Back to Journals » Drug Design, Development and Therapy » Volume 14
The Effect of Switching from Tenofovir Disoproxil Fumarate (TDF) to Tenofovir Alafenamide (TAF) on Liver Enzymes, Glucose, and Lipid Profile
Authors Squillace N , Ricci E , Menzaghi B , De Socio GV , Passerini S, Martinelli C, Mameli MS, Maggi P , Falasca K , Cordier L, Celesia BM , Salomoni E , Di Biagio A , Pellicanò GF , Bonfanti P
Received 29 July 2020
Accepted for publication 10 November 2020
Published 15 December 2020 Volume 2020:14 Pages 5515—5520
DOI https://doi.org/10.2147/DDDT.S274307
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Anastasios Lymperopoulos
Nicola Squillace,1 Elena Ricci,2 Barbara Menzaghi,3 Giuseppe Vittorio De Socio,4 Simone Passerini,5 Canio Martinelli,6 Maria Sabrina Mameli,7 Paolo Maggi,8 Katia Falasca,9 Laura Cordier,5 Benedetto Maurizio Celesia,10 Elena Salomoni,11 Antonio Di Biagio,12 Giovanni Francesco Pellicanò,13 Paolo Bonfanti1 On behalf of the CISAI Study Group
1Infectious Diseases Unit ASST-MONZA, San Gerardo Hospital-University of Milano-Bicocca, Monza, Italy; 2“ASIA” Foundation ONLUS, Milan, Italy; 3Unit of Infectious Diseases, ASST della Valle Olona, Busto Arsizio, Italy; 4Department of Internal Medicine 2, Infectious Diseases Unit, “Santa Maria della Misericordia” General Hospital, Perugia, Italy; 5 1st Department of Infectious Diseases, ASST Fatebenefratelli Sacco, Milan, Italy; 6Infectious Diseases Unit, Careggi Hospital, Florence, Italy; 7Unit of Infectious Diseases, Department of Medical, Surgical and Experimental Sciences, University of Sassari, Sassari, Italy; 8University of Campania “Luigi Vanvitelli”, Napoli, Italy; 9Clinic of Infectious Diseases, Department of Medicine and Science of Aging, University “G. d’Annunzio” Chieti-Pescara, Chieti, Italy; 10Unit of Infectious Diseases, University of Catania, ARNAS Garibaldi, Catania, Italy; 11Infectious Diseases Unit, Santa Maria Annunziata Hospital, Usl centro, Florence, Italy; 12Infectious Diseases, San Martino Hospital Genoa, Genoa, Italy; 13Department of Human Pathology of the Adult and the Developmental Age “G. Barresi”, Unit of Infectious Diseases, University of Messina, Messina, Italy
Correspondence: Nicola Squillace
Infectious Diseases Unit, Azienda Socio Sanitaria Territoriale di MONZA, San Gerardo Hospital-University of Milano-Bicocca, Via Pergolesi 33, Monza 20900, Italy
Tel +390392339588
Fax +390392339327
Email [email protected]
Objective: We aimed to investigate the effect of switching from tenofovir disoproxil fumarate (TDF) to tenofovir alafenamide (TAF) on the hepatic safety and metabolic profile.
Methods: Consecutive HIV patients, enrolled in the Surveillance Cohort Long-term Toxicity Antiretrovirals/Antivirals (SCOLTA) project, switching from TDF to TAF were included. Changes from baseline (T0) to 6-month follow-up (T1) were evaluated using paired t-test and signed rank test.
Results: A total of 190 patients switched from TDF to TAF and had one 6-month follow-up visit. They were 80% male, 74.2% at CDC stage A–B, 93.7% with undetectable HIV-viral load. Mean age was 46.7± 10.7 years, body mass index was 25.0± 3.9 kg/m2, median CD4 cell count was 634 cell/μL (interquartile range [IQR]=439– 900), aspartate aminotransferase (AST) was 23 (IQR=19– 30) IU/L, and alanine aminotransferase (ALT) was 24 (IQR=17– 34) IU/L. At T1, both AST (median=− 1, IQR=− 5– 2 IU/L, P=0.004) and ALT (median=− 2, IQR=− 7– 3 IU/L, P=0.0004) showed a significant decrease. Among 28 patients with ALT > 40 at baseline, reduction was significant both clinically (− 17, IQR=− 32–− 1) and statistically (P=0.0003). Total cholesterol levels (TC) increased (+13.4± 3.8 mg/dL, P=0.0006), as well as HDL-cholesterol (HDL-C) (+3.8± 1.2 mg/dL, P=0.02), LDL Cholesterol (LDL-C) (+7.6± 3.4, P=0.03) and glucose (+4.0± 1.8 mg/dL, P=0.02). D:A:D: and Framingham risk score did not change at 6 months after switch.
Conclusion: A significant reduction of liver enzymes was observed after switching from TDF to TAF, especially in subjects with initial level of ALT > 40 IU/L. Glucose, TC, HDL-C, and LDL-C increased, with no effect on cardiovascular risk scores.
Keywords: HIV, TDF, TAF, liver enzymes
Introduction
Switching from tenofovir disoproxil fumarate (TDF) to tenofovir alafenamide (TAF) showed a beneficial effect on bone and kidney toxicity.1,2 The impact on lipid profile is usually characterized by an increase in total cholesterol (TC) with a stable TC/high density lipoprotein cholesterol (HDL-C) ratio.3 Consistent findings emerged from different settings.4
Few data are available about potential hepatic toxicity of TDF. In 21,485 participants observed for 105,413 person-years,5 the D:A:D study reported an increased risk of chronic liver enzyme elevation, both with recent (<2 years) and prolonged exposure to TDF (>2 years), comparable to the risk related to didanosine and stavudine use. Data reported in a female pre-exposure prophylaxis (PREP) trial showed a higher risk of mild-to-moderate alanine transaminase (ALT) and aspartate transaminase (AST) elevation in subjects receiving TDF vs subjects in the placebo arm, especially if previously exposed to HBV virus or vaccination.6
Significant differences were also observed in patients with HBV infection: a normalization of liver enzymes was more frequently achieved in the TAF than in the TDF arm.7
In this analysis, our primary aim was to investigate the role of TAF on hepatic toxicity in a group of subjects, enrolled in the SCOLTA cohorts, who switched from emtricitabine (FTC)/TDF to FTC/TAF, maintaining the same third drug. The secondary objective was to evaluate the impact of the switch on lipid and glucose profile, and on estimated cardiovascular risk.
Methods
The SCOLTA Project (Surveillance Cohort Long-Term Toxicity of Antiretrovirals) is a prospective, observational, multicenter study created to assess the incidence of adverse events (AE) in patients receiving new antiretroviral drugs in clinical practice.
The SCOLTA Project is an on-line pharmacovigilance program currently involving 21 Italian infectious disease departments, where grade III and IV AEs (according to DAIDS table8) are recorded. All patients starting one of the cohort drugs are asked to participate in the study, after signing a written informed consent form.
Ethics
The study protocol was approved by the local ethics committee of the coordinating center at Hospital “L.Sacco” – University of Milan on September 18, 2002. A new protocol amendment was submitted and approved on June 13, 2013 by the same ethics committee. This last version was approved by the local ethics committee of each group and written consent was obtained from all participants. The study was conducted in accordance with the Declaration of Helsinki.
Data are available on reasonable request addressed to the corresponding author.
Patients
Patients undergo follow-up at 6-month intervals and AEs are notified when they are clinically observed. Complete data collection and follow-up procedures for the cohorts are described elsewhere.9
In this analysis, we included patients enrolled in three cohorts: darunavir (DRV)/cobicistat (COBI), elvitegravir (EVG)/COBI, and dolutegravir (DTG), who entered the study with TDF/FTC backbone and switched to TAF/FTC. After the switch, patients naïve at study entry were defined as on “second line antiretroviral therapy (ART)”, to distinguish them from subjects who were ART-experienced at study entry. We selected subjects with AST and ALT both at switch (T0) and at 6-month follow-up (T1). We also calculated the 5-year risk for coronary heart disease (CHD), using the D:A:D equation10 and the Framingham risk score (FRS) equation,11 keeping age and smoking habits at T0 both in the T0 and T1 score.
Statistical Analysis
Categorical and discrete variables were described as frequency and percentage (%). Continuous variables were described using mean and standard deviation (SD) if normally distributed, and median and interquartile range (IQR) if not normally distributed. At univariate analysis, groups were compared using chi-square for categorical variables and analysis of variance for continuous variables, or via non-parametric tests for non-normally distributed continuous variables. Repeated measures were analyzed as change from baseline and described as means (±standard error, SE) if normally distributed or medians (IQR) if not normally distributed; to evaluate if change from baseline was significantly different from zero, we used the paired t-test or the signed rank test, as appropriate.
Results
One hundred and ninety patients (mean age=44.8 years, range=19–74) were selected for this analysis. Forty-two individuals who switched from TDF to TAF and had not yet reached T1 were excluded: no statistically significant difference was observed between these groups, in terms of sex, age, ART experience, third drug, BMI, and baseline AST and ALT, although women were more frequent in the group without follow-up visit at the time of this analysis (33.3% vs 20.0%, P=0.06).
Among selected individuals, most were males (80.0%) and 50 (26.3%) were on their second-line ART. Median time from enrollment to switch was 23 months (IQR=14–31). The main characteristics are shown in Table 1. At baseline, we had complete data for calculating CHD risk for 70 (D:A:D:) and 77 (FRS) patients.
 |
Table 1 Patients Switching from Tenofovir Disoproxil Fumarate (TDF) to Tenofovir Alafenamide (TAF), with 6-Month Follow-Up |
After 6 months of follow-up (Table 2), we observed a significant decrease both in AST (median=−1, IQR=−5–2 IU/L, P=0.004) and in ALT (−2, IQR=−7–3 IU/L, P=0.0004) levels. Median ALT decrease was significant in patients with baseline values >40 IU/L (P=0.0003): 15 (53.6%) had ALT≤40 at T1, six (21.4%) did not normalize but experienced a decline, and seven (25.0%) showed unchanged or increased values.
 |
Table 2 Liver Transaminase Changes from TDF-TAF Switch to 6-Month Follow-Up |
Statistically significant AST and ALT variations were found in patients negative both for HCV-Ab and HBsAg (−1, IQR=−5–2, P=0.03; −2, IQR=−7–2, P=0.003 respectively), whereas an ALT decrease was of borderline significance in individuals with positive HCV-Ab and/or Hbs-Ag (Table 2). During the observation period, no patient with active HCV infection underwent treatment with direct-acting antivirals.
As regards metabolic variables and weight variation at T1 (Table 3), we observed that estimated glomerular filtration rate (eGFR) slightly increased (+3.6±1.0 mL/min, P=0.0008), whereas BMI value or weight did not significantly change. TC increased (+13.4±3.8 mg/dL, P=0.0006), as well as HDL-C (+3.8±1.2 mg/dL, P=0.02) and LDL-C (+7.6±3.4 mg/dL, P=0.03). As a result, mean TC/HDL ratio showed a negligible variation.
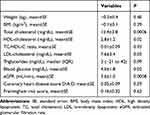 |
Table 3 Changes in BMI and Metabolic Variables from TDF-TAF Switch to 6-Month Follow-Up |
Glucose significantly increased (+4.0±1.8 mg/dL, P=0.02), in particular in patients on EVG/COBI as the third drug (+5±1.8 mg/dL, P=0.02).
As regards CHD risk, mean variations are reported in Table 3. According to D:A:D: score, five patients switched to a higher risk class (one low to intermediate risk, three from intermediate to high risk, one high to very high risk) and four switched to a lower risk class. According to Framingham risk score, four migrated to a higher risk class, vs eight to a lower risk class.
In the 6 months after switching to TAF, eight (4.2%) patients interrupted the treatment: two for adverse events (one central nervous system symptoms, one TC increase); one patient died for aplastic anemia; two switched to a one-pill regimen; one had a therapeutic failure; one patient moved to another center; and one patients switched because the current regimen had interactions with treatment for benign prostatic hyperplasia.
Discussion
In this sample of patients switching from FTC/TDF to FTC/TAF we found a significant decrease of liver enzymes levels (both AST and ALT). Since the most marked decline was observed in patients with initial ALT level >40 IU/L, this variation may be clinically relevant.
TDF liver toxicity was demonstrated in animal models. It was reported as mild/moderate and consisted in collagen deposition and cytomegaly, apparently reversible after TDF withdrawal.12,13 Increased oxidative stress and lipid peroxidation were proposed as possible mechanisms to explain the observed liver abnormalities.
Studies on TDF/FTC used for PREP focused on bone and kidney toxicity and usually did not report liver adverse events.14 A study on pre-exposure prophylaxis (PREP) in African women demonstrated an increase in AST/ALT levels in patients randomized to the TDF/FTC arm vs placebo, especially in patients with previous exposure to HBV.6 A beneficial effect in HBV infection could be explained by the higher concentration of TAF vs TDF in hepatocytes, demonstrated in animal models.15
Studies on switching from TDF to TAF showed that HBV-infected patients had a higher probability to normalize ALT level in the TAF than in the TDF arm.7
However, in our cohort HBV infection is not associated with a higher decrease of AST and ALT levels. This lack of evidence could be explained by the limited number of HBV positive patients in our cohort. Besides, liver transaminase variations were similar in HCV-Ab/HBs-Ag negative and HCV-AB and/or HBs-Ag positive patients, suggesting a potential mechanism not linked to viral co-infections. Liver toxicity is associated with mitochondrial dysfunction,16,17 and recent observations demonstrated a lower mitochondrial toxicity of TAF vs TDF.18,19 Thus, the better liver toxicity profile of TAF might be linked to a direct drug effect on liver, due to its lower mitochondrial toxicity. An alternative explanation could be the lower impact on progression of liver steatosis.
Glucose levels increased significantly in our cohort, in particular in patients on EVG. Although EVG was associated with alteration of adipokines and cytokines and glucose transporter GLUT4,20 no increase in insulin resistance was found in healthy male volunteers, exposed to a short-term treatment of 14 days with EVG/COBI/FTC/TAF.21 Nevertheless, our results could be justified by a longer exposure to EVG and TAF in our sample. The effect of EVG on glucose was not correlated with weight gain, because no significant difference in BMI was observed in patients on EVG vs patients on DTG or DRV. In the light of these results, EVG associated with TAF might have a direct effect on glucose metabolism.
Most patients in our sample were on an Integrase Strand Transfer Inhibitors (INSTI) containing regimen. INSTI class was recently associated with weight gain, especially in association with TAF, in naïve patients.22 We did not observe a significant change in BMI, probably because weight gain usually happens during the first year of INSTI treatment,23 and most patients in our sample switched to TAF after 12 months of INSTI-based treatment.
Consistent with findings from randomized controlled trials,1–3 we confirmed in a “real life setting” that eGFR showed a slight improvement. Moreover, we found that total cholesterol and LDL-C increased, with no significant change in TC/HDL ratio.
As regards cardiovascular risk, in a previous retrospective study, conducted on 273 patients introducing TDF,24 a significant modification of D:A:D score was observed after 3 months from switch. Similarly, in a randomized controlled trial,25 311 patients switched from ABC+3TC to TDF+FTC, with a significant reduction of Framingham risk both at 12 and 48 weeks. In our sample, changes in blood lipids did not determine a significant variation in cardiovascular risk scores after 6 months from switch.
Conclusions
Our findings suggest that switching from TDF to TAF has a beneficial effect on liver function. A significant increase of glucose, TC, HDL-C, and LDL-C did not result in significant change of cardiovascular risk estimations, as measured by D:A:D: and Framingham risk scores.
Acknowledgments
We thank all the members of Coordinamento Italiano Studio Allergie e Infezione da HIV (CISAI).
Coordinators: Paolo Bonfanti (Monza), Antonio Di Biagio (Genova).
Data Management: Elena Ricci (Monza).
Participating centers: G. Chichino, C Bolla, A. Parisini, E. Sarchi (Alessandria); A. Saracino, D. Bavaro, G. Angarano (Bari); L. Calza (Bologna); B. Menzaghi, M. Farinazzo (Busto Arsizio); G. Angioni (Cagliari); P. Maggi (Caserta); M. Gussio, B. M. Celesia (Catania); K. Falasca (Chieti); A. Mastroianni, G. Guadagnino (Cosenza); F. Vichi, E. Salomoni (Firenze); C. Martinelli (Firenze); S. Ferrara (Foggia); A. Di Biagio, L. Taramasso, M. Berruti, M. Bassetti (Genova); C. Molteni, S. Piconi (Lecco); G. F. Pellicanò, G Nunnari (Messina); L. Valsecchi, L. Cordier, S. Parisini, G. Rizzardini (Milano); S. Rusconi, F. Conti (Milano); A. Bandera, A. Gori (Milano); D. Motta, M. Puoti (Milano); N. Squillace, P. Bonfanti (Monza); S. Martini (Napoli); O. Bargiacchi, P. L. Garavelli (Novara); A. Cascio, M. Trizzino (Palermo); R. Gulminetti (Pavia); G. V. De Socio, M. Nofri, D. Francisci (Perugia); D. Cibelli, G. Parruti (Pescara); C. Dentone, G. Cenderello (Sanremo); G. Madeddu, M. S. Mameli (Sassari); G. Orofino, M. Guastavigna (Torino).
The abstract of this paper was presented at “HIV Drug Therapy” October 28–31, 2018, Glasgow, Scotland, UK as an abstract presentation with preliminary findings. The poster’s abstract was published in “Poster Abstracts” in the conference’s website (http://hivglasgow.org/wpcontent/uploads/2018/11/P218.pdf).
Disclosure
Nicola Squillace reports personal fees from ViiV Healthcare and grants from Gilead science, outside the submitted work. Benedetto Maurizio Celesia reports personal fees and non-financial support from MSD, Janssen cilag grants, personal fees, non-financial support, consultancy from Gilead sciences, grants, personal fees, non-financial support, consultancy from ViiV healthcare, outside the submitted work. Paolo Bonfanti reports personal fees from ViiV, Gilead, Jannsen, and Merck, outside the submitted work. The authors report no other potential conflicts of interest for this work.
References
1. Mills A, Crofoot G, McDonald C, et al. Tenofovir alafenamide versus tenofovir disoproxil fumarate in the first protease inhibitor-based single-tablet regimen for initial HIV-1 therapy: a randomized phase 2 study. J Acquir Immune Defic Syndr. 2015;69(4):439–445. doi:10.1097/QAI.0000000000000618
2. Raffi F, Orkin C, Clarke A, et al. Brief report: long-term (96-week) efficacy and safety after switching from tenofovir disoproxil fumarate to tenofovir alafenamide in HIV-infected, virologically suppressed adults. J Acquir Immune Defic Syndr. 2017;75(2):226–231. doi:10.1097/QAI.0000000000001344
3. Wohl D, Oka S, Clumeck N, et al. Brief report: a randomized, double-blind comparison of tenofovir alafenamide versus tenofovir disoproxil fumarate, each coformulated with elvitegravir, cobicistat, and emtricitabine for initial HIV-1 treatment: week 96 results. J Acquir Immune Defic Syndr. 2016;72(1):58–64. doi:10.1097/QAI.0000000000000940
4. Kauppinen KJ, Kivela P, Sutinen J. Switching from tenofovir disoproxil fumarate to tenofovir alafenamide significantly worsens the lipid profile in a real-world setting. AIDS Patient Care STDS. 2019;33(12):500–506. doi:10.1089/apc.2019.0236
5. Kovari H, Sabin CA, Ledergerber B, et al. Antiretroviral drugs and risk of chronic alanine aminotransferase elevation in human immunodeficiency virus (HIV)-monoinfected persons: the data collection on adverse events of anti-HIV drugs study. Open Forum Infect Dis. 2016;3(1):ofw009.
6. Mandala J, Nanda K, Wang M, et al. Liver and renal safety of tenofovir disoproxil fumarate in combination with emtricitabine among African women in a pre-exposure prophylaxis trial. BMC Pharmacol Toxicol. 2014;15:77. doi:10.1186/2050-6511-15-77
7. Agarwal K, Brunetto M, Seto WK, et al. 96weeks treatment of tenofovir alafenamide vs. tenofovir disoproxil fumarate for hepatitis B virus infection. J Hepatol. 2018;68(4):672–681. doi:10.1016/j.jhep.2017.11.039
8. Division of AIDS. Division of AIDS (DAIDS) Table for Grading the Severity of Adult and Pediatric Adverse Events. Bethesda, MD: National Institute of Allergy and Infectious Diseases; 2017. Available from: https://rsc.niaid.nih.gov/sites/default/files/daidsgradingcorrectedv21.pdf. Accessed December 9, 2020.http://rcc.tech-res-intl.com/tox_tables.htm
9. Bonfanti P, Martinelli C, Ricci E, et al. An Italian approach to postmarketing monitoring: preliminary results from the SCOLTA (Surveillance Cohort Long-Term Toxicity Antiretrovirals) project on the safety of lopinavir/ritonavir. J Acquir Immune Defic Syndr. 2005;39(3):317–320. doi:10.1097/01.qai.0000164248.56722.3c
10. Friis-Moller N, Thiebaut R, Reiss P, et al. Predicting the risk of cardiovascular disease in HIV-infected patients: the data collection on adverse effects of anti-HIV drugs study. Eur J Cardiovasc Prev Rehabil. 2010;17(5):491–501. doi:10.1097/HJR.0b013e328336a150
11. D’Agostino RB, Grundy S, Sullivan LM, Wilson P; Group CHDRP. Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. JAMA. 2001;286(2):180–187. doi:10.1001/jama.286.2.180
12. Adaramoye OA, Adewumi OM, Adesanoye OA, Faokunla OO, Farombi EO. Effect of tenofovir, an antiretroviral drug, on hepatic and renal functional indices of Wistar rats: protective role of vitamin E. J Basic Clin Physiol Pharmacol. 2012;23(2):69–75. doi:10.1515/jbcpp.2011.0042
13. Peter AI, Naidu EC, Akang E, et al. Investigating organ toxicity profile of tenofovir and tenofovir nanoparticle on the liver and kidney: experimental animal study. Toxicol Res. 2018;34(3):221–229. doi:10.5487/TR.2018.34.3.221
14. Fonner VA, Dalglish SL, Kennedy CE, et al. Effectiveness and safety of oral HIV preexposure prophylaxis for all populations. AIDS. 2016;30(12):1973–1983. doi:10.1097/QAD.0000000000001145
15. Murakami E, Wang T, Park Y, et al. Implications of efficient hepatic delivery by tenofovir alafenamide (GS-7340) for hepatitis B virus therapy. Antimicrob Agents Chemother. 2015;59(6):3563–3569. doi:10.1128/AAC.00128-15
16. Lee J, Park JS, Roh YS. Molecular insights into the role of mitochondria in non-alcoholic fatty liver disease. Arch Pharm Res. 2019;42(11):935–946.
17. Hua H, Zhang Z, Qian Y, et al. Inhibition of the mitochondrial complex-1 protects against carbon tetrachloride-induced acute liver injury. Biomed Pharmacother. 2019;115:108948. doi:10.1016/j.biopha.2019.108948
18. Ritou EKT. In vitro modelling of the impact of TAF on cellular bioenergetics in immune cells and hepatocytes. 21st International workshop on co-morbidities and adverse drug reactions in HIV; 5–6 November 2019, 2019; Basel, Switzerland. Antivir Ther. 2019;24(S1):A100.
19. Li M, Zhou L, Dorsey HG, et al. Tenofovir alafenamide does not inhibit mitochondrial function and cholesterol biosynthesis in human T lymphoblastoid cell line. Antiviral Res. 2020;183:104948. doi:10.1016/j.antiviral.2020.104948
20. Moure R, Domingo P, Gallego-Escuredo JM, et al. Impact of elvitegravir on human adipocytes: alterations in differentiation, gene expression and release of adipokines and cytokines. Antiviral Res. 2016;132:59–65. doi:10.1016/j.antiviral.2016.05.013
21. Spinner CD, Schulz S, Bauer U, et al. Effects of antiretroviral combination therapies F/TAF, E/C/F/TAF and R/F/TAF on insulin resistance in healthy volunteers: the TAF-IR study. Antivir Ther. 2018;23(7):629–632. doi:10.3851/IMP3271
22. Sax PE, Erlandson KM, Lake JE, et al. Weight gain following initiation of antiretroviral therapy: risk factors in randomized comparative clinical trials. Clin Infect Dis. 2020;71:1379–1389.
23. Taramasso L, Bonfanti P, Ricci E, et al. Factors associated with weight gain in people treated with dolutegravir. Open Forum Infect Dis. 2020;7(6):ofaa195. doi:10.1093/ofid/ofaa195
24. Gagliardini R, Fabbiani M, Colafigli M, et al. Lipid-lowering effect and changes in estimated cardiovascular risk after switching to a tenofovir-containing regimen for the treatment of HIV-infected patients. J Chemother. 2017;29(5):299–307. doi:10.1080/1120009X.2016.1269040
25. Campo R, DeJesus E, Bredeek UF, et al. SWIFT: prospective 48-week study to evaluate efficacy and safety of switching to emtricitabine/tenofovir from lamivudine/abacavir in virologically suppressed HIV-1 infected patients on a boosted protease inhibitor containing antiretroviral regimen. Clin Infect Dis. 2013;56(11):1637–1645. doi:10.1093/cid/cis1203
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
