Back to Journals » Drug Design, Development and Therapy » Volume 8
Exploratory meta-analysis on lisdexamfetamine versus placebo in adult ADHD
Authors Maneeton N , Maneeton B , Suttajit S, Reungyos J, Srisurapanont M , Martin S
Received 25 May 2014
Accepted for publication 30 July 2014
Published 3 October 2014 Volume 2014:8 Pages 1685—1693
DOI https://doi.org/10.2147/DDDT.S68393
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Shu-Feng Zhou
Narong Maneeton,1 Benchalak Maneeton,1 Sirijit Suttajit,1 Jirayu Reungyos,1 Manit Srisurapanont,1 Stephen D Martin2
1Department of Psychiatry, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand; 2Brandon Lane Neuropsychiatry Clinic, Durham, United Kingdom
Background: Recent studies have promised that lisdexamfetamine (LDX) is effective in the treatment of adults with attention-deficit hyperactivity disorder (ADHD).
Objectives: This systematic review was undertaken to summarize LDX efficacy, acceptability, and tolerability in adult ADHD. All randomized controlled trials (RCTs) of lisdexamfetamine compared with placebo were included for synthesis. Clinical trials published between January 1991 and January 2014 were evaluated.
Methods: The database of MEDLINE®, EMBASE™, CINAHL®, PsycINFO® and Cochrane Controlled Trials Register were searched in January 2014. Studies were also searched in ClinicalTrials.gov and the EU Clinical Trials Register database. Study eligibility criteria, participants, and interventions were considered. All RCTs of LDX vs placebo reporting final results of: 1) severity of ADHD symptoms and executive function deficit, 2) response or remission rates, 3) overall discontinuation rate, or 4) discontinuation rate due to adverse events were included. The language of the papers was not restricted. All abstracts of studies gathered from the database were examined. After excluding irrelevant trials, the full text version of relevant studies were assessed and extracted for outcomes of interest. Examination of risks of bias, based on the Cochrane bias assessment, was carried out. The efficacy outcomes consisted of the mean end point or change scores for ADHD rating scales, the response rate, and the remission rate. The overall discontinuation rate and the discontinuation rate due to adverse events were measured for acceptability and tolerability, respectively. A random effect model was applied for the synthesis of relative risks (RRs), and weighted mean differences or standardized mean differences (SMDs) with 95% confidence intervals (CIs).
Results: A total of 806 final study or safety participants were included. The dosage of lisdexamfetamine was 30 to 70 mg/day. The pooled mean scores of mean change and mean end point scores between LDX- and placebo-treated groups also had a significant difference (SMD [95% CI] of -0.97 [-1.15, -0.78], I2=18%). The pooled response rates for adult ADHD between the two groups had a significant difference (RR [95% CI] of 1.99 [1.50, 2.63], I2=0%). Based on the Behavior Rating Inventory of Executive Function – Adult version (BRIEF-A), the pooled end point mean scores for the Global Executive Composite (GEC) for the LDX-treated groups was greater than that of placebo-treated groups (MD [95% CI] of –9.20 [-14.11, -4.29], I2=34%). The pooled overall discontinuation rates between the two groups had no significant difference (RR [95% CI] of 0.82 [0.59, 1.14], I2=0%). Similarly, the pooled discontinuation rates due to adverse events between the two groups was not significantly different (RR [95% CI] of 1.77 [0.71, 4.40], I2=0%).
Conclusion: The number of included studies was limited (five RCTs), but based on this meta-analysis, LDX is efficacious and well tolerated in the treatment of adult ADHD. Additionally, it also improved the executive function deficits in this population. However, its acceptability is no higher than placebo. These findings should be carefully interpreted and considered as preliminary outcomes. To confirm these results, further studies are warranted. LDX is a viable alternative psychostimulant for adult ADHD.
Keywords: lisdexamfetamine, placebo, systematic review, adult ADHD, acceptability, tolerability
Background
Although its symptoms initially occur in early childhood and usually decline in adulthood, a symptom of inattention persisting through into adulthood is still common.1,2 Recent evidence suggests that adult attention-deficit hyperactivity disorder (ADHD) prevalence ranges from 2.5% to 4.4%.3,4 A previous study suggests that adult ADHD is associated with greater impairment in various areas of functioning.5
In addition to its inattention symptoms, frequently ADHD affects executive function.6,7 Therefore, adult ADHD patients may encounter several difficulties, including on-task behavior, academic achievement, and social functioning8,9 Recent evidence suggests that onset of ADHD in childhood may be associated with working disabilities in adults.10
Psychostimulants, including methylphenidate (MPH), dextroamphetamine, and mixed amphetamine salts are not only efficacious in the treatment of ADHD in children and adolescents but also, in adults.11,12 The novel psychostimulant, lisdexamfetamine (LDX), is also efficacious in the treatment of ADHD. After oral administration, LDX, an originally inactive molecule, is rapidly absorbed from the gastrointestinal tract and converted to l-lysine, a naturally occurring essential amino acid, and dextroamphetamine, which therapeutically affects ADHD symptoms.13 As a prodrug, LDX needs an enzyme in red blood cells to convert to the active form of amphetamine; therefore, it has less potential for abuse and diversion, and longer effect, as compared with other stimulants.14,15
The evidence suggests that LDX is an effective, safe, well-tolerated medication for children aged 6 to 12 years through to adulthood, with ADHD.16,17 Although some randomized controlled trials (RCTs) of LDX demonstrated its efficacy and tolerability, compared with placebo, in the treatment of adult ADHD,16,18–21 they had a limited sample size. Given small samples sizes in each trial, a systematic review, which is potentially more effective in calculating the true effect size, may be the method to determine the efficacy, acceptability, and tolerability of LDX.
The primary aim of this present meta-analysis was to examine the efficacy of LDX compared with placebo, in the treatment of adult ADHD. In addition, acceptability and tolerability of LDX were determined.
Methods
The first publication of LDX in the MEDLINE® search was in 2007; therefore, the related clinical trials were searched between January 2007 and January 2014.
Eligibility criteria
All RCTs of LDX compared with placebo performed regarding adult ADHD spectrum, and presenting scores of ADHD and executive function standard rating scales were included. In addition, response, remission, and discontinuation rates needed to be reported. ADHD may be viewed as a spectrum of disorders including ADHD, attention deficit disorder (ADD), hyperkinetic syndrome, and hyperkinetic reaction diagnosed by any set of criteria. The language of the papers was not an exclusion criterion.
Information sources
Searching, limited to “human”, was mainly carried out in MEDLINE, EMBASE™, CINAHL®, PsycINFO®, and the Cochrane Controlled Trials Register databases in January 2014. The ClinicalTrials.gov and EU Clinical Trials Register databases were also searched. Additionally, any article reference collected by any means was also applied. The relevant studies gathered in this review were either RCTs or clinical controlled trials (CCTs).
Searches
For optimal identification of the RCTs and CCTs, a searching strategy applied a combination of the following words and phrases: ([lisdexamfetamine] OR [Vyvanse]) AND ([attention-deficit hyperactivity disorder] OR [ADHD] OR [attention-deficit disorder] OR [hyperkinetic syndrome] OR [hyperkinetic reaction]). This strategy was used for searching all databases.
Study selection
To determine which studies conformed to the eligibility criteria, the abstracts, identified from the databases, were examined by the authors (NM and BM) independently. When attaining the full-text version of relevant articles, the authors then separately evaluated those studies. When disagreements took place, they were solved by consensus.
Data collection process
The first author (NM) extracted the relevant results into the data extraction form. Then, the second reviewer (BM) revised the extracted outcomes. All author disputes were also resolved by means of consensus.
Data items
The important extracted data gathered from all trials consisted of the following: 1) the evaluated details of the study validity; 2) basic characteristics of included subjects, criteria used for diagnosis, design of each trial, and exclusion and inclusion criteria; 3) forms, doses, and time course for LDX treatment; and 4) relevent outcomes used for synthesis. Additionally, the intention-to-treat results were also gathered.
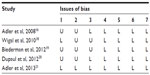
Risk of bias in individual studies
The internal validity (quality) was evaluated by the authors (NM and BM). According to the Cochrane Collaboration Handbook, risks of bias for individual study were assessed as follows: 1) the sequence of random generation; 2) allocation concealment, 3) blinding; 4) incomplete outcome; 5) selective reporting; 6) other sources of bias; and 7) baseline similarity.22
Summary measures
The essential criteria for inclusion in this analysis consisted of efficacy, acceptability and tolerability outcomes. The mean end point or mean change scores, based on the standardized ADHD measurement, and the rates of response and remission, evaluated by any set of criteria, were considered as efficacious outcomes. Acceptability and tolerability may be convertible terms; however, they individually have their specific definition. As in a previous meta-analysis, the acceptability in this review was assessed by the overall discontinuation rate,23 and the discontinuation rate due to adverse events – fundamentally evaluating the side effects – was defined as tolerability.24
Statistical analysis
To synthesize each continuous outcome, either weighted mean differences (WMD) or standardized mean differences (SMD) with the 95% confidence interval (CI) are regularly applied. When the same outcome measure across studies is applied, it is able to compare or combine the outcomes, by using the WMD. In cases where different measurements are used, a standardized value, for which there is no unit, is reasonably applied for those comparisons or combinations. In this review, therefore, either the WMDs or the SMDs were utilized for calculation, based on whether the included studies used the same or different rating scales. When the standard deviation (SD) of mean end point or mean change scores for ADHD rating scales in each study was not provided, it was estimated by performing direct substitution or any statistical method:25 All pooled mean end point or mean change scores with 95% CIs were estimated by using the inverse variance approach, and the significance of those scores as an effect estimation was calculated by using the Z-test.
As a rule, the dichotomous results were synthesized by using relative risks (RRs) with 95% CIs. When an RR is one, it suggests that there is no difference between two groups. In the case of an RR being less than one, it indicates that such outcome is less likely to occur. For the present review, the RRs were applied in the comparison of the response rates, remission rates, overall discontinuation rates, and discontinuation rates due to adverse events between two groups. All pooled RRs of dichotomous data, with 95% CIs, were calculated by using the Mantel–Haenszel approach, and estimation of the significance of those RRs as an effect was calculated by using the Z-test.
Synthesis of results
In general, synthesis for outcomes applies either a fixed or random effect(s) approach. When all included studies are speculated to contribute a common effect size, it is reasonable to apply the fixed effect model. This approach, contrasted to a random effects model, ignores the variations across various studies. Although the eligible studies are a relative similarity, it is not able to assume that they are entirely same since one true effect size less plausibly exists. Hence, it is unlikely to assume that those studies are exactly identical. By this reason, synthesis of all outcomes in the present review applied a random effects model.
Statistical software
In this review, the RevMan 5.1 (The Nordic Cochrane Centre, Copenhagen, Denmark) computer program was used for data synthesis.
Risk of bias across studies
A funnel plot is applied for detecting the publication bias in meta-analysis. It is a simple graph of the intervention effect, calculating from each trial against some measure of each trial’s size or precision.26 Consequently, we planned to use a funnel plot in this meta-analysis.
Test of heterogeneity
In general, use of a test of heterogeneity is necessary to determine the similarity of the study outcomes. We hypothesized that included study outcomes would not be the same effect due to the methodological quality in each trial. The extent of variation across the study outcomes was estimated. Based on the results outcomes presented by graphic display and the use of the test of heterogeneity, it was possible to estimate whether the study outcomes have greater differences than expected by chance alone. When an I2 is 50% or greater, a significant heterogeneity of outcome is recognized.
Results
Study selection
According to the searches from those databases, 260 citations were gathered (MEDLINE =50 studies, EMBASE =59 studies, PsycINFO =47 studies, CINAHL =5 studies, Cochrane Controlled Trials Register =69 studies, ClinicalTrials.gov =25 studies, and EU Clinical Trials Register =5 studies) (Figure 1). After the duplicate articles were removed, 185 studies were taken into account. Based on assessment of the titles and abstracts of the remaining articles, 175 studies were excluded since they did not meet the eligibility criteria. Ten full articles were thoroughly examined. Five more articles were excluded, since three were the post hoc analysis using data from previous studies,27–29 one had a randomized withdrawal study design,30 and one did not report the outcomes of interest applied for this analysis.9 Then, five studies were included in this review. There were no relevant and unpublished trials that met the eligibility criteria.
  | Figure 1 Flow diagram of study. |
Study characteristics
The duration of the five included studies ranged from 4 to 14 weeks.16,18–21 The washout periods were reported in three trials (1–6 weeks).16,18,21 Of 806 final study or safety population participants, 56.08% were male. Mean ages (SDs) for the LDX and placebo groups were 32.70 (10.72) years and 30.83 (10.99) years, respectively. The dosage of LDX was 30 to 70 mg/day. The baseline characteristics of participants in the included studies are presented in Table 1.
The SMDs were applied for calculation and synthesis, since mean end point and change scores were assessed by using the different ADHD rating scales across the studies. Mean end point or mean change scores were found in four studies,16,18,20,21 response rates were reported in two studies,16,20 and remission rate was presented in one study.16 However, overall discontinuation rates and discontinuation due to adverse events were found in four studies.16,19–21
Risk of bias within studies
The randomization, double-blind technique was applied in all eligible studies. Two trials used double-blind, crossover study designs.18,20 An intention-to-treat analysis was applied in two studies.16,18 A sequence generation of randomization was presented in one trial.21 Additionally, allocation concealment was reported in two trials18,21 and blinding of outcome assessment was reported in three trials.16,20,21 The rest of the biases were reported in all studies (Table 2).
Results of individual studies
Since two studies used several doses of LDX (30, 50, and 70 mg), pooled mean change scores (SD) of those studies were used for this analysis and synthesis.16,20 The mean end point or mean change scores of the ADHD Rating Scale version IV (ADHD-RS-IV) or Conners Adult ADHD Rating Scale (CAARS), short form in each study were significantly different between LDX- and placebo-treated groups (Figure 2). Similarly, the response rate of adult ADHD was significantly different between the two groups (Figure 3). The remission rate, gathered from only one study, showed a significant difference between the two groups (RR [95% CI] of 2.82 [1.58, 5.03]).
Synthesis of results
Efficacy
A significant heterogeneity was not found in all efficacious outcomes, except for the Behavioral Regulation Index (BRI). The pooled mean change ADHD-RS-IV scores of adult ADHD between LDX- and placebo-treated groups had a significant difference (SMD [95% CI] of −0.85 [−1.07, −0.64], I2=0%). In addition, the pooled end point mean ADHD-RS-IV and CAARS scores between the two groups were also significantly different (SMD [95% CI] of −1.14 [−1.41, −0.88], I2=0%). The pooled mean score of mean change and mean end point scores between two groups had also a significant difference (SMD [95% CI] of −0.97 [−1.15, −0.78], I2=18%) (Figure 2).
The pooled response rates for adult ADHD between LDX- and placebo-treated groups had a significant difference (RR [95% CI] of 1.99 [1.50, 2.63], I2=0%) (Figure 3). Based on its pooled response rates, the number need to treat (NNT) (95% CI) was 4 (2.2, 4.5). Unfortunately, only one study reported remission rates,16 and its pooled remission rate could not be calculated.
The self-reported BRIEF-A consists of two subscales, including the BRI and Metacognition Index (MI). The summation of the BRI and MI provides an overall index, called the Global Executive Composite.20,21 The pooled mean end point scores of the BRI and MI for the LDX-treated groups was greater than that of placebo-treated groups, with MD (95% CI) of −6.52 (−12.45, −0.60), I2=56, and MD (95% CI) of −10.38 (−14.47, −6.28), I2=0%, respectively. Finally, the pooled mean end point scores for the BRIEF-A Global Executive Composite for the LDX-treated groups was greater than that of placebo-treated groups, with MD (95% CI) of −9.20 (−14.11, −4.29), I2=34%.
Discontinuation rates
The pooled overall discontinuation rates in adult ADHD between LDX- and placebo-treated groups did not show any significant differences (RR [95% CI] of 0.82 [0.59, 1.14], I2=0%). Additionally, the pooled discontinuation rates due to adverse events in this population between the two groups was not significantly different (RR (95% CI) of 1.77 [0.71, 4.40], I2=0%).
Risk of bias across studies
The funnel plot asymmetry is normally used to detect the publication bias in a meta-analysis that includes at least ten studies. In this review, only five trials were included, so it was difficult to distinguish the real chance asymmetry;26 therefore, the funnel plot was not carried out in this meta-analysis.
Discussion
This meta-analysis found five RCTs of LDX compared with placebo, in the treatment of adult ADHD. This review suggests that LDX is effective in the treatment of adult ADHD. According to the pooled response rates, the NNT of 4 suggests that one in every four adult patients with ADHD will benefit from the LDX treatment. Additionally, this review also found that LDX improves executive function in those patients. The acceptability of LDX treatment, as measured by the pooled overall discontinuation rates, is comparable to placebo. In addition, its tolerability, based on the pooled rates of discontinuation due to adverse events, is also comparable. These outcomes may promise the efficacy, acceptability, and tolerability of LDX in adult ADHD.
Similar to present review, several stimulants are effective in the treatment of adult ADHD. For instance, recent evidence has shown the efficacy of the extended-release (ER) formulation of MPH31 and osmotic-release oral system (OROS) MPH.32,33 Previous studies have shown that the response rate of MPH ER treatment vs placebo (50% vs 18%)31 and of OROS MPH treatment vs placebo (67% vs 37%)32 in adult ADHD is comparable with the response rate in this review (LDX [70%] vs placebo [37%]). The efficacy of LDX in adult ADHD may be explained by its metabolite, dextroamphetamine, which blocks the reuptake of norepinephrine and dopamine into the presynaptic neuron and directly increases the release of these monoamines extraneuronally, similar to other psychostimulants.15
Based on the prospective study of ADHD in girls from childhood to young adulthood, it was found that both persistent and remitted adult ADHD evidently showed impairment of executive function. Executive function deficit is related to academic underachievement in children with ADHD,34 and with both academic and occupational difficulties in adults with ADHD.5 Based on the BRIEF-A, this review suggests that LDX improves executive function in adult ADHD. This finding is similar to previous studies in adults with ADHD treated with psychostimulants, such as MPH,35 and nonstimulants, such as atomoxetine.36
According to this review, the acceptability of LDX treatment in adult ADHD was not higher than that of placebo, which is similar to the findings for other psychostimulants. According to a recent meta-analysis, the acceptability of MPH treatment in adult ADHD was not greater than that of placebo (odds ratio [OR] 95% CI of 1.19 [0.82, 1.74]).37 Unfortunately, the acceptability of OROS MPH in a recent review was worse than that of placebo.37 These advantages of LDX may be explained by its prodrug formulation, which may reduce the side effects observed in several other psychostimulants, and by the LDX metabolite, dextroamphetamine, which is efficacious for ADHD treatment.
Although tolerability and acceptability of LDX are comparable with placebo, there is a concern of cardiomyopathy in LDX users. Recently, there was a report that three in 5,422 people reported adverse events when taking LDX had cardiomyopathy (one male adult and two male teenagers).38 Although its incidence is rare, cardiomyopathy is serious, and more trials are needed to investigate this potential side effect.
In this review, there were numerous limitations. Firstly, the number of included studies was limited (five RCTs), which may undermine the potential impact of meta-analysis. Therefore, these findings should be cautiously interpreted. Secondly, all included trials were funded by a pharmaceutical company holding the patent of LDX; hence, their outcomes should be carefully considered. Thirdly, pooled discontinuation rate alone was not sufficient to determine the safety of LDX. Unfortunately, other safety data, for instance adverse events, laboratory testing, and vital signs, were not examined in this review; therefore, this agent should be used cautiously. Fourthly, analysis of statistical outliers and artifacts study are useful in meta-analysis, unfortunately, they were not performed in this review. Finally, as is well accepted, publication bias should be examined in meta-analysis but was not assessed here due to the small number of included studies.26
Conclusion
Based on this meta-analysis, LDX is efficacious and well tolerated in the treatment of adult ADHD. Additionally, it also improves the executive function deficits in this population. However, its acceptability is no higher than that of placebo. These findings should be carefully interpreted and considered as preliminary outcomes. To confirm these results, further studies are warranted.
Author contributions
All authors conceived the idea, prepared the study protocol, analyzed the data and prepared the manuscript and approved the manuscript in its current form. NM and BM searched the databases, extracted the data.
Acknowledgment
This review received financial support from the Faculty of Medicine, Chiang Mai University, Thailand.
Disclosure
NM has received travel reimbursement from Servier and Lundbeck. BM has received honoraria and/or travel reimbursement from Lundbeck. SS has received honoraria and/or research grants from Janssen-Cilag, Thai-Otsuka, Lundbeck, and AstraZeneca. MS has received honoraria, consultancy fees, research grants, and/or travel reimbursement from AstraZeneca, GlaxoSmithKline, Pfizer, Janssen-Cilag, Johnson & Johnson, Lundbeck, Thai-Otsuka, Sanofi-Aventis, and Servier. SDM has received honoraria, consultancy fees and research grants from Astra Zeneca, Eli Lilly, Janssen-Cilag, Sanofi-Aventis, Novartis and Wyeth. The authors report no other conflicts of interest.
References
Weiss G, Hechtman L, Milroy T, Perlman T. Psychiatric status of hyperactives as adults: a controlled prospective 15-year follow-up of 63 hyperactive children. J Am Acad Child Psychiatry. 1985;24(2):211–220. | |
Davidson MA. ADHD in adults: a review of the literature. J Atten Disord. 2008;11(6):628–641. | |
Polanczyk G, Rohde LA. Epidemiology of attention-deficit/hyperactivity disorder across the lifespan. Curr Opin Psychiatry. 2007;20(4):386–392. | |
Simon V, Czobor P, Bálint S, Mészáros A, Bitter I. Prevalence and correlates of adult attention-deficit hyperactivity disorder: meta-analysis. Br J Psychiatry. 2009;194(3):204–211. | |
Biederman J, Faraone SV, Spencer TJ, Mick E, Monuteaux MC, Aleardi M. Functional impairments in adults with self-reports of diagnosed ADHD: A controlled study of 1001 adults in the community. J Clin Psychiatry. 2006;67(4):524–540. | |
Barkley RA, Grodzinsky G, DuPaul GJ. Frontal lobe functions in attention deficit disorder with and without hyperactivity: a review and research report. J Abnorm Child Psychol. 1992;20(2):163–188. | |
Clark C, Prior M, Kinsella GJ. Do executive function deficits differentiate between adolescents with ADHD and oppositional defiant/conduct disorder? A neuropsychological study using the Six Elements Test and Hayling Sentence Completion Test. J Abnorm Child Psychol. 2000;28(5):403–414. | |
Greenhill LL, Pliszka S, Dulcan MK, et al. Summary of the practice parameter for the use of stimulant medications in the treatment of children, adolescents, and adults. J Am Acad Child Adolesc Psychiatry. 2001;40(11):1352–1355. | |
Faraone SV, Spencer TJ, Kollins SH, Glatt SJ, Goodman D. Dose response effects of lisdexamfetamine dimesylate treatment in adults with ADHD: an exploratory study. J Atten Disord. 2012;16(2):118–127. | |
Mordre M, Groholt B, Sandstad B, Myhre AM. The impact of ADHD symptoms and global impairment in childhood on working disability in mid-adulthood: a 28-year follow-up study using official disability pension records in a high-risk in-patient population. BMC Psychiatry. 2012;12:174. | |
Castells X, Ramos-Quiroga JA, Rigau D, et al. Efficacy of methylphenidate for adults with attention-deficit hyperactivity disorder: a meta-regression analysis. CNS Drugs. 2011;25(2):157–169. | |
Castells X, Ramos-Quiroga JA, Bosch R, Nogueira M, Casas M. Amphetamines for Attention Deficit Hyperactivity Disorder (ADHD) in adults. Cochrane Database Syst Rev. 2011;(6):CD007813. | |
Blick SK, Keating GM. Lisdexamfetamine. Paediatr Drugs. 2007;9(2):129–135; discussion 136–138. | |
Elbe D, Macbride A, Reddy D. Focus on lisdexamfetamine: A review of its use in child and adolescent psychiatry. J Can Acad Child Adolesc Psychiatry. 2010;19(4):303–314. | |
Madaan V, Kolli V, Bestha DP, Shah MJ. Update on optimal use of lisdexamfetamine in the treatment of ADHD. Neuropsychiatr Dis Treat. 2013;9:977–983. | |
Adler LA, Goodman DW, Kollins SH, et al; 303 Study Group. Double-blind, placebo-controlled study of the efficacy and safety of lisdexamfetamine dimesylate in adults with attention-deficit/hyperactivity disorder. J Clin Psychiatry. 2008;69(9):1364–1373. | |
Faraone SV. Lisdexamfetamine dimesylate: the first long-acting prodrug stimulant treatment for attention deficit/hyperactivity disorder. Expert Opin Pharmacother. 2008;9(9):1565–1574. | |
Wigal T, Brams M, Gasior M, Gao J, Squires L, Giblin J; 316 Study Group. Randomized, double-blind, placebo-controlled, crossover study of the efficacy and safety of lisdexamfetamine dimesylate in adults with attention-deficit/hyperactivity disorder: novel findings using a simulated adult workplace environment design. Behav Brain Funct. 2010;6:34. | |
Biederman J, Fried R, Hammerness P, et al. The effects of lisdexamfetamine dimesylate on driving behaviors in young adults with ADHD assessed with the Manchester driving behavior questionnaire. J Adolesc Health. 2012;51(6):601–607. | |
Dupaul GJ, Weyandt LL, Rossi JS, et al. Double-blind, placebo-controlled, crossover study of the efficacy and safety of lisdexamfetamine dimesylate in college students with ADHD. J Atten Disord. 2012;16(3):202–220. | |
Adler LA, Dirks B, Deas PF, et al. Lisdexamfetamine dimesylate in adults with attention-deficit/hyperactivity disorder who report clinically significant impairment in executive function: results from a randomized, double-blind, placebo-controlled study. J Clin Psychiatry. 2013;74(7):694–702. | |
Higgins JPT, Altman DG, Sterne JAC, editors. Assessing risk of bias in included studies. In: Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0. The Cochrane Collaboration; 2009 [updated March 2011]. Available from: http://www.cochrane-handbook.org. Accessed August 3, 2014. | |
Cipriani A, Furukawa TA, Salanti G, et al. Comparative efficacy and acceptability of 12 new-generation antidepressants: a multiple-treatments meta-analysis. Lancet. 2009;373(9665):746–758. | |
Papakostas GI. Tolerability of modern antidepressants. J Clin Psychiatry. 2008;69 Suppl E1:8–13. | |
Wiebe N, Vandermeer B, Platt RW, Klassen TP, Moher D, Barrowman NJ. A systematic review identifies a lack of standardization in methods for handling missing variance data. J Clin Epidemiol. 2006;59(4):342–353. | |
Sterne JAC, Egger M, Moher D, editors. Addressing reporting biases. In: Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0. The Cochrane Collaboration; 2009 [updated March 2011]. Available from: http://www.cochrane-handbook.org. Accessed August 3, 2014. | |
Lasser R, Dirks B, Adeyi B, Babcock T. Comparative efficacy and safety of lisdexamfetamine dimesylate and mixed amphetamine salts extended release in adults with attention-deficit/hyperactivity disorder. Primary Psychiatry. 2010;17(9):44–54. | |
Surman CB, Roth T. Impact of stimulant pharmacotherapy on sleep quality: post hoc analyses of 2 large, double-blind, randomized, placebo-controlled trials. J Clin Psychiatry. 2011;72(7):903–908. | |
Mattingly GW, Weisler RH, Young J, et al. Clinical response and symptomatic remission in short- and long-term trials of lisdexamfetamine dimesylate in adults with attention-deficit/hyperactivity disorder. BMC Psychiatry. 2013;13:39. | |
Brams M, Weisler R, Findling RL, et al. Maintenance of efficacy of lisdexamfetamine dimesylate in adults with attention-deficit/hyperactivity disorder: randomized withdrawal design. J Clin Psychiatry. 2012;73(7):977–983. | |
Retz W, Rösler M, Ose C, et al; Study Group. Multiscale assessment of treatment efficacy in adults with ADHD: a randomized placebo-controlled, multi-centre study with extended-release methylphenidate. World J Biol Psychiatry. 2012;13(1):48–59. | |
Biederman J, Mick E, Surman C, et al. A randomized, 3-phase, 34-week, double-blind, long-term efficacy study of osmotic-release oral system-methylphenidate in adults with attention-deficit/hyperactivity disorder. J Clin Psychopharmacol. 2010;30(5):549–553. | |
Casas M, Rösler M, Sandra Kooij JJ, et al. Efficacy and safety of prolonged-release OROS methylphenidate in adults with attention deficit/hyperactivity disorder: a 13-week, randomized, double-blind, placebo-controlled, fixed-dose study. World J Biol Psychiatry. 2013;14(4):268–281. | |
Biederman J, Monuteaux MC, Doyle AE, et al. Impact of executive function deficits and attention-deficit/hyperactivity disorder (ADHD) on academic outcomes in children. J Consult Clin Psychol. 2004;72(5):757–766. | |
Fallu A, Richard C, Prinzo R, Binder C. Does OROS-methylphenidate improve core symptoms and deficits in executive function? Results of an open-label trial in adults with attention deficit hyperactivity disorder. Curr Med Res Opin. 2006;22(12):2557–2566. | |
Brown TE, Holdnack J, Saylor K, et al. Effect of atomoxetine on executive function impairments in adults with ADHD. J Atten Disord. 2011;15(2):130–138. | |
Castells X, Cunill R, Capellà D. Treatment discontinuation with methylphenidate in adults with attention deficit hyperactivity disorder: a meta-analysis of randomized clinical trials. Eur J Clin Pharmacol. 2013;69(3):347–356. | |
ehealthme.com [homepage on the Internet]. Could Vyvanse cause stress cardiomyopathy? eHealthMe; 2014 [cited May 25, 2014]. Available from: http://www.ehealthme.com/ds/vyvanse/stresscardiomyopathy. Accessed August 3, 2014. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.