Back to Journals » Clinical Interventions in Aging » Volume 11
Switching to low-dose oral prolonged-release oxycodone/naloxone from WHO-Step I drugs in elderly patients with chronic pain at high risk of early opioid discontinuation
Authors Lazzari M, Marcassa C, Natoli S , Carpenedo R, Caldarulo C, Silvi M, Dauri M
Received 4 February 2016
Accepted for publication 10 March 2016
Published 13 May 2016 Volume 2016:11 Pages 641—649
DOI https://doi.org/10.2147/CIA.S105821
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Richard Walker
Marzia Lazzari,1 Claudio Marcassa,2 Silvia Natoli,1 Roberta Carpenedo,1 Clarissa Caldarulo,1 Maria B Silvi,1 Mario Dauri1
1Department of Emergency and Critical Care Medicine, Pain Medicine and Anaesthesiology, Tor Vergata Polyclinic, University of Rome, Rome, 2Cardiology Division, Fondazione Maugeri IRCCS Veruno, Novara, Italy
Purpose: Chronic pain has a high prevalence in the aging population. Strong opioids also should be considered in older people for the treatment of moderate to severe pain or for pain that impairs functioning and the quality of life. This study aimed to assess the efficacy and safety of the direct switch to low-dose strong opioids (World Health Organization-Step III drugs) in elderly, opioid-naive patients.
Patients and methods: This was a single-center, retrospective, observational study in opioid-naive patients aged ≥75 years, with moderate to severe chronic pain (>6-month duration) and constipation, who initiated treatment with prolonged-release oxycodone/naloxone (OXN-PR). Patients were re-evaluated after 15, 30, and 60 days (T60, final observation). Response to treatment was defined as an improvement in pain of ≥30% after 30 days of therapy without worsening of constipation.
Results: One-hundred and eighty-six patients (mean ± SD age 80.7±4.7 years; 64.5% women) with severe chronic pain (mean average pain intensity 7.1±1.0 on the 11-point numerical rating scale) and constipation (mean Bowel Function Index 64.1±24.4; 89.2% of patients on laxatives) were initiated treatment with OXN-PR (mean daily dose 11.3±3.5 mg). OXN-PR reduced pain intensity rapidly and was well tolerated; 63.4% of patients responded to treatment with OXN-PR. At T60 (mean daily OXN-PR dose, 21.5±9.7 mg), the pain intensity was reduced by 66.7%. In addition, bowel function improved (mean decrease of Bowel Function Index from baseline to T60, -28.2, P<0.0001) and the use of laxatives decreased. Already after 15 days and throughout treatment, ~70% of patients perceived their status as much/extremely improved. Only 1.6% of patients discontinued treatment due to adverse events.
Conclusion: Low-dose OXN-PR in elderly patients naive to opioids proved to be an effective option for the treatment of moderate to severe chronic pain. Large-scale trials are needed to improve clinical guidance in the assessment and treatment of pain in older people.
Keywords: chronic pain, elderly, naloxone, opioid, oxycodone
Introduction
Chronic pain affects ~20% of the general population in Europe and its incidence significantly increases after the age of 60.1 According to current estimates, the prevalence of chronic pain in older people living in the community ranges from 25% to 76%, and reaches 83% to 93% among older people living in residential care.2 In older adults, chronic pain is predominantly nociceptive and caused by musculoskeletal disease; pain of neuropathic or mixed nature is also common.3 Persistent pain has a negative impact on the quality of life, is a cause of depression and morbidity, and can contribute to disability progression and to a decrease in daily functioning.1,4
According to guidelines for the pharmacological management of chronic pain in older patients, acetaminophen (paracetamol) should be considered as initial pharmacotherapy in the treatment of persistent pain, particularly musculoskeletal pain, while nonsteroidal anti-inflammatory drugs (NSAIDs) may be considered rarely and with caution in highly selected patients (ie, those without gastrointestinal, renal, and cardiovascular comorbidities, and not at risk for drug–drug and drug–disease interactions).5 Moreover, for older adults, an NSAID or a cyclooxygenase-2 selective inhibitor should be co-prescribed with a proton pump inhibitor.5 Opioid analgesics should be considered for all patients with moderate to severe pain, or for pain that impairs functioning and the quality of life.2,3,5,6 Opioid treatment should be initiated at the lowest possible dose, slowly up-titrated, and carefully tailored based on response and tolerability.2,3,5
Despite these recommendations, real-life management of chronic pain in geriatric patients is often inappropriate. Typical features suggesting treatment inappropriateness include the predominance of NSAIDs among analgesics prescribed and the prolonged treatment with acetaminophen and/or NSAIDs before switching to opioids when pain control is inadequate.5,7,8 Major barriers to the use of opioids in older patients are the fear of opioid-related adverse events (AEs), concerns about the development of drug dependence, and the uncertainty about the role of opioids in cognitive impairment.2,9 The most frequently reported opioid-induced AEs are constipation, sedation, drowsiness/dizziness (which may increase the risk of fall in the elderly population), respiratory depression, nausea/vomiting, and delirium.3,10,11 Unlike most AEs that resolve with prolonged opioid use due to the development of tolerance, constipation is persistent and is a frequent cause of dose reduction or treatment discontinuation.12–15 In elderly patients, constipation can be an even more relevant problem, as the predisposition to bowel dysfunction increases with age.2,5
Current guidelines recommend the use of laxatives for all older people during opioid therapy.2 The combination of oxycodone (a strong opioid) with naloxone (an opioid-receptor antagonist) was developed to prevent or reduce opioid-induced constipation.16 Oral prolonged-release oxycodone/naloxone combination (OXN-PR) was shown in a number of controlled, randomized trials to provide effective analgesia to patients with severe chronic pain and to significantly reduce the incidence of opioid-induced constipation, with an improvement in compliance and quality of life.17,18
The evidence from recent observational retrospective and prospective studies suggests that OXN-PR is also effective in older subjects.19–21 In addition, the evidence shows that these patients can be switched safely from acetaminophen and/or NSAIDs (Step I analgesics according to the analgesic ladder of the World Health Organization [WHO])22 to OXN-PR (a strong opioid, or a Step III analgesic according to the WHO ladder) with no need to try first a weak opioid (a Step II analgesic).21
The primary objective of this retrospective observational study was to evaluate the efficacy and safety of OXN-PR in elderly patients (≥75 years old) affected by chronic pain and constipation, who had never been treated before with opioids.
Patients and methods
Study design and patients
This single-center, retrospective, observational study was conducted at the Tor Vergata Polyclinic Pain Unit in Rome, Italy, a reference center for the treatment of pain in Italy. The study was approved by the Tor Vergata Polyclinic Review Board (registry number 27.16). As this was a retrospective study, patient consent was neither obtained nor required by the Tor Vergata Polyclinic Review Board. Data collected from the clinical records of consecutive patients referred to the center from February 2011 to December 2012 were evaluated. Over this time, all patients reporting chronic pain (>6-month duration) of moderate to severe intensity (assessed on a verbally administered 11-point numerical rating scale [NRS] where 0 indicated no pain, 1–3 mild pain, 4–6 moderate pain, and 7–10 severe pain) and symptoms of constipation were prescribed OXN-PR (Targin®; Mundipharma Pharmaceuticals Srl, Milano, Italy), unless contraindications were present.
The criteria for inclusion in the analysis were as follows: age ≥75 years; presence of chronic pain of cancer or noncancer etiology; opioid-naive; and complaining of constipation judged as clinically significant (ie, less than three complete spontaneous bowel movements per week, with difficulty passing stools despite appropriate dietary change and/or laxatives), and thus putting the subjects at high risk of discontinuing opioid treatment prematurely. Patients with a history of alcohol and/or drug abuse or with cognitive impairment not allowing an appropriate pain assessment were excluded. After the new OXN-PR prescription, patients were followed up for 60 days. Study visits were performed at baseline (T0) and at 15 days, 30 days, and 60 days (respectively, T15, T30, and T60 visits).
Treatments
Patients were prescribed OXN-PR for pain control and were instructed to interrupt other analgesics. They were allowed to continue adjunctive therapies (antidepressants, gabapentin, pregabalin, steroids) and laxatives, if present, with no further dose increase. Drugs for the treatment of concomitant conditions were continued at the usual dosages. The OXN-PR starting dose (5/2.5 mg or 10/5 mg) was determined by the treating pain specialist and was administered twice a day. If pain was not satisfactorily controlled, acetaminophen 500–1,000 mg was allowed as rescue therapy. In case of rescue therapy administrations more than twice in a day, patients were instructed to anticipate their scheduled follow-up visit and the OXN-PR dose was increased accordingly by the pain specialist. In the following visits, OXN-PR could be further titrated by the physician, according to patient’s needs. The maximum OXN-PR dose allowed in this study was 40/20 mg twice daily (the currently approved maximum daily dose of OXN-PR after titration is 160 mg of oxycodone and 80 mg of naloxone).23
Assessments
All assessments were performed by specialized clinicians trained in the management of pain, and data were recorded in a designed form. Demographic characteristics and medical history were recorded at baseline. Efficacy variables were assessed at each time point and included the average pain intensity (API) in the last 24 hours assessed on a verbally administered 11-point NRS, daily dosage of OXN-PR required, the need for rescue acetaminophen (number of doses per day), and patients’ perception of treatment effectiveness evaluated by a Patient Global Impression of Change (PGIC) seven-item response scale. Laxative use was also assessed at T0 and T60.
Bowel function in the last 7 days was also assessed, using the Bowel Function Index (BFI) at each time point and based on the use of laxatives (at T0 and T60). BFI is a measure of general bowel function recently validated as a reproducible tool that detects clinically meaningful changes in opioid-induced constipation, with scores ranging from 0 (no symptoms) to 100 (most severe symptoms).24 In patients with chronic pain, normal bowel function is defined as a BFI value <29, and a change in BFI ≥12 points represent a clinically meaningful change in constipation severity.
Safety evaluations were also performed at each time point, by recording drug-related AEs, defined as any new event that occurred or worsened in intensity and/or frequency after the first intake of OXN-PR. The potential correlation between the AE and OXN-PR was judged by the pain physician. Symptom intensity was graded as mild (not requiring any specific treatment, or OXN-PR dose reduction), moderate (not allowing any OXN-PR dose increase, or requiring OXN-PR dose reduction), or severe (requiring OXN-PR discontinuation).
Statistical analysis
The primary efficacy measure of the study – the response rate to OXN-PR at T30 – was a composite of API reduction ≥30% from baseline to T30 without worsening of constipation (ie, increase of BFI ≤12 from baseline to T30). Secondary efficacy measures included the absolute and percent changes in NRS, BFI, number of rescue analgesic and laxative doses from T0 to T60, and the proportions of patients reporting satisfaction with pain relief throughout the observation.
To determine the size of the sample to be included in the analysis, based on a Fleming’s design with 80% power and 1% Type 1 error, the null hypothesis was set at a response rate of at most 65%, ie, less than two-thirds of the considered population; the alternative hypothesis was set at a response rate of at least 76% (more than three-quarters of the population). To allow for dropouts and incomplete data (≅10%), the number of patients to be included in the retrospective sample was 186.
All data were analyzed by descriptive statistics. Mean (±SD) values were calculated and statistical comparisons over time were performed. Change in continuous variables over time was evaluated by the analysis of variance test, with a post-hoc Bonferroni’s correction to adjust for multiple comparisons. Statistical analysis was performed using STATISTICA software, version 8.0 (StatSoft Inc., Tulsa, OK, USA).
Results
Study population and interventions
Demographic and baseline (T0) characteristics of the study population are summarized in Table 1. Overall, 186 patients (64.5% women) were included in this retrospective analysis. Median age was 80 years (range: 75–95 years). Active cancer was the cause of pain in 17 patients (9.1%) only. Mean API was 7.1±1.0 (range: 4–10) and API was severe (NRS ≥7) in the majority of patients (69.4%). At baseline, half of our patients (49.5%) were taking around-the-clock acetaminophen or NSAIDs (including selective inhibitors of cyclooxygenase-2 [coxibs]), and one-fourth (25.3%) were taking adjuvants with or without acetaminophen or NSAIDs. One-third of the patients (33.9%) were not receiving any around-the-clock analgesic pharmacotherapy and were using instead over-the-counter, on-demand acetaminophen and/or NSAIDs (Table 1). Nearly two-thirds (62.6%) of the patients taking around-the-clock analgesics and/or adjuvants needed rescue acetaminophen (on average, two daily administrations). Despite the fact that most patients (89.2%) were using laxatives (on average, 4.7±1.7 administrations per week), the mean BFI value at baseline was >60, indicating severe bowel dysfunction.
The treatment with OXN-PR was started at a low dose, with a mean daily dose of 11.3±3.5 mg. In the following weeks, the mean daily dose of OXN-PR was increased slightly, reaching 21.5±9.7 mg at T60. Fourteen (87.5%) out of 16 patients on glucocorticoids at baseline, in the absence of a clear indication, discontinued steroids early after OXN-PR. Twenty-nine out of 31 subjects on anticonvulsants at baseline completed the 60-day observation: five of them (17.2%) stopped or decreased the daily anticonvulsant dosage, six (20.7%) slightly increased it, and the remaining 18 patients (62.0%) continued these adjuvants at the same baseline dosages.
Efficacy
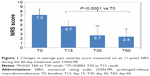
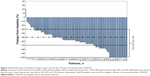
The switch to low-dose OXN-PR was associated with statistically significant improvements from baseline in pain intensity (mean difference in API scores from baseline to T15, T30, and T60, respectively, −2.5, −4.5, and −4.8; P<0.0001 for all comparisons vs baseline) (Figure 1). At T60, the mean API decreased by 66.7% compared to that at the beginning of treatment. Individual changes in pain intensity scores from baseline to T30 are shown as a waterfall graph in Figure 2. At T30, 170 (91.4%) patients had achieved a clinically relevant ≥30% API reduction from baseline; the proportion of patients who achieved an API improvement of ≥30% from baseline at T15 was 54.3% (P<0.001 vs T30) and 92.5% at T60 (not statistically significant vs T30). Although at T30, 16 patients (8.6%) did not achieve an API improvement ≥30% from baseline, only three patients (1.6%) were still complaining of severe pain (NRS ≥7). Overall, 41.4% (77/186) patients achieved complete or near-complete resolution of pain symptoms (NRS, 0–2). Moreover, a marked reduction in the need for rescue acetaminophen was reported throughout the study: at T30, 3.2% (6/186) patients reported using rescue acetaminophen (no more than one daily administration), while at T60 nobody was using rescue analgesics (P<0.0001 for both vs baseline).
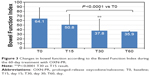
The improvement in pain intensity was paralleled by a marked improvement in bowel function, as shown by a statistically significant decrease in the mean BFI from 64.1±24.4 at baseline to 35.9±24.2 at T60 (mean difference −28.2, P<0.0001) (Figure 3). Mean BFI failed, however, to decrease below the threshold defining normal bowel function (ie, BFI <29). The improvement in BFI was statistically significant and clinically meaningful already after 15 days of treatment (mean difference in BFI from T0 to T15, −13.3, P<0.0001). The improved bowel function was associated with a decreased weekly use of laxatives (from 4.7±1.7 doses at baseline to 2.3±2.0 doses at T60, P<0.001).
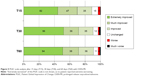
The primary combined efficacy measure (API reduction ≥30% from baseline to T30, with no constipation worsening) was achieved by 118 (63.4%) patients. A subgroup analysis according to age (75–85 years [n=148] and >85 years [n=38]) showed a trend toward greater improvements in pain control and bowel function in the subgroup aged >85 years (Figure 4). The rates of API improvement ≥30% from baseline to T15, T30, and T60 in patients aged 75–85 years and >85 years were 52.7% vs 60.5%, 89.9% vs 94.7%, and 91.2% vs 97.4%, respectively (P<0.05 overall). The proportions of responders in these two subgroups were, respectively, 61.5% and 71.0%.
The improvements in pain symptoms and constipation positively affected the patients’ global perception of treatment effectiveness (PGIC): already at T15, 69.7% (129/186) patients defined themselves as much or extremely improved compared with T0 (Figure 5). This high proportion of patients with a very positive perception of their status was maintained at later time points (71.3% for both T30 and T60). Only a minority of patients found their status much worse compared with T0 (0.5%, 1.6%, and 1.6% at T15, T30, and T60, respectively), and no patient felt extremely worsened at T30 or T60.
Safety and tolerability
Overall, the new treatment was well tolerated and the frequency of AEs was low. Severe AEs leading to treatment discontinuation occurred in only 1.6% (3/186) of patients and included somnolence/dizziness (one patient at T15), confusion (one patient at T15), and visual disturbance (one patient at T60). AEs of moderate severity and limiting further dose escalation of OXN-PR, or causing its reduction, were reported by 23 (12.4%) patients, with nine at T15 (4.8%), ten (5.3%) at T30, and four (2.1%) at T60. Gastrointestinal events and somnolence were the most frequently reported AEs (four [2.1%] patients for both events, at T15; three [1.6%] and five [2.7%] patients, respectively, at T30). Of note, in the age subgroup >85 years (n=38), only one patient experienced AEs (confusion at T60).
Discussion
The results of this analysis in patients aged ≥75 years, one-fifth of whom were older than 85 years, indicate that the fixed combination of strong opioid agonist–antagonist at low dose can be used effectively and safely for the treatment of chronic moderate to severe pain in subjects who have never been treated before with opioid analgesics. According to our findings, the switch from a non-opioid analgesic regimen to a strong opioid was successful even in patients at high risk of discontinuing opioid treatment early, due to potential opioid-induced worsening of the bowel dysfunction already present at baseline. Indeed, none of the patients discontinued treatment due to constipation. Among our patients with severe pain and bowel dysfunction, >60% responded to low-dose OXN-PR with a rapid and clinically relevant relief of pain and improvement, or no worsening, of constipation despite a reduction in the use of laxatives. Such clinical improvement was relevant for the patients, as highlighted by the high proportions of those who perceived themselves much or extremely improved. The treatment was well tolerated, with <2% of patients discontinuing treatment due to severe AEs (somnolence, confusion, visual disturbances).
Our findings confirm what has been shown by the few other studies addressing chronic pain treatment with OXN-PR in older patients. In the first prospective study designed specifically to test the efficacy and safety of low-dose OXN-PR in elderly patients (≥70 years) with chronic, noncancer pain and naive to strong opioids, most patients (71.7%) achieved the primary endpoint of ≥30% reduction in mean pain intensity from baseline to 4 weeks without deterioration of bowel function, in line with the present observation.20 Pain relief was substantial (−3.3 points on an 11-point NRS, P<0.0001) as was the reduction of the impact of pain on daily activities. Notably, daily functioning significantly improved, while no changes were observed in cognitive status, the impairment of which is among the reasons behind the reluctance to prescribe strong opioids to older people. In an observational multicenter study involving 7,836 patients with chronic pain of various etiology (mean age of 65.8 years; half of the patients aged between 61 years and 80 years), of whom only one-fourth were opioid-naive, OXN-PR significantly improved pain control, with an average 2.9 points reduction from baseline to 4 weeks in NRS intensity.25 OXN-PR was associated with a significant improvement of bowel function (decrease of mean BFI from 38.2 at baseline to 15.1 after 4 weeks), as shown also by our findings, and of quality of life. In that study, the frequency of overall AEs (20%) and serious AEs (2.3%) was apparently higher than in the present analysis; however, the causality between the AEs and PR OXN was assessed as possible in only a quarter (26.8%) of the cases. The sustained analgesia, improved bowel function, and the long-term safety of OXN-PR have been confirmed both in noncancer and cancer patients.26,27
The present study adds further evidence to the fact that older patients with pain inadequately controlled by Step I analgesics of the WHO ladder and naive to opioids can be safely switched to low-dose Step III analgesics (strong opioids). According to our findings, this could also be true for patients who have never received any around-the-clock analgesic pharmacotherapy, as was the case for one-third (33.9%) of our patients who were taking on-demand over-the-counter analgesics only, despite suffering from chronic pain of moderate to severe intensity. The high proportion of patients treating their pain only with on-demand analgesics reflects a common and still unresolved issue of chronic pain treatment, namely the undertreatment of elderly patients, and indicates that current guidelines are poorly implemented.
The direct progression from Step I to Step III analgesics has been investigated by a few authors. According to a subanalysis involving 162 opioid-naive patients with chronic pain from a large observational study, patients receiving OXN-PR (mean age 62.7 years) had significantly greater reduction in mean pain intensity, greater improvement of the quality of life, and fewer AEs compared with patients receiving other strong opioids (mean age 67.9 years).21 Over the course of treatment, the BFI of the OXN-PR group decreased (improvement), while that of the control group showed a slight increase. Different from our patients, both groups had BFI scores suggestive of normal bowel function at baseline.
The validity of skipping Step II of the WHO ladder is acknowledged also by current guidelines for the treatment of pain in older people, according to which the use of strong opioids at low doses is a valid option for the treatment of moderate to severe pain not adequately controlled with acetaminophen and/or NSAIDs.2,5 In addition, the usefulness and appropriateness of WHO-Step II analgesics (the weak opioids tramadol and codeine) for patients with pain not responding to Step I analgesics have been recently questioned.28–30 Besides the lack of strong evidence supporting the effectiveness of Step II analgesics, the equianalgesic doses of weak opioids are very high compared with strong opioids. This leads to an increase of AEs at higher doses, which may outweigh any additional analgesic effect. In addition, the analgesic activity of codeine and tramadol depends on their metabolization via the highly polymorphic CYP2D6. This results in insufficient analgesia in poor metabolizers and increased AEs in ultrarapid metabolizers. The European Medicines Agency has recently issued a series of limitations regarding the use of codeine, contraindicated in ultrarapid metabolizers (up to 10% of the Caucasian population) of any age.31 Furthermore, recent reports have shown that tramadol combined with antidepressants increases significantly the risk of serotonin syndrome in elderly patients.32,33
The extent of improvement of bowel function observed after switching to OXN-PR is unexpected, as our patients were opioid-naive and therefore their constipation at baseline was not caused by the action of exogenous opioids on opioid receptors in the gastrointestinal tract. The reason for such improvement is currently unclear. It may be speculated that naloxone antagonizes the effects of endogenous opioids (enkephalins, endorphins, and dynorphins) on opioid receptors in the gut wall, resulting in improved gut motility and function.34 Of note, in a recent investigation on naloxegol – an oral, peripherally acting μ-opioid receptor antagonist – the observed benefits of the drug in patients with opioid-induced constipation were unrelated to the response to laxatives.35
This study has several limitations, including the retrospective design, the absence of a control group, and the short period of observation. Moreover, influences on cognitive performance were not assessed after OXN-PR, and patients with cognitive impairment were excluded. Scant data are available on influences of opioids on cognitive performance in older patients with chronic pain, a major issue in a setting of care of the elderly. To our knowledge, only one study has prospectively explored the influences of OXN-PR on cognitive performance:20 no significant differences after OXN-PR were found by a serial mini-mental state examination. However, the observed population, prevalently females and patients suffering from severe chronic pain with concomitant bowel dysfunction, is well representative of older patients typically encountered in daily clinical practice. Despite its limitations, this study may therefore provide useful information for the management of chronic pain in older people in primary care.
Conclusion
The findings of this retrospective study suggest that low-dose OXN-PR is an effective option for analgesic treatment in the elderly. The switch from WHO-Step I analgesics to a Step III analgesic was easily and safely performed in our elderly population including patients aged >85 years, as was the initiation of OXN-PR in patients never previously treated with around-the-clock analgesics for their chronic pain, with benefits in terms of analgesia and bowel function, and without particular or unexpected safety and tolerability issues. Well-designed, long-term studies are necessary to fully understand the therapeutic potential and the safety of OXN-PR for the management of chronic pain in elderly outpatients and nursing home residents. Efforts to improve awareness among health care professionals of novel therapeutic options and updated treatment guidelines are also urgently needed.
Acknowledgments
Editing of the manuscript was performed by Lorenza Lanini, and native English editing and journal styling by Ray Hill, on behalf of HPS, Health Publishing and Services Srl. These services were funded by Mundipharma Pharmaceuticals Srl, Milano, Italy.
Disclosure
The authors report no conflicts of interest in this work.
References
Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10(4):287–333. | ||
Abdulla A, Adams N, Bone M, et al; British Geriatric Society. Guidance on the management of pain in older people. Age Ageing. 2013;42(suppl 1):i1–i57. | ||
Chai E, Horton JR. Managing pain in the elderly population: pearls and pitfalls. Curr Pain Headache Rep. 2010;14:409–417. | ||
Fredheim OM, Kaasa S, Fayers P, Saltnes T, Jordhøy M, Borchgrevink P. Chronic non-malignant pain patients report as poor health-related quality of life as palliative cancer patients. Acta Anaesthesiol Scand. 2008;52:143–148. | ||
American Geriatrics Society Panel on Pharmacological Management of Persistent Pain in Older Persons. Pharmacological management of persistent pain in older persons. J Am Geriatr Soc. 2009;57:1331–1346. | ||
Chou R, Fanciullo GJ, Fine PG, et al. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009;10(2):113–130. | ||
Gianni W, Madaio RA, Di Cioccio L, et al. Prevalence of pain in elderly hospitalized patients. Arch Gerontol Geriatr. 2010;51:273–276. | ||
Rianon N, Knell ME, Agbor-Bawa W, Thelen J, Burkhardt C, Rasu RS. Persistent non-malignant pain management using nonsteroidal anti-inflammatory drugs in older patients and use of inappropriate adjuvant medications. Drug Healthc Patient Saf. 2015;7:43–50. | ||
Kahan M, Srivastava A, Wilson L, Mailis-Gagnon L, Midmer D. Opioids for managing chronic non-malignant pain: safe and effective prescribing. Can Fam Physician. 2006;52:1091–1096. | ||
Vestergaard P, Rejnmark L, Mosekilde L. Fracture risk associated with the use of morphine and opiates. J Intern Med. 2006;260(1):76–87. | ||
Thorell K, Ranstad K, Midlöv P, Borgquist L, Halling A. Is use of fall risk-increasing drugs in an elderly population associated with an increased risk of hip fracture, after adjustment for multimorbidity level: a cohort study. BMC Geriatr. 2014;14:131. | ||
Kurz A, Sessler DI. Opioid-induced bowel dysfunction: pathophysiology and potential new therapies. Drugs. 2003;63:649–671. | ||
Bell TJ, Panchal SJ, Miaskowski C, Bolge SC, Milanova T, Williamson R. The prevalence, severity, and impact of opioid-induced bowel dysfunction: results of a US and European Patient Survey (PROBE 1). Pain Med. 2009;10:35–42. | ||
Nelson AD, Camilleri M. Chronic opioid induced constipation in patients with nonmalignant pain: challenges and opportunities. Therap Adv Gastroenterol. 2015;8(4):206–220. | ||
Wan Y, Corman S, Gao X, Liu S, Patel H, Mody R. Economic burden of opioid-induced constipation among long-term opioid users with noncancer pain. Am Health Drug Benefits. 2015;8(2):93–102. | ||
Meissner W, Leyendecker P, Mueller-Lissner S, et al. A randomised controlled trial with prolonged-release oral oxycodone and naloxone to prevent and reverse opioid-induced constipation. Eur J Pain. 2009;13:56–64. | ||
Simpson K, Leyendecker P, Hopp M, et al. Fixed-ratio combination oxycodone/naloxone compared with oxycodone alone for the relief of opioid-induced constipation in moderate to severe noncancer pain. Curr Med Res Opin. 2008;24(12):3503–3512. | ||
Löwenstein O, Leyendecker P, Hopp M, et al. Combined prolonged-release oxycodone and naloxone improves bowel function in patients receiving opioids for moderate-to-severe non-malignant pain: a randomised controlled trial. Expert Opin Pharmacother. 2009;10(4):531–543. | ||
Gatti A, Casali M, Lazzari M, et al. Prolonged-release oxycodone/naloxone in nonmalignant pain: single-center study in patients with constipation. Adv Ther. 2013;30(1):41–59. | ||
Guerriero F, Sgarlata C, Marcassa C, Ricevuti G, Rollone M. Efficacy and tolerability of low-dose oral prolonged-release oxycodone/naloxone for chronic nononcological pain in older patients. Clin Interv Aging. 2014;10:1–11. | ||
Hesselbarth S, Hermanns K, Oepen P. Prolonged-release oxycodone/naloxone in opioid-naïve patients – subgroup analysis of a prospective observational study. Expert Opin Pharmacother. 2015;16(4):457–464. | ||
World Health Organization [webpage on the Internet]. Cancer Pain Relief. 2nd ed. Geneva: 1996. Available from: http://apps.who.int/iris/bitstream/10665/37896/1/9241544821.pdf. Accessed January 11, 2016. | ||
Summary of Product Characteristics [webpage on the Internet]. Targin 5/2.5 mg, 10/5 mg, 20/10 mg and 40/20 mg Prolonged Release Tablets; 2015. Available from: http://www.medicines.ie/medicine/14383/SPC/Targin+5+2.5mg%2c+10mg+5mg%2c+20mg+10mg+and+40+20mg+prolonged+release+tablets/. Accessed February 28, 2016. | ||
Rentz AM, Yu R, Müller-Lissner S, Leyendecker P. Validation of the Bowel Function Index to detect clinically meaningful changes in opioid-induced constipation. J Med Econ. 2009;12:371–383. | ||
Schutter U, Grunert S, Meyer C, Schmidt T, Nolte T. Innovative pain therapy with a fixed combination of prolonged-release oxycodone/naloxone: a large observational study under conditions of daily practice. Curr Med Res Opin. 2010;26(6):1377–1387. | ||
Blagden M, Hafer J, Duerr H, Hopp M, Bosse B. Long-term evaluation of combined prolonged-release oxycodone and naloxone in patients with moderate-to-severe chronic pain: pooled analysis of extension phases of two Phase III trials. Neurogastroenterol Motil. 2014;26(12):1792–1801. | ||
Ahmedzai SH, Leppert W, Janecki M, et al. Long-term safety and efficacy of oxycodone/naloxone prolonged-release tablets in patients with moderate-to-severe chronic cancer pain. Support Care Cancer. 2015;23(3):823–830. | ||
Maltoni M, Scarpi E, Modonesi C, et al. A validation study of the WHO analgesic ladder: a two-step vs three-step strategy. Support Care Cancer. 2005;13:888–894. | ||
Furlan AD, Sandoval JA, Mailis-Gagnon A, Tunks E. Opioids for chronic noncancer pain: a meta-analysis of effectiveness and side effects. CMAJ. 2006;174:1589–1594. | ||
Natoli S, Lazzari M, Dauri M. Open questions in the treatment of cancer pain: time for a strong evidence-based approach? Expert Opin Pharmacother. 2015;16(1):1–4. | ||
European Medicines Agency [webpage on the Internet]. Restrictions on the Use of Codeine for Pain Relief in Children – CMDh Endorses PRAC Recommendation; 2013. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/Press_release/2013/06/WC500144851.pdf. Accessed January 11, 2016. | ||
Barber JB, Gibson SJ. Treatment of chronic non-malignant pain in the elderly: safety considerations. Drug Safety. 2009;32:457–474. | ||
Park SH, Wackernah RC, Stimmel GL. Serotonin syndrome: is it a reason to avoid the use of tramadol with antidepressants? J Pharm Pract. 2014;27(1):71–78. | ||
Holzer P. Opioid receptors in the gastrointestinal tract. Regul Pept. 2009;155(1–3):11–17. | ||
Chey W, Webster L, Sostek M, Lappalainen J, Barker P, Tack J. Naloxegol for opioid-induced constipation in patients with noncancer pain. N Engl J Med. 2014;370:2387–2396. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.