Back to Journals » Drug Design, Development and Therapy » Volume 14
Physical Compatibility and Chemical Stability of Fentanyl and Naloxone Hydrochloride in 0.9% Sodium Chloride Injection Solution for Patient-Controlled Analgesia Administration
Authors Chen P , Chen F, Lei J, Zhou B
Received 3 February 2020
Accepted for publication 27 April 2020
Published 9 October 2020 Volume 2020:14 Pages 4179—4187
DOI https://doi.org/10.2147/DDDT.S248209
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Yan Zhu
Peng Chen,1,* Fuchao Chen,2,* Jiexin Lei,3 Benhong Zhou1
1Department of Pharmacy, Renmin Hospital of Wuhan University, Wuhan, Hubei 430060, People’s Republic of China; 2Department of Pharmacy, Dongfeng Hospital, Hubei University of Medicine, Shiyan, Hubei 442008, People’s Republic of China; 3Department of Endocrinology, Renmin Hospital of Wuhan University, Wuhan, Hubei 430060, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Benhong Zhou
Department of Pharmacy, Renmin Hospital of Wuhan University, Wuhan, Hubei 430060, People’s Republic of China
Tel +86 15335898431
Email [email protected]
Background and Objective: The combination of naloxone hydrochloride (NH) and fentanyl citrate (FC) in patient-controlled analgesia (PCA) is examined to reduce the risk of opioid-induced nausea and vomiting. However, there are no such commercially available drug mixtures, and there is also no published evidence on the compatibility and stability of NH and FC. Thus, the primary purpose of the current research is to investigate the physical compatibility and chemical stability of NH when mixed with FC over a 72-h period in a 0.9% sodium chloride injection solution for PCA administration under storage at 4°C and 25°C.
Methods: Test solutions of 20 μg/mL FC and 4 μg/mL NH were prepared and stored in polyvinyl chloride (PVC) bags or glass bottles with a 0.9% sodium chloride injection solution as the diluent. During the 72-h storage period at 4°C or 25°C without light protection, the concentrations of the test drugs were assayed via high-performance liquid chromatography (HPLC), and the physical compatibility was determined with the naked eye. Furthermore, pH measurement of each sample was also performed with a pH meter.
Results: The percentages of the initial concentrations of FC and NH in the various solutions were maintained at a minimum of 98% over the 72-h study period. All of the mixtures remained clear and colourless throughout the observation period, and no precipitation or turbidity was observed in any of the batches.
Conclusion: The 20 μg/mL FC test solution was physically compatible and chemically stable with the 4 μg/mL NH test solution when stored at 4°C or 25°C in PVC bags or glass bottles containing the 0.9% sodium chloride injection solution.
Keywords: fentanyl, naloxone, patient-controlled analgesia, 0.9% sodium chloride, drug stability
Introduction
Patient-controlled analgesia (PCA) with different opioids has been confirmed to be a convenient treatment programme for postoperative pain management in clinics because it provides effective postoperative analgesia and a high patient satisfaction with minimal sedation and complications and is used extensively in the field of anesthesia.1,2 However, mixing 2 or more analgesic drugs in PCA delivery can create potential problems related to drug instability and incompatibility, which may reduce the efficacy and cause precipitation/crystallization.3 Hence, comprehensive information on the stability and compatibility of mixtures of these drugs is required to evaluate the feasibility of such a practice.
Fentanyl citrate (FC, Figure 1A), N-(1-phenethyl-4-piperidinyl) propionanilide dihydrogen citrate), is a strong synthetic opioid that is 80–100 times more powerful than morphine.4 Given its unique analgesic potency, PCA with FC is widely used to manage postoperative, gynaecologic, and obstetric pain in clinical patients, but it also has serious adverse reactions (ADRs), such as postoperative nausea and vomiting (PONV), dizziness, hypotension, pruritus, and respiratory depression.5,6 Naloxone hydrochloride (NH, Figure 1B, (5α)-4,5- epoxy-3,14-dihydroxy-17-(2-propen-1-yl) morphinan-6-one, is an easy-to-use opioid antagonist analgesic that binds to opioid receptors but does not affect the receptors themselves.7,8 It has been reported in recent years that a small amount of naloxone as an adjuvant to an opioid can help to reduce the requirements for and potential adverse effects of the opioid.9 Randomized controlled trials have evaluated the efficacy of NH in conjunction with FC-based intravenous PCA for postoperative pain, and superior pain control and a significantly reduced incidence and severity of PONV have been demonstrated.10,11
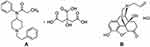 |
Figure 1 Structures of (A) fentanyl citrate and (B) naloxone hydrochloride. |
Currently, mixtures of FC and NH are often not commercially available; therefore, pharmacists in community or hospital pharmacy practices can provide these mixed liquors by blending the respective components in a 0.9% sodium chloride injection solution and storing the ready-to-use solution for PCA.12,13 However, to our knowledge, the stability of FC and NH in a 0.9% sodium chloride injection solution has not yet been reported. Therefore, the objective of the current study was to investigate the physical compatibility and chemical stability of the binary admixture of FC and NH prepared with a 0.9% sodium chloride injection solution and stored at temperatures of 4°C and 25°C in polyvinyl chloride (PVC) bags and glass bottles for up to 72 h and provide a theoretical basis for clinicians to guide the safe and rational use of these drugs in PCA.
Methods
Materials and Reagents
The reference standards of FC (lot 140,302, chemical purity higher than 99.8%) and NH (lot 121,430, chemical higher than purity 99.7%) were purchased from the Yichang Renfu Pharmaceutical Co., Ltd. (Hubei, China). Commercially available ampoules of the pharmaceutical formulations used in this study were FC injection (0.5 mg/10 mL, lot 2,121,002, Kelun Pharmaceutical Co., Ltd., Sichuan, China) and NH injection (4 mg/10 mL, lot 20,180,613, Enhua Pharmaceutical Co., Ltd., Jiangsu, China) solutions. The 0.9 mg/mL sodium chloride injection solution (250 mL, lot W1090302F) used to prepare the sample solution was obtained from the Kelun Pharmaceutical Co., Ltd. (Sichuan, China). All of the chemicals used in this study were of analytical grade and purchased from the Guoyao Chemical Reagent Co., Ltd. (Beijing, China), unless otherwise stated.
Instrumentation
High-performance liquid chromatography (HPLC) was performed to evaluate the sample concentrations. The HPLC instrument (Ultimate 3000, Dionex, Germering, Germany) was equipped with a quaternary liquid gradient system, WPS-3000RS auto-injector, TCC-100 column oven, and DAD-3000RS UV spectrophotometer. Chromoleon chromatography software (version 6.80) was used for the chromatographic data acquisition and analysis. The pH of each solution was measured with a PHS-3C pH meter (Shanghai Leici Instrument Co., China).
Chromatographic Conditions
Chromatographic separation of the analytes was achieved with a Thermo Scientific Hypersile Gold C18 column (1.9 μm particle size, 100 mm×2. mm) equipped with a prefilter. The mobile phase composition was a mixture of 0.1% formic acid in a 50 mM potassium dihydrogen phosphate buffer (Wuhan Huashen Chemical Reagent Co. Ltd., Wuhan, China, A) and 0.1% formic acid in acetonitrile (HPLC grade, Agilent Technologies, B) (70:30, v/v), which was pumped at a flow rate of 0.5 mL/min for the chromatography assay. The column temperature was maintained at 25°C, and an injection volume of 10 μL for each sample was adopted for all determinations. The FC and GH samples were spectrophotometrically evaluated at 220 and 210 nm, respectively.14,15
Preparation of the Stock and Standard Curve Solutions
The stock standard solutions containing 0.5 mg/mL FC and 0.4 mg/mL NH in the mobile phase were prepared from the analytical reference standards. The analytical grade powder was dissolved in deionized water to produce the stock standard solutions that remained stable for 72 h or longer at 4°C. Calibration curves were constructed by injecting six different concentrations ranging from 5.0 to 100.0 μg/mL for FC and from 4.0 to 40.0 μg/mL for NH.
Method Validation
The proposed method was validated by determining the linearity range, accuracy, intra- and inter-day precision and parameters for drug stability testing. The linearity was assessed by preparing mixed standard solutions of FC and NH at six concentration levels and three replicates. The linearity of the detector response for FC and NH was demonstrated by the prepared solutions over the concentration ranges of 5.0–100 and 1.0–12 μg/mL, respectively. Linear regression analysis of the calibration data was performed by plotting the standard curve of the detector response (peak areas) against the concentration of the reference standards. The coefficient of determination (r2) was calculated. To determine the accuracy and intra- and inter-day precision, three control samples (QCs) of FC (10.0, 30.0, and 60.0 μg/mL) and NH (2.0, 4.0, and 8.0 μg/mL) were prepared and analysed. The recovery and relative standard deviation (RSD%) of the peak area values were calculated from the 3 QCs of FC and NH, and each concentration was measured 5 times on the same day to estimate the accuracy and intra- or inter-day precision.
Stability Study of the Analgesic Solutions
A mixture of FC and NH was injected into 100-mL PVC bags to yield final concentrations of 20 and 4 μg/mL, respectively, and stored at 4°C and 25°C in the dark.10,11 This operation was repeated three times. The concentration of these drugs in the current study was selected based on daily clinical use. Three PVC bags and three glass containers containing these solutions were prepared at storage conditions of 4 °C or 25°C. At each time point (0, 4, 8, 12, 24, 48 and 72 h), a 2-mL sample was removed from each container immediately after preparation for use in the stability study. In this study, the infusion samples were visually inspected with the naked eye for the solution colour and clarity each time, and duplicate pH measurements were conducted.16 All samples from each test were then aliquoted and frozen at −20°C until further analysis. The samples from each bag and bottle were analysed in triplicate (n=3).
Stability Indication
To confirm the separation of the degradation products from the parent molecules, a chromatographic concentration detection method was adopted for the degraded samples in 0.9% sodium chloride. The FC, NH and mixtures of FC and NH in the injectable sodium chloride solutions were degraded by heating at 60°C for 5 h under the following conditions: 0.1 mol/L hydrochloric acid (HCl), 0.1 mol/L sodium hydroxide (NaOH), and 3% hydrogen peroxide (H2O2).8,12 After completing the degradation preparations, the solutions were assessed by HPLC assay.
Analysis of the Data
The results are presented as the mean ± standard deviation (mean ± sd). The drug concentration at the starting time of preparation for FC and NH was identified as 100%, and all subsequent sample concentrations were defined as a percentage of the initial concentration. The drug admixtures were considered chemically unstable if a change of more than 10% occurred within each individual container. The change in drug concentration in the solutions at the different time points was analysed by linear regression analysis. The SPSS version 15.0 statistical software package (SPSS Inc., USA) was used to perform all statistical analyses.
Results
Validation of the HPLC Method
Simultaneous determination of the FC and NH concentrations was performed through the validated stability-indicating HPLC assay method. For FC, the results of the study showed a good linear response between the peak area vs the concentration with a correlation coefficient (r) better than 0.9998 (y =106.4x-0.27). For NH, linear regression analysis of the peak area of the drug concentration yielded a correlation coefficient (r) better than 0.9994 (y =1045x - 2.42). The degradation study results are shown in Figures. 2–4, demonstrating that the degradation of the compounds was baseline separated from the analytes (all decomposition products were less than 3% isolated from all analytes), and there was no interference with the quantification of each drug and the combination of drugs. Under the chromatographic conditions, the average retention times for FC and NH were 4.84 and 9.08 minutes, respectively. The intra- and inter-day precision and accuracy of the assay method were measured, and these data are provided in Table 1. The results of the study showed that the proposed HPLC method is simple, accurate and precise, which is useful for the determination of FC and NH in sodium chloride solutions (0.9%).
 |
Table 1 Validation of HPLC Method for Determination of Fentanyl Citrate and Naloxone Hydrochloride |
Stability of the Analgesic Mixtures
The results of the physical compatibility tests for FC and NH showed that no instability signal was observed for any test samples; for example, no precipitation, colour change or opacity was detected. The stability data of FC and NH in the 0.9% sodium chloride injection solution for PCA administration stored at 4°C or 25°C are summarized in Tables 2 and 3, respectively. As indicated by these results, the products in the mixtures over the 72-h trial period and the percentages of FC and NH remaining in the drug admixtures were all higher than 98.6%. The chromatography analysis demonstrated that the degradation products detected during the accelerated degradation study are not readily apparent in these chromatograms and did not increase in quantity over the study period (Figure 5AD). Moreover, the pH of the admixtures ranged from 4.3 to 4.6, and the changes were smaller than 0.14 throughout the study period in all samples.
Discussion
Combinations of different classes of drug solutions are commonly used to manage postoperative pain with PCA.17 However, these analgesic mixtures in clinical practice are not available through commercial channels, and these solutions should be prepared and administered by hospital pharmacists under sterile conditions.18 In addition to the above, it would be further beneficial if we can provide such combinations or mixtures that can be directly used for clinical practices to strengthen sterilisation and sterility assurance for pharmaceuticals and reduce the risk of ADRs caused by medication administration errors.19 Currently, the combination of fentanyl citrate with naloxone hydrochloride in solutions via PCA to reduce opioid-induced nausea and vomiting is now accepted, but to date, there are no published data describing the compatibility and stability of such mixtures.10,11 Therefore, the present study aims to address this issue.
Previously, the physical compatibility and/or stability of FC as a single drug or in combination with other drugs in infusion solutions has been widely studied. Evidence has been found that FC remains stable for at least 90 days when mixed in 5% dextrose injection or 0.9% sodium chloride injection solutions and stored at 25°C.20–22 Moreover, previous studies have revealed that there were no signs of chemical degradation of FC during the experimental period. It has also been reported that most of the other tested drugs, such as hydromorphone hydrochloride, ketamine hydrochloride, midazolam, morphine sulphate, bupivacaine hydrochloride, epinephrine hydrochloride and pentobarbital sodium, remained stable and were compatible in the presence of FC.23,24 However, precipitation was observed when FC was mixed with lornoxicam in 0.9% sodium chloride injection solutions for PCA.25 This phenomenon most likely occurred because FC is a weak acid with a pKa of 8.4.26 NH, which is structurally similar to oxymorphone, exhibits a weak acidity, and the compound remains stable under acidic solutions.27 To date, there is limited published information regarding the compatibility and stability of NH alone or combined with other drugs in infusion solutions.28 C. Kistner and others studied the effect of different concentrations and time periods of NH injections mixed with morphine sulphate prepared in 0.9% sodium chloride solutions.16 They reported that 1000 µg/mL morphine sulphate and NH at concentrations of 4, 12.5, or 25 µg/mL in a 0.9% sodium chloride solution for injection remained stable for 72 h at room temperature and for 30 days under refrigeration.
In this experiment, the quantitative analysis methods of FC with NH were adapted from the published literature on chromatographic analysis methods. An acidic aqueous solution and acetonitrile were employed to design the optimal mobile phases used for the separation of mixtures of FC with NH. The results of these trials showed that a reversed-phase C18 HPLC column with an acidic mobile phase resulted in notable peaks. In our study, there was no sign of precipitation during the experimental period, and no evidence of chromatographic peak modification in the binary mixtures at either of the temperatures was observed. The pH values of the binary mixtures containing FC with NH varied between 4.3 and 4.6, and their acidity was equal to that of some organic acids. The satisfactory compatibility and stability results showed that the binary mixtures of FC with NH in the 0.9% sodium chloride injection solutions remained stable for up to 72 h when stored at 4°C or 25°C in PVC bags or glass bottles.
Bacterial contamination may occur when mixtures of drugs are retrieved from ampoules of sterile solutions.29 In this study, the physicochemical stability of mixing drugs was researched, but the issue of microbial contamination was ignored. Hence, Chapter 797 of the United States Pharmacopoeia (USP)/national prescription should be respected and enforced in clinical practices.30 According to these standards, the agents we analysed were classified as low-risk composite aseptic products. In this regulation, the preparation is a low-risk compounding sterile product. Given that sterility can change according to the site, equipment, operator, and procedures used, the following cautionary measures are suggested: (1) the preparation should not be used beyond 48 h or 14 days when stored at room temperature or under refrigeration, respectively, on the basis of the USP standards; (2) the infusion can be safely prepared and stored by a pharmacist using aseptic techniques or by licensed central additive (CIVA) services in hospitals.
Conclusion
In summary, the clinical implications of our results are that a diluted infusion solution containing 20 μg/mL FC mixed with 4 μg/mL NH in a 0.9% sodium chloride injection solution may be pre-prepared and used with confidence up to at least 72 h following preparation when stored in PVC bags or glass bottles under specified temperature conditions (both at 4°C or 25°C) and protected from light. Given that in the current study satisfactory stability results for these 2 chemicals were obtained, it can be concluded that the combined solution can be safely prepared in advance and stored (in the dark) for up to 72 h by CIVA services, which may be convenient in hospitals.
Disclosure
The authors report no conflicts of interest for this work.
References
1. Singelyn FJ, Ferrant T, Malisse MF, et al. Effects of intravenous patient-controlled analgesia with morphine, continuous epidural analgesia, and continuous femoral nerve sheath block on rehabilitation after unilateral total-hip arthroplasty. Reg Anesth Pain Med. 2005;30:452–457.
2. Mann C, Pouzeratte Y, Boccara G, et al. Comparison of intravenous or epidural patient-controlled analgesia in the elderly after major abdominal surgery. Anesthesiology. 2000;92:433–441.
3. Bonner JC, Mcclymont W. Respiratory arrest in an obstetric patient using remifentanil patient-controlled analgesia. Anaesthesia. 2012;67:538–540.
4. Madej TH, Strunin L. Comparison of epidural fentanyl with sufentanil. Analgesia and side effects after a single bolus dose during elective caesarean section. Anaesthesia. 2010;42:1156–1161.
5. Marwah R, Hassan S, Carvalho JC, et al. Remifentanil versus fentanyl for intravenous patient-controlled labour analgesia: an observational study. Can J Anasth. 2012;59:246–254.
6. Jin HK, Sun YJ, Kim MJ, et al. Comparison of pain-relieving effects of fentanyl versus ketorolac after eye amputation surgery. Kjo. 2013;27:229–234.
7. Cepeda MS, Alvarez H, Morales O, et al. Addition of ultralow dose naloxone to postoperative morphine PCA: unchanged analgesia and opioid requirement but decreased incidence of opioid side effects. Pain. 2004;107:41–46.
8. Firouzian A, Gholipour BA, Alipour A, et al. Ultra-low-dose naloxone as an adjuvant to patient controlled analgesia (PCA) with morphine for postoperative pain relief following lumber discectomy: a double-blind, randomized, placebo-controlled trial. J Neurosurg Anesth. 2016;30:26–31.
9. Carr DB, Cepeda MS. ‘Simply no difference’ in pain intensity and opioid requirement when ultralow doses of naloxone are added to morphine PCA. Pain. 2004;110:502–503.
10. Zheng J, Han W, Han XD, et al. Effect of naloxone on intravenous fentanyl patient-controlled analgesia after laparoscopic cholecystectomy. Medicine. 2016;95:e5074.
11. Tian H, Dong D, Song C, et al. Postoperative intravenous analgesia with fentanyl alone or fentanyl in combination with naloxone, ketamine or dexmedetomidine in elderly patients. Int J Clin Exp Med. 2018;11:1015–1020.
12. Chapalain-Pargade S, Laville I, Paci A, et al. Microbiological and physicochemical stability of fentanyl and sufentanil solutions for patient-controlled delivery systems. J Pain Symptom Manga. 2006;32:90–97.
13. Selbach S, Diederich WE, Fett S, et al. Stability-indicating HPLC assays for the determination of piritramide and droperidol in PCA solution. J Clin Pharm Ther. 2015;36:161–165.
14. Sattler A, Jage J, Krämer I. Physico-chemical stability of infusion solutions for epidural administration containing fentanyl and bupivacaine or lidocaine. Pharmazie. 1998;53:386–391.
15. Lewin AH, S E F, Zhong D, et al. Caged naloxone: synthesis, characterization, and stability of 3-O-(4,5-dimethoxy-2-nitrophenyl) carboxymethyl naloxone (CNV-NLX). ACS Chem Neurosci. 2018;9:563–567.
16. Kistner C, Ensom MH, Decarie D, et al. Compatibility and stability of morphine sulphate and naloxone hydrochloride in 0.9% sodium chloride for injection. CanJ Hosp Pharm. 2013;66:163–170.
17. Chen F, Xiong H, Yang J, et al. Butorphanol and ketamine combined in infusion solutions for patient-controlled analgesia administration: a long-term stability study. Med Sci Monitor. 2015;21:1138–1145.
18. Chen FC, Zhu J, Li B, et al. Stability of tramadol with three 5-HT3 receptor antagonists in polyolefin bags for patient-controlled delivery systems. Drug DesDev Ther. 2016;10:1869–1875.
19. Chen FC, Fang BX, Li P, et al. Compatibility of butorphanol and droperidol in0.9% sodium chloride injection. Am J Health Syst Pharm. 2013;70:515–519.
20. Peterson G, Miller K, Galloway J, et al. Compatibility and stability of fentanyl admixtures in polypropylene syringes. J Clin Pharm Ther. 2010;23:67–72.
21. Pharm DRMCB. Chemical stability of fentanyl in polypropylene syringes and polyvinylchloride bags. Int J Pharm Compd. 2005;9:482–484.
22. Mccluskey SV, Graner KK, Kemp J, et al. Stability of fentanyl 5 microg/mL diluted with 0.9% sodium chloride injection and stored in polypropylene syringes. Am J Health Syst Pharm. 2009;66:860–862.
23. Anderson C, Mackay M. Stability of fentanyl citrate, hydromorphonehydrochloride, ketamine hydrochloride, midazolam, morphine sulfate, and pentobarbital sodium in polypropylene syringes. Pharmacy. 2015;3:379–385.
24. A L J, Stiles ML, Wang DP, et al. Stability of bupivacaine hydrochloride, epinephrine hydrochloride, and fentanyl citrate in portable infusion-pump reservoirs. Am J Hosp Pharm. 1993;50:714–718.
25. Chen FC, Fang BX, Peng L, et al. Compatibility and stability of lornoxicam with morphine, tramadol or fentanyl in infusion solutions. Afr J Pharm Pharmacol. 2012;6:2055–2060.
26. Helin-Tanninen M, Lehtonen M, Naaranlahti T, et al. Stability of an epidural analgesic admixture of levobupivacaine, fentanyl and epinephrine. J Clin PharmTher. 2013;38:104–108.
27. Panchagnula R, Sharma P, Khandavilli S, et al. RP-HPLC method and its validation for the determination of naloxone from a novel transdermal formulation. Farmaco. 2004;59:839–842.
28. Cloutier C, Taliano J, O’Mahony W, et al. Controlled-release oxycodone and naloxone in the treatment of chronic low back pain: A placebo-controlled, randomized study. Pain Res Manag. 2016;18:75–82.
29. Robustelli Della Cuna FS, Mella M, Magistrali G, et al. Stability and compatibility of methylprednisolone acetate and ropivacaine hydrochloride in polypropylene syringes for epidural administration. Am J Health-Syst Pharm. 2001;58:1753–1756.
30. Kastango ES, Bradshaw BD. USP chapter 797: establishing a practice standard for compounding sterile preparations in pharmacy. Am J Health-Syst Pharm. 2004;61:192–1938.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.






