Back to Journals » Clinical Interventions in Aging » Volume 15
Risk Prediction for Adverse Outcomes for Frail Older Persons with Complex Healthcare and Social Care Needs Admitted to a Community Virtual Ward Model
Authors Lewis C , O'Caoimh R , Patton D , O'Connor T , Moore Z , Nugent LE
Received 31 October 2019
Accepted for publication 2 May 2020
Published 22 June 2020 Volume 2020:15 Pages 915—926
DOI https://doi.org/10.2147/CIA.S236895
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Walker
Clare Lewis,1 Rónán O’Caoimh,2,3 Declan Patton,1 Tom O’Connor,1 Zena Moore,1 Linda E Nugent1
1School of Nursing and Midwifery, Royal College of Surgeons Ireland, Dublin, Ireland; 2Clinical Sciences Institute, National University of Ireland Galway, Galway City H91 TK33, Ireland; 3Mercy University Hospital, Cork City T12 WE28, Ireland
Correspondence: Clare Lewis Email [email protected]
Purpose: Population ageing is challenging healthcare systems with limited resources, necessitating the development of new care models to address the needs of older, frail community-dwellers. Community Virtual Wards (CVW) reduce adverse events in these patients. We examined the effect of an established CVW on pre-defined health trajectories (between “stable”, “deteriorating”, and “unstable” states) and characteristics that increased the likelihood of adverse healthcare outcomes (hospitalization, institutionalization and death).
Patients and Methods: We collected prospective data on frail patients admitted to a CVW in a single centre in Ireland. Relationships between risk scores, health states and adverse outcomes at 30, 60 and 90 days after admission were examined using multinomial regression analysis.
Results: In total, 88 community-dwellers, mean (±SD) age of 82.8 ± 6.4 years, were included. Most were severely frail on the Rockwood Clinical Frailty Scale (mean 6.8/9 ± 1.33). Reaching stability (“stable” state) within 30 days was a predictor for stability at 60 and 90 days and remaining at home. Stability was also associated with fewer care episodes (< 2) (p=< 0.001), a requirement for fewer healthcare professionals (HCP) (< 7) (p< 0.001) and lower risk of delirium (p< 0.001). By contrast, being “unstable” at 60 days increased the numbers of HCP referrals (> 7) and was predictive of more acute episodes (> 2) and institutionalization or death (p< 0.001). Predictors of adverse outcomes of either institutionalization or death included frailty status, function, mobility, nutrition, pressure ulcer risk and cognition.
Conclusion: A CVW model can provide a framework for monitoring and case management to support older people to remain at home or identify those at risk of institutional care. The use of defined health states helped to stratify those at lower or higher risk in an already high-risk frail population. Level of frailty, function, mobility, nutrition, pressure ulcer risks and cognition were predictive of remaining at home and reaching a level of stability or instability/deterioration and institutional care.
Keywords: community virtual ward, older persons, complex care, case management, risk prediction, health states
Background and Introduction
Population ageing is occurring rapidly worldwide particularly in more developed countries.1,2 As a result, a greater proportion of frail older adults are expected to be living in the community but at increased risk of adverse health outcomes including emergency department (ED) admission, institutionalization and hospitalization.3,4 While risk-stratification is useful in allocating limited resources, few instruments or models are available to support healthcare professionals to manage the complex health and social care needs of these patients.
Community Virtual Wards (CVW), defined as a team of trained healthcare professionals providing specialist interdisciplinary case management to community-based older adults at risk of fragmented care and adverse healthcare outcomes, were first developed in the United Kingdom.5,6 These are coordinated by dedicated case managers and are based on a conceptual model of risk, targeting supports and interventions to older community-dwellers likely to experience adverse health outcomes.5 CVW models improve health-related quality of life, reduce unplanned hospital admissions, reduce the length of stay (LOS) after Emergency Department (ED) presentation and statistically significantly reduce ED presentations.5,7
Such a CVW model was developed to address increasing complexity in community care in an area with a rapidly ageing population (North Dublin, Ireland) aiming to identify predictors of adverse healthcare outcomes in older, frail community-dwellers and tailor limited resources accordingly.5 The model of care in North Dublin supported older persons to remain at home and transitioning from hospital to community. Care was coordinated by a senior nurse working with hospital consultants, general practitioners, public health nurses (PHN), occupational therapists, physiotherapists, social workers, geriatricians, and hospital specialists in chronic disease management. This aligns with health policy including Ireland’s National Clinical Programme for Older People, Integrated Care Programme for Older Persons and Sláintecare report, with services from acute and primary care working together as a continuum.8–10
The model operated under three levels of CVWs separated to include red (high risk) amber (moderate risk) and green (low risk). Patients were considered suitable based on criteria. This included a recent hospital admission with a longer length of stay (>11 days), and evidence of more complex care needs associated with frailty that included cognitive and functional level, and social care needs A recent Day hospital review with evidence of decline within 30 days and considered a high risk of a hospital admission.5 Evidence of gradual deterioration over the last 3 months and an increase in health and social care needs.5
Although previous research has shown the impact of the North Dublin model on reducing ED attendances and unplanned hospital admission little is known about the factors that influence decision-making in CVW models such as this or their effect on other important healthcare outcomes.5 Specifically, it is unclear what factors influence levels of risk of adverse outcomes over time and decisions to transfer patients to lower CVW levels and subsequent discharge from the ward. Given this, we examined health trajectories ie changes in health status between pre-defined states (stable, deteriorating, and unstable) and the impact of patient-specific factors on risk of hospitalization, institutionalization and death using individual screening and assessment scale scores for patients admitted to a CVW.
Patients and Methods
Study Design
This study used a non-experimental correlational design using prospective data over a period of 90-day post-admission to the CVW.
Sample
A convenience sample of frail, community-dwelling older persons admitted to the CVW and referred from specialist gerontology services including the local Day hospital and acute hospital were recruited. Inclusion criterion including participants aged >65 years, evidence of frailty and community dwellers i.e. living in their own or relative’s homes and not in residential care, evidence of deterioration in the last 3 months. Exclusion criterion was <65 years, no evidence of frailty and/or living in residential care.
The North Dublin CVW has three levels: green, amber and red from low to high risk; all patients initially enter the red or amber wards after assessment by the CVW case manager before being transferred to lower levels after interval assessment (triage phase). Flow within the CVW including the triage phase is presented in Figure 1. This study was conducted in accordance with the Declaration of Helsinki. Ethics approval was obtained from the research ethics committee of the Royal College of Surgeons Ireland on April 21, 2016 (REC1219). Patients provided written informed consent after admission. Assent was obtained by family or a legal representative if required following processes outlined in the Assisted Decision Making Capacity Act 2015.11 To protect confidentiality and anonymity each participant’s information was coded on entry to the CVW.
 |
Figure 1 The North Dublin community virtual ward (CVW) assessment and triage process. |
Data Collection
Data collection began in March 2016 and ended in July 2017. This duration was necessary to ensure that all participants completed a CVW admission. Descriptive statistics collected included demographic data, co-morbidities, medications, social history (including signs suggestive of self-neglect, see below), continence status, and the number of prior hospital admissions, emergency department (ED) presentations and falls in the previous 3 months. Resource provision and utilization was captured through episodes of care, the type of events, interventional strategies and number of healthcare professional (HCPs) involved. Direct and indirect contact by HCPs was measured based on the Nursing Interventions Classification System: “Direct Care” comprises interventions provided through direct interaction with the patient; “Indirect Care” includes therapeutic interventions provided away from the patient to support or enhance care.12 Outcome data on adverse events after admission to the CVW were obtained from primary care (discussion with family doctors), hospital coding systems and patient case records/charts. Complex care was defined based on common characteristics within the data after the initial presentation the CVW.
Outcomes
Outcomes were measured by (a) the ability to reach/achieve a level of stability i.e. to become stable (dichotomized into yes/no) at 30, 60 and 90 days after admission to the CVW. Health states were pre-defined as “unstable”, “deteriorating”, or “stable”, adapting previous hospital criteria following an acute clinical event (Table 1) and (b) the occurrence of an adverse event/outcome (dichotomized into yes/no) including ED presentations, hospitalizations, institutionalization (decision to admit rather than the date of admission) and death at 30, 60 and 90 days after admission to the CVW.13–16 Mortality data were collected up to 120 days.
 |
Table 1 Health States Measured at 30, 60 and 90 Days After Admission to the Community Virtual Ward |
Data collected including validated scales/questionnaires and the domain (risk area) assessed are presented in Table 2. Hospitalizations and ED presentations were compared pre-and post-CVW. Experiencing a delirium was compared with health states and risk of adverse outcomes. The level of frailty was measured using the Rockwood Clinical Frailty Scale (CFS) on admission to the CVW. The CFS is a 9-point scale measuring the level of frailty from robust and vulnerable stages through to mild, moderate, severe, very severe and terminal stages of frailty.17 Signs of self-neglect were collected based on previous criteria.18,19
 |
Table 2 Summary of Data Items and Scales Collected as Part of the Community Virtual Ward (CVW) Model |
This included failure to attend to personal hygiene, repeated refusal of (required/appropriate) services reasonable to improve quality of life, signs of self-endangerment and inadequate food provisions.18,19 Mobility level was measured using the Timed up and Go test (TUG) and a modified version of the Functional Independence Measure (FIM), activities of daily living (ADL) function was captured using a modified version of the Barthel Index (BI), pressure ulcer risk was measured using the Walsall pressure ulcer risk tool.20–22 Nutritional status was based on the Malnutritional Universal Malnutrition Screening Tool (MUST).23 Cognition was measured using the Mini-Mental state examination (MMSE) and mood through the application of the Geriatric Depression Scale (GDS).24,25 Risk of further hospital admission based on the Identification of Seniors at Risk (ISAR) was scored on admission and at 60 days and 90 days.26 These time-periods were chosen as recovery periods almost double for frail older persons with risks of deterioration and hospitalization observed up to 90 days.27,28
Descriptive data were used to characterise the type of events experienced including delirium (no bespoke delirium measure was recorded), the reason for referral to the CVW, the events experienced during admission and interventional strategies (including resource provision). The degree of co-morbidity was summarised using the Charlson co-morbidity index.29
Defining Complex Care
Complex care for older persons was defined based on common characteristics on presentation to the CVW. This included having an age of 75 years, two or more co-morbidities, evidence of moderate-to-severe frailty, one or more acute events in the last 3–6 months, specialist support/interventions required as current care needs to be exceeding the capacity of the core primary care team to manage them, and/or high-intensity users of health and social care services defined as requiring regular access for more than 3 months.
Study participants could experience multiple types of events following the initial acute episode, and this presented challenges in measuring the impact of a singular event. To account for this, care episodes were grouped measuring the impact of these on study outcomes.30 Care episodes were characterised by the acuteness of the episode(s), defined as occurring over a 14–30-day time-period. An episode was counted as complete if there were no further events observed in the 14–30 days’ following interventions and the individual showed evidence of stability (using the stability criteria in Table 1). A measure of 30-days was selected as a metric to assess stability. This is often considered as a critical period of risk for further events after an acute care episode e.g. after ED attendance or hospitalization (Table 3) details the type of interventions used to address and manage patient’s complex care needs.7,31–33,45
 |
Table 3 Typical Events and Interventions Applied as Part of the North Dublin Community |
Data Analysis
Data were analysed using SPSS version 25 (IBM statistics, Chicago, IL, USA). Univariate analysis was performed initially to test variables individually comparing to outcome variables to determine the significance of interactions. This informed the development of a logit multinomial regression analysis model.34 Measure of goodness of fit was tested through Chi-Square determining the level of independence of observations seen between two variables and how these related to the population under investigation.
Results
Patient Characteristics
The characteristics of patients included in the CVW are presented in Table 4. In summary, their mean age was 82.7 with a standard deviation (SD) of ±6.4 years. In all, 100% (N=88) were classed as frail. Most of the sample (66%) were female (n=58/88). The average length of stay on the CVW was 123 days ± SD of 100.13. Most were living with two or more co-morbidities, see Table 4. The Charlson co-morbidity index estimated that the majority (n=36/88) of patients had a 20% chance of survival, with 30% (n=26/88) having 0% chance of survival over the next 10 years. Incontinence was common (n=64/88, 73%) and most patients had at least one fall within a 3-month period prior to admission (n=51/88, 58%). Signs suggestive of depression (GDS > 5) were present in a quarter of the sample (n=21/88, 23.9%). Malnutrition risk was present in nearly half the sample (n=42/88, 48%) and a third of the sample were at high risk of developing a pressure ulcer (n=30/88, 43%). Over half of patients admitted to the CVW (n=5/88, 55%) had an unplanned hospital admission and an ED presentation within a 3-month period, with a mean of 50.6 (median 31) unplanned hospital bed days prior to admission. Over half of patients lived with a caregiver (n=55/88), the remainder lived alone (n=33/88). Signs suggestive of self-neglect were observed in over half of the sample (n=45/88, 51%). Levels of mobility were relatively equally distributed ranging from independent/modified independent (n=19/88, 21%), supervision (n=30/88, 34%) to assistance of 1 person (n=25/88, 28%), with a small proportion requiring the assistance of 2 persons (n=9/88, 10%) or hoist (n=5/88, 5%).
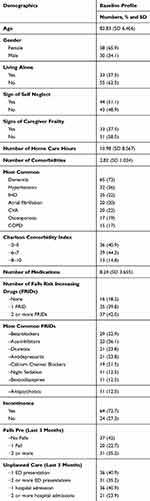 |
Table 4 Characteristics of Patient Included in the Community Virtual Ward |
The TUG was prolonged for most measuring between 20 and 30 seconds for one-third (n=29/88, 33%), and > 30 seconds for 43% (n=38/88, 43%). The estimated means for TUG scores within this study cohort were adjusted for age, gender, level of mobility, and level of cognitive impairment on admission to the CVW. The expected durations of TUG scores for this study cohort were between 20 and 30 seconds (F, 4=15.79, p<0.001). The level of cognitive impairment was not associated with TUG scores at baseline (p=0.12). The majority had cognitive impairment (65/88) and were diagnosed with dementia based on symptoms and MMSE scores (MMSE mean score 21.31, median 21.00). Lower MMSE scores (0–17) were associated with increasing age (> 85 years n=19/88) (p=0.001). Many of the patients (n=47/88, 53%) were classed as functionally highly dependent measured through the Barthel Functional index (BI) with maximum scores (0–5) mean 2.84, median 2 increasing within the 85-year age group (n=15/88).
Transfer Between Levels of the CVW
Most participants (N=78/88) were admitted to the Red (high risk) CVW following an acute event (within the last 30 days) with the remainder admitted to amber (N=10/88) (moderate risk). Those admitted direct to the amber CVW had no event(s) in the last 30 days, with evidence of gradual decline over a 3–6 month period (n=10/88, 12%). The highest point of risk following admission to the Red (high risk) to experience a further event (N=71/88) was during the first 14-day post-admission.
Type of Events
Examples of several events, which often overlapped, and the types of interventional strategies delivered are described in Table 3. Events were grouped and categorized based on their frequency during an episode of care. These included clinical events (21%, 18/88), functional decline resulting in an increase in social care needs (34%, 30/88), falls, functional and cognitive decline with behavioural and emotional changes and an increase in social care needs (28%, 24/88), and falls with functional decline in addition to weight loss, clinical events and an increase in social care needs (8%, 16/88). There were significant gender differences observed, with men more likely to deteriorate at 60 days and require a higher number of HCPs involved in their care (>7) (F, 3=4.14, p=0.009) compared to women (F, 3=4.14, p=0.009).
Self-Neglect
Signs suggestive of self-neglect on admission to the CVW including neglect to personal hygiene and inadequate food previsions were significantly associated with institutionalisation (p<0.001). However, on further analysis, signs of self-neglect were not predictors for adverse outcomes within this study sample (p=0.29).
Adverse Outcomes
At the end of the observational period in July 2017, 13% (12/88) of patients had died with 20% having a hospital admission (18/88) including those who had 2 or more admissions (6/88, 6.8%). The number of participants presenting to the ED were significantly lower while admitted to the CVW (30%, n=27, mean 0.36, SD 0.61) in comparison to their previous ED presentations (76%, n=67, mean 1.11 SD 0.76). There was a reduction in unplanned hospital admissions during the study period (20.5%, n=18, p<0.001). This included a reduction in bed day use from 4449 bed days (mean bed days per participant 50.56, SD 58.39) to 555 bed days (mean bed days per participant 6.31, SD 18.27).
Experiencing a delirium during the first 30-day post-admission was significantly associated and correlated to instability at 60 days of the admission (b=1.96, Wald X2 (1)=7.67, p=0.006, OR 7.13). Once adjusted for age and gender the risk of experiencing a delirium was statistically higher in men than in women (p<0.001) with a higher number of events including falls, cognitive and functional decline (F, 1=14.72 p=0.01) observed. The highest risk of a fall post-admission to the CVW was observed in the first 30 days of admission (25%, n=22) with a reduction in falls observed beyond 30 days (5%, n=5) (p<0.001).
Predictors of Institutionalization
Higher risk of institutionalization observed at 90 days was seen in those experiencing a delirium at 30 days (b=1.89, Wald X2 (1) 11.76, p<0.001, OR 6.64). Several screening and assessment tools (scales and questionnaires) were predictive of an increased risk for institutional care compared with the likelihood of remaining at home. Neither age (p=0.48) or gender (p=0.13) significantly predicted institutionalization. Moderate levels of frailty observed in the Rockwood CFS on admission was an independent predictor for remaining at home at the end of the study period. (b=−1.93, Wald X2(1) =5.66, p=0.017, OR 0.14). Lower levels of mobility observed at 60 days of the admission (requirement for assistance of 1–2 people or a hoist) were predictors for institutionalization at the end of the study period (b=−1.14, Wald X2(1)= 6.03, p=0.01, OR 0.31).
Lower levels of cognitive impairment ranging from between mild to moderate levels (MMSE scores18–30) were predictive of remaining at home (b=−1.81, Wald X2(1) = 6.85, p=0.009, OR.163). Advanced stages of cognitive impairment (MMSE scores 0–17) increased the risk of institutionalization (b=−0.86, Wald X2(1)=1.93, p= 0.04, OR 0.41). Risks of institutionalization were higher at the end of the study period in those with MUST scores of >2 (high risk) measured at 60 days (b=−4.08, Wald X2(1) =8.32 p=0.004, OR 0.01). Lower levels of ISAR scores (3/4) measured at 60 days were predictive of home at the end of the study period (b=−5.47, Wald X2(1) =14.06, p<0.001, OR, 2.64). Similarly, Walsall pressure ulcer risk scores of low (0–3, 6–9) were predictors for home with higher risk scores of medium (10–14) to high risk (>15) predictors for institutionalization (b=2.15, Wald X2 (1) =4.20, p=0.040, OR 0.11). Risk scores and their relationship to institutionalization are presented in Table 5.
 |
Table 5 Multinomial Logit Regression Analysis Factors Associated with Institutionalization |
Health States
The majority of patients were classed as “unstable” on admission (60/88, 68%) with 50% (44/88) progressing to a stable state within 60 days following interventions. Patients reaching a stable state within the first 30 days were more likely to remain at home at the end of the study (Wald X2 (1) 15.23, p=0.001, OR 3.39) versus longer durations > 30 days and higher risk of institutionalization (b=0.68, Wald X2 (1)=7.40, p=0.006, OR 2.09) (Table 6). The total number of episodes of care was predictive of health states. Patients maintaining a level of stability at 60 days were 21 times more likely to remain at home at the end of the study period (90 days) (b=3.04, Wald X2 (1)=18.89, p<0.001, OR 21.06). The risks of institutionalization were higher in patients remaining in an unstable state or had deteriorated at the end of the study period (b=−0.88, Wald X2 (1) =18.04, p<0.001, OR 4.15). The total number of episodes of care were predictive of health states. Achieving a level of stability was observed in those experiencing <2 episodes of care and increased the likelihood of remaining at home (b=19.9, Wald X2(1) =48.92, p<0.001, OR 44.89).
 |
Table 6 Health States Measured at 30 and 60 Days and Outcomes |
Healthcare Utilization
The number of HCPs involved across the 3 levels of CVWs was predictive of higher risk health states. This was most significant in the red (high risk) CVW with >7 HCPs and an increased risk of an unstable (b=2.24, Wald X2(1) =8.25, p=0.004, OR 9.43) or deteriorating health state (b=2.69, Wald X2(1) =10.79, p=0.001, OR 14.77). Similarly, >5 HCPs directly involved in the amber (moderate risk) ward (b=0.53, Wald X2(1) =6.22, p=0.01, OR 0.58) or green (low risk) ward (b=15.10, Wald X2 (1) =20.12, p<0.001, OR 6.22) increased the likelihood of deteriorating by the end of the CVW admission.
The types of interventions were predictors of health states. Patients requiring standard interventions were more likely to achieve a level of stability at 30 and 60 days versus those requiring standard plus behavioural interventions (b=1.91, Wald X2(1) =9.06, p=0.003, OR 0.14). There were differences in gender and type of interventions required. Women were more likely to require standard interventions (clinical, functional, nutritional, social) and men required additional behavioural management strategies (b= −1.32, Wald X2(1) =7.12, p=0.008, OR 1.18).
Discussion of Results
The CVW model provided the framework for risk prediction expanding on previous research in the management of older persons in a community setting.5 This included the process of assessment and identification of risk often observed in a frail community-dwelling older population. Previous CVW models have focused on reducing unplanned hospital care and used risk scores pre-admission and upon discharge to predict outcomes.6,7,32 This can be challenging in a vulnerable older population as risk scores are often high.35 Therefore, this study’s findings support HCPs in decision-making at stages of care delivery rather than on admission and discharge.6,7,32 This includes core areas of risk including self-neglect, frailty, cognition, function, mobility, nutrition and pressure ulcer development in addition to health states and transitions of care (number of episodes, types of interventions, number of HCPs involved). These provide clinical metrics to assist with decision-making and predict outcome.
Self-Neglect
The likelihood of experiencing signs of self-neglect increases with advanced levels of frailty and cognitive impairment.36 Within this study, signs suggestive of self-neglect were present among half (n=45/88, 51%) of patients. The most common signs were lack of attention to personal hygiene and inadequate food provisions and were associated with a higher risk of institutionalization. Although there were no significant relationships seen during the deeper analysis of results, these are clinically meaningful results identifying potential risks in a frail population. Early identification of these symptoms highlights that this model offers a pathway of care to potentially reduce the risks of hospitalization and institutionalization often associated with signs of self-neglect.18,36
Falls
There was a strong relationship between a reduction in the number of falls post-admission to the CVW and period (>30 days) to first fall post-admission. Falls decreased as the number of days to the first fall increased beyond 30 days with a reduction in falls rates by a quarter (28%). This is significant in a frail population where risks of falls are reported as high due to the presence of physical decline, reduced co-ordination and impaired balance.37 Early intervention and appropriate monitoring in the red (high risk) CVW following admission with the delivery of a home-based interventional programme of care may have resulted in a falls reduction.38
Unplanned Hospital Admissions and ED Presentations
There was evidence of a reduction in unplanned hospital admissions and ED presentations during the study period. This was potentially due to appropriate risk stratification resulting in higher levels of monitoring and intervention in the red (high risk) CVW if an event had occurred in last 30 days (including a hospital admission). In an older population, the first 30 days following an event is considered the most unstable period with increased risks of hospital admission.28 This was observed in this study population experiencing a further event on average 14 days post-admission with higher risks observed in those recently discharged from the hospital. A recent hospitalization within the preceding 3-month period increases the numbers of adverse clinical events, hospital admissions and mortality within the next 12 months.39 This is higher in older persons (> 79 years) with evidence of frailty, cognitive impairment and lower levels of function.39 Therefore, the 30-day risk for events pre- and post-admission to the CVW is a key finding and adds to the development of this model of care including the selection of the red level (high risk) CVW.
Transitions of Care
The number of episodes, delirium, types of interventions and number of HCPs directly involved were predictive of adverse outcomes (institutionalization) and were part of transitions of care. Experiencing more than two episodes of care increased the risks of institutional care. Risk of delirium was also higher in patients who experienced more than two episodes of care and were seven times more likely to be unstable at 60 days. Institutionalization was also higher with patients six times more likely to be institutionalized at the end of the study period. This is consistent with previous study findings reporting that patients were five times more likely to be institutionalized following a delirium in an acute hospital setting.40 In this study sample, lower risks for experiencing a delirium included less than two episodes of care and achieving a level of stability at 60 days.
Interventions
In this study, gender was predictive of the types of interventions required and health states. Requiring standard interventions (clinical, functional, nutritional, social) increased the likelihood of achieving stability. Achieving a level of stability was reduced if required a behavioural component to care with patients more likely to be unstable at 60 days of the admission. This was associated with gender with male gender more likely to require behavioural interventions versus female gender. Gender differences have been observed in the previous research investigating a frail older population.41 Women over 65 years were more likely to experience events requiring functional and social interventions in comparison to men experiencing greater complexity.41 More recently, researchers reported that women tolerated higher levels of frailty with lower levels of complexity, and evidence of reverse response or delay in transitions observed in frailty over 4 years.42 These study findings add to a growing body of evidence of gender differences and variances in care needs. This is important to assist in the development of strategy and policy that incorporate gender as well as population growth to address population healthcare needs.10
Healthcare Professional Involvement
Higher numbers of HCPs directly involved in care increased the risk of adverse outcomes. This included greater than seven HCPs directly involved in the red (high risk) CVW level a predictor for an unstable health state and risk of institutionalization. The same outcomes were observed in amber (moderate) level, and green (low) level CVWs with greater than five HCPs directly involved. This provides new evidence on measuring risk using direct resource provision rather than the accumulation of deficits and risk scores as measures for outcomes. Using numbers of HCPs as measures of risk has the potential to guide HCPs and questions high-intensity use of resources in a home environment if no evidence of achieving a level of stability. This is also important for effective and efficient workforce and resource planning in determining optimal numbers of HCPs to deliver safe levels of care to older persons at home.10 Accounting for complexity and predicting outcome in this population is challenging.43 Therefore, the use of episodic-based measurements to include the type of events and interventions and number of healthcare professionals shows promise in measuring complexity in the community.
Risk Screening Tools as Predictors for Home or Institutionalization
Within risk assessment tools, screening for frailty, mobility, BI, MMSE, ISAR, MUST and pressure ulcer risk were predictive of home or institutionalization and was most significant at 60 days of the CVW admission. Interestingly, the cut off scores were higher for predicting home versus institutionalization than has been observed in the previous research. This was detected in the Rockwood, BI, MMSE, ISAR and MUST with moderate to higher levels of risk predictive of home in this study once achieved a level of stability at 60 days of the admission.
Health States
Health states predicted favourable and adverse outcomes moving from a state of unstable to stability versus remaining in an unstable state or deteriorating. Patients that had transitioned from unstable to stable at 30 days and remained stable (measured at 60 days) were 21 times more likely to be at home at the end of the study period. By contrast, patients in an unstable state or had deteriorated at 60 days were 4 times more likely to be institutionalized. The use of health states is a novel approach to risk prediction and adds to the CVW as a contemporary model of care. This assisted in stratifying groups that were at lower and higher risk in a multi-morbid frail population. This determined the likelihood of remaining at home or requiring institutional care supported by a selection of risk screening tools. Development of risk predictive models in high risk populations has been criticized as often fail to characterize risk correctly.44 Measuring health states offers an additional approach to determine the effectiveness of care and predict the outcome.
Limitations
This study has several limitations, that are noteworthy including lack of a comparison group to investigate potential differences. This includes risk stratification processes, interventions and outcomes between those admitted to the CVW, versus those receiving standard care in the community. As such, comparisons between groups and impact of CVW is limited to observations seen in a single subpopulation of a severely frail cohort. Nevertheless, repeated measures of overtime within the sample did demonstrate changes within a high-risk group. This allowed for differences to be compared within the study sample to differentiate classes of lower and higher risk in a population with advanced levels of frailty.
Conclusion
We identified that a CVW case management model has the potential to support a frail older population at home delaying and/or reversing the downward trajectories observed in more advanced levels of frailty. This includes progression within health states from unstable to stable following interventions within a CVW programme of care. Patients achieving stability at 30 days maintaining this up to 60 days experienced better outcomes (remaining at home). By contrast, those remaining in an unstable state or deteriorating despite high-intensity levels of service input more likely to be institutionalized or at risk of higher mortality rates. Further studies are required to test this approach to care in the community.
Acknowledgments
The researchers would like to thank the Nursing and Midwifery Planning and Development Unit in North Dublin, the School of Nursing and Midwifery, Royal College of Surgeons Ireland and the Chief Nurse’s Office Department of Health Ireland (An Roinn Slainte). This paper was presented at the International Federation of Ageing 14th Global Conference 2018 held in Toronto, Canada and Royal College of Physicians Ireland, Transforming Care for Older Persons 2019 held in Dublin Ireland.
Disclosure
The authors report no conflicts of interest in this work.
References
1. WHO. Global Health and Aging World Health Organisation. National Institute on Aging and Health; 2010. 1–32.
2. Rechel B, Grundy E, Robine JM, et al. Ageing in the European Union. Lancet (London, England). 2013;381(9874):1312–1322. doi:10.1016/s0140-6736(12)62087-x
3. Small C, Spooner L, Costello M, et al. 147 Frailty in an emergency department: predictors and point prevalence of frailty and pre-frailty in an irish cohort. Age Ageing. 2016;45(suppl 2):ii1–ii12. doi:10.1093/ageing/afw159.28
4. O’Caoimh R, Gao Y, Svendrovski A, et al. The risk instrument for screening in the community (RISC): a new instrument for predicting risk of adverse outcomes in community dwelling older adults. BMC Geriatr. 2015;15(1):92. doi:10.1186/s12877-015-0095-z
5. Lewis C, Moore Z, Doyle F, et al. A community virtual ward model to support older persons with complex health care and social care needs. Clin Interv Aging. 2017;12:985–993. doi:10.2147/CIA.S130876
6. Lewis G, Georghiou T, Steventon A, et al. Impact of virtual wards on hospital use: a research study using propensity matched controls and a cost analysis. National institute for health research service delivery and organisation programme. 2013: 1–157. Report.
7. Leung DYP, Lee DTF, Lee IFK, et al. The effect of a virtual ward program on emergency services utilization and quality of life in frail elderly patients after discharge: a pilot study. Clin Interv Aging. 2015;10:413–420. doi:10.2147/CIA.S68937
8. HSE. National Clinical Care Programme for Older People: Specialist Geriatric Services Model of Care. Health Service Executive & Royal College of Surgeons Ireland; 2012.
9. Kennelly S, Fitzgerald M, O’Shea D. Making a Start in Integrated Care for Older Persons: A Practical Guide to Local Implementation of Integrated Care for Older Persons. Health Service Executive; 2017:1–72.
10. Oireachtas. The future of healthcare report. Sláintecare report Dublin. 2017: 1–192.
11. Oireachtas. Assisted decision making (capacity) act; 2015. Available from: oireachtas.ie/en/bills/bill/2013/83/.
12. Bulecheck GM, Butcher HK, Dochterman JM. Nursing Interventions Classification.
13. Sonnenberg FA, Beck JR. Markov models in medical decision making: a practical guide. Med Decis Making. 1993;13(4):322–338. doi:10.1177/0272989x9301300409
14. Halm EA, Fine MJ, Marrie TJ, et al. Time to clinical stability in patients hospitalized with community-acquired pneumonia: implications for practice guidelines. JAMA. 1998;279(18):1452–1457. doi:10.1001/jama.279.18.1452
15. Aliberti S, Zanaboni AM, Wiemken T, et al. Criteria for clinical stability in hospitalised patients with community-acquired pneumonia. Eur Respir J. 2013;42(3):742. doi:10.1183/09031936.00100812
16. Poulos CJ, Magee C, Bashford G, et al. Determining level of care appropriateness in the patient journey from acute care to rehabilitation. BMC Health Serv Res. 2011;11(1):291. doi:10.1186/1472-6963-11-291
17. Rockwood K, Song X, MacKnight C, et al. A global clinical measure of fitness and frailty in elderly people. Can Med Assoc J. 2005;173(5):489–493. doi:10.1503/cmaj.050051
18. Pavlou MP, Lachs MS. Self-neglect in older adults: a primer for clinicians. J Gen Intern Med. 2008;23(11):1841–1846. doi:10.1007/s11606-008-0717-7
19. Turner A, Hochschild A, Burnett J, et al. High prevalence of medication non-adherence in a sample of community-dwelling older adults with adult protective services-validated self-neglect. Drugs Aging. 2012;29(9):741–749. doi:10.1007/s40266-012-0007-2.
20. Podsiadlo D, Richardson S. The timed “up & go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–148. doi:10.1111/j.1532-5415.1991.tb01616.x
21. Mahoney FI, Barthel DW. Functional evaluation: the barthel index. Md State Med J. 1965;14:61–65.
22. Chaloner DM, Franks PJ. Validity of the walsall community pressure sore risk calculator. Br J Community Nurs. 2000;5(6):266–270 263p. doi:10.12968/bjcn.2000.5.6.7395
23. Cawood A, Elia M, Sharp S, et al. Malnutrition self-screening by using MUST in hospital outpatients: validity, reliability, and ease of use. Am J Clin Nutr. 2012;96(5):1000–1007.
24. Galea M, Woodward M. Mini-mental state examination (MMSE). Aust J Physiother. 2005;51(3):198. doi:10.1016/S0004-9514(05)70034-9
25. Korner A, Lauritzen L, Abelskov K, et al. The geriatric depression scale and the cornell scale for depression in dementia. a validity study. Nord J Psychiatry. 2006;60(5):360–364. doi:10.1080/08039480600937066
26. Salvi F, Morichi V, Grilli A, et al. Screening for frailty in elderly emergency department patients by using the identification of seniors at risk (ISAR). J Nutr Health Aging. 2012;16(4):313–318. doi:10.1007/s12603-011-0155-9
27. Rockwood K, Mitnitski A. Frailty defined by deficit accumulation and geriatric medicine defined by frailty. Clin Geriatr Med. 2011;27(1):17–26. doi:10.1016/j.cger.2010.08.008
28. Kahlon S, Pederson J, Majumdar SR, et al. Association between frailty and 30-day outcomes after discharge from hospital. CMAJ. 2015;187(11):799–804. doi:10.1503/cmaj.150100
29. Austin SR, Wong Y-N, Uzzo RG, et al. Why summary comorbidity measures such as the charlson comorbidity index and elixhauser score work. Med Care. 2015;53(9):e65–e72. doi:10.1097/MLR.0b013e318297429c
30. Hussey P, Sorbero M, Mehrotra A, et al. Using episodes of care as a basis for performance measurement and payment: moving from concept to practice. Health Aff (Project Hope). 2009;28(5):1406–1417. doi:10.1377/hlthaff.28.5.1406
31. Silverstein MD, Qin H, Mercer SQ, et al. Risk factors for 30-day hospital readmission in patients ≥65 years of age. Proc (Bayl Univ Med Cent). 2008;21(4):363–372. doi:10.1080/08998280.2008.11928429
32. Dhalla IA, O’Brien T, Moora D, et al. Effect of postdischarge virtual ward on readmission or death for high-risk patients: a randomized clinical trail. JAMA. 2014;312(13):1305–1312. doi:10.1001/jama.2014.11492
33. Torner N, Izquierdo C, Soldevila N, et al. Factors associated with 30-day mortality in elderly inpatients with community acquired pneumonia during 2 influenza seasons. Hum Vaccin Immunother. 2017;13(2):450–455. doi:10.1080/21645515.2017.1264782
34. Field A. Discovering Statistics Using IBM SPSS.
35. Weathers E, O’Caoimh R, O’Sullivan R, et al. The inter-rater reliability of the risk instrument for screening in the community. Br J Community Nurs. 2016;21(9):469–475. doi:10.12968/bjcn.2016.21.9.469
36. Dong X. Elder self-neglect: research and practice. Clin Interv Aging. 2017;12:949–954. doi:10.2147/CIA.S103359
37. Kojima G. Frailty as a predictor of future falls among community-dwelling older people: a systematic review and meta-analysis. J Am Med Dir Assoc. 2015;16(12):1027–1033 1027p. doi:10.1016/j.jamda.2015.06.018
38. Nikolaus T, Bach M. Preventing falls in community-dwelling frail older people using a home intervention team (HIT): results from the randomized falls-HIT trial. J Am Geriatr Soc. 2003;51(3):300–305. doi:10.1046/j.1532-5415.2003.51102.x
39. Marengoni A, Nobili A, Romano V, et al. Adverse clinical events and mortality during hospitalization and 3 months after discharge in cognitively impaired elderly patients. J Gerontol a Biol Sci Med Sci. 2013;68(4):419–425. doi:10.1093/gerona/gls181
40. Krogseth M, Wyller TB, Engedal K, et al. Delirium is a risk factor for institutionalization and functional decline in older hip fracture patients. J Psychosom Res. 2014;76(1):68–74. doi:10.1016/j.jpsychores.2013.10.006
41. Shi J, Yang Z, Song X, et al. Sex differences in the limit to deficit accumulation in late middle-aged and older chinese people: results from the beijing longitudinal study of aging. J Gerontol a Biol Sci Med Sci. 2014;69(6):702–709. doi:10.1093/gerona/glt143
42. Trevisan C, Veronese N, Maggi S, et al. Factors influencing transitions between frailty states in elderly adults: the progetto veneto anziani longitudinal study. J Am Geriatr Soc. 2017;65(1):179–184. doi:10.1111/jgs.14515
43. Hendry A, Vanhecke E, Samaniego LL, et al. Models of care for frailty: a systematic review advantage. EU Health Programme. 2017;2014–2020:1–21.
44. Aven T. Improving risk characterisations in practical situations by highlighting knowledge aspects, with applications to risk matrices. Reliab Eng Syst Safety. 2017;167:42–48. doi:10.1016/j.ress.2017.05.006
45. Hassler AP, Menasalvas E, García-García FJ, et al. Importance of medical data preprocessing in predictive modeling and risk factor discovery for the frailty syndrome. BMC Med Inform Decis Mak. 2019;19(1):33. doi:10.1186/s12911-019-074
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
