB, McHutchison JG, Manns MP, Harvey J, Albrecht J. Early virologic response to treatment with peginterferon alfa-2b plus ribavirin in patients with chronic hepatitis C. Hepatology. 2003;38(3):645–652. | ||
Fried MW, Hadziyannis SJ, Shiffman ML, Messinger D, Zeuzem S. Rapid virological response is the most important predictor of sustained virological response across genotypes in patients with chronic hepatitis C virus infection. J Hepatol. 2011;55(1):69–75. | ||
Wedemeyer H, Jensen DM, Godofsky E, Mani N, Pawlotsky JM, Miller V; Definitions/Nomenclature Working Group* of the HCV DrAG (HCV Drug Development Advisory Group), under the auspices of the Forum for Collaborative HIV Research. Recommendations for standardized nomenclature and definitions of viral response in trials of hepatitis C virus investigational agents. Hepatology. 2012;56(6):2398–2403. | ||
AASLD/IDSA HCV Guidance Panel. Hepatitis C Guidance. AASLD-IDSA recommendations for testing, managing, and treating adults infected with hepatitis C virus. Hepatology. 2015;62(3):932–954. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.