Back to Journals » Drug Design, Development and Therapy » Volume 12
Sintered dicalcium pyrophosphate treatment attenuates estrogen deficiency-associated disc degeneration in ovariectomized rats
Authors Chen CH, Chen WC, Lin CY , Chen CH , Tsuang YH, Kuo YJ
Received 11 April 2018
Accepted for publication 19 July 2018
Published 18 September 2018 Volume 2018:12 Pages 3033—3041
DOI https://doi.org/10.2147/DDDT.S170816
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Qiongyu Guo
Chia-Hsien Chen,1–3 Wei-Chuan Chen,4 Chun-Yi Lin,5 Chih-Hwa Chen,1–3 Yang-Hwei Tsuang,1,2 Yi-Jie Kuo2,6
1Department of Orthopedics, Shuang Ho Hospital, Taipei Medical University, New Taipei, Taiwan; 2Department of Orthopedic Surgery, School of Medicine, College of Medicine, Taipei Medical University, Taipei, Taiwan; 3School of Biomedical Engineering, College of Biomedical Engineering, Taipei Medical University, Taipei, Taiwan; 4Graduate School of Biotechnology and Bioengineering, Yuan Ze University, Taoyuan City, Taiwan; 5Department of Orthopedic Surgery, Taipei Medical University Hospital, Taipei, Taiwan; 6Department of Orthopedic Surgery, Wan Fang Hospital, Taipei Medical University, Taipei, Taiwan
Background: Estrogen deficiency is associated with musculoskeletal disorders. Sintered dicalcium pyrophosphate (SDCP) is a novel antiosteoporotic agent. In this study, we examined its use for restoration of bone quality and attenuation of disc degeneration in ovariectomy rats.
Methods: Sixty female Sprague Dawley rats were randomly divided into 3 groups, namely sham group undergoing sham surgery, ovariectomy (OVX) group receiving an equivalent volume of isotonic sodium chloride solution, and OVX/SDCP group orally administered with 0.25 mg/mL SDCP. Animals were sacrificed at 3 and 6 months post ovariectomy and lumbar vertebrae and intervertebral discs were harvested. Bone mineral density, micro-computed tomography analysis, and biomechanical testing were performed to assess bone quality. Histological analysis with hematoxylin and eosin, Alcian blue, and Masson’s trichrome stain were conducted to determine disc degeneration. Immunohistochemistry and real-time PCR were carried out to measure the expressions of aggrecan, type I collagen, type II collagen, and MMP-1, MMP-3, and MMP-13.
Results: SDCP improved bone quality as observed by the results of increased bone mineral density and stiffness in OVX rats. The improvement in disc degeneration induced by estrogen withdrawal was associated with reduced gene expressions of MMPs and increased production of collagen type II.
Conclusion: SDCP prevents osteoporosis and ameliorates disc degeneration in OVX rats. It represents a favorable therapeutic agent for osteoporotic and osteoarthritic conditions in clinical practice.
Keywords: sintered dicalcium pyrophosphate, ovariectomy, disc degeneration, matrix metalloprotease, inflammation
Introduction
Musculoskeletal conditions are defined as abnormalities of bone, joint, and muscles affecting hundreds of millions of people worldwide.1 They encompass a broad spectrum of disorders including osteoporosis, osteoarthritis, low back pain, and rheumatoid arthritis.2 Among these conditions, osteoporosis and osteoarthritis are increasingly prevalent with age and in the female population. While osteoporosis is a bone disorder with decreased bone mineral density (BMD) and consequent increased bone fragility, osteoarthritis is characterized by degeneration of articular cartilage with inflammation. These 2 disease entities are clinically distinct and have an inverse relationship in which there is a protective effect of one disease on the other.3,4 In postmenopausal women, coexistence of osteoporosis and osteoarthritis is suggested.4,5 Recent studies have demonstrated their coexistence in postmenopausal women as well as in animal models. Nevertheless, a treatment for these 2 coexisting disorders in women with estrogen deprivation remains challenging due to their different pathological processes.
Bisphosphates are commonly prescribed antiresorptive agents for osteoporotic patients, as they reduce bone resorption through directly inhibiting osteoclast activity. They are found to attach to hydroxyapatite on bone surfaces, particularly those undergoing active remodeling. Bisphosphonates have been shown to retard subchondral bone remodeling in an animal model of cartilage lesion.6 A research has reported that bisphosphonate reduces cartilage degeneration and the progression of osteoarthritis.7 They have been reported to reduce biomarkers of cartilage degradation and bone remodeling in osteoarthritis patients.8 On the other hand, a study has reported that use of bisphosphonate failed to ameliorate knee pain and radiographic changes of osteoarthritis in elderly women.9 In addition to antiresorptive property, several bisphosphonates have been demonstrated to have immunomodulatory activity.10–12
Sintered dicalcium pyrophosphate (SDCP) is a pyrophosphate analog which is biocompatible with bone in vivo and in vitro.13–15 It has been shown to exert antiosteoporotic effects comparable to that of alendronate in ovariectomized rats though inducing osteoclast apoptosis.13 Unlike bisphosphonates, SDCP has a high affinity for osteoblasts and induces osteoclast apoptosis by degradation of the Golgi apparatus in these cells.16 Inflammation has been suggested to contribute to the severity of osteoporosis.17 Several antiosteoporotic agents such as bisphosphate have been shown to exert immunomodulatory activities that improve bone loss in osteoporosis.6,7 It is of interest to explore the immunomodulatory effect of SDCP in osteoporotic setting. We hypothesized that SDCP exerts beneficial effects on estrogen deficiency-induced bone remodeling and disc degeneration in ovariectomized rats with emphasis on immunomodulatory activity. In the present study, we investigated role of estrogen deficiency in bone integrity and microstructure. We evaluated the effects of SDCP on gene expressions, BMD, biomechanical parameters, and disc degeneration in the ovariectomized rats. Proinflammatory mediators in situ were evaluated.
Materials and methods
Animals
Female Sprague Dawley rats aged 3 months and weighing 150 g were obtained from BioLasco, Taiwan (Taipei, Taiwan), and housed in environmentally controlled conditions (22°C, 50%±10% humidity, 12 hours light/dark cycle) with ad libitum access to standard laboratory chow and water. Rats received sham-operation (n=20) or bilateral ovariectomy (OVX, n=40) as previously described.16,18 OVX rats were divided into 2 groups, namely OVX group treated with isotonic sodium chloride solution as vehicle and OVX/SDCP group orally administered with 1 mL of 0.25 mg/mL (oral administration of 1.0 mg/kg/d) SDCP once a day (Purzer Pharmaceutical Co., Taipei, Taiwan).13,15 Rats were treated 5 times/wk for 3 and 6 months post-OVX, respectively. Guideline for the Care and Use of Laboratory Animals issued by Council of Agriculture Executive Yuan, Taiwan, was used for maintaining and handling animals. The animal study was approved by the animal care committee of Taipei Medical University (Affidavit of Approval of Animal Use Protocol Taipei Medical University) (IACUC Approval No LAC-2014-0335).
Micro-computed tomography (CT)
At designated time point, animals were sacrificed and the tail vertebrae samples were harvested and prepared for further scanning by micro-CT. Bruker SkyScan 1176 (SkyScan, Kontich, Belgium) was used to scan samples with 9×9×9 μm3 voxel size. Scanning was done at 65 keV of voltage, 380 μA of current, 985 ms of exposure time, and with a 1 mm aluminum filter. Reconstruction of sections was carried out with GPU-based scanner software (NRecon, SkyScan). The grayscale was based on the Hounsfield unit, and the validated calcium standards were scanned as its density reference. CTAn (SkyScan) was used to analyze the epiphysis area which can be identified refer to the growth plate. The region of interest was analyzed and the binary density (85–255) was considered as positive in this study. The 3D morphometric indices and BMD of the target volume were then calculated using the CTAn software. For illustration, CTVox (Version 2.7, SkyScan) was used to provide 3D images.
Histological analysis
Whole discs with adjacent vertebrae was harvested, dissected, and fixed in 10% formalin. The tissue samples were embedded in paraffin blocks and sectioned at a thickness of 5 μm. Sections were stained with hematoxylin and eosin, Alcian blue, and Masson trichrome stain. The slides were examined by 2 independent pathologists blinded to the experiment. The degrees of degenerative changes of intervertebral disc were graded according to the scoring system described previously.19
Immunohistochemistry staining
The blocks of tissue sample were sliced at a thickness of 5 μm. Tissue sections were subsequently deparaffinized in xylene and rehydrated in ethanol, followed by antigen retrieval and the blocking of endogenous peroxidase. The resulting slides were incubated overnight at 4°C with anti-rat MMP-1, MMP-3, MMP-13, type II collagen, aggrecan, and VEGF (1:100; Abcam Inc., Cambridge, MA, USA). The remaining procedures were performed according to the user manual (Dako, Agilent Technologies, Santa Clara, CA, USA), and the color (brown) was developed by incubation in DAB. The sections were counterstained with hematoxylin. Five representative regions of each section were selected and analyzed. Quantitative analysis was carried out using Image-Pro Plus 6.0 (Media Cybernetics, Rockville, MD, USA). The positive areas were considered as brown-yellow color, and integrated OD was calculated.
Real-time PCR (RT-PCR) analysis
Total RNA was extracted from tissue using Trizol (Sigma, St Louis, MO, USA) according to the manufacturer’s protocol. The mRNA levels of the genes analyzed were measured by RT-PCR amplification. Sequences for mRNAs from the nucleotide data bank (National Center for Biotechnology Information, Bethesda, MD, USA) were used to design primer pairs for RT-PCR reactions (Primer Express, Applied Biosystems, Foster City, CA, USA). The specific oligonucleotide primers used in this study are listed in Table 1. PCR cycles were adjusted to have linear amplification for all the targets. Each RT-PCR reaction was repeated at least 3 times. GAPDH was amplified under the same conditions to be used as internal controls, which is not affected by the treatment.20
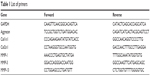  | Table 1 List of primers |
Following micro-CT, a 3-point bending test was carried out on the fracture site of the lumbar vertebra (L3) using a load mechanical testing machine (Instron, Series 4467 table-top loading frame, Norwood, MA, USA) as previously described.18 In brief, the planoparallel surfaces were obtained by removing the cranial and caudal ends of the vertebral specimen on which load bar was positioned, thereby allowing for a uniform compression test to be performed on individual rodent vertebrae. From the vertebral body, a central cylinder with planoparallel ends and a height of approximately 5 mm was obtained. All compression tests were performed in the displacement-control mode at a cross-head speed of 1 mm/min to eliminate any strain rate effects. Maximum load, yield stress, maximum stress, and the elastic modulus were obtained from the compression tests of vertebral bodies.
Statistical analysis
Mean and standard deviation were calculated for each group. Comparisons were performed using analysis of variance with post hoc comparison adjusted by the Bonferroni method. Data were analyzed with SAS 9.0 (SAS Institute Inc., Cary, NC, USA), and a P-value <0.05 was considered statistically significant.
Results
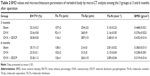
SDCP improves BMD of tail vertebrae in OVX rats
We examined the antiabsorptive effects of SDCP on tail vertebral body. The results showed that the BMD values in ovariectomized rats were decreased in association with advanced age (Table 2). BMD value of the OVX + SDCP group was significantly higher compared with that of OVX group regardless of the length of time after ovariectomy. Quantification of 3-dimensional trabecular structures revealed that bone volume percentage, trabecular thickness, and trabecular number in OVX group were significantly decreased in association with higher trabecular separation compared with that of the sham group (P<0.05) at 3 or 6 months postoperatively. SDCP treatment restored the decreases in values of bone volume percentage, trabecular thickness, and trabecular number in OVX rats (P<0.05), respectively, at 3 or 6 months postoperatively.
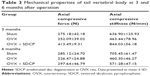
SDCP increases biomechanical strength of vertebrae in OVX rats
We next examined biomechanical strength of T5–T6 in each rat by determining the axial compressive force in Newtons (N) that each bone and axial compressive stiffness in N/mm that each bone could sustain before structural failure. As shown in Table 3, the values of axial compressive force and axial compressive stiffness were significantly decreased in the OVX group compared with that of the sham group (P<0.05). The data showed that SDCP improved the values of axial compressive force and axial compressive stiffness in ovariectomized rats at 3 or 6 months postoperatively (P<0.05). Interestingly, the OVX + SDCP group exhibited lower values of axial compressive force and axial compressive stiffness at 6 months compared with those at 3 months postoperatively (P<0.05).
We investigated the effect of SDCP on intervertebral disc degeneration in OVX rats. In sham group, hydrated nucleus pulposus with smooth cartilage and surrounding extracellular matrix was observed. OVX rats exhibited shrunken nucleus pulposus, cluster formation, and cleft formation with fissures. Histological analysis showed an increase in chondrocyte-like cell density in annulus fibrosus and moderate mucoid degeneration in nucleus pulposus. Our data showed that OVX-associated changes in the histological morphology were restored in presence of SDCP, showing normal number of notochordal cells in the nucleus pulposus and minor mucoid degeneration (Figure 1).
SDCP reduces MMP expression and collagen degradation
To determine the molecular mechanism by which SDCP attenuates disc degeneration induced by ovariectomy, we analyzed the expressions of MMP in the nucleus pulposus at mRNA and protein levels using RT-PCR and immunohistochemistry. As shown in Figure 2, OVX rat exhibited significantly increased mRNA expressions of MMP-1, MMP-3, and MMP-13 at 3- and 6-months compared with those of sham group. The data showed that SDCP treatment reduced the OVX-associated elevation of expressions of 3 MMPs at mRNA level in intervertebral disc. A significant immunohistochemical staining of MMP-1, MMP-3, and MMP-13 was observed in OVX rats compared with the sham group (Figure 2D–F). The results showed that the OVX-associated increase in protein expressions of MMPs were reduced in response to SDCP treatment both at 3 and 6 months postoperatively. In addition to MMPs, we determined the expression on type I and type II collagen in intervertebral disc. The data showed that ovariectomy led to a significant elevation of expression of type I collagen and a reduction in type II collagen expression at mRNA levels (Figure 3). Treatment of SDCP restored the expressions of 2 types of collagen at 3 months post-OVX (P<0.05). Immunohistochemistry assay showed that OVX rats exhibited a lower OD value of type II collagen in intervertebral discs compared with that of the sham group. Decreased expressions of type II collagen and aggrecan in OVX rats were restored in presence of SDCP at 3 and 6 months (Figure 3).
Discussion
In the present study, we demonstrated that SDCP inhibited the progression of osteoporosis and ameliorated the corresponding degeneration of intervertebral disc in OVX rats. We found that SDCP reduced OVX-associated increases in MMP expression in intervertebral discs. Moreover, SDCP treatment led to a restoration of type II collagen in intervertebral discs after OVX. The results suggest that OVX-associated inflammatory responses in disc tissue are attenuated by SDCP treatment.
Estrogen deprivation is associated with the development of many health conditions including bone abnormalities.21–24 It contributes to age-related bone loss affecting cortical and cancellous bones in women. Age-associated osteoporosis is treated by lifestyle measures and medications such as bisphosphonates. Bisphosphonates have been commonly prescribed for treatment of osteoporosis, and they theoretically inhibit osteoclast activity through impairing farnesyl pyrophosphate synthetase in mevalonic acid pathway. Several bisphosphonates have been shown to improve BMD and reduce vertebral fracture.25,26 In the present study, we demonstrated that SDCP improved vertebral BMD in OVX rats. The results are in support to previous findings that SDCP attenuates the osteoporotic effect of ovariectomy on long bones including tibia and femur.13,27 It is suggested that SDCP represents a favorable antiosteoporotic agent improving estrogen deficiency-associated bone loss in axial and long bones. We found no significant difference in bone fragility and quality between 3 and 6 months in OVX/SDCP group. The possible explanation is that the bone remodeling in OXV rats reaches a dynamic balance of resorption and formation. It has been reported that ovariectomy causes significant bone loss in the lumbar vertebral body at 60 days postoperation.28 Moreover, the animals used in this study were relatively young compared with those in previous study, showing difference growth pattern after OVX. Further studies are required to elucidate the effectiveness of SDCP on reduction of fracture rate in preclinical and clinical settings.
Increasing evidence has highlighted the role of inflammation in pathogenesis of estrogen-deficiency musculoskeletal disorders. Estrogen has been shown to inhibit production of proinflammatory cytokines such as IL-1β, IL-6, and TNF-α; hematopoietic growth factors like M-CSF; and cell differentiation agents RANKL in resident inflammatory cells.29–31 17β-estradiol is known to downregulate expression of IL-6 through interfering with NF-κB signaling.30 Estrogen deficiency has been reported to induce IL-17 production, which in turn induces production of proinflammatory cytokine including TNF-α, IL-6, and RANKL in joint and bone.32–34 It has been shown that estrogen plays a critical role in quality of connective tissues. Estrogen withdrawal leads to excessive productions of proinflammatory cytokines, which in turn increase the productions of several inflammatory mediators such as MMPs in degenerated disc and joints. In the present study, we found that OVX rats exhibited increased expression of MMP-1, MMP-3, and MMP-13. The results are consistent with that of previous study in which OVX was shown to cause acute inflammation.35–37 It has been demonstrated that exposure of disc to IL-1β increased the expression of MMP-1, MMP-3, and MMP-13 and decreased the levels of aggrecan, collagen type I, and collagen type II in nucleus pulposus cells and annulus fibrosus cells.38–42 In addition, IL-6 was shown to increase MMP-3 and decrease collagen and aggrecan expression in discs. Our results are in agreement with previous findings showing that SDCP restored the OVX-decreased level of aggrecan and type II collagen. We showed that SDCP inhibited production of MMPs in intervertebral disc in OVX rats, suggesting the anti-inflammatory effect of SDCP against OVX-induced inflammation. However, it is agreed that profile of inflammatory mediators in intervertebral disc after ovariectomy is complicated and that the OXV rat model is not suitable for study of long-term effect of antidegenerative disorders. Studies with a proper setting are necessary to reveal the mechanism underlying the pharmacological activity of SDCP for treating disc degeneration.
Conclusion
Altogether, it is indicated that SDCP treatment inhibits osteoporosis and attenuates disc degeneration in OVX rats. The mechanism underlying the antidegenerative effect of SDCP is postulated to be associated with modulation of the expression of MMPs, aggrecan, Col-II, and Col-I. Further studies are required to determine the dosage of SDCP, with a focus on its use to reduce fracture rates and ameliorate low back pain in postmenopausal females in preclinical and clinical setting.
Acknowledgment
This study was supported by Grant from Taipei Medical University (TMU104-AE1-B20).
Disclosure
The authors report no conflicts of interest in this work.
References
Woolf AD, Pfleger B. Burden of major musculoskeletal conditions. Bull World Health Organ. 2003;81(9):646–656. | ||
Smith E, Hoy DG, Cross M, et al. The global burden of other musculoskeletal disorders: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014;73(8):1462–1469. | ||
Yokozeki H, Igarashi M, Karube S, Shiraki M, Kurokawa T. The relation between osteoporosis of the spine and osteoarthritis of the knee. A study using dual energy X-ray absorptiometry and radiographs. Int Orthop. 1995;19(5):282–284. | ||
Verstraeten A, van Ermen H, Haghebaert G, Nijs J, Geusens P, Dequeker J. Osteoarthrosis retards the development of osteoporosis. Observation of the coexistence of osteoarthrosis and osteoporosis. Clin Orthop Relat Res. 1991;(264):169–177. | ||
Marcelli C, Favier F, Kotzki PO, et al. The relationship between osteoarthritis of the hands, bone mineral density, and osteoporotic fractures in elderly women. Osteoporos Int. 1995;5(5):382–388. | ||
Hayami T, Pickarski M, Wesolowski GA, et al. The role of subchondral bone remodeling in osteoarthritis: reduction of cartilage degeneration and prevention of osteophyte formation by alendronate in the rat anterior cruciate ligament transection model. Arthritis Rheum. 2004;50(4):1193–1206. | ||
Muehleman C, Green J, Williams JM, Kuettner KE, Thonar EJ, Sumner DR. The effect of bone remodeling inhibition by zoledronic acid in an animal model of cartilage matrix damage. Osteoarthritis Cartilage. 2002;10(3):226–233. | ||
Spector TD, Conaghan PG, Buckland-Wright JC, et al. Effect of risedronate on joint structure and symptoms of knee osteoarthritis: results of the BRISK randomized, controlled trial [ISRCTN01928173]. Arthritis Res Ther. 2005;7(3):R625–R633. | ||
Carbone LD, Nevitt MC, Wildy K, et al. The relationship of antiresorptive drug use to structural findings and symptoms of knee osteoarthritis. Arthritis Rheum. 2004;50(11):3516–3525. | ||
Frith JC, Mönkkönen J, Auriola S, Mönkkönen H, Rogers MJ. The molecular mechanism of action of the antiresorptive and antiinflammatory drug clodronate: evidence for the formation in vivo of a metabolite that inhibits bone resorption and causes osteoclast and macrophage apoptosis. Arthritis Rheum. 2001;44(9):2201–2210. | ||
Moreau M, Rialland P, Pelletier JP, et al. Tiludronate treatment improves structural changes and symptoms of osteoarthritis in the canine anterior cruciate ligament model. Arthritis Res Ther. 2011;13(3):R98. | ||
Pelletier JP, Troncy E, Bertaim T, et al. Treatment with tiludronic acid helps reduce the development of experimental osteoarthritis lesions in dogs with anterior cruciate ligament transection followed by reconstructive surgery: a 1-year study with quantitative magnetic resonance imaging. J Rheumatol. 2011;38(1):118–128. | ||
Kuo YJ, Sun JS, Rau G, Chen CH, Tsai TH, Tsuang YH. Better Osteoporotic Fracture Healing with Sintered Dicalcium Pyrophosphate (SDCP) Treatment: A Rat Femoral Fracture Model. J Histochem Cytochem. 2014;62(8):565–576. | ||
Sun JS, Chang WH, Chen LT, et al. The influence on gene-expression profiling of osteoblasts behavior following treatment with the ionic products of sintered beta-dicalcium pyrophosphate dissolution. Biomaterials. 2004;25(4):607–616. | ||
Sun JS, Tsuang YH, Lin FH, Chen LT, Hang YS, Liu HC. The application potential of sintered beta-dicalcium pyrophosphate in total joint arthroplasty. J Arthroplasty. 2003;18(3):352–360. | ||
Sun JS, Huang YC, Lin FH, Chen LT. The effect of sintered dicalcium pyrophosphate on osteoclast metabolism: an ultrastructural study. J Biomed Mater Res A. 2003;64(4):616–621. | ||
Mundy GR. Osteoporosis and inflammation. Nutr Rev. 2007;65(12 Pt 2):147–151. | ||
Mosekilde L, Danielsen CC, Knudsen UB. The effect of aging and ovariectomy on the vertebral bone mass and biomechanical properties of mature rats. Bone. 1993;14(1):1–6. | ||
Wang T, Zhang L, Huang C, Cheng AG, Dang GT. Relationship between osteopenia and lumbar intervertebral disc degeneration in ovariectomized rats. Calcif Tissue Int. 2004;75(3):205–213. | ||
Luo Y, Zhang L, Wang WY, et al. Alendronate retards the progression of lumbar intervertebral disc degeneration in ovariectomized rats. Bone. 2013;55(2):439–448. | ||
Felson DT. The epidemiology of knee osteoarthritis: results from the Framingham Osteoarthritis Study. Semin Arthritis Rheum. 1990;20(3 Suppl 1):42–50. | ||
Gokhale JA, Frenkel SR, Dicesare PE. Estrogen and osteoarthritis. Am J Orthop. 2004;33(2):71–80. | ||
Felson DT, Nevitt MC. The effects of estrogen on osteoarthritis. Curr Opin Rheumatol. 1998;10(3):269–272. | ||
Ivey JL, Baylink DJ. Postmenopausal osteoporosis: proposed roles of defective coupling and estrogen deficiency. Metab Bone Dis Relat Res. 1981;3(1):3–7. | ||
Crandall CJ, Newberry SJ, Diamant A, et al. Comparative effectiveness of pharmacologic treatments to prevent fractures: an updated systematic review. Ann Intern Med. 2014;161(10):711–723. | ||
Freemantle N, Cooper C, Diez-Perez A, et al. Results of indirect and mixed treatment comparison of fracture efficacy for osteoporosis treatments: a meta-analysis. Osteoporos Int. 2013;24(1):209–217. | ||
Kuo YJ, Tsuang FY, Sun JS, et al. Calcitonin inhibits SDCP-induced osteoclast apoptosis and increases its efficacy in a rat model of osteoporosis. PLoS One. 2012;7(7):e40272. | ||
Wronski TJ, Dann LM, Horner SL. Time course of vertebral osteopenia in ovariectomized rats. Bone. 1989;10(4):295–301. | ||
Shu L, Guan SM, Fu SM, et al. Estrogen modulates cytokine expression in human periodontal ligament cells. J Dent Res. 2008;87(2):142–147. | ||
Cheung J, Mak YT, Papaioannou S, et al. Interleukin-6 (IL-6), IL-1, receptor activator of nuclear factor kappaB ligand (RANKL) and osteoprotegerin production by human osteoblastic cells: comparison of the effects of 17-beta oestradiol and raloxifene. J Endocrinol. 2003;177(3):423–433. | ||
Shevde NK, Bendixen AC, Dienger KM, Pike JW. Estrogens suppress RANK ligand-induced osteoclast differentiation via a stromal cell independent mechanism involving c-Jun repression. Proc Natl Acad Sci U S A. 2000;97(14):7829–7834. | ||
Tyagi AM, Srivastava K, Mansoori MN, Trivedi R, Chattopadhyay N, Singh D. Estrogen deficiency induces the differentiation of IL-17 secreting Th17 cells: a new candidate in the pathogenesis of osteoporosis. PLoS One. 2012;7(9):e44552. | ||
Jochems C, Islander U, Erlandsson M, et al. Role of endogenous and exogenous female sex hormones in arthritis and osteoporosis development in B10.Q-ncf1*/* mice with collagen-induced chronic arthritis. BMC Musculoskelet Disord. 2010;11:284. | ||
Bezerra MC, Carvalho JF, Prokopowitsch AS, Pereira RM. RANK, RANKL and osteoprotegerin in arthritic bone loss. Brazilian journal of medical and biological research = Revista brasileira de pesquisas medicas e biologicas 38, 161–170. | ||
Reel B, Korkmaz CG, Arun MZ, et al. The Regulation of Matrix Metalloproteinase Expression and the Role of Discoidin Domain Receptor 1/2 Signalling in Zoledronate-treated PC3 Cells. J Cancer. 2015;6(10):1020–1029. | ||
Cui Z, Xu C, Li X, Song J, Yu B. Treatment with recombinant lubricin attenuates osteoarthritis by positive feedback loop between articular cartilage and subchondral bone in ovariectomized rats. Bone. 2015;74:37–47. | ||
Zhu S, Chen K, Lan Y, Zhang N, Jiang R, Hu J. Alendronate protects against articular cartilage erosion by inhibiting subchondral bone loss in ovariectomized rats. Bone. 2013;53(2):340–349. | ||
Le Maitre CL, Freemont AJ, Hoyland JA. The role of interleukin-1 in the pathogenesis of human intervertebral disc degeneration. Arthritis Res Ther. 2005;7(4):R732–R745. | ||
Millward-Sadler SJ, Costello PW, Freemont AJ, Hoyland JA. Regulation of catabolic gene expression in normal and degenerate human intervertebral disc cells: implications for the pathogenesis of intervertebral disc degeneration. Arthritis Res Ther. 2009;11(3):R65. | ||
Studer RK, Vo N, Sowa G, Ondeck C, Kang J. Human nucleus pulposus cells react to IL-6: independent actions and amplification of response to IL-1 and TNF-α. Spine. 2011;36(8):593–599. | ||
Richardson SM, Doyle P, Minogue BM, Gnanalingham K, Hoyland JA. Increased expression of matrix metalloproteinase-10, nerve growth factor and substance P in the painful degenerate intervertebral disc. Arthritis Res Ther. 2009;11(4):R126. | ||
Wei Y, Zhi-Hong W, Gui-Xing Q, Bin Y, Jun C, Yi-Peng W. Extracellular signal-regulated kinase inhibition modulates rat annulus fibrosus cell response to interleukin-1. Spine. 2013;38(17):E1075–E1081. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.