Back to Journals » Clinical Interventions in Aging » Volume 11
Lifestyle and lifestyle-related comorbidities independently associated with colorectal adenoma recurrence in elderly Chinese people
Received 31 January 2016
Accepted for publication 11 March 2016
Published 17 June 2016 Volume 2016:11 Pages 801—805
DOI https://doi.org/10.2147/CIA.S105472
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Zhi-Ying Wu
Adake Saiken, Fang Gu
Department of Gastroenterology, Peking University Third Hospital, Beijing, People’s Republic of China
Objective: The purpose of this study was to determine the lifestyle and lifestyle-related comorbidities independently associated with colorectal adenoma (CRA) recurrence in elderly Chinese people.
Methods: During the 5-year follow-up after the initial colonoscopy, participants aged >60 years with the diagnosis and removal of CRA underwent a complete surveillance colonoscopy, and 152 participants with CRA recurrence plus 152 participants free of recurrence were included in this analysis.
Results: Participants with CRA recurrence were more likely to consume less vegetables and fruits, and more red meats compared with the control group (P<0.05 for all). Lifestyle-related comorbidities, including hypertension and nonalcoholic fatty liver disease (NAFLD), were more common in participants with CRA recurrence than in the control group (P<0.05 for all). In the multivariate analysis, pack-years of smoking were independently associated with an increased CRA recurrence (odds ratio [OR]: 1.03; P<0.05). Eating less vegetables (OR: 099; P<0.05) and fruits (OR: 0.98; P<0.05) was identified as a statistically independent factor influencing CRA recurrence, as was eating more red meats (OR: 1.01; P<0.05). Hypertension was also found to be a factor independently associated with an increased CRA recurrence (OR: 2.44; P<0.05). NAFLD had an independent association, with an increased CRA recurrence (OR: 3.43; P<0.05).
Conclusion: Smoking cigarettes, high consumption of red meats, low intake of fruits and vegetables, and the presence of hypertension and NAFLD were independently associated with an increased CRA recurrence in elderly Chinese people. This conclusion helps elderly Chinese people to make effective behavioral changes, such as smoking cessation, substitution of fruits and vegetables for red meats, and timely treatment of hypertension and NAFLD, to reduce CRA recurrence and colorectal cancer risk.
Keywords: elderly Chinese, colorectal adenoma recurrence, lifestyle, lifestyle-related comorbidities
Introduction
Colorectal cancer (CRC) is a common lethal malignancy in the People’s Republic of China and other countries.1,2 Mortality caused by CRC in the West is declining, but there is a rapidly rising trend in the People’s Republic of China.3 In view of the adenoma–carcinoma sequence, colorectal adenomas (CRAs) are the precursor lesions of CRC, and CRA recurrence serves as an informative end point for colorectal carcinogenesis because it shares common etiopathogenesis with CRC.4 Colonoscopic removal of CRAs not only reduces the prevalence of CRC but also decreases deaths from CRC, and identifying the possible factors associated with CRA recurrence has become important to prevent, detect, and remove CRAs.5,6 Lifestyle characterized by smoking cigarettes, high consumption of red meats, and low intake of fruits and vegetables has been suggested to be associated with an increased risk for CRA and CRC.7–9 However, other studies have reported inconsistent results regarding these associations.10,11 Meanwhile, several lifestyle-related diseases, such as hypertension and nonalcoholic fatty liver disease (NAFLD), have been related to CRAs and CRC, and most cases of CRA and CRC occur in elderly people who commonly have these lifestyle-related comorbidities,12,13 but previous studies have shown insignificant associations.14 Although prior studies have demonstrated an increased prevalence of CRC associated with aging in elderly people, few studies have investigated whether lifestyle and lifestyle-related comorbidities were linked to CRA recurrence in elderly people.1,5 Additionally, in elderly Chinese people, little is known about lifestyle and lifestyle-related comorbidities correlating highly with CRA recurrence. Hence, the purpose of this study was to determine the lifestyle and lifestyle-related comorbidities independently associated with CRA recurrence in elderly Chinese people.
Methods
Study participants
CRAs were diagnosed and removed through a complete colonoscopy in individuals aged >60 years at Peking University Third Hospital between May 2009 and December 2009. The colonoscopy technique required the colonoscopy up to the level of the cecum, good bowel preparation, and removal of all the detected CRAs >5 mm in size.15 Participants were excluded for the following reasons: inflammatory bowel disease, appendectomy, familial adenomatous polyposis, hereditary nonpolyposis CRC, colorectal resection, no data available, or life expectancy <2 years because of severe infection, liver dysfunction, renal dysfunction, or cancer. During the 5-year follow-up after the initial colonoscopy, these participants underwent a complete surveillance colonoscopy, and 152 participants with CRA recurrence plus 152 participants free of recurrence were included in this analysis. The study protocol was approved by the Ethics Committee of Peking University Third hospital and performed according to the Declaration of Helsinki. Each participant provided written informed consent to be included in the study.
Information acquisition and diagnostic criteria
Participants responded to a questionnaire regarding demographic details, family histories, and lifestyle characteristics, and then all the responses were assessed by the research group. Dietary intake was assessed by an experienced dietitian. Red meats were defined as beef, lamb, or pork. Pack-years of smoking were calculated according to the total duration of regular cigarette smoking and packs of cigarettes smoked per day. Alcohol intake was calculated according to the equivalent of ethanol grams for each alcoholic beverage. Anthropometric measurements, including height, weight, waist circumference (WC), and blood pressure, were taken by experienced nursing staff. Height was measured using a wall-mounted measuring tape with individuals wearing light clothing and no shoes, and weight was measured using a digital scale. Body mass index was calculated as weight divided by height squared (kg/m2). WC was measured on standing subjects with a nonmetallic, constant-tension tape placed around the body at the midpoint between the lowest ribs and iliac crests. Participants with blood pressure >140/90 mmHg or taking antihypertensive therapy were considered to have hypertension.16 Dyslipidemia was diagnosed when participants had triglyceride >1.70 mmol/L, low-density lipoprotein cholesterol >3.37 mmol/L, and high-density lipoprotein cholesterol >1.04 mmol/L.17 Participants with fasting blood glucose >7.0 mmol/L, postprandial blood glucose >11.1 mmol/L, or taking antidiabetic therapy were defined as having diabetes mellitus.18 Colonoscopy was carried out by a skilled gastroenterologist, and colonoscopic findings, including size and number, were recorded. An experienced pathologist confirmed the diagnosis of CRAs by histological examination after colonoscopic polypectomy.19 Whether the size of CRAs was >1 cm or not; number of CRAs was >3 or not; and pathologic type of CRAs was tubular adenoma or others were checked. Liver ultrasound examination was conducted by an experienced sonographer, and NAFLD was diagnosed if the contrast between the liver and parenchyma of the right kidney was increased without viral, autoimmune, alcoholic, or other liver diseases.13
Statistical methods
Descriptive statistics were carried out to characterize the participants with and without CRA recurrence. Student’s t-test or Mann–Whitney U-test was carried out for difference in mean (with standard deviation) or median (with interquartile range) and chi-square test for comparison of proportion. Multivariate analysis was carried out by multiple logistic regression analysis (backward stepwise), and the result was presented as odds ratio (OR) with 95% confidence interval. All statistical analyses were carried out using SPSS Version 17.0 statistical software (SPSS Inc., Chicago, IL, USA). A two-tailed P-value <0.05 represented statistical significance.
Results
Participants had a median age of 65 years (range 60–87 years) at baseline, with 63.8% being male (194 participants). Baseline characteristics of the study participants with and without CRA recurrence are provided in Table 1. No difference in age, sex, and family history was seen between the two groups (P>0.05 for all). Participants with CRA recurrence had higher body mass index and WC than the control group (P<0.05 for all). Pack-years of smoking (P<0.05) rather than drinking (P>0.05) differed significantly between the two groups. Participants with CRA recurrence were more likely to consume less vegetables and fruits and more red meats compared with the control group (P<0.05 for all). Lifestyle-related comorbidities, including hypertension, dyslipidemia, and NAFLD (P<0.05 for all) but not diabetes mellitus (P>0.05), were more common in participants with CRA recurrence than the control group. All adenoma-related factors, such as the maximum diameter of CRAs >1 cm, the number of CRAs >3, and the pathological types of CRAs other than tubular adenoma, tended to exist in participants with CRA recurrence rather than the control group (P<0.05 for all).
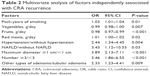
In the multivariate analysis, pack-years of smoking was independently associated with an increased CRA recurrence (OR: 1.03; P<0.05). Eating less vegetables (OR: 099; P<0.05) and fruits (OR: 0.98; P<0.05) was identified as a statistically independent factor influencing the CRA recurrence, as was eating more red meats (OR: 1.01; P<0.05). Hypertension was also found to be a factor independently associated with an increased CRA recurrence (OR: 2.44; P<0.05). NAFLD had an independent association with an increased CRA recurrence (OR: 3.43; P<0.05). With regard to the adenoma-related factors, participants with the maximum diameter of CRAs >1 cm (OR: 3.89; P<0.05) and the number of CRAs >3 (OR: 3.46; P<0.05) were at increased CRA recurrence. Participants with other types of adenoma except tubular adenoma experienced an increased CRA recurrence (OR: 2.33; P<0.05). OR and P-value of each factor with multivariate analysis are shown in Table 2.
Discussion
Lifestyle and lifestyle-related comorbidities have generated interest because their associations with CRA recurrence shed more light on the prevention of CRC. During the 5-year follow-up, this study confirmed that smoking cigarettes, high consumption of red meats, low intake of fruits and vegetables, and the presence of hypertension and NAFLD were independently associated with an increased CRA recurrence after the diagnosis and removal of CRAs at the initial colonoscopy in elderly Chinese people.
Associations of CRA and CRC development with low intake of fruits and vegetables have been observed in some but not all studies.20–23 The current data proved the independent associations of CRA recurrence with low intake of both the fruits and vegetables among elderly Chinese people, and adjustment for other lifestyle and lifestyle-related factors did not significantly alter these associations with low intake of fruits and vegetables, suggesting that fruits and vegetables not only are the markers for healthier lifestyle but also confer protection against future CRA recurrence as good sources of various antioxidant vitamins, dietary fiber, folate, and flavonoids themselves.24,25 These ingredients play a role in modulating DNA methylation, protecting from DNA damage, promoting apoptosis, and inducing detoxifying enzymes.26
Some previous studies have provided some evidence for the associations of CRAs and CRC with intake of red meat, but other studies provided opposite results.27,28 In this study, high consumption of red meat was reported as an independent factor associated with CRA recurrence. Heterocyclic amines, N-nitroso compounds, and other related substances that are formed during the cooking process of red meats result in the development of CRAs and CRC.29
Several studies have examined the associations of smoking cigarettes with CRAs and CRC and realized that exposure to smoking significantly increases the prevalence, size, and number of CRAs and CRC, but other studies supported that smoking is not a strong factor correlated with CRA and CRC development.30–32 The current results pointed out that cigarette smoking had an independent association with CRA recurrence. Cigarette smoking causes oxidative stress and DNA damage in the body.33
Hypertension appeared to be related to CRA and CRC formation in previous studies, but other studies obtained conflicting finding.13,34 Meanwhile, some studies that evaluated CRA recurrence did not pay any attention to hypertension as a relevant factor for analysis.35 This study concluded that hypertension had an independent relationship with CRA recurrence, but the possible interaction between hypertension and CRA recurrence remains unclear and needs further elucidation.
There exists a strong relationship between the intestine and liver.36 Previous clinical researches have already discovered that patients with NAFLD had the higher prevalence of CRAs and CRC.13 Suggestion from data recently indicated that NAFLD was a potential factor associated with CRAs, but this point still remains controversial.37 Not only do they have the same origin in embryology, but the liver also continuously receives intestinal blood through the portal system. An independent correlation between NAFLD and CRA recurrence was noted in this study, and its underlying mechanism is still uncertain. The effects of leptin and adipokines are the possible mechanisms responsible for the interaction between NAFLD and CRA recurrence.38,39
Conclusion
The current findings demonstrated that smoking cigarettes, high consumption of red meats, low intake of fruits and vegetables, and the presence of hypertension and NAFLD were independently associated with an increased CRA recurrence in elderly Chinese people. This conclusion helps elderly Chinese people to make effective behavioral changes, such as smoking cessation, substitution of fruits and vegetables for red meats, and timely treatment of hypertension and NAFLD, to reduce the CRA recurrence and CRC risk.
Disclosure
The authors report no conflicts of interest in this work.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65(1):5–29. | ||
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127(12):2893–2917. | ||
Sung JJ, Lau JY, Young GP, et al; Asia Pacific Working Group on Colorectal Cancer. Asia Pacific consensus recommendations for colorectal cancer screening. Gut. 2008;57(8):1166–1176. | ||
Leslie A, Carey FA, Pratt NR, Steele RJ. The colorectal adenoma-carcinoma sequence. Br J Surg. 2002;89(7):845–860. | ||
Zauber AG, Winawer SJ, O’Brien MJ, et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med. 2012;366(8):687e96. | ||
Levin B, Lieberman DA, McFarland B, et al; American Cancer Society Colorectal Cancer Advisory Group; US Multi-Society Task Force; American College of Radiology Colon Cancer Committee. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Gastroenterology. 2008;134(5):1570–1595. | ||
Magalhaes B, Peleteiro B, Lunet N. Dietary patterns and colorectal cancer: systematic review and meta-analysis. Eur J Cancer Prev. 2012;21(1):15–23. | ||
Chan DS, Lau R, Aune D, et al. Red and processed meat and colorectal cancer incidence: meta-analysis of prospective studies. PLoS One. 2011;6(6):e20456. | ||
Botteri E, Iodice S, Bagnardi V, Raimondi S, Lowenfels AB, Maisonneuve P. Smoking and colorectal cancer: a meta-analysis. JAMA. 2008;300(23):2765–2778. | ||
Yang B, Thyagarajan B, Gross MD, Fedirko V, Goodman M, Bostick RM. No evidence that associations of incident, sporadic colorectal adenoma with its major modifiable risk factors differ by chromosome 8q24 region rs6983267 genotype. Mol Carcinog. 2014;53(suppl 1):E193–E200. | ||
Wark PA, Van der Kuil W, Ploemacher J, et al. Diet, lifestyle and risk of K-ras mutation-positive and -negative colorectal adenomas. Int J Cancer. 2006;119(2):398–405. | ||
Klabunde CN, Legler JM, Warren JL, Baldwin LM, Schrag D. A refined comorbidity measurement algorithm for claims-based studies of breast, prostate, colorectal, and lung cancer patients. Ann Epidemiol. 2007;17(8):584–590. | ||
Huang KW, Leu HB, Wang YJ, et al. Patients with non-alcoholic fatty liver disease have higher risk of colorectal adenoma after negative baseline colonoscopy. Colorectal Dis. 2013;15(7):830–835. | ||
Liu CS, Hsu HS, Li CI, et al. Central obesity and atherogenic dyslipidemia in metabolic syndrome are associated with increased risk for colorectal adenoma in a Chinese population. BMC Gastroenterol. 2010;10:51. | ||
Paggi S, Rondonotti E, Amato A, et al. Resect and discard strategy in clinical practice: a prospective cohort study. Endoscopy. 2012;44(10):899–904. | ||
Chobanian AV, Bakris GL, Black HR, et al; Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42(6):1206–1252. | ||
Joint Committee for Developing Chinese guidelines on Prevention and Treatment of Dyslipidemia in Adults. Chinese guidelines on prevention and treatment of dyslipidemia in adults. Zhonghua Xin Xue Guan Bing Za Zhi. 2007;35(5):390–419. | ||
Genuth S, Alberti KG, Bennett P, et al; Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care. 2003;26(11):3160–3167. | ||
Lieberman DA, Rex DK, Winawer SJ, et al; United States Multi-Society Task Force on Colorectal Cancer. Guidelines for colonoscopy surveillance after screening and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2012;143(3):844–857. | ||
Millen AE, Subar AF, Graubard BI, et al; PLCO Cancer Screening Trial Project Team. Fruit and vegetable intake and prevalence of colorectal adenoma in a cancer screening trial. Am J Clin Nutr. 2007;86(6):1754–1764. | ||
Wu H, Dai Q, Shrubsole MJ, et al. Fruit and vegetable intakes are associated with lower risk of colorectal adenomas. J Nutr. 2009;139(2):340–344. | ||
Chiu BC, Gapstur SM. Changes in diet during adult life and risk of colorectal adenomas. Nutr Cancer. 2004;49(1):49–58. | ||
Michels KB, Giovannucci E, Chan AT, Singhania R, Fuchs CS, Willett WC. Fruit and vegetable consumption and colorectal adenomas in the Nurses’ Health Study. Cancer Res. 2006;66(7):3942–3953. | ||
George SM, Park Y, Leitzmann MF, et al. Fruit and vegetable intake and risk of cancer: a prospective cohort study. Am J Clin Nutr. 2009;89(1):347–353. | ||
Ben Q, Sun Y, Chai R, Qian A, Xu B, Yuan Y. Dietary fiber intake reduces risk for colorectal adenoma: a meta-analysis. Gastroenterology. 2014;146(3):689–699. | ||
Khuda-Bukhsh AR, Das S, Saha SK. Molecular approaches toward targeted cancer prevention with some food plants and their products: inflammatory and other signal pathways. Nutr Cancer. 2014;66(2):194–205. | ||
Ferrucci LM, Sinha R, Graubard BI, et al. Dietary meat intake in relation to colorectal adenoma in asymptomatic women. Am J Gastroenterol. 2009;104(5):1231–1240. | ||
Rohrmann S, Hermann S, Linseisen J. Heterocyclic aromatic amine intake increases colorectal adenoma risk: findings from a prospective European cohort study. Am J Clin Nutr. 2009;89(5):1418–1424. | ||
Alexander DD, Cushing CA. Red meat and colorectal cancer: a critical summary of prospective epidemiologic studies. Obes Rev. 2011;12(5):e472–e493. | ||
Shin A, Hong CW, Sohn DK, et al. Associations of cigarette smoking and alcohol consumption with advanced or multiple colorectal adenoma risks: a colonoscopy-based case-control study in Korea. Am J Epidemiol. 2011;174(5):552–562. | ||
Abrams JA, Terry MB, Neugut AI. Cigarette smoking and the colorectal adenoma-carcinoma sequence. Gastroenterology. 2008;134(2):617–619. | ||
Giovannucci E. An updated review of the epidemiological evidence that cigarette smoking increases risk of colorectal cancer. Cancer Epidemiol Biomarkers Prev. 2001;10(7):725–731. | ||
Ulvik A, Evensen ET, Lien EA, et al. Smoking, folate and methylenetetrahydrofolate reductase status as interactive determinants of adenomatous and hyperplastic polyps of colorectum. Am J Med Genet. 2001;101(3):246–254. | ||
Wong VW, Wong GL, Tsang SW, et al. High prevalence of colorectal neoplasm in patients with non-alcoholic steatohepatitis. Gut. 2011;60(6):829–836. | ||
Chung SJ, Kim YS, Yang SY, et al. Five-year risk for advanced colorectal neoplasia after initial colonoscopy according to the baseline risk stratification: a prospective study in 2452 asymptomatic Koreans. Gut. 2011;60(11):1537–1543. | ||
Miele L, Marrone G, Lauritano C, et al. Gut-liver axis and microbiota in NAFLD: insight pathophysiology for novel therapeutic target. Curr Pharm Des. 2013;19(29):5314–5324. | ||
Lin XF, Shi KQ, You J, et al. In-creased risk of colorectal malignant neoplasm in patients with nonalcoholic fatty liver disease: a large study. Mol Biol Rep. 2014;41(5):2989–2997. | ||
Oh JS, Kim HH, Hwang HS, et al. Comparison of blood leptin concentration and colonic mucosa leptin expression in colon adenoma patients and healthy control. Korean J Gastroenterol. 2014;63(6):354–360. | ||
Ding WJ, Wang Y, Fan JG. Regulation of adipokines by polyunsaturated fatty acids in a rat model of non-alcoholic steatohepatitis. Arch Iran Med. 2014;17(8):563–567. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.