Back to Journals » Clinical Interventions in Aging » Volume 15
Prediction of Early Postoperative Major Cardiac Events and In-Hospital Mortality in Elderly Hip Fracture Patients: The Role of Different Types of Preoperative Cardiac Abnormalities on Echocardiography Report
Authors Chen X, Ma Y, Deng Z, Li Q, Liao J, Zheng Q
Received 20 February 2020
Accepted for publication 11 May 2020
Published 27 May 2020 Volume 2020:15 Pages 755—762
DOI https://doi.org/10.2147/CIA.S250620
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Zhi-Ying Wu
Xuepan Chen,1,2,* Yuanchen Ma,1,* Zhantao Deng,1 Qingtian Li,1 JunXing Liao,1 Qiujian Zheng1
1Department of Orthopedics, Guangdong Provincial People’s Hospital, Guangdong Academy of Medical Sciences;School of Medicine, South China University of Technology, Guangzhou, People’s Republic of China; 2Shantou University Medical College, Shantou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Qiujian Zheng
Department of Orthopedics, Guangdong Provincial People’s Hospital, Guangdong Academy of Medical Sciences, School of Medicine, South China University of Technology, No. 106, Zhongshan Second Road, Yuexiu District, Guangzhou 510000, People’s Republic of China
Email [email protected]
Introduction: Transthoracic echocardiography (TTE) is a common cardiac screening test before hip fracture surgery. However, the general TTE test delays surgery, so it would be meaningful if we could simplify the TTE by only assessing cardiac abnormality specifically. Therefore, we aimed to establish the most clinically relevant abnormality by comparing the predictive value of each major cardiac abnormality in postoperative cardiac complications and mortality in elderly hip fracture patients.
Patients and Methods: From January 2014 to January 2019, the medical records of all surgically treated elderly patients (> 65 years) with hip fracture were analyzed. The major TTE abnormalities were defined as left ventricular hypertrophy, systolic pulmonary arterial pressure > 25 mm Hg, moderate-severe valve abnormality, left ventricular ejection fraction (LVEF) < 50%, and pericardial effusion. The outcomes were postoperative cardiac complications and in-hospital mortality.
Results: There were 354 patients involved finally. Postoperative cardiac complications were encountered in 7.6% (n=27) of patients. The mortality rate was 2.8% (n=10). History of coronary artery disease (CAD) (OR: 3.281, 95% CI: 1.332– 8.079, p=0.010) and presence of aortic stenosis (AS) (OR:5.656, 95% CI: 1.869– 17.117, p=0.002) were independent predictors of postoperative cardiac complications. In addition, age (OR: 1.264, 95% CI: 1.047– 1.527, p=0.015), history of CAD (OR: 19.290, 95% CI: 2.002– 185.885, p=0.010), presence of AS (OR:7.164, 95% CI: 1.988– 51.413, p=0.040) and LVEF < 50% (OR:8.803, 95% CI: 1.115– 69.472, p=0.039) were independent predictors of mortality. However, the rest of preoperative TTE abnormalities were not associated with postoperative cardiac complications or mortality.
Conclusion: Among the TTE abnormalities presented by elderly patients with hip fracture, moderate-severe AS was the predictor of postoperative cardiac complications. Moreover, moderate-severe AS and LVEF < 50% were the predictors of in-hospital mortality. Therefore, we could simplify the TTE process by assessing aortic valve and LVEF specifically on focused echocardiography, which could avoid surgery delay.
Keywords: aging, hip fracture surgery, mortality, postoperative cardiac complications, echocardiographic abnormality
Introduction
Hip fracture is the major reason for hospital admission in elderly patients and is becoming the most important public health issue. With constantly increasing incidence, it is estimated to increase to 6.3 million worldwide by the year 2050.1 Despite advances in surgical technique, the surgery is still associated with high mortality rate and frequent postoperative cardiac complications in elderly patients with hip fracture.2 The mortality rate was reported as high as 4–12% during hospitalization and 10–40% within the first postoperative year.3–5 Moreover, the postoperative cardiac complications were the most fearsome perioperative complications that account for morbidity and mortality in elderly hip fracture.6,7 Therefore, early identification of patients at risk for postoperative cardiac complications is crucial, which promotes early preventive medical intervention. To date, several studies have discovered the predictors of postoperative cardiac complications in elderly hip fracture, including cardiac biomarkers,6,8 Cardiac Risk Index,9 and C-reactive protein.10 However, to the best of our knowledge, the association between different types of preoperative echocardiographic abnormalities and postoperative cardiac complications in elderly patients following hip fracture surgery has not been studied yet.
Preoperative transthoracic echocardiography (TTE) is frequently considered in elderly patients with hip fracture, because it is a reliable tool to assess cardiac structural and functional abnormality.11 So far, only few studies have shown preoperative TTE abnormality as the predictor of postoperative complications and mortality after hip fracture, including mild pericardial effusion,12 aortic stenosis (AS).13,14 However, available studies mainly focused on the association between the preoperative TTE abnormality and postoperative complications rather than cardiac complications specifically.12 In addition, the conclusion of the previous study was still controversial.13,14 Furthermore, previous studies mainly focused on one type of preoperative TTE abnormality rather than comprehensively evaluating multiple TTE abnormalities at the same time.12–14
Therefore, we conducted this study to evaluate the predictive value of different types of cardiac abnormalities, evaluated with preoperative TTE, in cardiac complications and in-hospital mortality in elderly patients after hip fracture surgery.
Patients and Methods
Study Design
The study was based on data collected from January 2014 to January 2019 in a large tertiary hospital. The medical records of elderly patients aged over 65 years with hip fracture (femoral neck, intertrochanteric or subtrochanteric) undergoing surgery were retrospectively analyzed. Only patients with a preoperative TTE examination were included in this study. We excluded patients with polytrauma, patients with pathological fractures, patients with periprosthetic fractures, patients with history of malignant tumor, and patients without complete medical records. The current study’s protocol was approved by the Ethics Committee of Guangdong Provincial People’s Hospital, Guangdong Academy of Medical Sciences. (No.GDREC2018522H(R1)). In the process of the study, researchers covered all data confidentiality and compliance with the Declaration of Helsinki. We retrospectively extracted the patients’ impact data without any intervention measures. Thus, patient consent to review their medical records was not required in this retrospective study.
Data Collection
Hospital records were reviewed for age, sex, fracture type, preoperative medical comorbidities, surgery type, American Society of Anesthesiologists (ASA) class, anesthesiologic type, preoperative TTE report, in-hospital postoperative cardiac complications, and in-hospital mortality. The primary study endpoint was in-hospital postoperative cardiac complications. The secondary outcome of interest was in-hospital mortality.
Definition of Postoperative Cardiac Complications
Postoperative cardiac complications were defined as acute myocardial infarction, congestive heart failure, major arrhythmia, or primary cardiac death. Postoperative acute myocardial infarction (AMI) was defined as elevation of myocardial necrosis markers two times above the upper limits of the normal range in patients presenting with specific features (clinical or electrocardiogram signs). Congestive heart failure was diagnosed by means of clinical examination, specific features of chest radiography and elevation of related biomarkers. Cardiac arrhythmia was defined as new onset arrhythmia detected by electrocardiogram, mainly including ventricular tachycardia or atrial fibrillation. Cardiac death was defined as sudden death that could not be explained by any other non-cardiovascular postoperative complications.
Preoperative TTE and Major Abnormality
After the patient was sent to the orthopedic department, a flowchart including medical history, physical examination, electrocardiography, and standard blood tests was done. Usually, patients with the following were recommended to undergo TTE in our clinic according to ACC/AHA guidelines, including dyspnea of unknown origin, worsening of known signs or symptoms of cardiac disease, known history of valvular dysfunction or heart failure without TTE in the last year or worsened symptoms, and suspicion of moderate or greater valvular stenosis or regurgitation.15 But the final decision whether to undergo TTE or not was not fully based on the recommendations but influenced by other factors, including preoperative consultation with anesthesiologist, cardiologist and orthopedic surgeons’ clinical experience. Preoperative TTE was performed using Cardiovascular Ultrasounds System (General Electrics TM, Milwaukee, WI, USA). Standard parasternal and apical two- and four-chamber views were assessed with the patient in the left lateral decubitus position, calculating the diameter of chamber, wall thickness. Left ventricular ejection fraction (LVEF) was calculated using the modified Simpson’s method.16 Transvalvular flow was assessed by early peak (E) and late peak (A) velocities, E/A ratio and deceleration time of E velocity (DTE). Standard echocardiographic evaluation of mitral or aortic valvular disease was assessed similar to previous method.17 The systolic pulmonary artery pressure (PAPS) was estimated using Bernoulli, s formula.18 Space between the visceral and parietal pericardium was assessed through the cardiac cycle.
Major TTE abnormalities were defined as: 1) left ventricular hypertrophy, defined by ratio of posterior wall/septal thickness <1.1; 2) moderate-severe aortic valve stenosis, defined by a mean pressure gradient >40 mmHg and/or an indexed aortic valvular area < 1 cm2m−2; 3) severe mitral valve stenosis, defined by a mean pressure gradient >10 mmHg and/or an indexed mitral valvular area < 1 cm2m−2; 4) Grade III–IV mitral or aortic valvular regurgitation; 5) left ventricle ejection fraction (LVEF) <50%; 6) systolic pulmonary artery pressure (PAPs) >25 mmHg; 7) pericardial effusion.
Statistical Analysis
The Kolmogorov–Smirnov test was carried out to assess the normality of the continuous variables. Continuous variables are expressed as mean ± standard deviation (SD) and compared using Student’s t-test. Categorical variables are expressed as percentages and compared using the Chi-squared test or Fisher’s exact test as appropriate. To identify relationship between preoperative TTE abnormality and postoperative cardiac complications, in-hospital mortality after hip fracture surgery, only variables with P-values <0.05 in the t-test, Chi-squared test or Fisher’s exact test were subjected to multivariate logistic regression model. Variables with statistical significance (p<0.05) retained in the final model were considered as independent risk factors. Odds ratio (OR) and 95% confidence interval (95% CI) were calculated. The calibration of each model was assessed by the Hosmer–Lemeshow goodness-of-fit test, with p>0.05 indicating an acceptable result. Statistical analyses were performed using SPSS 20.0 statistics software (SPSS Inc. Chicago, IL, USA).
Results
Clinical Characteristics
The clinical characteristics of the study population were shown in Table 1. A total of 1052 elderly patients underwent hip fracture surgery in our clinic during the study period. Among them, 399 elderly patients underwent preoperative TTE, of whom 354 (88.7%) were included in the study. Among the excluded patients (n=45), 9 patients presented with polytrauma other than the hip fracture, 15 patients presented with periprosthetic or pathological fractures, 16 patients with malignant tumor history, and 5 patients were without complete medical records. Of the 354 patients included, 270 (76.3%) were female and 84 (23.7%) were male. The mean age of patients was 81.97±6.52 years. Patients with femoral neck fracture accounted for 56.5% of the study population. Proximal femoral nail anti-rotation (PFNA) was the most common type of treatment accounting for 43.5%. Postoperative cardiac complications occurred in 27 (7.6%) cases, 13 cases of acute non-fatal myocardial infarction; 7 cases of new-onset arrhythmia (2 atrial fibrillation, 1 ventricular fibrillation, 4 atrioventricular block), 6 cases of heart failure, 1 case of sudden cardiac death. The in-hospital mortality rate of the included patients was 2.8% (n=10).
 |
Table 1 Clinical Characteristics of the Patients |
As for distribution of preoperative TTE abnormality in elderly patients, 67 cases (18.9%) showed left ventricular hypertrophy, 20 cases (5.6%) had severe AS, 11 cases (3.1%) presented with severe mitral valve stenosis, 12 cases (3.4%) presented with moderate-severe aortic or mitral valve regurgitation, 10 cases (2.8%) demonstrated LVEF <50%, 77 cases (21.8%) presented with PAPs >25mmHg, 15 cases (4.2%) showed pericardial effusion.
Postoperative Cardiac Complications
Patients were divided into 2 groups based on whether there were postoperative cardiac complications or not. The differences between 2 groups were shown in Table 2. There were no statistically significant differences in age, sex, fracture type, treatment type, distribution of ASA class, anesthesiology type. Patients who presented with postoperative cardiac complications had significantly higher prevalence of coronary artery disease (CAD)(44.4% vs 17.1%), higher presence of moderate-severe AS (22.2% vs 4.3%) and LVEF <50% (11.1% vs 2.1%) compared with uncomplicated patients. As shown in the multivariate analysis (Table 3), history of CAD (OR: 3.281, 95% CI: 1.332–8.079, p=0.010), presence of moderate-severe AS (OR:5.656, 95% CI: 1.869–17.117, p=0.002) were the dominant predictors of postoperative cardiac complications. The Hosmer–Lemeshow test showed the good fit (x2=0.376, p=0.540).
 |
Table 2 Comparison of Patients with and Without In-Hospital Postoperative Cardiac Complications |
 |
Table 3 Multivariate Analysis for the Prediction of In-Hospital Postoperative Cardiac Complications |
In-Hospital Mortality
Comparing characteristics in relation to in-hospital mortality, the group of patients who died and those who survived were homogeneous in terms of the sex, fracture type, treatment type, anesthesiology type. However, those patients who died were significantly older than the survivors (86.42 vs 80.99, p=0.005). The prevalence of CAD, arrhythmia, chronic obstructive pulmonary disease (COPD), ASA IV were significantly higher in those patients who died. In particular, the presence of LVEF <50% and moderate-severe AS were more prominent in those who died (Table 4). As the multivariate analysis showed (Table 5), age (OR: 1.264, 95% CI: 1.047–1.527, p=0.015), history of CAD (OR: 19.290, 95% CI: 2.002–185.885, p=0.010), presence of AS (OR:7.164, 95% CI: 1.988–51.413, p=0.040), and LVEF <50% (OR:8.803, 95% CI: 1.115–69.472, p=0.039) were the dominant predictors of in-hospital mortality. The Hosmer–Lemeshow test showed the good fit (x2=0.902, p=0.999).
 |
Table 4 Characteristics of Hip Fracture Patients Classified by Survival Status Within Hospitalization |
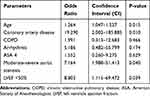 |
Table 5 Multivariate Analysis for the Prediction of In-Hospital Mortality |
Discussion
Postoperative cardiac complications are one of the most common and life-threatening adverse events in elderly patients following hip fracture and TTE is the most common tool used to assess cardiac risk preoperatively. However, the prognostic value of preoperative TTE abnormalities and postoperative outcome is still controversial.19 To the best of our knowledge, this was the first study comprehensively investigating the association between different types of preoperative TTE abnormalities and postoperative cardiac complications or mortality in elderly patients following hip fracture surgery. Our results showed that moderate-severe AS was an independent predictor of postoperative cardiac complications and in-hospital mortality. In addition, LVEF <50% was also an independent predictor of in-hospital mortality. However, no significant relationship was found in the rest of listed preoperative TTE abnormalities.
The postoperative cardiac complications rate was 7.6% in our study, which was similar to previous studies.10,20 The presence of significant valvular disease has been identified as an important predictor for cardiac events in patients undergoing noncardiac surgery in a previous study, which was similar to ours.21 To date, only a few studies have investigated the prognostic value of AS in postoperative outcome in elderly patients following hip fracture surgery.13,14,22,23 Rostagno et al conducted a study involving 428 elderly patients with hip fracture (145 with AS and 283 controls) and in agreement with our result, they showed there was a higher rate of postoperative myocardial infarction in patients with AS (8.3% vs 1.1%, p<0.001).23 However, a study from Keswani et al, involving a total of 153 elderly patients (46 with moderate or severe AS and 107 controls) showed there was no difference in the perioperative cardiac complication rate (17% vs 8.4%), which contradicts our study (30% vs 6.3%, p=0.001).13 One possible explanation was that their study regarded vascular accidents (deep vein thrombosis) as part of postoperative cardiac complications, which we thought were due to surgical complications rather than underlying cardiac abnormality. Besides, history of CAD was also identified as independent risk factor for postoperative cardiac complications, in agreement with a previous study.24
The in-hospital mortality rate was 2.8% in our study, which is in agreement with a previous study result.25 Both AS and LVEF <50% were independent predictors of in-hospital mortality. AS was established as an important factor that was associated with higher mortality in previous studies.14,22 In agreement with the results from our study, in-hospital mortality (6.2% vs 3.3%) reported by Adunsky et al22 and 30-day mortality (14.7% vs 4.2%, p < 0.001) reported by Leibowitz et al14 were significantly higher for AS patients as compared to controls.
The presence of LVEF <50% was shown to be associated with mortality in patients undergoing vascular surgery.26 However, to our knowledge, only few studies have reported the association between LVEF and postoperative outcome in elderly hip fracture.27,28 A recent study based on national database involving 2,020,712 patients, demonstrated that LVEF <50% increased the rate of postoperative adverse events such as in-hospital all-cause death, in-hospital cardiac arrest or acute ischemic stroke.27 However, another study involving 181 patients diagnosed with intertrochanteric fracture (only 65 had preoperative TTE) did not show the association between low LVEF and mortality.28 One explanation for this was that their study only included patients with intertrochanteric fracture, which had different baseline demographic characteristics compared with our study. Besides, some clinical factors were also identified as independent risk factors for mortality in our study, and these included advanced age, history of CAD. Increasing age has been widely identified as a risk factor for mortality in hip fracture patients because the patient with advanced age has poor physiological reserve to cope with the surgery and trauma stress.29,30 Preexisting CAD was a risk factor for in-hospital mortality in our study. In agreement with our result, Norring-Agerskov et al investigated the impact of cardiovascular disease on mortality among 113,211 patients with hip fracture, they showed that 30-day mortality was significantly increased in individuals with preexisting cardiac disease.31
With our study, we have demonstrated that presence of AS, LVEF <50% had a negative impact on postoperative cardiac complications or mortality, which could be explained by the hemodynamic instability in these patients. AS causes a reduction in left ventricular compliance and in coronary reserve. In addition, patients with LVEF <50% have poor cardiac reserve. As a result, the hemodynamic changes appear to be more pronounced in patients undergoing surgical procedures.
This study had another clinical implication. A previous study showed concern about the surgery delay caused by TTE,4 but early operative treatment is generally advocated for patients with a hip fracture to minimize the potential morbidity.32 The physical examination (murmur), cardiac biomarkers, and electrocardiogram could provide some information associated with cardiac disease (CAD, severe AS), but it is less reliable compared with echo especially in the medical centers without co-management models pairing orthopedic surgeons with anesthesiologists or cardiologists. Cardiac abnormalities including aortic stenosis, cardiac failure, and pulmonary hypertension, are all reliably evaluated by echocardiography.33–35 Therefore, our study may propose a method to balance the surgery delay and TTE test. Among the different types of TTE abnormalities, aortic stenosis and LVEF were the dominant predictors of postoperative cardiac complications and in-hospital mortality in elderly hip fracture. So, we could simplify the TTE process by assessing aortic valve and LVEF specifically on focused echocardiography, which could decrease the waiting time for surgery. However, further prospective studies with larger study population are required for better clarification.
To the best of our knowledge, this was the first study evaluating impact of the different types of TTE abnormalities on postoperative cardiac complications specifically and in-hospital mortality. However, there are several limitations to our study. Firstly, this was a retrospective study with natural selection bias. However, we minimized the bias in patient enrollment by using data from an electronic medical record database. Secondly, the patients involved were elderly patients with preoperative TTE, so our results cannot be directly applied to all patients undergoing hip fracture surgery.
Conclusion
In elderly patients undergoing hip fracture surgery, presence of AS and history of CAD were the predictive factors of postoperative cardiac complications. In addition, advanced age, history of CAD, presence of AS and LVEF <50% were the independent predictive factors of in-hospital mortality. Therefore, we could simplify the TTE process by assessing aortic valve and LVEF specifically on focused echocardiography, which could avoid surgery delay.
Abbreviations
TTE, transthoracic echocardiography; LVEF, left ventricular ejection fraction; CAD, coronary artery disease; AS, aortic stenosis; ASA, American Society of Anesthesiologists; AMI, acute myocardial infarction; PAPS, systolic pulmonary artery pressure; CI, confidence interval; PFNA, proximal femoral nail anti-rotation; COPD, chronic obstructive pulmonary disease.
Acknowledgment
Xuepan Chen and Yuanchen Ma are co-first authors in this study.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sheikh HQ, Hossain FS, Aqil A, Akinbamijo B, Mushtaq V, Kapoor H. A comprehensive analysis of the causes and predictors of 30-day mortality following hip fracture surgery. Clin Orthop Surg. 2017;9(1):10–18. doi:10.4055/cios.2017.9.1.10
2. Muhm M, Walendowski M, Danko T, Weiss C, Ruffing T, Winkler H. Factors influencing course of hospitalization in patients with hip fractures: complications, length of stay and hospital mortality. Z Gerontol Geriatr. 2015;48(4):339–345. doi:10.1007/s00391-014-0671-4
3. Brauer CA. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302(14):1573–1579. doi:10.1001/jama.2009.1462
4. Luttrell K, Nana A. Effect of preoperative transthoracic echocardiogram on mortality and surgical timing in elderly adults with hip fracture. J Am Geriatr Soc. 2015;63(12):2505–2509. doi:10.1111/jgs.13840
5. Simunovic N, Devereaux PJ, Sprague S, et al. Effect of early surgery after hip fracture on mortality and complications: systematic review and meta-analysis. CMAJ. 2010;182(15):1609–1616. doi:10.1503/cmaj.092220
6. Spurrier E, Wordsworth D, Martin S, Norris R, Parker MJ. Troponin T in hip fracture patients: prognostic significance for mortality at one year. Hip Int. 2011;21(6):757–761. doi:10.5301/HIP.2011.8840
7. Taheriazam A, Saeidinia A, Keihanian F. Total hip arthroplasty and cardiovascular complications: a review. Ther Clin Risk Manag. 2018;14:685–690. doi:10.2147/TCRM.S155918
8. Dawson-Bowling S, Chettiar K, Cottam H, et al. Troponin T as a predictive marker of morbidity in patients with fractured neck of femur. Injury. 2008;39(7):775–780. doi:10.1016/j.injury.2008.01.025
9. Ford MK. Systematic review: prediction of perioperative cardiac complications and mortality by the revised cardiac risk index. Ann Intern Med. 2010;152(1):26–35. doi:10.7326/0003-4819-152-1-201001050-00007
10. Choi JH, Cho DK, Song YB, et al. Preoperative NT-proBNP and CRP predict perioperative major cardiovascular events in non-cardiac surgery. Heart. 2010;96(1):56–62. doi:10.1136/hrt.2009.181388
11. Heyburn G, McBrien ME. Pre-operative echocardiography for hip fractures: time to make it a standard of care. Anaesthesia. 2012;67(11):1189–1193. doi:10.1111/j.1365-2044.2012.07330.x
12. Acan AE, Gultac E, Kilinc CY, Ozlek B, Gursan O, Biteker M. Preoperative mild pericardial effusion is associated with perioperative complications in elderly patients following hip fracture surgery. J Invest Surg. 2019;1–6. doi:10.1080/08941939.2019.1637484
13. Keswani A, Lovy A, Khalid M, et al. The effect of aortic stenosis on elderly hip fracture outcomes: a case control study. Injury. 2016;47(2):413–418. doi:10.1016/j.injury.2015.10.015
14. Leibowitz D, Rivkin G, Schiffman J, et al. Effect of severe aortic stenosis on the outcome in elderly patients undergoing repair of hip fracture. Gerontology. 2009;55(3):303–306. doi:10.1159/000209245
15. Fleisher LA, Fleischmann KE, Auerbach AD, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery. J Am Coll Cardiol. 2014;64(22):e77–137. doi:10.1016/j.jacc.2014.07.944
16. Schiller NB, Acquatella H, Ports TA, et al. Left ventricular volume from paired biplane two-dimensional echocardiography. Circulation. 1979;60(3):547–555. doi:10.1161/01.CIR.60.3.547
17. Zoghbi WA. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr. 2003;16(7):777–802. doi:10.1016/S0894-7317(03)00335-3
18. Guerra Ramos FJ. Role of echocardiography in suspected pulmonary hypertension. Arch Bronconeumol. 2011;47(Suppl 7):7–11. doi:10.1016/S0300-2896(11)70053-9
19. Memtsoudis SG. Preoperative echocardiography in hip fracture patients: a waste of time or good practice? Anesth Analg. 2019;128(2):207–208. doi:10.1213/ANE.0000000000003970
20. Ushirozako H, Ohishi T, Fujita T, et al. Does N-terminal pro-brain type natriuretic peptide predict cardiac complications after hip fracture surgery? Clin Orthop Relat Res. 2017;475(6):1730–1736. doi:10.1007/s11999-017-5245-5
21. Fleisher LA, Fleischmann KE, Auerbach AD, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: executive summary. Circulation. 2014;130(24):2215–2245. doi:10.1161/CIR.0000000000000105
22. Adunsky A, Kaplan A, Arad M, Mizrahi EH, Gottlieb S. Aortic stenosis in elderly hip fractured patients. Arch Gerontol Geriatr. 2008;46(3):401–408. doi:10.1016/j.archger.2007.05.013
23. Rostagno C, Ranalli C, Polidori G, Cartei A, Boccaccini A, Peris A. Outcome in elderly patients with aortic stenosis undergoing hip fracture surgery. Results may suggest a different postoperative strategy? Trauma Surg Acute Care Open. 2019;4(1):e000218. doi:10.1136/tsaco-2018-000218
24. Kim BS, Kim TH, Oh JH, et al. Association between preoperative high sensitive troponin I levels and cardiovascular events after hip fracture surgery in the elderly. J Geriatr Cardiol. 2018;15(3):215–221. doi:10.11909/j.issn.1671-5411.2018.03.002
25. Yonekura H, Ide K, Onishi Y, Nahara I, Takeda C, Kawakami K. Preoperative echocardiography for patients with hip fractures undergoing surgery: a retrospective cohort study using a nationwide database. Anesth Analg. 2019;128(2):213–220. doi:10.1213/ANE.0000000000003888
26. Flu WJ, van Kuijk JP, Hoeks SE, et al. Prognostic implications of asymptomatic left ventricular dysfunction in patients undergoing vascular surgery. Anesthesiology. 2010;112(6):1316–1324. doi:10.1097/ALN.0b013e3181da89ca
27. Bohsali F, Klimpl D, Baumgartner R, Sieber F, Eid SM. Effect of heart failure with preserved ejection fraction on perioperative outcomes in patients undergoing hip fracture surgery. J Am Acad Orthop Surg. 2019;28(3):e131–138.
28. Kalem M, Kocaoglu H, Sahin E, Kocaoglu MH, Basarir K, Kinik H. Impact of echocardiography on one-month and one-year mortality of intertrochanteric fracture patients. Acta Orthop Traumatol Turc. 2018;52(2):97–100. doi:10.1016/j.aott.2017.12.006
29. Forni C, Gazineo D, D’Alessandro F, et al. Predictive factors for thirty day mortality in geriatric patients with hip fractures: a prospective study. Int Orthop. 2019;43(2):275–281. doi:10.1007/s00264-018-4057-x
30. Karres J, Kieviet N, Eerenberg JP, Vrouenraets BC. Predicting early mortality after hip fracture surgery: the hip fracture estimator of mortality amsterdam. J Orthop Trauma. 2018;32(1):27–33. doi:10.1097/BOT.0000000000001025
31. Norring-Agerskov D, Madsen CM, Bathum L, et al. History of cardiovascular disease and cardiovascular biomarkers are associated with 30-day mortality in patients with hip fracture. Osteoporos Int. 2019;30(9):1767–1778. doi:10.1007/s00198-019-05056-w
32. Pincus D, Ravi B, Wasserstein D, et al. Association between wait time and 30-day mortality in adults undergoing hip fracture surgery. JAMA. 2017;318(20):1994–2003. doi:10.1001/jama.2017.17606
33. Karthikeyan G, Moncur RA, Levine O, et al. Is a pre-operative brain natriuretic peptide or N-terminal pro-B-type natriuretic peptide measurement an independent predictor of adverse cardiovascular outcomes within 30 days of noncardiac surgery? A systematic review and meta-analysis of observational studies. J Am Coll Cardiol. 2009;54(17):1599–1606. doi:10.1016/j.jacc.2009.06.028
34. Jansen S, Koster RW, de Lange FJ, et al. Electrocardiographic abnormalities in patients admitted for hip fracture. Neth J Med. 2014;72(9):455–461.
35. Sawhney C, Trikha V, Janani S, Bajwa SJS, Sharma V, Khanna M. Impact of preoperative echocardiography on perioperative management in geriatric hip trauma: a retrospective observational study. Int J Appl Basic Med Res. 2017;7(2):104–107. doi:10.4103/2229-516X.205816
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
