Back to Journals » Drug Design, Development and Therapy » Volume 10
Efficacy and safety of two fixed-dose combinations of S-amlodipine and telmisartan (CKD-828) versus S-amlodipine monotherapy in patients with hypertension inadequately controlled using S-amlodipine monotherapy: an 8-week, multicenter, randomized, double-blind, Phase III clinical study
Authors Ihm SH , Jeon HK, Cha TJ, Hong TJ, Kim SH, Lee NH, Yoon JH, Yoon NS, Hwang KK, Jo SH, Youn HJ
Received 9 July 2016
Accepted for publication 22 September 2016
Published 23 November 2016 Volume 2016:10 Pages 3817—3826
DOI https://doi.org/10.2147/DDDT.S116847
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Frank Boeckler
Sang-Hyun Ihm,1 Hui-Kyung Jeon,1 Tae-Joon Cha,2 Taek-Jong Hong,3 Sang-Hyun Kim,4 Nae-Hee Lee,5 Jung Han Yoon,6 Namsik Yoon,7 Kyung-Kuk Hwang,8 Sang-Ho Jo,9 Ho-Joong Youn1
1Division of Cardiology, Department of Internal Medicine, The Catholic University of Korea, Seoul, 2Division of Cardiology, Department of Internal Medicine, Kosin University College of Medicine, 3Division of Cardiology, Department of Internal Medicine, Pusan National University Hospital, Busan, 4Division of Cardiology, Department of Internal Medicine, Boramae Medical Center, Seoul National University College of Medicine, Seoul, 5Department of Cardiology, Soonchunhyang University Hospital, Bucheon, 6Division of Cardiology, Wonju College of Medicine, Yonsei University, Wonju, 7Department of Cardiology, Chonnam National University Hospital, Gwangju, 8Department of Internal Medicine, Chungbuk National University, College of Medicine, Cheongju, 9Division of Cardiology, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, Anyang, South Korea
Purpose: To evaluate the blood pressure (BP) lowering efficacy and safety of CKD-828, a fixed-dose combination of S-amlodipine (the more active isomer of amlodipine besylate, which is calcium channel blocker) and telmisartan (long acting angiotensin receptor blocker), in patients with hypertension inadequately controlled with S-amlodipine monotherapy.
Patients and methods: Eligible patients (N=187) who failed to respond after 4-week S-amlodipine 2.5 mg monotherapy (sitting diastolic blood pressure [sitDBP] ≥90 mmHg) to receive CKD-828 2.5/40 mg (n=63), CKD-828 2.5/80 mg (n=63), or S-amlodipine 2.5 mg (n=61) for 8 weeks. The primary efficacy endpoint, mean sitDBP change from baseline to Week 8, was compared between the combination (CKD-828 2.5/40 mg and CKD-828 2.5/80 mg) and S-amlodipine monotherapy groups. The safety was assessed based on adverse events, vital signs, and physical examination findings.
Results: After the 8-week treatment, changes in sitDBP/systolic BP (SBP) were -9.67±6.50/-12.89±11.78, -10.72±6.19/-13.79±9.41, and -4.93±7.26/-4.55±11.27 mmHg in the CKD-828 2.5/40 mg (P<0.0001/P<0.0001), CKD-828 2.5/80 mg (P<0.0001/P<0.0001), and S-amlodipine 2.5 mg (P<0.0001/P=0.0027) groups, respectively, which were all significant BP reductions. At Week 8, the CKD-828 2.5/40 mg (sitDBP/SBP: P=0.0002/P<0.0001) and CKD-828 2.5/80 mg (sitDBP/SBP: P=0.0001/P<0.0001) showed superior BP-lowering effects to S-amlodipine 2.5 mg (P<0.001). At Week 4, all groups showed significant antihypertensive effects but both CKD-828 combinations (CKD-828 2.5/40 mg and CKD-828 2.5/80 mg) exhibited superior BP-lowering effects to that of S-amlodipine 2.5 mg (sitDBP/SBP: P=0.0028/P=0.0001 and P<0.0001/P=0.0012, respectively). The adverse event incidence was significantly lower in the CKD-828 2.5/40 mg (9.52%, P=0.0086) than in the S-amlodipine 2.5 mg group (27.87%) and increasing the telmisartan dose induced no unexpected adverse events, suggesting the safety of CKD-828.
Conclusion: CKD-828 is an effective and safe option for patients with inadequate responses to S-amlodipine monotherapy.
Keywords: blood pressure, antihypertensive, calcium channel blocker, angiotensin receptor blocker, efficacy, safety
Introduction
Cardiovascular disease is the most common cause of death in the population, and hypertension is the most important treatable risk factor.1 The risk of cardiovascular disease is the lowest at a blood pressure (BP) of ~115/75 mmHg, and above this, each increment in the systolic blood pressure (SBP) or diastolic blood pressure (DBP) of 20 and 10 mmHg, respectively, doubles the risk of major cardiovascular and stroke events.2 Therefore, considerable benefits including the reduced risks of cardiovascular mortality are associated with lowering the BP. More than two-third of patients with hypertension require treatment with two or more antihypertensive drugs to achieve their target BP goals.1,3,4 The concomitant use of drugs with different mechanisms of action can offset potential side effects of each drug.
Therefore, various fixed-dose combinations have recently been developed and used to improve patient compliance with a more convenient regimen.3,5 The combination drugs of renin angiotensin system blocker, such as angiotensin converting enzyme inhibitor/diuretic, angiotensin receptor blocker/diuretic, angiotensin converting enzyme inhibitor/calcium channel blocker, and angiotensin receptor blocker/calcium channel blocker, are superior to other combination drugs.3,6 The renin angiotensin system blocker/calcium channel blocker combination is particularly recommended as an effective BP-lowering combination because angiotensin receptor blocker or angiotensin converting enzyme inhibitor relieves peripheral edema, the major calcium channel blocker-related adverse effect.7,8
Amlodipine besylate is a conventional widely used form of the third-generation dihydropyridine calcium channel blocker. Moreover, S-amlodipine besylate is the more active isomer of amlodipine besylate and was approved for treating hypertension, stable angina, and variant angina. S-amlodipine besylate is also effective for hypertension caused by fluid retention (nonrenin-dependent hypertension) due to its additional natriuretic activity.9 Telmisartan selectively acts on the angiotensin II receptor. Angiotensin II is a potent vasoconstrictor in the renin-angiotensin system, especially at the angiotensin type 1 receptor, which is involved in important physiological functions, such as vasoconstriction.10,11 The antihypertensive effect lasts for more than 24 h and is safe even until the next morning when the BP may suddenly rise. With a renal excretion rate <2%, telmisartan does not require dosage adjustment in patients with mild or moderate renal impairment and is particularly effective for those with renin-dependent hypertension.10
Compared with high-dose monotherapies, fixed-dose combination antihypertensive drugs have been associated with improved BP control as a result of enhanced adherence and reduction of side effects.12–14 Among the numerous fixed-dose combinations, those consisting of a calcium channel blocker and angiotensin receptor blocker have exhibited better beneficial antihypertensive efficacy than have the others.15,16 In addition, telmisartan has a different pharmacokinetic profile compared with that of other angiotensin receptor blockers, and S-amlodipine besylate has a more potent antihypertensive efficacy than other calcium channel blockers or amlodipine.10,16 Fixed-dose combination formulations of S-amlodipine besylate (2.5 mg) and telmisartan (40 or 80 mg), which have two different mechanisms of action, have been developed as antihypertensive drugs (CKD-828 2.5/40 or 2.5/80 mg). Therefore, the aim of this confirmatory clinical trial was to evaluate the efficacy and safety of the CKD-828 fixed-dose combinations in patients with hypertension who are inadequately controlled using S-amlodipine monotherapy.
Patients and methods
Patients
The patients who were eligible for this study were Korean men and women aged ≥18 years with uncomplicated, mild-to-moderate essential hypertension. Inclusion criteria were patients with a mean sitting diastolic blood pressure (sitDBP) ≥100 or 90 mmHg who were treatment-naïve or receiving antihypertensive drugs, respectively. After a 4-week S-amlodipine 2.5 mg run-in treatment, subjects who failed to respond adequately to this monotherapy (defined as sitDBP ≥90 mmHg) received the trial drugs.
Exclusion criteria were patients showing the following BP readings at screening (Visit 1): difference in sitDBP ≥10 mmHg or sitting systolic blood pressure (sitSBP) difference ≥20 mmHg on a selected arm (the arm with a higher mean sitDBP), mean sitDBP ≥120 mmHg, or sitSBP ≥200 mmHg and at randomization (Visit 2): mean sitDBP ≥120 mmHg or sitSBP ≥180 mmHg; patients with suspected or known secondary hypertension; serious cardiovascular disease, such as myocardial infarction, unstable angina, heart failure (NYHA class III or IV), or serious arrhythmia, requiring medication within the last 3 months; and severe cerebrovascular disorder along with a history of cerebrovascular disease, such as cerebral infarction and cerebral hemorrhage, in the past 6 months. In addition, the authors excluded patients with type 1 diabetes or uncontrolled type 2 diabetes (HbA1C >8%); known severe or malignant retinopathy; abnormal laboratory findings suggesting hepatic impairment (with aspartate aminotransaminase/alanine aminotransaminase >2× the upper limit of normal); renal impairment (serum creatinine >1.5× the upper limit of normal); acute or chronic inflammation requiring treatment; a history of angioedema or serious hypersensitivity after taking angiotensin converting enzyme inhibitor, angiotensin receptor blocker, or amlodipine; and a malignancy within the past 5 years.
Apart from the study drug, the use of other antihypertensive drugs or those that may affect the BP during the clinical study or other drugs that may interact with the study drug was not permitted. Women who were pregnant, breast-feeding, or of childbearing age and were not using an effective method of contraception were not allowed to participate in the study. The patients who were participating in other investigational studies and those with legal or psychological conditions were not suited for this clinical study and were also excluded.
Study design
This study was a multicenter, 8-week, randomized, double-blind, parallel group, Phase III clinical trial evaluating the efficacy and safety of S-amlodipine plus telmisartan fixed-dose combination (CKD-828) versus S-amlodipine 2.5 mg monotherapy in patients with hypertension inadequately controlled with S-amlodipine 2.5 mg monotherapy. This study was conducted according to the Declaration of Helsinki and Good Clinical Practice guidelines. The study was approved by the Korea Food and Drug Administration and the Institutional Review Board of each participating study center. Written informed consent was obtained from all patients prior to participation.
After screening, patients who met the eligibility criteria were given once-daily S-amlodipine 2.5 mg for 4 weeks (run-in period). At randomization, patients with sitDBP ≥90 mmHg were randomly assigned (1:1:1) to receive CKD-828 2.5/40 mg, CKD-828 2.5/80 mg, or S-amlodipine 2.5 mg and commenced the 8-week double-blind treatment. During this period, subjects visited the study site for Visit 2, 3, and 4 (Day 0, 28, and 56, respectively) to undergo the efficacy and safety assessments as well as other tests (Figure 1).
Efficacy and safety evaluations
The vital sign monitoring and physical examinations were performed at every visit, and the severity of adverse events and their association with study drugs were assessed by the investigator using WHO Adverse Reaction Terminology (WHO-ART; 2009 2nd quarter version). The sitting in-clinic BP was measured using automatic BP monitor (HEM-70801T, Omron Corporation, Kyoto, Japan) at the initial screening, the end of the run-in treatment period prior to randomization, and after 4 and 8 weeks of double-blind treatment. The BP, pulse rate, and body temperature were measured. The BP was recorded as the mean of three consecutive measurements.17
The primary efficacy endpoints were assessed after 8 weeks of treatment. The primary efficacy endpoint was the change in sitDBP from baseline (Visit 2) to Week 8 (Visit 4) between the study drugs and the comparator (Figure 1). The secondary efficacy endpoints were the change in sitDBP from baseline to Week 4 (Visit 3) with the study drug versus the comparator, the changes in sitSBP from baseline to Weeks 4 and 8 with the study drug versus the comparator, the control rate (rate of subjects who achieved the target sitDBP <90 mmHg at Weeks 4 and 8), and response rate (rate of subjects with a decrease in sitDBP ≥10 mmHg or a mean sitDBP <90 mmHg, or both at Weeks 4 and 8).
The safety variables included adverse events, vital signs, height, weight, and resting 12-lead electrocardiography, as well as chest and clinical laboratory test (hematology, blood chemistry, and urinalysis). The adverse events were assessed and recorded in the case report form. Adverse events occurring after randomization were assessed separately to determine whether they were associated with the study drug or comparator (S-amlodipine besylate or telmisartan) taken by the subjects during the treatment period, or if they were caused by any underlying disease or S-amlodipine 2.5 mg monotherapy. The adverse events were further assessed to determine their clinical significance. Any serious adverse event was reported to the Chong Kun Dang Pharmaceutical Corp within 24 h or at least by the next business day.
Subjects with an adverse event were examined and treated properly. Serious adverse events were followed-up until the event was resolved, abnormal laboratory finding had returned to baseline levels, or a satisfactory explanation could be found for the observed change unless the subject was lost to follow-up.
Sample size
The following hypothesis was formulated:
H0: μt − μc ≤0 vs H1: μt − μc >0 |
where μt, mean sitDBP change in each combination dose group; μc, mean sitDBP change in the S-amlodipine monotherapy group.
Aiming at a power of 80% and setting a two-sided alpha level at 0.05, considering a BP difference of 5.6 mmHg as clinically significant, with a standard deviation (SD) of 8.4, and assuming a dropout rate of 20%, 54 patients per group were required (Bonferroni test, with correction for multiple comparisons). According to the Phase II clinical trial of CKD-828 (ClinicalTrials.gov identifier; NCT01128322, unpublished), a BP difference of 5.6 mmHg was required to confirm the superiority of each combination treatment versus S-amlodipine monotherapy. When the SD for the measured variable was 8.4, it was estimated that 54 subjects were required for each group, assuming a 20% dropout rate. Therefore, the total target number of subjects was 162 for the two treatments groups and one control group.
Statistical analyses
Two-sided tests were performed at a significance level of 0.05 for all statistical analysis in this clinical trial. For any missing value at a certain point or subject dropout before the end of the clinical trial, the last observation carried forward method was applied for the efficacy analysis if the subject had been assessed for efficacy at least once after the baseline. The last observation carried forward method was not applied to the safety analysis. The subjects’ demographic information, past medical history, present illness, hematological condition, and concomitant medications were summarized for each group in the full analysis set.
The categorical data, such as sex, were presented as frequencies and percentages while the continuous data including age were presented as descriptive statistics, such as mean ± SD, median, minimum, and maximum. The frequency and percentage of each group were presented for past medical history and present illness. The frequency and percentage of subjects who had taken each category of concomitant medications were obtained and compared using a chi-square test to investigate if there was a statistically significant difference among the groups.
The efficacy was analyzed mainly in the full analysis set and secondarily in the per-protocol set. The change in sitDBP from baseline to Week 8 was obtained and compared between the groups to demonstrate the superiority of the study drug to the S-amlodipine 2.5 mg monotherapy. To demonstrate the superiority of the study drug to the comparator, an independent samples t-test was performed for the mean difference in BP reductions between the groups. In addition, the changes in sitDBP at Week 4 and sitSBP at Weeks 4 and 8 were compared among the groups using an independent samples t-test. As described earlier, the control and response rates were calculated and compared between the groups using the chi-square test.
Laboratory findings were described using descriptive statistics such as mean ± SD at each visit as well as pre- and posttreatment change. The between-group comparison was performed using independent samples t-test while pre- and posttreatment comparison were performed using a paired samples t-test. The McNemar test was used to analyze the change in the results of the physical examinations before and after treatment while the Chi-square or Fisher’s exact test was used for pre- and posttreatment comparison between the groups. The number of cases was estimated for the serious adverse events and adverse events related to the study drug while the chi-square or Fisher’s exact test was used to compare the groups.
Results
Patient characteristics
Among the 294 patients with hypertension screened, a total of 187 eligible patients were randomly assigned to receive CKD-828 2.5/40 mg (n=63), CKD-828 2.5/80 mg (n=63), or S-amlodipine 2.5 mg (n=61) after a 4-week treatment with once-daily S-amlodipine 2.5 mg. All the 187 randomized subjects were included in the safety set, and 184 were included in the full analysis set, 3 subjects were dropped out. Among the 184 subjects in the full analysis set, 158 were included in the per-protocol set, excluding 26 subjects who dropped out or took any drug that could have affected the results of the study or did not achieve 80% medication compliance (Figure 2).
Among the 187 randomized subjects, 23 had 27 cases of major protocol violations, and the most common being the use of contraindicated medications (n=12, 6.42%). Protocol violations were most frequently observed in the S-amlodipine 2.5 mg group (n=10, 16.39%), followed by the CKD-828 2.5/80 mg (n=8, 12.70%) and CKD-828 2.5/40 mg (n=5, 7.94%) groups, with no statistically significant difference. No differences were identified in the baseline demographic data, baseline medical history, laboratory findings, and vital signs among the three groups (Table 1).
Efficacy assessments
Primary endpoint
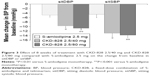
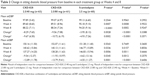
The mean sitDBP change from baseline to Week 8 was −9.67±6.50, −10.72±6.19, and −4.93±7.26 mmHg in the CKD-828 2.5/40 mg (P<0.0001), CKD-828 2.5/80 mg (P<0.0001), and S-amlodipine 2.5 mg (P<0.0001) groups, respectively, which were all significant BP reductions. The difference in mean sitDBP change was −4.73 and −5.79 mmHg in the CKD-828 2.5/40 mg and CKD-828 2.5/80 mg groups, respectively, versus the S-amlodipine 2.5 mg group. After adjusting the results of the independent samples t-test using the Bonferroni method, there was a significant difference between the S-amlodipine 2.5 mg and each CKD-828 group (CKD-828 2.5/40 mg: P=0.0002 and CKD-828 2.5/80 mg: P<0.0001), which indicated the superior antihypertensive effect of both combination treatments over the S-amlodipine 2.5 mg (Figure 3, Table 2).
Secondary endpoints
The mean sitDBP change from baseline to Week 4 was −8.29±7.65, −9.56±7.08, and −3.95±8.13 mmHg in the CKD-828 2.5/40 mg (P<0.0001), CKD-828 2.5/80 mg (P<0.0001), and S-amlodipine 2.5 mg (P=0.0002) groups, respectively, indicating a statistically significant antihypertensive effect compared to the baseline in all the groups. The difference in mean sitDBP change was −4.34 and −5.61 mmHg in the CKD-828 2.5/40 mg (P=0.0028) and CKD-828 2.5/80 mg (P<0.0001) groups versus the S-amlodipine 2.5 mg group, indicating the statistically superior antihypertensive effect of both combination treatments over S-amlodipine 2.5 mg.
The mean sitSBP change from baseline to Week 4 was −9.54±12.37, −11.93±10.97, and −4.62±13.16 mmHg in the CKD-828 2.5/40 mg (P<0.0001), CKD-828 2.5/80 mg (P<0.0001), and S-amlodipine 2.5 mg (P=0.0027) groups, respectively, indicating a statistically significant antihypertensive effect in all the groups. The difference in mean sitSBP change was −4.92 and −7.32 mmHg in the CKD-828 2.5/40 mg (P=0.0345) and CKD-828 2.5/80 mg (P=0.0012) groups versus the S-amlodipine 2.5 mg group (Table 2).
The mean sitSBP change from baseline to Week 8 was −12.89±11.78, −13.79±9.41, and −4.55±11.27 mmHg in the CKD-828 2.5/40 mg (P<0.0001), CKD-828 2.5/80 mg (P<0.0001), and S-amlodipine 2.5 mg (P<0.0001) groups, respectively. The difference in mean sitSBP change was −8.34 and −9.24 mmHg in the CKD-828 2.5/40 mg (P=0.0001) and CKD-828 2.5/80 mg (P<0.0001) groups versus the S-amlodipine 2.5 mg group (Figure 3, Table 2).
The number of subjects who achieved the target BP at Week 8 (ie, control rate) was 38 (60.32%), 37 (60.66%), and 17 (28.33%) in the CKD-828 2.5/40 mg (P=0.0004), CKD-828 2.5/80 mg (P=0.0003), and S-amlodipine 2.5 mg groups, respectively. Furthermore, the number of subjects who showed a response (ie, response rate) was 43 (68.25%, P=0.0017), 44 (72.13%, P=0.0004), and 24 (40.00%), respectively (Figure 4, Table 3).
Safety assessment
Among the 187 subjects in the safety set, 32 (17.11%) experienced 42 cases of adverse events, which were all mild or moderate. Adverse events were reported in six, nine, and 17 subjects in the CKD-828 2.5/40 mg, CKD-828 2.5/80 mg, and S-amlodipine 2.5 mg groups, respectively. The incidence of adverse events was significantly lower in the CKD-828 2.5/40 mg (9.52%, 10 cases) group than it was in the S-amlodipine 2.5 mg group (27.87%, 21 cases) (P=0.0086). Six cases of adverse drug reactions were reported in six subjects (3.21%), which were all mild or moderate, and were adverse events that are commonly reported with the use of the monotherapy (S-amlodipine besylate or telmisartan) or combination therapy of each drug on the market.
The nausea and serum aspartate aminotransferase elevation, which were reported only in the CKD-828 2.5/80 mg group, were also the adverse events that may have been caused by the monotherapy of either drug. The difference in the incidence of adverse drug reactions was not significant among the groups. Furthermore, edema, one of most common adverse event associated with amlodipine was not reported after the randomization and no other unexpected adverse events due to increasing the telmisartan dose were observed in the CKD-828 2.5/80 mg group compared to the CKD-828 2.5/40 mg. Finally, no serious adverse events were associated with the study drugs (Table 4).
Discussion
CKD-828 is a unique fixed-dose combination of telmisartan and S-amlodipine besylate as opposed the conventional amlodipine besylate. In the present study, the authors showed that the two fixed-dose combinations of S-amlodipine and telmisartan (CKD-828 2.5/40 mg and 2.5/80 mg) effectively lowered the BP in Korean patients with hypertension that was inadequately controlled with S-amlodipine 2.5 mg monotherapy. To the best of the authors knowledge, this is the first study to demonstrate the superiority of the efficacy of telmisartan and S-amlodipine besylate fixed-dose combinations over the conventional amlodipine besylate in reducing the BP of Korean patients with hypertension.
At 8 weeks, the authors discovered that the CKD-828 2.5/80 mg induced a significant double-digit reduction in the sitDBP/SBP (−10.72±6.19/−13.79±9.41 mmHg, P<0.0001) compared with that of the S-amlodipine monotherapy. The CKD-828 2.5/40 mg also induced a considerably higher sitDBP/SBP reduction (9.67±6.50/−12.89±11.78 mmHg, P<0.001) than the S-amlodipine monotherapy did. Furthermore, at 4 weeks, both fixed-dose combinations (CKD-828 2.5/80 and 2.5/40 mg) exhibited a more significant antihypertensive efficacy than the S-amlodipine monotherapy did. Comparing the antihypertensive effects of CKD-828 2.5/40 mg and CKD-828 2.5/80 mg, there was a nonsignificant tendency for CKD-828 2.5/80 mg providing a greater reduction in sitDBP and SBP at Weeks 4 and 8 than CKD-828 2.5/40 mg. Furthermore, both CKD-828 groups showed statistically significant control and response rates compared to the S-amlodipine group.
In a previous study, TEAMSTA-516 also showed a similar trend where amlodipine 5 mg/telmisartan 80 mg exhibited a greater antihypertensive effect than amlodipine 5 mg/telmisartan 40 mg did. The trend of greater antihypertensive effect with increasing telmisartan dose was also shown in this clinical trial. The authors findings are consistent with recent studies of telmisartan and amlodipine fixed-dose combinations.15,16,18–20
In general, angiotensin receptor blockers are preferred to angiotensin converting enzyme inhibitors because of the associated side effects, such as dry cough. Therefore, combination therapies, especially fixed-dose combinations consisting of an angiotensin receptor blocker and calcium channel blocker are frequently prescribed in clinical practice.
Among the fixed-dose combinations of angiotensin receptor blocker and calcium channel blocker, the combination of telmisartan and amlodipine has considerable clinical evidence supporting its beneficial antihypertensive efficacy.15,16 Achieving a comparable BP lowering effect requires a dose of S-amlodipine that is only half of the conventional amlodipine besylate.9,21 In addition, the dose reduction also beneficially decreases the rate of adverse events such as edema due to the additional natriuretic activity of telmisartan.9,21 However, no studies have reported the efficacy and safety of fixed-dose combinations of S-amlodipine/telmisartan in patients with hypertension.
Although numerous studies have shown similar adverse event incidences between a fixed-dose combination containing amlodipine/telmisartan and amlodipine monotherapy,15,16,18,19 this clinical trial showed a significantly lower adverse event incidence in the CKD-828 2.5/40 mg group than there was in the S-amlodipine 2.5 mg group. The differences of adverse event incidence between two groups in this clinical study may be due to the differences in the incidences of respiratory disorders.
Edema, one of the most common adverse events associated with amlodipine, was not reported in any group after the randomization. The authors guess that the additional natriuretic activity and relatively reduced dose of S-amlodipine besylate may have contributed to decreasing the rate of edema. Headache, one of the most common adverse events associated with amlodipine and telmisartan, was reported in one and three subjects (1.59% and 4.92%) in the CKD-828 2.5/80 mg and S-amlodipine 2.5 mg groups, respectively. Previous studies comparing a fixed-dose combination of amlodipine and telmisartan with amlodipine monotherapy reported that the incidence of headache was 2%–5.7% for the combination and 2.5%–6% for amlodipine monotherapy.15,16,19 Although the incidence of headache reported in the S-amlodipine 2.5 mg group in the present study was similar to those of the previous studies; it was lower in the CKD-828 2.5/80 mg group with no incidences in the CKD-828 2.5/40 mg group.
This study had several limitations that are worth mentioning. First, the authors only enrolled patients with mild-to-moderate hypertension without cardiovascular disease or other significant target organ damage and used a relatively short treatment duration. Therefore, it was not possible to observe the outcomes of hypertension including target organ damage and long-term adverse effects. Furthermore, this study included only Korean patients with hypertension, which would preclude, or at least limit, the application of these results to the general global population. In this study, the adverse events were assessed by only one method. However, this global introspection is a well-known and reliable method. The study design of this trial was not completely innovative or ethical, however, the study showed effectively the efficacy and safety of two fixed-dose combinations of S-amlodipine and telmisartan (CKD-828). In addition, this study did not assess concurrent life style modification or compare with other drug regimens or intensive life style modification. And the authors did not include an arm of switch to another medication after insufficient response to amlodipine monotherapy during the run-in period. This study design was focused to evaluate BP lowering efficacy and safety of only CKD-828 in patients with hypertension inadequately controlled with S-amlodipine monotherapy for a relatively short duration. Finally, the authors did not assess tolerability, acceptability, and palatability.22 However, compliance was assessed by means of check of returned medications. The authors enrolled the patients who achieved more than 80% medication compliance. On the other hand, the strength of this study was the BP measurement. The BP was obtained as the mean of three consecutive measurements. The potential advantages of this methodology are minimizing the white coat effect.
Conclusion
The two fixed-dose combination CKD-828 (2.5/40 and 2.5/80 mg) formulations of S-amlodipine/telmisartan exhibited superior antihypertensive effects. The authors safety analysis revealed that all the reported adverse drug reactions were mild or moderate, and were not different from the adverse events previously reported with combination or monotherapies of these drugs. The CKD-828 2.5/40 mg-associated adverse events incidence was significantly lower than that of S-amlodipine monotherapy. Furthermore, increasing the telmisartan dose did not result in the occurrence of any unexpected or serious adverse event, indicating the safety of CKD-828. Taken together, these results indicate that the CKD-828 combination is an effective and safe option for patients with inadequate responses to S-amlodipine monotherapy.
Acknowledgments
This study was initiated and financially supported by the Chong Kun Dang Pharmaceutical Co., Ltd. They provided financial support for procuring the medicines and laboratory tests and engaging the clinical research coordinator. The funding body had no role in the analysis and interpretation of the data or writing of the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
Weber MA, Schiffrin EL, White WB, et al. Clinical practice guidelines for the management of hypertension in the community: a statement by the American society of hypertension and the international society of hypertension. J Clin Hypertens (Greenwich). 2014;16(1):14–26. | ||
Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349):1903–1913. | ||
2013 Practice guidelines for the management of arterial hypertension of the European society of hypertension (ESH) and the European society of cardiology (ESC): ESH/ESC Task Force for the Management of Arterial Hypertension. J Hypertens. 2013;31(10):1925–1938. | ||
Shin J, Park JB, Kim KI, et al. 2013 Korean Society of Hypertension guidelines for the management of hypertension. Part II – treatments of hypertension. Clin Hypertens. 2015;21:2. | ||
Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2572. | ||
Hung YJ, Chen JF, Wang CY, Lee WJ, Sheu WH. Comparison of the efficacy and safety profiles of two fixed-dose combinations of antihypertensive agents, amlodipine/benazepril versus valsartan/hydrochlorothiazide, in patients with type 2 diabetes mellitus and hypertension: a 16-week, multicenter, randomized, double-blind, noninferiority study. Clin Ther. 2012;34(8):1735–1750. | ||
Kostis JB. Antihypertensive therapy with CCB/ARB combination in older individuals: focus on amlodipine/valsartan combination. Am J Ther. 2010;17(2):188–196. | ||
Fogari R, Malamani G, Zoppi A, Mugellini A, Rinaldi A, Perrone T. Effect on the development of ankle edema of adding delapril to manidipine in patients with mild to moderate essential hypertension: a three-way crossover study. Clin Ther. 2007;29(3):413–418. | ||
Kim SA, Park S, Chung N, et al. Efficacy and safety profiles of a new S(-)-amlodipine nicotinate formulation versus racemic amlodipine besylate in adult Korean patients with mild to moderate hypertension: an 8-week, multicenter, randomized, double-blind, double-dummy, parallel-group, Phase III, noninferiority clinical trial. Clin Ther. 2008;30(5):845–857. | ||
Noh YH, Lim HS, Kim YH, et al. Pharmacokinetic interaction of telmisartan with s-amlodipine: an open-label, two-period crossover study in healthy Korean male volunteers. Clin Ther. 2012;34(7):1625–1635. | ||
Rizos CV, Elisaf MS, Liberopoulos EN. Are the pleiotropic effects of telmisartan clinically relevant? Curr Pharm Des. 2009;15(24):2815–2832. | ||
Bangalore S, Kamalakkannan G, Parkar S, Messerli FH. Fixed-dose combinations improve medication compliance: a meta-analysis. Am J Med. 2007;120(8):713–719. | ||
Law M, Morris JK, Bestwick JP, Wald NJ. Combination therapy versus monotherapy in reducing blood pressure: meta-analysis on 11,000 participants from 42 trials. Am J Med. 2009;122(3):290–300. | ||
Salahuddin A, Mushtaq M, Materson BJ. Combination therapy for hypertension 2013: an update. J Am Soc Hypertens. 2013;7(5):401–407. | ||
Littlejohn TW, Majul CR, Olvera R, et al. Results of treatment with telmisartan-amlodipine in hypertensive patients. J Clin Hypertens. 2009;11(4):207–213. | ||
Neldam S, Lang M, Jones R. Telmisartan and amlodipine single-pill combinations vs amlodipine monotherapy for superior blood pressure lowering and improved tolerability in patients with uncontrolled hypertension: results of the TEAMSTA-5 study. J Clin Hypertens. 2011;13(7):459–466. | ||
Pickering TG, Hall JE, Appel LJ, et al. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the subcommittee of professional and public education of the American heart association council on high blood pressure research. Hypertension. 2005;45(1):142–161. | ||
Sharma A, Bagchi A, Kinagi S, Sharma Y, Baliga V, Bollmall C. Results of a comparative, phase III, 12-week, multicenter, prospective, randomized, double-blind assessment of the efficacy and tolerability of a fixed-dose combination of telmisartan and amlodipine versus amlodipine monotherapy in Indian adults with stage II hypertension. Clin Ther. 2007;29(12):2667–2676. | ||
Sharma AM, Bakris G, Neutel JM, et al. Single-pill combination of telmisartan/amlodipine versus amlodipine monotherapy in diabetic hypertensive patients: an 8-week randomized, parallel-group, double-blind trial. Clin Ther. 2012;34(3):537–551. | ||
Segura J, Ruilope LM. Clinical utility of fixed-combination telmisartan-amlodipine in the treatment of hypertension. Integr Blood Press Control. 2011;4:27–34. | ||
Liu F, Qiu M, Zhai SD. Tolerability and effectiveness of (S)-amlodipine compared with racemic amlodipine in hypertension: a systematic review and meta-analysis. Curr Ther Res. 2010;71(1):1–29. | ||
Ferrarini A, Bianchetti AA, Fossali EF, et al. What can we do to make antihypertensive medications taste better for children? Int J Pharm. 2013;457(1):333–336. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.