Back to Journals » Clinical Interventions in Aging » Volume 12
Evaluation on the implementation of respiratory protection measures in old age homes
Authors Lee DT, Yu D , Ip M, Tang JY
Received 24 May 2017
Accepted for publication 13 July 2017
Published 11 September 2017 Volume 2017:12 Pages 1429—1438
DOI https://doi.org/10.2147/CIA.S142522
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Zhi-Ying Wu
Diana TF Lee,1 Doris Yu,1 Margaret Ip,2 Jennifer YM Tang3
1The Nethersole School of Nursing, The Chinese University of Hong Kong, 2Department of Microbiology, The Chinese University of Hong Kong, Prince of Wales Hospital, Sha Tin, 3Sau Po Centre on Ageing, The University of Hong Kong, Pok Fu Lam, Hong Kong
Purpose: Old age homes (OAHs) represent a vulnerable community for influenza outbreaks. Effective implementation of respiratory protection measures has been identified as an effective prevention measure to reduce mortality and morbidity caused by such outbreaks. Yet, relatively little is known about this aspect in these homes. This study evaluated the implementation of respiratory protection measures among infection control officers (ICOs) and health care workers (HCWs) in these homes in Hong Kong.
Patients and methods: A territory-wide, cross-sectional survey was conducted in 87 OAHs. A total of 87 ICOs and 1,763 HCWs (including nurses, health workers, care workers, allied HCWs and assistants) completed the questionnaires that evaluated the implementation at the organizational level and individual level, respectively. Generalized estimating equations with unstructured working correlation matrix were used to analyze the simultaneous influence of organizational and individual factors on the implementation.
Results: At the organizational level, all homes had a policy on respiratory protection and implementation of such measures was generally adequate. Basic resources such as paper towels/hand dryers and equipment disinfectants, however, were rated as most inadequate by HCWs. Training opportunities were also identified as grossly inadequate. Only less than half of the ICOs and HCWs participated in training on infection control either at the initiation of employment or on a regular basis. Twenty-five percent of HCWs even indicated that they had never participated in any infection control training. At the individual level, hand hygiene, among other protection measures, was found to be less well implemented by HCWs. In terms of the association of various organizational and individual characteristics, private homes and health workers rated significantly higher scores in the implementation of various domains in respiratory protection.
Conclusion: Addressing the unmet training needs and promoting hand hygiene practice are efforts suggested to further enhance the implementation of respiratory protection measures in OAHs.
Keywords: influenza outbreaks, health care workers, long-term care, infection control
Introduction
Influenza is primarily a community-based infection that is transmitted in households and community settings. Old age homes (OAHs) represent a vulnerable community for nosocomial outbreaks of influenza. Increasing incidence of outbreaks of influenza-like illness has been reported in these homes. In Hong Kong, for example, the reported episodes of such outbreaks in OAHs have increased from 127 in 2004 to 259 in 2008.1,2 Considering that the elderly people have diminished response to influenza vaccine,3 it is generally agreed that practicing respiratory protection measures among health care workers (HCWs) is a highly important means to prevent the outbreak of influenza in OAHs. Indeed, effective implementation of and adherence to such measures have been shown to reduce influenza-related infections, hospitalization, mortality and morbidity.1,4–6 However, relatively little is known about the implementation of such measures in OAHs which are often characterized by limited resources and less educated HCWs.
Respiratory protection measures for HCWs in OAHs generally cover a wide range of practices, including immunization, standard precautions, provision of facilities and resources, surveillance and monitoring, visitor restrictions, management of influenza-like illness, and outbreak preparedness.7–10 Some studies have explored HCW’s compliance with specific respiratory measures such as vaccination uptake11–13 and hand hygiene.5 Vaccination uptake is found to be low, and common reasons for refusing vaccination are associated with inadequate information about the vaccine and subjective perception of inefficacy and risk.13 Hand hygiene compliance among HCWs is also found to be low. For example, a local study in 8 OAHs in Hong Kong has identified the hand hygiene compliance among HCWs to be 45% only.14 Moreover, according to a survey conducted by the Infection Control Stewardship Program in Hong Kong, less than one-third of the OAH staff received annual training in infection control.15 These findings, both local and international, have highlighted the need to have a comprehensive evaluation of the implementation of respiratory protection measures in OAHs.
Indeed, infection control compliance in various health care settings has been proposed as a cornerstone in the prevention and control of health care-associated infections. A cross-sectional survey reported that nurses who had poorer knowledge on standard precautions, no prior training, lower staff grade and lower general self-efficacy were predicted to have lower compliance.16 A randomized controlled trial found that hand hygiene compliance in long-term care facilities increased two- to threefold with improved equipment (eg, racks, pull reels), environmental cues (eg, posters), education and training.14 These findings suggest that promoting compliance with infection control measures depends on both organizational and individual factors. Promoting the compliance of respiratory protection measures in OAHs is of no exception. However, little is known about the implementation of respiratory protection measures at both these levels in OAHs. A study was therefore conducted to evaluate the implementation of respiratory protection measures in OAHs in Hong Kong at both organizational and individual levels. The challenges, facilitators and barriers to such implementation were also explored.
Materials and methods
Study design and sampling
A territory-wide, cross-sectional survey was conducted from September 2014 to August 2015.
Proportional cluster sampling was used to recruit OAHs. The funding mode of the OAHs was used as cluster, as this factor would directly influence the care practice and resources of the homes. There are a total of 767 residential care homes for the elderly (RCHEs) in Hong Kong that are operated by 3 major funding modes, including non-private homes (n=203, 26.4%), private homes (n=282, 36.8%) and private enhanced bought place scheme (EBPS) homes (n=282, 36.8%).17 In the EBPS homes, the government purchases places from these private homes with a view to upgrading the service standard of these homes through enhanced service requirements in terms of staffing and space. According to previous studies, the average compliance to various infection control practices is, in general, over 60%.15,18,19 A 95% confidence interval and 10% margin of error in sample size calculation was therefore adopted in sample size calculation. It was therefore proposed to recruit 86 OAHs (22 non-private homes, 32 private homes and 32 private EBPS homes).
For each recruited OAH, 2 target staff groups were recruited as participants. The first group was the infection control officers (ICOs), who were responsible for coordinating matters related to the prevention and handling of infectious diseases in these homes. The second group was all the HCWs of the homes. HCWs in OAHs refer to registered nurses, enrolled nurses, health workers, care workers or others such as allied health professionals. A health worker is a person who has completed a course of training for working in OAHs as approved by the government and whose name appears on the register. He/she is responsible for the overall health care of residents in OAHs. A care worker is any person employed by the home to render daily personal care to the residents.
Data collection and study instruments
Two sets of questionnaires were developed to collect data about the implementation of the respiratory protection measures from the ICOs and HCWs. The questionnaires were developed according to international and local infection control guidelines.7–10 With the consent of the home managers, the research nurse held 2 concurrent briefing sessions in each recruited OAH to explain the background, study objectives and procedures to the ICOs and HCWs and invited them to participate. Posters were also used to publicize this research activity in the homes. For those who showed interest to join the study, the research nurse further explained the study objectives and procedures to the ICOs and HCWs with the use of an information sheet, invited them to participate, obtained their written informed consent and distributed the corresponding set of questionnaires. A sealed and opaque collection box was placed in the office area of each OAH for the participants to return their questionnaires. The research nurse collected the questionnaires from the collection box every week. All the questionnaires were anonymous. A coding system was used to allow identification of the OAHs.
Questionnaire for ICOs
For the ICOs, the questionnaire evaluated 10 perspectives of implementation at the organizational level. The content covered several domains such as rules and resources, training activities, quality control measures, surveillance and monitoring, outbreak preparedness and management. The response set was a “4-point” Likert scale. A higher score represented a higher level of implementation of respiratory protection measures at the organizational level. Open-ended questions were included to explore the challenges, facilitators and barriers for implementing such measures at the organizational level.
Questionnaire for HCWs
As for the HCWs, the questionnaire focused on evaluating the implementation of respiratory protection measures at the individual level. The content covered several domains such as hand hygiene, respiratory hygiene and etiquette and management of waste. The response set was a “4-point” Likert scale, with higher scores representing a higher level of implementation. Open-ended questions were included to explore why they do or do not comply with the respiratory protection measures.
Data analysis
All statistical analyses were performed using SPSS 22.0 software. Descriptive statistics such as mean, standard deviation, frequency and percentage were used to identify the central tendency and frequency distribution of the responses on the implementation of respiratory protection measures. Cronbach’s α (alpha) was used to test the reliability of the 7 domains in the section of “Performing respiratory protection measures” of the questionnaire for HCWs. These domains were “hand hygiene,” respiratory hygiene/cough etiquette, use of personal protective equipment, handling soiled and contaminated articles, environmental control, handling residents with influenza-like illness and rules for visitors. Content analysis was performed on the answers in the open-ended questions. To analyze the simultaneous influence of organizational and individual factors on HCWs’ implementation of respiratory protection measures, generalized estimating equations (GEE) with unstructured working correlation matrix were applied. Organizational factors included manpower structure, number of residents and types of OAHs. Individual factors included age, gender, ranking, education level, training of infection control and years of working experience. A P-value of <0.05 was considered statistically significant.
Ethical considerations
Ethical approval was obtained from the Survey and Behavioural Research Ethics Committee, The Chinese University of Hong Kong.
Results
Characteristics of the RCHEs
A total of 87 RCHEs (17 non-private homes, 35 private homes and 35 private EBPS homes) were recruited from September 2014 to May 2015. Table 1 summarizes the characteristics of these homes. Private homes have significantly (P=0.016) lower nurse to resident ratio (1:61.16) when compared with non-private homes (1:23.62) and private homes with EBPS (1:33.90) but not health worker to resident ratio.
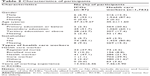
Characteristics of the participants
A final sample of 87 ICOs and 1,763 HCWs participated in the study. The response rate was 100% and 74.5%, respectively. Table 2 summarizes the characteristics of the participants. Majority of the ICOs (93.1%) and HCWs (87.6%) were female and had attained secondary educational level. Their mean age was 47.3 and 45.2 years, respectively. Majority of the ICOs were health workers (41%) or registered nurses (37.9%) while most of the HCWs were care workers (39.9%) or health workers (21.9%).
Implementation of respiratory protection measures at the organizational level
Infection control policies and practices
All OAHs had an infection control guideline for the prevention and control of respiratory transmissible diseases. Majority of the homes (96.6%) adopted local government codes and guidelines as references. Most of the homes reviewed the guidelines either every year (46%) or every 6 months (42.5%). A minority of homes (5.7%) reported that they would review the guidelines and update if necessary while 4.6% of homes indicated that they had no review at all. Among the various aspects in the guidelines, 13% of the homes did not have instructions/recommendations on staff exclusion policy. Of all the homes that had a staff exclusion policy, 21.9% of them indicated that this policy was not adhered to at all. Inadequate resources (34.5%) were the most frequently reported barrier for implementation, followed by inadequate manpower (26.4%), uncooperative staff (16.1%) and inadequate organizational support (10.3%).
Preparedness of the environment and resources
Among all the types of hygiene products and personal protective equipment, supply of paper towels or hand dryers (22.9%) and disinfectants (22.5%) was perceived as most inadequate/very much inadequate in OAHs. IT support for handling data on infection surveillance and control (18.4%), and isolation area (16.1%) was also perceived as inadequate/very much inadequate.
In terms of training activities, most of the ICOs (51.7%) received training on respiratory protection measures at the initiation of employment and 58.6% of them also received training when taking up the role of ICO. About 81.6% of them also attended training annually. Staff exclusion policy and sentinel surveillance of respiratory diseases were indicated as topics not well-covered in the training. As for HCWs, most of the homes required health workers (100%), care workers (90.8%) and nurses (69.0%) to attend training on respiratory protection measures. It was reported that this training was provided at initiation of employment (54.7%) and annually (89.7%). Yet, 25.4% of the HCWs indicated that they had never attended any training, and only about one-third of them (35.5%) indicated that they had attended training in the previous year (ie, 2014).
Most of the homes (66.7%) kept records of the training activities most of the time. The most common ways to evaluate the effectiveness of the training activities was by collecting verbal feedback from the HCWs (60.9%), followed by the use of evaluation forms (25.3%) and examination (7.6%). Some of the homes (14.9%) did not evaluate the effectiveness of the training activities. The most frequently reported barriers for OAHs to organize training activities were inadequate manpower (32.2%), inadequate knowledge (27.6%) and inadequate resources (26.4%).
Surveillance and monitoring system
Most of the homes conducted observations (77.0%) and monitored the usage of hand hygiene supplies and disposable personal protective equipment (70.1%) to evaluate the effectiveness of the implementation of respiratory protection measures. Some homes collected feedback from HCWs (46.0%), residents and visitors (34.5%), and external bodies, such as Department of Health, Center for Health Protection or outreach nurses (12.6%). In terms of the frequency of the evaluation, most of the homes indicated that they would conduct evaluation every year (51.7%). A few homes (4.6%) would review the implementation if necessary, while 1.1% OAHs indicated that they had not evaluated the implementation at all.
The most frequently reported respiratory transmissible disease included in the surveillance and monitoring activities at OAHs were influenza (71.3%), tuberculosis (40.2%) and pneumococcal infection (28.7%). In terms of the surveillance measures being used, most of the homes had an up-to-date line listing of both vaccinated residents (93.1%) and HCWs (94.1%) as well as documentation of staff who had refused vaccination (93.1%) all or most of the time. Some homes, however, did not have a system for collecting data on respiratory infections among the HCWs (17.2%) or the residents (13.8%). Sharing statistics on respiratory infections to the home manager and HCWs regularly was not practiced in some homes (18.4%). The most commonly reported barriers in coordinating the surveillance of respiratory infections were inadequate manpower (39.1%), inadequate resources (37.9%), uncooperative staff (26.4%) and inadequate organizational support (10.3%). Uncooperative patients and visitors were also cited as barriers.
Outbreak preparedness and management
A total of 57 outbreaks of influenza-like illness involving 455 residents and 86 staff in 35 OAHs were reported in the past 3 years (2012–2015), with 1 outbreak reported in 20 OAHs, 2 outbreaks reported in 8 OAHs, and 3 outbreaks reported in 7 OAHs in the past 3 years. Of the homes with 3 outbreaks, 4 were private and private EBPS homes. The mean duration for each outbreak was 15.17 (SD =7.06) days, the means of residents and HCWs infected per outbreak were 10.43 (SD =7.79) and 2.90 (SD =3.79), respectively.
ICOs were usually responsible for managing the outbreaks (85.1%). A few homes (9.2%) convened an outbreak control team to be responsible for outbreak management. Most of the homes (92%) had a protocol to support outbreak preparedness and response, and most ICOs (95%) agreed that their homes were well equipped for the outbreaks. Inadequate manpower (43.7%), uncooperative staff (16.1%) and lack of organizational support (6.9%) were cited as barriers in managing influenza outbreaks.
Implementation of respiratory protection measures at individual level
Vaccination status for respiratory transmissible diseases
Residents
The mean proportions of the residents who had received seasonal influenza vaccine in the past year (ie, 2014) and ever received pneumococcal vaccine were 86.1% (SD =9.60) and 66.8% (SD =31.4), respectively.
Staff
The uptake of seasonal influenza vaccination in ICOs and HCWs was 66.7% and 54.8%, respectively. For those who had not received the seasonal influenza vaccination, worries about the side effects of vaccination and lack of confidence in the effectiveness of the vaccine were perceived as the major barriers.
Implementation of respiratory protection measures among HCWs
Table 3 summarizes the extent to which HCWs implement protection measures. In general, hand hygiene measures were less well implemented when compared with other measures. In terms of why HCWs implement or not implement the protection measures, perceived personal health risk (97.9%), promotion of health and safety of residents (97.6%) and level of knowledge of respiratory protection measures (97.2%) were rated as the main reasons.
Association between organizational and individual characteristics in the implementation of respiratory protection measures
The scores and Cronbach’s alpha of the 7 domains of respiratory protection measures as implemented by HCWs are summarized in Table 4. Cronbach’s alpha of the various domains are acceptable and range from 0.806 to 0.888.
  | Table 4 Scores and reliability of different domains of respiratory protection measures |
Tables 5 and 6 present the GEE results with regard to the association between implementation of respiratory protection measures and organizational characteristics and individual socio-demographic characteristics of the HCWs. “Type of home” and “type of health care worker” were found to have the greatest association with “private homes” and “health workers” rated significantly higher scores in a number of domains. “Private homes” rated higher implementation scores in various domains such as “hand hygiene” (P=0.010), “handling residents with influenza-like illness” (P=0.34), “implementation of rules for visitors during normal condition” (P=0.01) and “implementation of rules for visitors during peak season/influenza outbreak” (P=0.04). When compared with other HCWs in the OAHs, “health workers” rated significantly higher scores in a number of domains, including “hand hygiene” (P<0.001), “handling residents with influenza-like illness” (P=0.034), “implementation of rules for visitors during normal condition” (P=0.001) and “implementation of rules for visitors during peak season/influenza outbreak” (P=0.004).
Discussion
To the best of our knowledge, this is the first study that evaluated the implementation of respiratory protection measures in OAHs in Hong Kong. Our results have not only provided a profile of the implementation of such measures at the organization and individual level but have also identified the simultaneous influence of organizational and individual factors on such implementation.
At the organization level, all homes stated that they had an infection control policy and majority of the homes had adopted local government guidelines as references. Among the various aspects in the guidelines, policy and practices on staff exclusion was found to be either absent or not adhered to in a number of homes. Indeed, when compared to international guidelines in the UK and Australia,20,21 our guideline in Hong Kong22 on staff exclusion was rather vague and nonspecific. Therefore, OAHs did not have adequate information to formulate and implement this policy and guideline. In terms of facilities and resources, it was a concern that basic resources such as paper towels/hand dryers and equipment disinfectants were seen as most inadequate. With regard to training activities, it is important to note that over 25% of the HCWs indicated that they had never participated in any training activities and only 35.5% had attended training in the previous year (2014). Also, only about half of the ICOs and HCWs had received training on infection control at the initiation of employment. This was in contrast to the training policy as reported by the ICOs and further highlighted the unmet training needs of HCWs in OAHs in Hong Kong when compared with international practice.18 As frequently identified in the literature, inadequate manpower, lack of knowledge and resources were also described by ICOs in this study as barriers.18 It has been frequently reported that poor knowledge and no prior training on standard precautions are important factors for low compliance with respiratory protection measures.16 Findings of this study have further highlighted that training on respiratory protection is an area that requires attention in OAHs.
At the individual level, the uptake of seasonal influenza vaccine as reported by the participants in this study was comparatively higher than the uptake rate for HCWs in OAHs (39.8%) and the general population (14%) as reported by the Centre for Health Protection in Hong Kong in 2012/13.23 This coverage is indeed comparable to those reported in the US24 and UK.25 This may be a result of the various promotional work that has been conducted in the past few years on vaccination. Concurring with the literature,23,25,26 worries about the side effects of vaccination and lack of confidence in the effectiveness of the vaccine were perceived as the major barriers. Among the different domains of protection measures, hand hygiene was found to be less well implemented by the HCWs. This could be related to the findings that paper towels, hand dryers and equipment disinfectants were perceived as the most inadequate resources in the study homes. Yet, compliance with hand hygiene practice is fundamental to respiratory protection. Various interventions such as provision of pocket-sized antiseptic gel and gloves have been found to successfully increase hand hygiene compliance.5,14 More efforts are indicated in promoting hand hygiene practice in OAHs. Capitalizing on the importance of minimizing personal health risk is an important strategy to promote the implementation of protection measures among HCWs27 and this study has further reinforced this as a viable strategy.
In terms of the association of various organizational and individual characteristics with health workers’ implementation of respiratory protection measures, “type of home” and “type of health care worker” are found to have the greatest association. Private homes rated significantly higher scores in the implementation of hand hygiene, respiratory hygiene, implementing rules for visitors during normal condition and peak season/influenza outbreak. Among the various types of HCWs, health workers rated significantly higher scores in a number of domains, including hand hygiene, handling residents with influenza-like illness, implementing rules for visitors during normal condition and peak season/influenza outbreak. This is an interesting finding as private homes in this study have significantly lower nurse to resident and other staff to resident ratios but not health worker to resident ratio when compared with non-private homes and private homes with EBPS. In face of the shortage of nurses, health workers are the key health care personnel who are specially trained to work in OAHs and are registered under the Residential Care Homes (Elderly Persons) Regulation. Findings of this study suggest that empowering them with the necessary knowledge and skills in respiratory protection is pivotal in enhancing the implementation of such measures in these homes.
Limitations
This study uses self-report to evaluate the implementation of respiratory protection measures in OAHs. As a common form of evaluation, self-report collects direct report of information from the participants. While this method is direct and versatile and allows for large samples to be included to provide a general overview of the topic under study,28 it has its methodological weaknesses. It is likely that participants in this study may claim to be more competent in implementing respiratory protection measures than what they actually are to avoid criticism. Or, in the reverse, to claim they are less competent to increase chance of training development or resources to their OAHs. It should be cautioned that the results of this study have the above limitations, and other more qualitative forms of methodologies such as observation and objective competence assessment should be used alongside with this study to provide broader assessment of the implementation of respiratory protection measures in these homes.
Conclusion
This study has identified the important areas that require further action in enhancing the implementation of respiratory protection measures in OAHs. The unmet training needs of HCWs would need to be fulfilled. OAHs should be supported in developing and implementing a mandatory training policy on respiratory protection for HCWs at initiation of employment, and refresher training should be organized on a regular basis. This mandatory training policy could be considered as a licensing criteria. Ad hoc training to reinforce protection measures during peak season/outbreaks should also be considered. The government could set up a training team to take responsibilities for such ad hoc training. As hand hygiene has been identified as a less well implemented area, continuous education and evaluation of practice in this area is warranted. The roles of ICOs in enhancing training should be further supported and reinforced. Our local guidelines on staff exclusion policy should be revisited and properly formulated so that OAHs are provided with adequate information to formulate and implement this policy. The promotional work on vaccination has resulted in higher vaccination coverage for both HCWs and residents when compared with previous years. Work in this area should be further supported. Future study should use more qualitative forms of methodologies such as observation and objective competence assessment to provide broader assessment of the implementation of respiratory measures in OAHs.
Acknowledgments
The investigators would like to thank the Health and Medical Research Fund, Food and Health Bureau of the Hong Kong Special Administrative Region for funding this study. We are grateful to the OAHs and those staff and visitors of the homes who have participated in the survey. We also thank Ms Ma Haixia and Ms Poon Miu Ho for their assistance with data collection and analysis.
Disclosure
The authors report no conflicts of interest in this work.
References
Lau T. Effectiveness of Influenza Vaccine Among Elderly People Living in Residential Care Homes During Outbreak Situations [master’s thesis]. Hong Kong: The University of Hong Kong; 2005. | ||
Hui DS, Woo J, Hui E, et al. Influenza-like illness in residential care homes: a study of the incidence, aetiological agents, natural history and health resource utilization. Thorax. 2008;63(8):690–697. | ||
Grubeck-Loebenstein B, Della Bella S, Iorio AM, Michel J, Pawelec G, Solana R. Immunosenescence and vaccine failure in the elderly. Aging Clin Exp Res. 2009;21(3):201–209. | ||
Bin-Reza F, Lopez Chavarrias V, Nicoll A, Chamberland ME. The use of masks and respirators to prevent transmission of influenza: a systematic review of the scientific evidence. Influenza Other Respir Viruses. 2012;6(4):257–267. | ||
Yeung WK, Tarn WSW, Wong TW. Clustered randomized controlled trial of a hand hygiene intervention involving pocket-sized containers of alcohol-based hand rub for the control of infections in long-term care facilities. Infect Control Hosp Epidemiol. 2011;32(1):67–76. | ||
Nichol KL, Nordin J, Mullooly J, Lask R, Fillbrandt K, Iwane M. Influenza vaccination and reduction in hospitalizations for cardiac disease and stroke among the elderly. N Engl J Med. 2003;348(14):1322–1332. | ||
Department of Health. Guidelines on Prevention of Communicable Diseases in Residential Care Homes for the Elderly. Hong Kong: Department of Health, The Government of the Hong Kong Special Administrative Region; 2007. | ||
Smith PW, Bennett G, Bradley S, et al. SHEA/APIC guideline infection prevention and control in the long-term care facility. Am J Infect Control. 2008;36(7):504–535. | ||
World Health Organization. WHO Guidelines on Hand Hygiene in Health Care. Geneva: World Health Organization; 2009. | ||
Chami K, Gavazzi G, de Wazieres B, et al. Guidelines for infection control in nursing homes: a Delphi consensus web-based survey. J Hosp Infect. 2011;79(1):75–89. | ||
Mody L, Langa KM, Saint S, Bradley SF. Preventing infections in nursing homes: a survey of infection control practices in southeast Michigan. Am J Infect Control. 2005;33(8):489–492. | ||
Heimberger T, Chang HG, Shaikh M, Crotty L, Morse D, Birkhead G. Knowledge and attitudes of healthcare workers about influenza: why are they not getting vaccinated? Infect Control Hosp Epidemiol. 1995;16(7):412–415. | ||
Maltezou HC, Dedoukou X, Patrinos S, et al. Determinants of intention to get vaccinated against novel (pandemic) influenza A H1N1 among health-care workers in a nationwide survey. J Infect. 2010;61(3):252–258. | ||
Ho M, Seto W, Wong L, Wong T. Effectiveness of multifaceted hand hygiene interventions in long-term care facilities in Hong Kong: a cluster-randomized controlled trial. Infect Control Hosp Epidemiol. 2012;33(8):761–767. | ||
Yau C. Infection control and prevention in residential care homes for the elderly (RCHE); 2012. Available from: http://icidportal.ha.org.hk/sites/en/Lists/Training%20Calendar/Attachments/81/IC_forum-_Part_II.pdf. Accessed January 25, 2014. | ||
Luo Y, He GP, Zhou JW, Luo Y. Factors impacting compliance with standard precautions in nursing, China. Int J Infect Dis. 2010;14(12):e1106–e1114. | ||
Social Welfare Department [homepage on the Internet]. Hong Kong: Social Welfare Department; 2014. Available from: http://www.swd.gov.hk/en/index/site_pubsvc/page_elderly/sub_residentia/id_overviewon/. Accessed January 22, 2014. | ||
Zoutman DE, Ford BD, Gauthier J. A cross-Canada survey of infection prevention and control in long-term care facilities. Am J Infect Control. 2009;37(5):358–363. | ||
Smith PW, Shostrom V, Smith A, Kaufmann M, Mody L. Preparedness for pandemic influenza in nursing homes: a 2-state survey. JAMA. 2008;300(4):392–394. | ||
Department of Health and Health Protection Agency. Prevention and Control of Infection in Care Homes: An Information Resource. London: Department of Health and Health Protection Agency; 2013. | ||
Communicable Diseases Network Australia. A Practical Guide to Assist in the Prevention and Management of Influenza Outbreaks in Residential Care Facilities in Australia. Australia: Communicable Diseases Network Australia; 2009. | ||
Department of Health. Guidelines on Prevention of Communicable Diseases in Residential Care Home for the Elderly. 3rd ed. Hong Kong: Department of Health, The Government of Hong Kong Special Administrative Region; 2015. | ||
Chan D. Seasonal influenza vaccination coverage survey for the 2012/13 season. Commun Dis Watch. 2013;10(19):74–75. | ||
Centers for Disease Control and Prevention. Health Care Personnel and Flu Vaccination, Internet Panel Survey, United States; 2015. Available from: https://www.cdc.gov/flu/pdf/fluvaxview/hcp-ips-nov2015.pdf. Accessed November 24, 2015. | ||
Public Health England. Seasonal Influenza Vaccine Uptake Amongst Frontline Healthcare Workers in England. Winter Season 2014–2015. London: Public Health England; 2015. | ||
Prematunge C, Corace K, McCarthy A, Nair RC, Pugsley R, Garber G. Factors influencing pandemic influenza vaccination of healthcare workers: a systematic review. Vaccine. 2012;30(32):4733–4743. | ||
Zhang J, While AE, Norman IJ. Seasonal influenza vaccination knowledge, risk perception, health beliefs and vaccination behaviours of nurses. Epidemiol Infect. 2012;140(9):1569–1577. | ||
Polit DF, Beck CT. Nursing Research: Generating and Assessing Evidence for Nursing Practice. 10th ed. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2012. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.