Back to Archived Journals » Research and Reports in Endocrine Disorders » Volume 5
Prevalence of 25-hydroxyvitamin D deficiency in healthy personnel from an academic institution of an urban area in Costa Rica
Authors Gamboa-Gamboa T, Abarca-Soto G, José G Jiménez-Montero
Received 13 June 2015
Accepted for publication 23 August 2015
Published 12 October 2015 Volume 2015:5 Pages 135—140
DOI https://doi.org/10.2147/RRED.S90435
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Mingzhao Xing
Tatiana Gamboa-Gamboa,1 Gabriel Abarca-Soto,2 José G Jiménez-Montero3,4
1Department of Research and Nutrition, Universidad de Ciencias Médicas, San José, Costa Rica; 2Department of Research, School of Medicine, Universidad de Ciencias Médicas, San José, Costa Rica; 3Department of Postgraduate Studies, Universidad de Ciencias Médicas, San José, Costa Rica; 4Department of Endocrinology, Hospital CIMA, San José, Costa Rica
Objective: The aim of this study was to determine 25-hydroxyvitamin D concentrations in healthy employees of the Universidad de Ciencias Médicas, Costa Rica.
Methods: Levels of 25-hydroxyvitamin D, calcium, phosphorus, intact parathyroid hormone (iPTH), and creatinine were measured in 80 people. Solar ultraviolet radiation exposure and 25-hydroxyvitamin D intake were estimated using a previously designed questionnaire. Participants were 52 women aged (mean ± standard deviation) 35.8±10.0 years old, body mass index of 27.1±5.9 kg/m2, and 26 men aged 36.4±10.8 years old, body mass index of 27.5±5.0 kg/m2.
Results: All participants were normocalcemic, eight females were postmenopausal, three were hypertensive; none had renal, gastrointestinal, or thyroid disease. The level of 25-hydroxyvitamin D was 23.9±7.0 ng/dL and iPTH 40.1±17.5 pg/dL. A level of 25-hydroxyvitamin D $30 ng/dL was seen in 17% of the population. The eight participants with iPTH higher than 67 ng/dL, had 25-hydroxyvitamin D of 18.9±4.8 ng/dL. Two participants who received 25-hydroxyvitamin D and calcium supplements were excluded.
Conclusion: The 25-hydroxyvitamin D insufficiency and deficiency found in healthy employees from an academic center in Costa Rica may be due to working long hours in-doors and solar ultraviolet radiation exposure. It is unknown whether secondary hyperparathyroidism seen in nearly 10% of this population, may have long-term effects on bone health.
Keywords: vitamin D deficiency, osteoporosis, secondary hyperparathyroidism, bone metabolism
Introduction
Vitamin D plays a fundamental role in bone health due to its effects on calcium absorption.1–3 Inadequate concentrations of 25-hydroxyvitamin D are associated with an increased bone turnover and osteoporosis.4,5 This condition has been linked to alterations in neuromuscular function, increasing the risk of falls.6,7 Moreover, it has been reported that low levels of 25-hydroxyvitamin D are related to an increased risk of diabetes, hyperlipidemia, cardiovascular disease,8,9 and asthma.10
The prevalence of 25-hydroxyvitamin D deficiency has become a worldwide health problem.11,12 In recent years, in the United States the prevalence of 25-hydroxyvitamin D deficiency has doubled13,14 and studies from some Latin American countries, have shown a high prevalence of 25-hydroxyvitamin D deficiency in postmenopausal women with osteoporosis.15,16 In Central America, however, little is known about the prevalence of 25-hydroxyvitamin D deficiency.
This prompted us to perform an exploratory investigation in a tropical country located in Central America, aimed to determine 25-hydroxyvitamin D concentrations and examine its relationship to solar ultraviolet radiation exposure and dietary 25-hydroxyvitamin D intake in a group of apparently healthy personnel from Universidad de Ciencias Médicas (UCIMED), and academic institution located in San José, Costa Rica. Additionally, we evaluated the relationship between 25-hydroxyvitamin D and intact parathyroid hormone (iPTH) concentration. It is expected that this pilot study will support evidence to perform future investigations in a larger population in this country.
Methods
From 130 healthy staff members of the UCIMED, 100 were randomly selected and 80 of them agreed to participate in the study; two were excluded from the analysis because they took vitamin D and calcium supplements. All the participants signed an informed consent, underwent a medical history and physical examination, which included measuring blood pressure, body weight, and height. Body mass index (kg/m2) was calculated for all the participants. Solar ultraviolet radiation exposure, and 25-hydroxyvitamin D intake were evaluated by applying a designed questionnaire previously tested. The time in minutes of solar ultraviolet radiation exposure during weekdays and weekends, the use sunscreen, and skin type of each participant were evaluated. The skin type was classified using the skin scale; this scale used the constitutional color and the results of exposure to ultraviolet radiation to indicate the skin type.17 Additionally, we inquired about the consumption of milk and vitamin supplements to estimate the intake of 25-hydroxyvitamin D.
Fasting venous blood sample was obtained to measure serum calcium, phosphorus, and creatinine concentrations (480 Beckman Coulter, Brea, CA, USA); 25-hydroxyvitamin D was determined using Architect Automatic equipment (Abbott Laboratories, Abbott Park, IL, USA [coefficient of variation of 4.5%]). iPTH (normal range 11–67 pg/mL) was determined by chemiluminescence (IMMULITE 2000 DPC, [coefficient of variation 7%]). Venous blood was spun and serum was frozen until analysis. All the determinations were done in the same run. We defined 25-hydroxyvitamin D deficiency as serum 25-hydroxyvitamin D level <20.0 ng/mL, and insufficiency as 25-hydroxyvitamin D levels between 20 and 29.9 ng/mL.1 This study was conducted during rainy season (August and September) in Costa Rica; this country is located in North latitude 11°13′12″ and South latitude 08°, 102′, 26″.6 Results are expressed as mean ± standard deviation. Student’s t-test and analysis of variance were used to compare means; Fisher’s exact test was used to analyze the independence of sex and ultraviolet sun radiation vs vitamin D status, defined as vitamin D ≥30 ng/dL and ≤29.9 ng/dL. Also, logistic regressions, using single independent variables, were employed to evaluate the effect of sex and ultraviolet sun radiation exposure during weekdays and weekends using vitamin D status as dependent variable. The Scientific Ethics Committee of UCIMED approved this study.
Results
The clinical characteristics and biochemical variables of the study population with an age range of 18–60 years old are shown in Table 1. Thirty-five percent had normal body weight, while 40% and 22.5% were overweight and obese, respectively. All had normal calcium, phosphorous, and creatinine concentrations. Table 2 illustrates the skin type distribution and the use of sunscreen in each photo type group. Twenty-two participants (19 females and three males) utilized sunscreen, (27.5% of the study population). No associations were found between 25-hydroxyvitamin D concentrations, skin photo types, and the use of sunscreen, or adiposity.
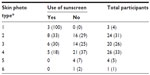  | Table 2 Skin type distribution and use of sunscreen in the study population in each skin photo type category |
During weekdays individuals’ solar ultraviolet radiation exposure was limited to the early morning or late afternoon hours (between 6 and 7 am, and between 4 and 5 pm). The 25-hydroxyl-vitamin D concentrations were higher in males than in females (P=0.031) as shown in Table 1. The duration of solar ultraviolet radiation exposure, (less than 5 minutes vs more than 5 minutes during weekdays and weekends) and 25-hydroxyvitamin D concentrations are illustrated in Table 3. Moreover, the Fisher’s exact test yielded a significant association only between vitamin D status and ultraviolet sun radiation during weekends (P=0.0221). Similarly, the logistic analysis demonstrated a significant association of vitamin D status and weekend ultraviolet sun radiation (P=0.0164), with an odds ratio of 0.24 (confidence interval 95%: 0.075–0.769).
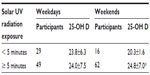  | Table 3 Solar ultraviolet (UV) exposure and 25-hydroxyvitamin D (25-OH D) |
Fifteen participants drank at least one glass of milk per day; each glass contains 1.25 μg of 25-hydroxyvitamin D, corresponding to 50 U of this vitamin, thus the impact of vitamin D intake on 25-hydroxyvitamin D concentrations was insignificant.
Table 4 illustrates the prevalence of sufficiency, insufficiency, and deficiency of 25-hydroxyvitamin D in the study population. A 25-hydroxyvitamin D ≥30 ng/dL concentration was seen in 11% of females and 27% of males, respectively. As compared to participants with normal body mass index, overweight and obese individuals had lower 25-hydroxyvitamin D concentrations, but the differences were not significant (data not shown). As shown in Figure 1, an inverse relation between 25-hydroxyvitamin D and iPTH was observed. Four individuals with 25-hydroxyvitamin D below 20 ng/mL and four with 25-hydroxyvitamin D lower than 25 ng/dL had iPTH of 74.1±4.6 ng/mL (normal range 11–67 pg/mL), concordant with secondary hyperparathyroidism. As shown in Figure 2, higher iPTH concentrations were seen in those individuals with 25-hydroxyvitamin D deficiency compared to those with 25-hydroxyvitamin D higher than 30 ng/dL (P=0.037).
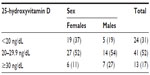  | Table 4 25-hydroxyvitamin D in males and females |
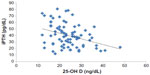  | Figure 1 Inverse relationship between 25-hydroxyvitamin D and intact parathyroid hormone (iPTH) concentrations. |
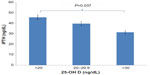  | Figure 2 Higher mean intact parathyroid hormone (iPTH) concentrations and 25-hydroxyvitamin D deficiency. |
Discussion
This study evaluated the concentration of 25-hydroxyvitamin D in a small sample of an apparently healthy population without evidence of kidney disease as creatinine concentrations were within normal range, who live in the Central Valley in San José, Costa Rica. The participants reported low dietary intake of fortified milk with 25-hydroxyvitamin D, and had low solar ultraviolet radiation exposure.
The cumulative prevalence of 25-hydroxyvitamin D insufficiency and deficiency was striking and unexpectedly high as seen in Table 4. It was believed that 25-hydroxyvitamin D deficiency was more common in countries far from the equator. However, a number of recent reports have shown that this was not the case.12,13
In the United States, the prevalence of 25-hydroxyvitamin D deficiency has doubled, attaining figures of 41.6% in the whole population. In Latinos living in the United States, 25-hydroxyvitamin D deficiency reaches up to 69.2%.11,12 Of note, studies conducted in Latin America, in osteoporotic postmenopausal women demonstrated 25-hydroxyvitamin D deficiency in 67%, 50%, and 42% of the subjects, respectively.4,15,16 This study was performed during the rainy season in Costa Rica and found a high prevalence of 25-hydroxyvitamin D insufficiency and deficiency despite the fact that this country is located in North latitude 11°13′12″ and South latitude 08°, 102′, 26″.6 In this region there is only a dry and a rainy season. All throughout the year there is sunlight but during this particular period of the year it rains in the afternoon. This study demonstrated that individuals’ sun exposure was limited to the early morning or late afternoon hours. Factors associated with 25-hydroxyvitamin D production include incident angle of the sun, season, latitude, time of the day, skin photo type, people older than 65 years old, and the use of sunscreen.13,17–20 In this investigation, 27% of the population used sunscreen, particularly individuals with fair skin and women, a factor which could contribute to a reduction of 25-hydroxyvitamin D synthesis. Higher 25-hydroxyvitamin D concentrations were seen in males as compared to females. This may be associated to a lower ultraviolet sun radiation in females. Our study did not demonstrate any effect of the use of sunscreen or weekdays’ solar ultraviolet radiation exposure on vitamin D concentrations. Nonetheless, weekends’ solar ultraviolet radiation exposure did have an impact on 25-hydroxyvitamin D concentrations and, the risk to develop vitamin D insufficiency/deficiency for individuals who had ultraviolet sun radiation for more than 5 minutes during weekends was 24% of the risk for individuals who had less than 5 minutes exposure on weekends. Overall, the high prevalence of 25-hydroxyvitamin D insufficiency/deficiency could be explained by the duration of ultraviolet sun radiation exposure, particularly during weekends and, the incident angle of the sun, as it occurred in early morning hours or late in the afternoon.
Low 25-hydroxyvitamin D concentrations have been reported in overweight and obese individuals.21 The mechanisms by which excess of adipose tissue reduces 25-hydroxyvitamin D could be linked to storage of this sterol in the expanded adipose mass, or to a lower 25-hydroxyvitamin D binding globulin.22,23 In this report, the normal weight participants had higher 25-hydroxyvitamin D levels than the overweight and obese participants, although the difference was not significant, likely due to the small sample size.
We observed an inverse relationship between serum 25-hydroxyvitamin D and iPTH as previously shown24,25 and found that nearly 10% of the participants had high iPTH concentrations. Secondary hyperparathyroidism may occur in individuals with kidney disease, with gastrointestinal disorders including celiac disease and after parathyroidectomy, due to inadequate 25-hydroxyvitamin D concentrations.26–28 Secondary hyperparathyroidism associated with 25-hydroxyvitamin D deficiency is commonly seen in elderly and institutionalized individuals,29,30 in subjects with low body weight, with a history of falls and fractures, and with 25-hydroxyvitamin D deficiency.6 Since all the participants of our study had normal renal function, and none had gastrointestinal disease, it is likely that the cause of elevated iPTH levels were due to 25-hydroxyvitamin D insufficiency/deficiency. The health implications of 25-hydroxyvitamin D insufficiency/deficiency and secondary hyperparathyroidism observed in this study are not known. The results raises concerns about long-term effects of low vitamin D levels on bone health, as the participants of the study were of young age. Whether this condition would predispose to early bone loss, particularly in women is not clear. Furthermore, low 25-hydroxyvitamin D may increase the risk of cardiovascular disease as shown in recent studies.8,9.
There were some limitations in this study. For example, we did not provide 25-hydroxyvitamin D supplementation to those participants with 25-hydroxyvitamin D concentrations below 30 ng/mL to determine if replacement therapy would reduce iPTH.30 Likewise, it was not possible to rule out normocalcemic primary hyperparathyroidism. However, the latter condition is uncommon and follow-up evaluation is required to confirm this diagnosis.
The high prevalence of 25-hydroxyvitamin D concentrations below 30 ng/dL associated with secondary hyperparathyroidism needs to be documented during other months of the year. The findings of this study were unexpected because the participants live in a region with abundant exposure to sunlight, the main natural source of 25-hydroxyvitamin D production.18–20 If our findings were confirmed, the deficit of 25-hydroxyvitamin D would be identified as a public health problem in Costa Rica.
In conclusion, changes in lifestyle, long working hours, low solar ultraviolet radiation exposure and potentially, the use of sunscreen could explain the high prevalence of insufficiency and deficiency of 25-hydroxyvitamin D levels in this population. These results are worrisome as this condition could impact bone health promoting osteopenia and osteoporosis later in life31 and may increase cardiovascular risk.8,9 Whether dietary and vitamin D supplementation has beneficial effects on bone health or on diabetes prevention is unclear. As recently shown, this approach has no effects on osteoporosis, fracture risk32 or on glucose homeostasis and diabetes prevention.33 However, from a public health approach, healthy solar ultraviolet radiation exposure of at least 10 minutes daily along with physical activity and vitamin D supplementation, could be recommended in office workers and homebound citizens with severe 25-hydroxyvitamin D deficiency. This recommendation clearly has to be balanced in order to prevent skin cancer.
Acknowledgments
The authors thank Lic Kathya Arrieta-Morera and Dr Jorge Camacho for their contribution in literature search and in statistical analysis, respectively.
Disclosure
JG Jimenez-Montero has been on the insulin advisory board, received a research grant from Sanofi-Aventis and has been speaker for Merck Sharp and Dohme, and Novartis. The other authors have no conflict of interest to disclose.
References
Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, Treatment, and Prevention of Vitamin D Deficiency: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2011;96(7):1911–1930. | |
Holick MF. High Prevalence of Vitamin D Inadequacy and Implications for Health. Review. Mayo Clin Proc. 2006;81(3):353–373. | |
Lips P. Vitamin D physiology. Prog Biophys Mol Biol. 2006;92(1):4–8. | |
Mithal A, Wahl DA, Bonjour JP, et al. Global vitamin D status and determinants of hypovitaminosis D. Osteoporos Int. 2009;20(11):1807–1820. | |
Burgaz A, Akersson A, Oster A, Michaelsson K, Wolk A. Association of diet, supplement use, and ultraviolet B radiation exposure with vitamin D status in Swedish women during winter. Am J Clin Nutr. 2007;86(5):1399–1404. | |
Chen-Ku C, Jiménez N, Ulate L. Hipovitaminosis D en Costa Rica Estudio de casos y controles [Hypovitaminosis D in Costa Rica, case control study]. Acta Médica Costarricense. 2012;54:146–151. Spanish. | |
Bischoff HA, Dawson B, Willett WC, et al. Effect of Vitamin D on Falls: A Meta-Analysis. JAMA. 2004;291(16):1999–2066. | |
Chen WR, Chen YD, Shi Y, Yin D, Wang H, Sha Y. Vitamin D, parathyroid hormone and risk factors for coronary artery disease in an elderly Chinese population. J Cardiovasc Med (Hagerstown). 2015;16(1):59–68. | |
Durup D, Jørgensen HL, Christensen J, et al. A Reverse J-Shaped Association Between Serum 25-Hydroxyvitamin D and Cardiovascular Disease Mortality: The CopD Study. Clin Endocrinol Metab. 2015;100(6):2339–2346. | |
Brehm JM, Celedón JC, Soto ME, et al. Serum Vitamin D Levels and Markers of Severity of Childhood Asthma in Costa Rica. Am J Respir Crit Care Med. 2009;179(9):765–771. | |
Sociedad Española de Investigación ósea y del Metabolismo Mineral y Sociedades Afines. Documento de posición sobre las necesidades y niveles óptimos de vitamina D [Position paper of the requirements and optimal levels of vitamin D]. Rev Osteoporos Metab Miner. 2011;3:53–64. Spanish. | |
Holick MF, Chen TC. Vitamin D deficiency: a worldwide problem with health consequences. Am J Clin Nutr. 2008;87(4):1080–1086. | |
Forrest KY, Stuhldreher WL. Prevalence and correlates of vitamin D deficiency in US adults. Nutr Res. 2011;31(1):48–54. | |
Engelman C. Vitamin D Recommendations: The Saga Continues. J Clin Endocrinol Metab. 2011;96(10):3065–3066. | |
González G, Alvarado JN, Rojas A, Navarrete C, Velásquez CG, Arteaga E. High prevalence of vitamin D deficiency in Chilean healthy postmenopausal women with normal sun exposure: additional evidence for a worldwide concern. Menopause. 2007;14(3 Pt 1):455–461. | |
Lips P, Hosking D, Lippuner K, et al. The prevalence of vitamin D inadequacy amongst women with osteoporosis: an international epidemiological investigation. J Intern Med. 2007;260(3):245–254. | |
Sachdeva S. Fitzpatrick skin typing: application in dermatology. Indian J Dermalog Venereol Leprol. 2009;75(1):93–97. | |
Holick MF. Vitamin D Deficiency. N Engl J Med. 2007;357(3):266–281. | |
Holick MF. Vitamin D and health: Evolution, biologic functions, and recommended dietary intakes for vitamin D. Clin Rev Bone Miner Metab. 2009;7(1):2–19. | |
Wacker M, Holick MF. Vitamin D-effects on skeletal and extraskeletal health and the need for supplementation. Nutrients. 2013;5(1):111–148. | |
Earthman CP, Beckman LM, Masodkar K, Sibley SD. The link between obesity and low circulating 25-hydroxyvitamin D concentrations: considerations and implications. Int J Obes (Lond). 2012;36(3):387–396. | |
Konradsen A, Lindberg F, Hexeberg S, Jorde R. Serum 1,25-dihydroxy vitamin D is inversely associated with body mass index. Eur J Nutr. 2008;47(2):87–91. | |
Wortsman J, Matsuoka LY, Chen TC, Lu Z, Holick MF. Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr. 2000;72(3):690–693. | |
Karaguzel G, Dilber B, Can G, Okten ADO, Holick MF. Seasonal Vitamin D Status of Healthy Schoolchildren and Predictors of Low Vitamin D Status. J Pediatr Gastroenterol Nutr. 2014;58(5):654–660. | |
Adams J, Hewison M. Update in Vitamin D. J Clin Endocrinol Metab. 2010;95(2):471–478. | |
Jimenez JG, Lobo E, Picado A, Molina MA. Secondary hyperparathyroidism after removal of a parathyroid adenoma. Endocr Pract. 2002;8(6):429–432. | |
Jiménez J, Rosabal A. Inadequate vitamin D levels in an osteoporotic woman with celiac Disease. Annual Meeting and Scientific Congress of American Association of Clinical Endocrinology; 21 April 2010, Boston, MA, USA. | |
Saliba W, Barnett O, Rennert HS, Lavi I, Rennert G. The relationship between serum 25(OH) D and parathyroid hormone levels. Am J Med. 2011;124(12):2014–2136. | |
Thomas MK, Demay MB. Vitamin D deficiency and disorders of vitamin D metabolism. Endocrinol Metab Clin North Am. 2000;29(3):611–627. | |
Chapuy MC, Arlot ME, Duboeuf F, et al. Vitamin D3 and Calcium to Prevent Hip Fractures in Elderly Women. N Engl J Med. 1992; 327(23):1637–1642. | |
Dawson B, Harris SS, Krall EA, Dallal GE. Effect of calcium and vitamin D supplementation on bone density in men and women 65 years of age or older. N Engl J Med. 1997;337(10):670–676. | |
Snellman G, Byberg L, Lemming EW, et al. Long-term dietary vitamin D intake and risk of fracture and osteoporosis: a longitudinal cohort study of Swedish middle-aged and elderly women. J Clin Endocrinol Metab. 2014;99(3):781–790. | |
Seida JC, Miltri J, Colmers IN, et al. Effect of vitamin D3 supplementation on improving glucose homeostasis and preventing diabetes: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2014;99(10):2014–2136. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

