Back to Journals » Clinical Interventions in Aging » Volume 9
Oral health status, dental treatment needs, and barriers to dental care of elderly care home residents in Lodz, Poland
Authors Gaszynska E, Szatko F, Godala M, Gaszynski T
Received 22 June 2014
Accepted for publication 22 July 2014
Published 25 September 2014 Volume 2014:9 Pages 1637—1644
DOI https://doi.org/10.2147/CIA.S69790
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Ewelina Gaszynska,1 Franciszek Szatko,1 Malgorzata Godala,2 Tomasz Gaszynski3
1Department of Hygiene and Health Promotion, Medical University of Lodz, Lodz, Poland; 2Department of Nutrition and Epidemiology, Medical University of Lodz, Lodz, Poland; 3Department of Emergency Medicine and Disaster Medicine, Medical University of Lodz, Lodz, Poland
Objectives: To determine oral health status, dental treatment needs, and to identify barriers that prevent easy access to dental care by elderly care home residents in Lodz.
Background: Studies in many countries show that oral health status of elderly care home residents is poor and there is an urgent need to improve it.
Methods: The study included 259 care home residents, aged 65 years and older. The oral examination was performed. In face-to-face interviews, subjects were asked about frequency of cleaning teeth and/or dentures, whether they needed assistance, and whether the assistance was available; they were also asked about the perceived dental needs, and about the time since their last visit to a dentist and the purpose of the visit. If they had not visited the dentist in the past 12 months, they were asked about reasons for failing to visit the dentist.
Results: Forty-six percent of the subjects were edentulous. Only 5.8% of all participants had a sufficient number of functional natural teeth. Dental treatment was found to be necessary in 59.8% of the respondents. One in four subjects reported reduced ability of correctly cleaning teeth and dentures themselves, of whom only one-third were helped by others. An insufficient level of hygiene was found in every other subject. About 42% of residents had not visited a dentist for over 5 years, mainly due to organizational reasons.
Conclusion: Expanding the current scope of medical care for the elderly care home residents to include dental care would improve their currently poor oral health status.
Keywords: dental care, institutionalized elderly, treatment needs, oral behaviors
Background
The proportion of elderly people in the population of most European countries is steadily increasing. More and more attention is paid to maintaining optimal physical and mental health of elderly people and improving their quality of life. Impaired oral function represents one of the most common and potentially serious problems contributing to the deterioration in the quality of life of elderly people.1–4 Poor oral health often coexists with other age-related conditions: comorbidities and metabolic dysregulations, cognitive impairment, or even elevated overall mortality.5–7 Unsatisfactory oral health and unhealthy behaviors contribute to development of many ailments, including chronic cardiac and pulmonary diseases, or metabolic diseases, such as diabetes.8–14 The impaired health of elderly people causes deterioration of their oral health status, which then acts to exacerbate the existing chronic diseases. World Health Organization (WHO) experts, who are aware that this issue is an important social problem, have addressed the authorities worldwide to implement strategies intended to improve oral health and dental care for the elderly.1
Healthy diet and not using tobacco are also essential for preserving good oral health in addition to other behavioral factors, such as daily dental care and regular visits to the dentist.15,16 Relevant awareness among elderly people and their caretakers, as well as their adequate physical fitness constitute essential prerequisites for effective and systematic removal of dental plaque. Other people should help the elderly persons in daily removal of dental plaque or do it totally themselves in cases of severely impaired motoric and/or cognitive functions.
However, studies in many countries show that the oral health status (OHS) of elderly care home residents is poor and there is an urgent need to improve it.17–22 Most of those studies have attempted to evaluate factors that, in the opinion of the medical staff/caregivers and care home managers, prevent maintaining oral hygiene and causes dental care not to be easily accessible.23,24 In our study, we have included opinions obtained directly from the care home residents. The information from caregivers and care home management was regarded as supplementary.
In Poland, there is little research about the accessibility of dental care in care homes,25,26 and the assistance in maintaining oral hygiene has not been explicitly included in the duties of nursing home staff.
The demographic transformation of Polish society has resulted, among other things, in a rapidly growing proportion of people aged 65 and older in the general population, accompanied by reduced welfare and increasing demand for institutional long-term care. It is estimated that in 2015, elderly people shall account for over 12% of the total population of Poland.27
The objectives of the study are: to evaluate dental treatment needs and identify barriers that prevent easy access to dental care of elderly care home residents in Lodz.
Methods
Subjects
In Lodz, a city of over 800,000 inhabitants located in central Poland, there are 13 state-run care homes for adults, including four for the elderly, five for people with chronic somatic diseases, and four for patients with chronic mental diseases. This cross-sectional study was carried out in seven care homes (four for the elderly and three for people with somatic diseases). Directors in the remaining two homes for people with somatic diseases did not agree to participate in the research.
The eligible participants comprised persons aged 65 years and older, with normal cognitive function. Based on a survey conducted by geriatric medicine specialists, 315 people were enrolled. However, as a result of disagreement of some residents to participate in the study, or withdrawal during the course of the study, the final number of participants was 259 (97 men, 162 women).
The study was approved by the Ethics Committee at the Medical University of Lodz, decision number RNN/181/13/KB.
Questionnaire surveys
In face-to-face interviews, subjects were asked about frequency of cleaning their teeth and/or dentures (twice or more a day, once a day or less), whether they needed direct assistance or maybe even had to rely completely on somebody else for their oral hygiene practices, and about who they receive such assistance from (visiting family members, nursing home staff). Questions were also asked about self-perceived dental needs and whether the subjects had reported those needs to the personnel. They were asked about the time since their last visit to a dentist and the purpose of visiting a dentist (check-up, immediate treatment, prosthetic treatment). If the reviewed resident had not visited the dentist in the past 12 months, the interviewer tried to determine reasons for the resident’s failure to do so, such as health problems, lack of awareness, organizational problems, anticipated high cost, and fear of pain. Demographic data were also recorded, including age, sex, and level of education.
Oral examination
Dental assessment was carried out by one dentist (the first author) using dental mirror, probe, and optic fiber head lamp.28
The following data were recorded: the number of remaining natural teeth (the number of natural teeth including the number of teeth with prosthetic crowns), and the number of functional teeth (the number of occluding natural teeth, teeth with prosthetic crowns, and prosthetic teeth on fixed and removable prostheses). Remaining roots ≤2 mm were not counted either as present or functional teeth. Third molars were not included as functional or own teeth, unless a molar/premolar was missing. The clinical status of remaining teeth was evaluated by sum of decayed, missing, and filled teeth (DMFT). Teeth with prosthetic crowns were assigned as filled teeth.
Oral hygiene was assessed using mucosal plaque score (MPS).24,29 The size of plaque on teeth/dentures (range: 1 – normal to 4 – excessive amount of plaque) and gingival/mucosal inflammation (range: 1 – normal to 4 – high degree of inflammation) was assayed. The index was dichotomized into acceptable and unacceptable oral hygiene scores. If the sum of the two components (MPS index) was greater than 4, the subject was included in the group with insufficient oral hygiene. Eleven residents who did not use any dentures and had no natural teeth were excluded from the MPS assessment part of the study.
Dental treatment needs were assessed from the clinical examination, without radiological testing. The need for conservative treatment had been recorded if a cavity was diagnosed and the tooth surface was soft when probing, while the need for tooth extraction had been noted if the cavity was very extensive, the crown was shorter than 2 mm or third-degree tooth mobility was assigned according to classification of Miller (tooth mobility >1 mm in any direction, including vertical displacement and/or rotation) and the need for functional prosthetic treatment was reported if a number of teeth <20 or dentures had extensive cracks and/or fractures.
Statistical analysis
Chi-squared and Fisher’s exact tests were applied when testing association between two categorical variables. Kruskal–Wallis test was used to analyze continuous variable distributions’ differentiation on categorical variable categories. Multiple regression analysis was used to test the association between visits to the dentist more than 12 months ago and the number of remaining natural teeth, number of functional teeth, number of prescribed medication, ten activities of daily living, systemic ailments, and cleaning of teeth and/or dentures less than twice a day. The level of significance was set at 0.05. Statistica version 10.0 (StatSoft, Tulsa, OK, USA) was applied for statistical analysis.
Results
Sociodemographic characteristics
The mean age of subjects was 75.3±8.9 years (range, 65–99 years), mean age of women was 78.2±6.3 years (65–99 years), mean age of men was 70.4±8.9 years (65–90 years). The proportion of men in the study population decreased with age; women dominated the group of subjects above 75 years of age. Seventy-three percent of the respondents had primary or vocational education, 21.6% had secondary, and 5.4% had incomplete or full higher education. The structure of the study population was similar to the population of elderly people in the general population of Poland.30 As many as 97% of subjects had systemic ailments, most prevalent were cardiac/circulatory 64.5%, musculoskeletal 37.3%, and endocrine/metabolic/nutritional 29.3%. The mean number of prescribed medication was 6.9±2.9 medications. Ability to perform ten activities of daily living assessed by a nurse or a medical carer ranged from nine to 20.
Current dental status
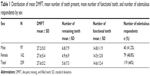
Edentulism was found in 46% of the residents (Table 1). Women had a smaller mean number of remaining teeth than men and more often were edentulous, but these differences were not statistically significant.
Among the edentulous individuals only 9.2% used upper and lower dentures, and among the dentate residents with an insufficient number of functional teeth (less than 20 occluding teeth), less than half used prostheses (Table 2). Only one person had fixed dental prosthesis, two people used frame prostheses, and the remaining wore removable partial dentures supported by mucous membrane.
  | Table 2 Dental status of examined elderly respondents |
An insufficient level of hygiene was diagnosed in 47.2% of dentate and/or denture-using participants. In the group of women, a sufficient level of oral/denture hygiene was noted more frequently than in men, 73.8% and 47.1%, respectively (P<0.001).
Dental treatment needs
Over half of the surveyed residents (59.8%) had objective dental treatment needs. Only 27% were aware of the need for treatment, and only 9.7% reported the need to the personnel. Residents were over-optimistic in the assessment of their oral health condition and dental needs compared to the objective needs identified during the clinical examination. Nearly every second elderly person having an objective serious need of dentures (54.4% of all respondents) was aware of the need and only one in seven reported it. Every third person found to have an objective need for the removal of one or more teeth was not aware of such need. Relatively little need for conservative treatment (3.5%) resulted from the small number of natural teeth (mean 5.6±7.3).
As expected, the level of hygiene determined the magnitude of individual needs. Patients with inadequate oral health were significantly more likely to have a need for removal of teeth and prosthetic treatment compared to those with acceptable oral hygiene, P=0.006 and P=0.037, respectively (Table 3).
Oral/denture hygiene practices
Among people with dentures, 44.3% cleaned it at least twice a day (Figure 1) and only every third person (34.7%) cleaned their natural teeth at least twice a day (Figure 2).
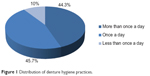  | Figure 1 Distribution of denture hygiene practices. |
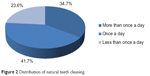  | Figure 2 Distribution of natural teeth cleaning. |
The effectiveness of plaque removal by the elderly people was low. Of those cleaning teeth and/or dentures at least twice a day with a toothbrush and fluoride toothpaste, almost every third person (29.5%) had an insufficient level of oral hygiene (MPS >4) (Table 3).
Every fourth person (25.9%) was aware of his/her own limited ability to properly clean his/her teeth and/or dentures, and would like to be helped with teeth cleaning. The impaired tooth cleaning ability was in the first place due to restricted mobility (17.4%), followed by reduced manual dexterity (5.8%), or both at the same time (2.7%).
People with considerable difficulty in cleaning their teeth were asked about the availability of the aid from both the staff and family members. Unfortunately, only every third person (35.8%) expressing such need might hope to receive such aid. Every fifth person (19.4%) expecting help in cleaning their teeth is helped by visitors and relatives, while only every tenth is aided by a medical nurse or caregiver. The remaining 73% of the respondents declared that they did not need help. In the group of people who did not perceive themselves to be restricted in their cleaning abilities, 54.7% were cleaning their teeth and/or dentures at least twice a day with a brush and toothpaste. However, as many as 26% of those “fully operational tooth cleaners” cleaning their teeth at least twice a day with a brush and toothpaste were also found to have an insufficient level of oral hygiene. An insufficient level of oral hygiene was also found in nearly half (45.8%) of those patients who were helped with cleaning their teeth (Table 2).
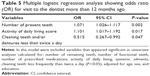
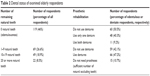
Dental care utilization and barriers to dental care use
The frequency of elderly care home residents’ visits to the dentist was also unsatisfactory. Seventy-five percent of the respondents had not visited the dentist’s studio in the past 12 months (Figure 3). The main reason mentioned by the residents was the difficulty in organizing visits, underestimation of the dental problem, and no awareness of the needs (Table 4). At a higher risk of failing to visit the dentist within the last 12 months were respondents with fewer remaining teeth, with less activities of daily living, and cleaning teeth and/or dentures less frequently than twice a day (Table 5).
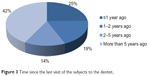  | Figure 3 Time since the last visit of the subjects to the dentist. |
  | Table 4 Main reason for not visiting the dentist within the last 12 months mentioned by the respondents (n=193) |
The last visit to the dentist was most frequently associated with: making prostheses (43.2%) or immediate treatment (52%) (Figure 4). In contrast, a check-up was the reason for visiting the dentist for only 4.2% of respondents.
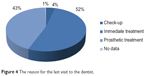  | Figure 4 The reason for the last visit to the dentist. |
Discussion
The prevalence of edentulism in the group of institutionalized elderly people (45.95%) was similar to the results in the group of 65 years and older participants of the National Monitoring of Oral Health in Poland study of 2009 (43.9%).37 In the study population, the proportion of institutionalized elderly edentulous people was higher than the number of edentulous people currently recorded in similar populations in other European countries, where the proportion of those people ranges from 26.9% to 35.8%. In addition, the average number of teeth present in our study population was lower than in the institutionalized elderly population in other developed countries.24,30–33 The target for the year 2000 – a 25% reduction in edentulousness at age 65 and over compared with the 1982 level – has not been achieved,34 and indeed there has been an alarming trend of a growing proportion of edentulous people during the last two decades.35–37 The continuing increase in the percentage of edentulous persons aged 65 years and older and very low average number of natural teeth reflect deteriorating accessibility of free-of-charge dental services (only 16% of the costs of dental care is covered by public funds), while no incentives are undertaken to improve oral health.
The proportion of edentulous people who did not use dentures was similar to that recorded currently among institutionalized elderly people in Turkey or to that recorded 24 years ago in Finland.38,39
Poor oral hygiene was found in a significant proportion of people cleaning their teeth at least twice a day. Therefore, elderly people need assistance in oral hygiene measures and regular contact with a dental specialist (dentist or dental hygienist). This study also revealed the lack of involvement, as part of their daily duties, of nurses and medical caregivers to help care home residents in their oral health care activities. Adequate oral care in elderly care home residents has continued to be a problem in many countries.24,40 This is a result of poor knowledge of, and wrong attitudes to, oral hygiene, as well as improper organization of work or insufficient time. The improvement of oral health care provided by the staff of the care homes depends on nurses’ education and organization strategies to provide more time for oral care.41 In Poland, even in routine training of nurses and caregivers, there is no instruction on oral health care; it is not specified in terms of daily duties.
Only 7% of the Polish gross domestic product is allocated to the health care system, and public expenditure on health care amounts to 995 US dollar purchasing power parity, of which only 3% (approximately 25 US dollars per capita/year) is spent on dental care.42 The existing common health insurance fund finances, among other things, annual check-up, removal of teeth, and upper and lower mucous membrane-supported dentures provided every 5 years by the facilities operated within the National Health Fund. Despite the fact that in terms of health expenditures, Poland occupies one of the last places among European Union countries, the financial barrier is mentioned relatively rarely, unlike in the elderly populations of most European countries.
The problem of ensuring adequate dental care in care homes affects every country, but in Poland, in addition to the lack of training of nursing staff in the field of oral hygiene, one of the lowest European financial resources allocated to the operation of permanent care facilities certainly constitutes the major barrier. Residents of Polish state-run care homes, in exchange for 70% of their income, are provided with bed and board, nursing and medical care of a physician or geriatrician, and rehabilitation. Other essential health needs of care home residents (including dental care) are provided by facilities located outside the care homes, unlike in other developed countries, such as the UK, where dental care is provided by a salaried or domiciliary dentist.29 None of the elements of dental care are provided on the spot in Polish care homes, nor is there any facility that collaborates on a permanent basis with the care homes. Access to dental care is limited for organizational reasons: the necessary transport generates costs that must be paid by the care homes, thus limiting the resources available for other purposes. The needs of dental treatment are regarded as secondary and the problem is usually solved “on an emergency basis”, eg, by transporting the care home resident to the dental facility to extract the aching tooth.
The disproportion between the serious objective needs, especially in the field of prosthetic treatment, and small needs experienced and expressed by care home residents results both from low dental health awareness among the elderly people as well as ignoring the dental needs by care home personnel. In the Polish model of dental care, among other things, due to financial constraints, no dental programs, even those limited to periodic inspection of oral health and education in the field of oral hygiene, are currently being implemented. The circumstances in which the present study was conducted seem to validate the claim that the suggestion to perform oral examination in the residents’ rooms, or even directly at the bed of a severely disabled person was positively received by both the residents themselves and the staff. Group education sessions arranged immediately after completion of the study in individual rooms and the lounge in each nursing home were received with equal enthusiasm.
The very low expenditures on dental care for the elderly can be regarded as an objective system-related barrier difficult to overcome at the present stage of Poland’s socio-economic transformation. This does not mean, however, that even considering the very low level of the financial outlays, it is completely impossible to overcome the obstacles, implement education programs, and motivate residents to obey the fundamental principles of oral hygiene.
Conclusion
In the study group of elderly institutionalized people, the proportion of edentulous people and those requiring prosthetic treatment is very high. In Poland, which is a medium-developed country, a low average level of dental care results from low-level financing of the Polish health care system. This, however, does not mean that even in the current poor economic conditions, it is impossible to improve dental awareness of both the residents of care homes and their professional medical caregivers. The improvement is also possible through the inclusion of dental check-ups into the schedule of general medical examinations of the residents performed once a year.
Disclosure
The study was funded by the Medical University of Lodz internal grant number 502-03/6-024-01/502-64-073. The authors declare no conflicts of interest in this work.
References
Petersen PE, Yamamoto T. Improving the oral health of older people: the approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol. 2005;33(2):81–92. | ||
Kandelman D, Petersen PE, Ueda H. Oral health, general health, and quality of life in older people. Spec Care Dentist. 2008;28(6):224–236. | ||
Marino R, Schoefeld M, Wright C, Calache H, Minichiello V. Self-reported and clinically determined oral health status predictors for quality of life in dentate older migrant adults. Community Dent Oral Epidemiol. 2008;36(1):85–94. | ||
Tsakos G, Steele JG, Marcenes W, Wallas AW, Sheiham A. Clinical correlates of oral health-related quality of life: evidence from national sample of British older people. Eur J Oral Sci. 2006;114(5):391–395. | ||
Kelsey JL, Lamster IB. Influence of musculoskeletal conditions on oral health among older adults. Am J Public Health. 2008;98(7): 1177–1183. | ||
Hämäläinen P, Rantanen T, Keskinen M, Meurman JH. Oral health status and change in handgrip strength over a 5-year period in 80-year-old people. Gerodontology. 2004;21(3):155–160. | ||
Ohrui T, Matsui T, Yoshida M, et al. Dental status and mortality in institutionalized elderly people. Geriatr Gerontol Int. 2006;6(2):101–108. | ||
Polzer I, Schimmel M, Müller F, Biffar R. Edentulism as part of the general health problems of elderly adults. Int Dent J. 2010;60(3): 143–155. | ||
Pihlstrom BL, Michalowicz BS, Johnson NW. Periodontal diseases. Lancet. 2005;366(9499):1809–1820. | ||
Blaizot A, Vergnes JN, Nuwwareh S, Amar J, Sixou M. Periodontal diseases and cardiovascular events: meta-analysis of observational studies. Int Dent J. 2009;59(4):197–209. | ||
Preshaw PM, Alba AL, Herrera, D et al. Periodontitis and diabetes: a two-way relationship. Diabetologia. 2012;55(1):21–31. | ||
Azarpazhooh A, Leake JL. Systematic review of the association between respiratory diseases and oral health. J Periodontol. 2006;77(9): 1465–1482. | ||
Russell SL, Boylan RJ, Kaslick RS, Scannapieco FA, Katz RV. Respiratory pathogen colonization of the dental plaque of institutionalized elders. Spec Care Dentist. 1999;19(3):128–134. | ||
Wang Z, Zhou X, Zhang J, et al. Periodontal health, oral health behaviours, and chronic obstructive pulmonary disease. J Clin Periodontol. 2009;36(9):750–755. | ||
Attin T, Hornecker E. Tooth brushing and oral health: how frequently and when should tooth brushing be performed? Oral Health Prev Dent. 2005;3(3):135–140. | ||
Hancock EB, Newell DH. Preventive strategies and supportive treatment. Periodontol 2000. 2001;25:59–76. | ||
Forsell M, Sjogren P, Johannson O. Need of assistance with daily oral hygiene measures among nursing home resident elderly versus the actual assistance received from the staff. Open Dent J. 2009;3:241–244. | ||
Mello AL, Erdmann AL, Brondani M. Oral health care in long-term care facilities for elderly people in southern Brazil: a conceptual framework. Gerodontology. 2010;27(1):41–46. | ||
Montal S, Tramini P, Triay JA, Valcarcel J. Oral hygiene and the need for treatment of the dependent institutionalized elderly. Gerodontology. 2006;23(2):67–72. | ||
Samson H, Strand GV, Haugejorden O. Change in oral health status among institutionalized Norwegian elderly over a period of 16 years. Acta Odontol Scand. 2008;66(6):368–373. | ||
Sweeney MP, Williams C, Kennedy C, Macpherson LM, Turner S, Bagg J. Oral health care and status of elderly care home residents in Glasgow. Community Dent Health. 2007;24(1):37–42. | ||
Unluer S, Gokalp S, Dogan BG. Oral health status of the elderly in a residential home in Turkey. Gerodontology. 2007;24(1):37–42. | ||
Belsi A, Gonzalez-Maffe J, Jones K, Wright D, Gallagher JE. Care home managers’ views of dental services for older people living in nursing and residential homes in inner city London. Community Dent Health. 2013;30(2):77–82. | ||
Willumsen T, Karlsen L, Naess R, Bjorntvedt S. Are the barriers to good oral hygiene in nursing homes within the nurses or the patients. Gerodontology. 2012;29(2):e748–e755. | ||
Barczak K. Stan zebow i przyzebia u seniorow z domow pomocy spolecznej i domow rodzinnych w wojewodztwie pomorskim. [The condition of teeth and periodontium in the elderly from social care centers and family-run care homes in the province of West Pomerania]. Ann Acad Med Stetin. 2011;57(2):104–109. Polish. | ||
Blaszczak J. Clinical assessement of dental status and Candida albicans presence in care home residents in Lublin [doctoral thesis]. Medical University, Lublin; 2011. | ||
stat.gov.pl [homepage on the Internet]. Statistical yearbook of Poland 2010. Available from: http://www.stat.gov.pl/gus/roczniki_PLK_HTML.htm. Accessed April 29, 2014. | ||
World Health Organization. Oral Health Surveys: Basic Methods, 4th Ed. Geneva: World Health Organization, 1997:21–52. | ||
Henriksen BM, Ambjarrnsen E, Axell TE. Evaluation of a mucosal-plaque index (MPS) designed to assess oral care in groups of elderly. Spec Care Dentist. 1999;19(4):154–157. | ||
Petelin M, Cotič J, Perkič K, Pavlič A. Oral health of the elderly living in residential homes in Slovenia. Gerodontology. 2012;29(2):e447–e457. | ||
Marin-Zuluaga DJ, Sandvik L, Gil-Montoya JA, Willumsen T. Oral health and mortality risk in the institutionalised elderly. Med Oral Patol Oral Cir Bucal. 2012;17(4):e618–e623. | ||
Tramini P, Montal S, Valcarcel J. Tooth loss and associated factors in long-term institutionalised elderly patients. Gerodontology. 2007; 24(4):196–203. | ||
Bøge Christensen L, Hede B, Nielsen E. A cross-sectional study of oral health and oral health-related quality of life among frail elderly persons on admission to a special oral health care programme in Copenhagen City, Denmark. Gerodontology. 2012;29(2):e392–e400. | ||
No authors listed. Global goals for oral health by the year 2000. Federation Dentaire Internationale. Int Dent J. 1982;32(1):74–77. | ||
Wierzbicka M, Szatko F, Radziejewska M, et al. Nationwide Monitoring of Oral Health Status of 1998. Report prepared for Ministry of Health. Warsaw, Ministry of Health, 1998 (in Polish). | ||
Wierzbicka M, Szatko F, Zawadziński M, et al. Nationwide Monitoring of Oral Health Status of 2002. Report prepared for Ministry of Health. Warsaw, Ministry of Health, 2003 (in Polish). | ||
Jodkowska E, Wierzbicka M, Szatko F, et al. Nationwide Monitoring of Oral Health Status and Its Conditioning of 2009. Report prepared for Ministry of Health. Warsaw, Ministry of Health, 2009 (in Polish). | ||
Ozkan Y, Özkan M, Kulak Y, Kazazoglu E, Arikan A. General health, dental status and perceived dental treatment needs of an elderly population in Istanbul. Gerodontology. 2011;28(1):28–36. | ||
Ekelund R. Dental state and subjective chewing ability of institutionalized elderly people. Community Dent Oral Epidemiol. 1989; 17(1):24–27. | ||
Nicol R, Sweeney MP, McHugh S, Bagg J. Effectiveness of health care worker training on the oral health of elderly residents of nursing homes. Community Dent Oral Epidemiol. 2005;33(2):115–124. | ||
Willumsen T, Frenkel H, Harvey I, Newcombe RG. Improving oral health in institutionalized elderly people by educating caregivers: a randomized controlled trial. Community Dent Oral Epidemiol. 2001; 29(4):289–297. | ||
Wojtyniak B, Gorynski P, Moskalewicz B. Health status report and its conditioning 2012. Narodowy Instytut Zdrowia Publicznego. Available from: http://www.pzh.gov.pl/page/fileadmin/user_upload/statystyka/Raport_stanu_zdrowia_2012.pdf. Accessed April 30, 2014. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.