Back to Journals » Drug Design, Development and Therapy » Volume 12
The role of hypoxia-inducible factor stabilizers in the treatment of anemia in patients with chronic kidney disease
Authors Zhong H, Zhou T , Li H, Zhong Z
Received 31 May 2018
Accepted for publication 6 August 2018
Published 18 September 2018 Volume 2018:12 Pages 3003—3011
DOI https://doi.org/10.2147/DDDT.S175887
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Manfred Ogris
Hongzhen Zhong,1,* Tianbiao Zhou,1,* Hongyan Li,2,* Zhiqing Zhong1,*
1Department of Nephrology, The Second Affiliated Hospital, Shantou University Medical College, Shantou, China; 2Department of Nephrology, Huadu District People’s Hospital of Guangzhou, Southern Medical University, Guangzhou, China
*These authors contributed equally to this work
Introduction: The purpose of this study was to analyze the effects of hypoxia-inducible factor (HIF) stabilizers on anemia in non-dialysis-dependent (NDD) and dialysis-dependent (DD) chronic kidney disease (CKD) patients.
Methods: Published studies were extracted from PubMed, China Biological Medicine Database (CBM), Wanfang database, and Cochrane Library on March 10, 2018, and relevant studies were pooled and included in a meta-analysis. Data on hemoglobin (Hb), ferritin, and hepcidin levels, total iron-binding capacity (TIBC), and incidence of adverse events (AEs) were extracted and pooled using Review Manager Version 5.3.
Results: Data from nine selected studies were extracted. Meta-analysis of the included studies showed that HIF stabilizers reduced ferritin and hepcidin levels and increased Hb level and TIBC in NDD-CKD patients. However, HIF stabilizers only increased TIBC, and did not affect ferritin, hepcidin, and Hb levels in DD-CKD patients. Furthermore, no notable differences in AEs and severe AEs between NDD-CKD and DD-CKD patients were detected.
Conclusion: HIF stabilizers are effective for the treatment of anemia in NDD-CKD patients and safe for short-term use.
Keywords: hypoxia-inducible factor stabilizer, anemia, chronic kidney disease, meta-analysis
Introduction
Chronic kidney disease (CKD) has become a global public health problem and results in significant morbidity and mortality.1,2 Anemia is one of the hallmarks of advanced CKD and is correlated with a lower quality of life and increased mortality.3–5 Renal anemia develops secondary to CKD, and its incidence increases with CKD progression. With the development of disease, patients inevitably develop end-stage renal disease, which often requires dialysis or kidney transplantation.6 Anemia is a common complication of CKD.7 Currently, recombinant human erythropoietin (rhEPO) is a cornerstone in the treatment of anemia associated with CKD. In the past, super-physiological doses of erythropoiesis-stimulating agents were employed to treat anemia; however, this has been associated with risk of cardiovascular events, as well as induces endothelial dysfunction.8
Hypoxia-inducible factor (HIF) is a heterodimer composed of HIF-α and HIF-β subunits.9 HIF-β is constitutively expressed, whereas HIF-α is modulated by oxygen tension via a family of HIF-prolyl hydroxylases (PHDs) regulating its degradation by the proteasome.10 During hypoxia, HIF plays an important role in survival by regulating the levels of erythropoietin (EPO), glucose transporter-1, vascular endothelial growth factor, and pyruvate dehydrogenase kinases 1 and 4.11 HIF-prolyl hydroxylase inhibitors (PHIs) are small-molecule oral agents that stabilize HIF, resulting in the activation of HIF-mediated gene expression.12 With increased HIF levels, concomitant expression of downstream molecules, such as EPO, occurs. HIF-1α induces the production of inflammatory cytokines and autoantibodies by promoting the persistence of interactions between synovial fibroblasts, T cells, and B cells. Therefore, targeting HIF-1α may be a potential therapeutic strategy for persistent disease.13 Anemia secondary to CKD is a type of chronic inflammatory anemia,14,15 and HIF stabilizers may improve the inflammatory status of CKD patients.16 Despite this theory, the therapeutic use of HIF stabilizers in the clinic has not been thoroughly analyzed. This meta-analysis was performed to assess the effects of HIF stabilizers on anemia resulting from CKD.
Materials and methods
Search strategy
The website www.ClinicalTrials.gov was queried to determine the HIF stabilizers that have been investigated in clinical trials up to March 10, 2018. The keywords roxadustat, vadadustat, daprodustat, and molidustat were entered into PubMed, China Biological Medicine Database (CBM), Wanfang database, and Cochrane Library, and relevant studies were identified without any language limitation. The references cited in the recruited articles were also checked to identify additional reports.
Inclusion and exclusion criteria
Inclusion criteria
The inclusion criteria for the studies were as follows: 1) study type: randomized controlled trials, randomized crossover studies, and prospective studies; 2) study subjects: patients who met the diagnostic criteria only for anemia of CKD, regardless of race; 3) interventions: HIF stabilizer (roxadustat, vadadustat, daprodustat, molidustat) for treatment; and 4) outcome: different HIF stabilizers were compared with placebo or traditional drugs.
Exclusion criteria
Exclusion criteria for the studies were as follows: 1) the study focused on primary anemia or anemia secondary to other causes, such as blood loss, blood diseases, and infectious diseases; 2) the clinical trial involved healthy individuals; 3) the study only described individuals treated with HIF stabilizers and did not include a reference group; and 4) the diagnostic criteria were not clear.
Outcome measures
Hemoglobin (Hb; g/L or g/dL), ferritin (ng/mL or μg/L), and hepcidin (ng/mL or μg/L) levels, total iron-binding capacity (TIBC; μg/dL or μmol/L), and adverse events (AEs) were used as outcome measures.
Data collection
According to the predetermined inclusion criteria, two observers scanned the titles and abstracts, or read the full text to screen out possible relevant literature. Discordant opinions were resolved by the other reviewers. Only randomized controlled trials, randomized crossover studies, and prospective studies that were related to HIF stabilizer treatment were included in the analysis.
Statistical analysis
Using Review Manager Version 5.3 software, data were extracted from the included literature. On the basis of the heterogeneity test results, a fixed-effects model was used when the P-value was ≥0.1; otherwise, a random-effects model was used. The results were expressed as weighted mean differences for continuous data, and additionally, 95% CIs were calculated. Heterogeneity between included studies was assessed using chi-squared test with an alpha of 0.05 indicating statistical significance. Subgroup analysis was conducted to explore the underlying causes of heterogeneity in treatment outcomes. The following factors were identified for analysis in the experimental (HIF stabilizers) and control groups: 1) a change in mean Hb levels from baseline (ΔHb), 2) a change in mean ferritin levels from baseline (Δferritin), 3) a change in mean hepcidin levels from baseline (Δhepcidin), and 4) AEs between the experimental group and control group. For all analyses, a two-tailed P-value <0.05 indicated statistical significance.
Results
Search results
In this meta-analysis, nine articles,17–25 describing 12 clinical trials, related to use of HIF stabilizers in anemia due to CKD (Table 1) were included. There were five multicenter, randomized, blinded, placebo-controlled studies17–19,21,22 and three randomized, double-blinded, placebo-controlled studies.20,23,25 Moreover, the meta-analysis included two open-label studies.20,24 These nine studies comprised 353 cases and 234 controls (Table 1).
ΔHb values between the HIF stabilizer and placebo groups
All the nine reports17–25 involved comparison of ΔHb levels between the case and placebo groups. ΔHb was statistically significant between the experimental and control groups (P<0.00001; Table 2). The P-value of the heterogeneity test was <0.00001, so a random-effects model was chosen. The pooled mean difference was 2.70 (95% CI: 1.79–3.61). A subgroup analysis was also conducted between NDD-CKD patients and DD-CKD patients to analyze the causes of heterogeneity. For the NDD-CKD patients, seven reports18–23,25 that compared the ΔHb levels between the HIF stabilizer and placebo groups were included. The P-value of the heterogeneity test was <0.00001, so a random-effects model was chosen. The pooled mean difference was 3.51 (95% CI: 2.20–4.82). The difference in the ΔHb levels was statistically significant between the HIF stabilizer and placebo groups among the NDD-CKD patients (P<0.00001; Table 2 and Figure 1A).
For the DD-CKD patients, five reports17,19–21,24 that compared the ΔHb levels between the HIF stabilizer and control groups were included. The P-value of the heterogeneity test was <0.00001, so a random-effects model was chosen. The pooled mean difference was 1.20 (95% CI: −0.12 to 2.51). The difference in the ΔHb levels between the HIF stabilizer and control groups among the DD-CKD patients was not statistically significant (P=0.07; Table 2 and Figure 1B).
ΔFerritin values between the HIF stabilizer and placebo groups
Nine reports17–25 including data from 11 trials were included in this meta-analysis for the assessment of Δferritin levels. The pooled mean difference between the case and placebo groups was −0.65 (95% CI: −1.12 to −0.18). The difference in the Δferritin levels between the experimental and control groups was statistically significant (P=0.006; Table 2). The P-value of the heterogeneity test was <0.00001, prompting us to utilize a random-effects model, and an additional subgroup analysis was conducted.
For the NDD-CKD patients, six reports18,20–23,25 were included in the meta-analysis for comparing the Δferritin levels between the HIF stabilizer and placebo groups. The P-value of the heterogeneity test was <0.00001, so a random-effects model was chosen. The pooled mean difference was −1.12 (95% CI: −1.92 to −0.32). The difference in Δferritin levels between the HIF stabilizer and placebo groups among the NDD-CKD patients was statistically significant (P=0.006; Table 2 and Figure 2A). This indicates that Δferritin levels in the HIF stabilizer group were lower than the placebo group among the NDD-CKD patients.
For the DD-CKD patients, five reports17,18,20,21,24 were included in the meta-analysis for assessing the Δferritin levels. The P-value of the heterogeneity test was 0.05, so a random-effects model was chosen. The pooled mean difference was −0.22 (95% CI: −0.65 to 0.21). The difference in Δferritin levels between the HIF stabilizer and the control group among the DD-CKD patients was not statistically significant (P=0.32; Figure 2B and Table 2).
ΔHepcidin values between the HIF stabilizer and placebo groups
Six reports18–20,22–24 including eight clinical trials were included in this meta-analysis for assessing the Δhepcidin levels between the case and placebo groups. The difference in Δhepcidin between the experimental and the control group was statistically significant (P=0.007; Table 2). The P-value of the heterogeneity test was <0.00001, so a random-effects model was chosen. The pooled mean difference was −1.65 (95% CI: −2.86 to −0.44). A subgroup analysis was conducted as well.
For the NDD-CKD patients, five reports18–20,22,23 were included in the meta-analysis for assessing the Δhepcidin levels. The P-value of the heterogeneity test was <0.00001, so a random-effects model was chosen. The pooled mean difference was −2.55 (95% CI: −4.60 to −0.49). The difference in Δhepcidin levels between the HIF stabilizer and the placebo group among the NDD-CKD patients was statistically significant (P=0.02; Figure 3A and Table 2). This indicates that the Δhepcidin levels in the HIF stabilizer group were lower than the placebo group among the NDD-CKD patients.
For the DD-CKD patients, three reports19,20,24 were included in the meta-analysis for assessing the Δhepcidin levels. The P-value of the heterogeneity test was <0.1, so a random-effects model was chosen. The pooled mean difference was −0.19 (95% CI: −0.64 to 0.26). The difference in Δhepcidin levels was not statistically significant between the two groups among the DD-CKD patients (P=0.41; Figure 3B and Table 2).
ΔTIBC between the HIF stabilizer and the placebo group
Nine reports17–25 including 11 trials were included in this meta-analysis for assessing the ΔTIBC between the case and placebo groups. The difference in ΔTIBC between the experimental and the control group was statistically significant (P<0.00001; Table 2). The P-value of the heterogeneity test was <0.00001, so a random-effects model was chosen. The pooled mean difference was 1.64 (95% CI: 0.98–2.31). In addition, a subgroup analysis comparing the NDD-CKD and DD-CKD patients was performed. For the NDD-CKD patients, six reports18,20–23,25 describing the ΔTIBC levels between the HIF stabilizer and placebo groups were included. The P-value of the heterogeneity test was <0.00001, so a random-effects model was chosen. The pooled mean difference was 2.05 (95% CI: 1.00–3.10). The difference in ΔTIBC levels between the HIF stabilizer and placebo groups among the NDD-CKD patients was statistically significant (P=0.0001; Figure 4A and Table 2). This indicates that ΔTIBC levels in the HIF stabilizer group were higher than the placebo group among the NDD-CKD patients.
For the DD-CKD patients, five reports17,18,20,21,24 were included in this meta-analysis for assessing the ΔTIBC levels between the HIF stabilizer and control groups. The P-value of the heterogeneity test was <0.00001, so a random-effects model was chosen. The pooled mean difference was 1.30 (95% CI: 0.35–2.24). The difference in ΔTIBC levels between the two groups was not statistically significant (P=0.007; Table 2 and Figure 4B). This indicates that the differences in ΔTIBC levels between the HIF stabilizer and control groups among the DD-CKD patients were not statistically significant.
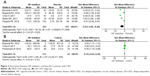
AEs between the experimental and the control groups
The most common AEs included gastrointestinal disorders, hyperkalemia, nausea, dizziness, headache, infections, and infestations. The proportion of patients with one or more AEs18–20,22,23 was similar between the experimental and control groups. The P-value of the heterogeneity test was 0.71, so a fixed-effects model was chosen. The pooled mean difference was 1.16 (95% CI: 0.81–1.67). There was no difference in AEs between the two groups (P=0.42; Figure 5 and Table 2).
  | Figure 5 Association between HIF stabilizers and rate of AEs in patients with CKD. |
Severe AEs (SAEs) included vascular access complications, femoral neck fracture, noncardiac chest pain, and dyspnea. Four reports21–24 were included in this meta-analysis for patients with SAEs. The P-value of the heterogeneity test was 0.72, so a fixed-effects model was chosen. The pooled mean difference was 1.56 (95% CI: 0.91–2.66). The SAEs between the experimental and control groups were not statistically different (P=0.11; Figure 6 and Table 2).
  | Figure 6 Association between HIF stabilizers and SAEs in patients with CKD. |
Discussion
HIF stabilizers promote erythropoiesis by stimulating endogenous EPO secretion via PHD inhibition.19,21 This meta-analysis showed that treatment with HIF stabilizers resulted in higher ΔHb levels in CKD patients. HIF stabilizers have been shown to effectively ameliorate anemia resulting from CKD. Based on the results of heterogeneity test (P<0.00001, I2=93%), we made a subanalysis of the NDD-CKD (HIF stabilizer group vs placebo group) and DD-CKD (HIF stabilizer group vs control group) subgroups. The pooled mean difference in the NDD-CKD subgroup was 3.51 (95% CI: 2.20–4.82, P<0.00001); however, the mean difference in the DD-CKD subgroup was 1.20 (95% CI: −0.12 to 2.51, P=0.07), although it was not statistically significant. Iron metabolism indexes between the NDD-CKD and DD-CKD subgroups were found to be varied. The findings of the present study were discordant with those of earlier investigations,9,17,21,24,26 showing that HIF stabilizers correct anemia in DD-CKD patients. This discrepancy in findings may be attributable to three reasons. First, due to a moderate sample size and a short treatment period, we were unable to generate a robust conclusion on the effect of HIF stabilizers in DD-CKD patients. Second, anemia secondary to CKD is generally due to endogenous EPO deficiency,20 and desensitization of the oxygen-sensing mechanism may result in abnormally low EPO production under hypoxia. Third, HIF stabilizers are essentially less effective in DD-CKD than in NDD-CKD patients. Regardless of the mechanism of normal feedback control of erythropoiesis in CKD patients, stimulation of endogenous EPO production by HIF serves as a novel method for the treatment of anemia.9
CKD anemia is a type of chronic inflammatory anemia, and hepcidin is induced in large quantities in infected and inflammatory states, resulting in intracellular iron retention and decreased plasma iron levels, eventually leading to anemia. PHIs induce erythropoiesis by improving the bioavailability and utilization of iron.27 Our meta-analysis indicated that in the NDD-CKD subgroup, the Δferritin and Δhepcidin levels in the HIF stabilizer group were lower than the placebo group. The HIF stabilizer group exhibited higher ΔTIBC compared to the placebo group. However, we did not find such changes in the DD-CKD subgroup. Our results on iron metabolism index in the DD-CKD subgroup were similar to those described by Holdstock et al.21 In their hemodialysis-dependent study, the authors hypothesized that the mean levels of hepcidin in patients who needed to receive rhEPO were suppressed before detection. Solak et al suggested that hepcidin gene suppression is not due to a direct effect of HIFs, but rather is secondary to erythropoiesis induced by EPO.28 Similarly, our analysis of the DD-CKD subgroup showed that there were no statistically significant differences in the ΔHb and Δhepcidin levels between the HIF stabilizer and control groups. However, it is also possible that we were unable to detect subtle differences due to our small sample size. Therefore, we plan to conduct further investigations to confirm the role of HIF stabilizers in hepcidin metabolism.
This study has some limitations, thereby requiring confirmation using additional studies. The chemical formulas of roxadustat, daprodustat, molidustat, and vadadustat are all different. However, no clinical trial to determine whether these have differential efficacies has been conducted to date. The sample size used in EPO measurements was relatively small, thereby preventing us from conducting meta-analysis for EPO levels. Furthermore, the present study was conducted for a short term, and thus, no long-term follow-up in terms of mortality, cardiovascular morbidity, and quality of life was performed.
Conclusion
In this meta-analysis, HIF stabilizers reduced ferritin and hepcidin levels, and increased Hb level and TIBC in NDD-CKD patients. However, HIF stabilizers only increased the TIBC, and did not affect the ferritin, hepcidin, and hemoglobin levels in DD-CKD patients. In summary, HIF stabilizers increase Hb levels and TIBC, and decrease the levels of ferritin and hepcidin in NDD-CKD patients, indicating that these are safe for short-term use in the treatment of anemia in NDD-CKD patients. However, the long-term safety and efficacy of HIF stabilizers in DD-CKD patients remain to be investigated.
Acknowledgments
This work was supported by Guangzhou Medical Key Subject Construction Project (2017-2019), Guangdong Province Science and Technology Plan Project Public Welfare Fund and Ability Construction Project (no 2014A020212519), the Natural Science Foundation of the Guangdong Province (no 2015A030310386), and Guangdong Medical Science and Technology Research Fund Project (no A2018336).
Disclosure
The authors report no conflicts of interest in this work.
References
Hu C, Yang M, Zhu X, et al. Effects of Omega-3 Fatty Acids on Markers of Inflammation in Patients With Chronic Kidney Disease: A Controversial Issue. Ther Apher Dial. 2018;22(2):124–132. | ||
Lew QLJ, Allen JC, Nguyen F, Tan NC, Jafar TH. Factors Associated with Chronic Kidney Disease and Their Clinical Utility in Primary Care Clinics in a Multi-Ethnic Southeast Asian Population. Nephron. 2018;138(3):202–213. | ||
del Vecchio L, Locatelli F. Roxadustat in the treatment of anaemia in chronic kidney disease. Expert Opin Investig Drugs. 2018;27(1):125–133. | ||
Mikhail A, Brown C, Williams JA, et al. Renal association clinical practice guideline on Anaemia of Chronic Kidney Disease. BMC Nephrol. 2017;18(1):345. | ||
Riley MV, Vess J, Dumas BP. Home Therapy to Reduce Office Visits for Patients with Chronic Kidney Disease and Anemia. Nephrol Nurs J. 2017;44(1):29–33. | ||
Groenendaal-van de Meent D, Adel MD, Noukens J, et al. Effect of Moderate Hepatic Impairment on the Pharmacokinetics and Pharmacodynamics of Roxadustat, an Oral Hypoxia-Inducible Factor Prolyl Hydroxylase Inhibitor. Clin Drug Investig. 2016;36(9):743–751. | ||
Daugirdas JT. Iron and anemia in chronic kidney disease: New treatments changing old paradigms. Hemodial Int. 2017;21(Suppl 1):S3–S5. | ||
Flamme I, Oehme F, Ellinghaus P, Jeske M, Keldenich J, Thuss U. Mimicking hypoxia to treat anemia: HIF-stabilizer BAY 85-3934 (Molidustat) stimulates erythropoietin production without hypertensive effects. PLoS One. 2014;9(11):e111838. | ||
Bernhardt WM, Wiesener MS, Scigalla P, et al. Inhibition of prolyl hydroxylases increases erythropoietin production in ESRD. J Am Soc Nephrol. 2010;21(12):2151–2156. | ||
Ariazi JL, Duffy KJ, Adams DF, et al. Discovery and Preclinical Characterization of GSK1278863 (Daprodustat), a Small Molecule Hypoxia Inducible Factor-Prolyl Hydroxylase Inhibitor for Anemia. J Pharmacol Exp Ther. 2017;363(3):336–347. | ||
Olson E, Demopoulos L, Haws TF, et al. Short-term treatment with a novel HIF-prolyl hydroxylase inhibitor (GSK1278863) failed to improve measures of performance in subjects with claudication-limited peripheral artery disease. Vasc Med. 2014;19(6):473–482. | ||
Licea Perez H, Knecht D, Evans CA. Overcoming bioanalytical challenges associated with the separation and quantitation of GSK1278863, a HIF-prolyl hydroxylase inhibitor, and its 14 stereoisomeric metabolites. J Chromatogr B Analyt Technol Biomed Life Sci. 2016;1009–1010:7–16. | ||
Hu F, Liu H, Xu L, et al. Hypoxia-inducible factor-1α perpetuates synovial fibroblast interactions with T cells and B cells in rheumatoid arthritis. Eur J Immunol. 2016;46(3):742–751. | ||
Yilmaz MI, Solak Y, Covic A, Goldsmith D, Kanbay M. Renal anemia of inflammation: the name is self-explanatory. Blood Purif. 2011;32(3):220–225. | ||
Akchurin OM, Kaskel F. Update on inflammation in chronic kidney disease. Blood Purif. 2015;39(1–3):84–92. | ||
Souma T, Nezu M, Nakano D, et al. Erythropoietin Synthesis in Renal Myofibroblasts Is Restored by Activation of Hypoxia Signaling. J Am Soc Nephrol. 2016;27(2):428–438. | ||
Akizawa T, Tsubakihara Y, Nangaku M, et al. Effects of Daprodustat, a Novel Hypoxia-Inducible Factor Prolyl Hydroxylase Inhibitor on Anemia Management in Japanese Hemodialysis Subjects. Am J Nephrol. 2017;45(2):127–135. | ||
Besarab A, Provenzano R, Hertel J, et al. Randomized placebo-controlled dose-ranging and pharmacodynamics study of roxadustat (FG-4592) to treat anemia in nondialysis-dependent chronic kidney disease (NDD-CKD) patients. Nephrol Dial Transplant. 2015;30(10):1665–1673. | ||
Brigandi RA, Johnson B, Oei C, et al. A Novel Hypoxia-Inducible Factor-Prolyl Hydroxylase Inhibitor (GSK1278863) for Anemia in CKD: A 28-Day, Phase 2A Randomized Trial. Am J Kidney Dis. 2016;67(6):861–871. | ||
Chen N, Qian J, Chen J, et al. Phase 2 studies of oral hypoxia-inducible factor prolyl hydroxylase inhibitor FG-4592 for treatment of anemia in China. Nephrol Dial Transplant. 2017;32(8):1373–1386. | ||
Holdstock L, Meadowcroft AM, Maier R, et al. Four-Week Studies of Oral Hypoxia-Inducible Factor-Prolyl Hydroxylase Inhibitor GSK1278863 for Treatment of Anemia. J Am Soc Nephrol. 2016;27(4):1234–1244. | ||
Martin ER, Smith MT, Maroni BJ, Zuraw QC, Degoma EM. Clinical Trial of Vadadustat in Patients with Anemia Secondary to Stage 3 or 4 Chronic Kidney Disease. Am J Nephrol. 2017;45(5):380–388. | ||
Pergola PE, Spinowitz BS, Hartman CS, Maroni BJ, Haase VH, Vadadustat HVH. Vadadustat, a novel oral HIF stabilizer, provides effective anemia treatment in nondialysis-dependent chronic kidney disease. Kidney Int. 2016;90(5):1115–1122. | ||
Provenzano R, Besarab A, Wright S, et al. Roxadustat (FG-4592) Versus Epoetin Alfa for Anemia in Patients Receiving Maintenance Hemodialysis: A Phase 2, Randomized, 6- to 19-Week, Open-Label, Active-Comparator, Dose-Ranging, Safety and Exploratory Efficacy Study. Am J Kidney Dis. 2016;67(6):912–924. | ||
Ren YH. Therapeutic Effect of Stable Hypoxia-Inducible Factor on Anemia of Chronic Kidney Disease and its Mechanism of Regulating Related Target Genes [doctoral dissertation]. Shanghai: Fudan University; 2013. | ||
Besarab A, Chernyavskaya E, Motylev I, et al. Roxadustat (FG-4592): Correction of Anemia in Incident Dialysis Patients. J Am Soc Nephrol. 2016;27(4):1225–1233. | ||
Hara K, Takahashi N, Wakamatsu A, Caltabiano S, Pharmacokinetics CS. Pharmacokinetics, pharmacodynamics and safety of single, oral doses of GSK1278863, a novel HIF-prolyl hydroxylase inhibitor, in healthy Japanese and Caucasian subjects. Drug Metab Pharmacokinet. 2015;30(6):410–418. | ||
Solak Y, Cetiner M, Siriopol D, et al. Novel Masters of Erythropoiesis: Hypoxia Inducible Factors and Recent Advances in Anemia of Renal Disease. Blood Purif. 2016;42(2):160–167. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.