Back to Journals » Drug Design, Development and Therapy » Volume 11
Efficacy and safety of quadruple therapy including tirofiban in the treatment of Chinese NSTE-ACS patients failing to receive timely percutaneous coronary intervention
Authors Li L, Ge Z, Zhang D, Kuang J, Ma X, Jiang S
Received 4 April 2017
Accepted for publication 24 July 2017
Published 21 November 2017 Volume 2017:11 Pages 3299—3307
DOI https://doi.org/10.2147/DDDT.S138714
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Qiongyu Guo
Lan Li,1 Zhenrong Ge,1 Dengke Zhang,1 Jun Kuang,2 Xiang Ma,3 Shubin Jiang1
1Coronary Care Unit, The Traditional Chinese Medicine Hospital, Xinjiang Medical University, 2Department of Cardiology, General Hospital of Xinjiang Military Command, 3Department of Cardiology, First Affiliated Hospital of Xinjiang Medical University, Urumqi, People’s Republic of China
Background: Although it has been shown to be superior to simple antithrombotic drug therapy, most patients are unable to receive timely percutaneous coronary intervention (PCI) and are treated with conventional triple antithrombotic therapy (aspirin, clopidogrel, low-molecular-weight heparin). Here, we evaluate the efficacy and safety of adding low-dose tirofiban to this regimen.
Methods: A total of 1,783 patient records (unable to receive PCI) indicating non-ST-segment elevation acute coronary syndrome (NSTE-ACS) were included. A total of 882 received conventional triple antithrombotic therapy; 901 received quadruple antithrombotic therapy. Efficacy was evaluated in terms of major adverse cardiovascular event (MACE) parameters. Safety was evaluated based on the occurrence of bleeding events. Data were collected over a 6-month period post treatment.
Results: The rate of occurrence of MACE was significantly lower in the quadruple antithrombotic group (10.5% versus 14.1% at 6 months, P=0.02). The log-rank test showed improved survival in the quadruple antithrombotic group. Total bleeding events were higher in the quadruple antithrombotic group (9.7%) than in the triple antithrombotic group (7.1%) (P=0.04); however, this may be attributed to increased clinically insignificant minor bleeding events.
Conclusion: Quadruple antithrombotic therapy demonstrated a superior alternative for the treatment of high-risk NSTE-ACS patients failing to receive PCI.
Keywords: low-dose tirofiban, non-ST-segment elevation acute coronary syndrome, quadruple drug therapy
Introduction
Cardiovascular disease is a major cause of mortality worldwide, and coronary artery disease and acute coronary syndrome (ACS) account for two of its major manifestations. ACS is also known to be one of the leading causes of mortality in the Asia-Pacific region, and studies in Chinese non-ST-segment elevation acute coronary syndrome (NSTE-ACS) patients have shown that there is a higher variability in treatment outcomes associated with higher mortality rates when compared to the rest of the Asia-Pacific region.1 This difference may be attributed to the fact that relevant guidelines, although present, are not strictly followed by clinicians for a variety of reasons.2 Recent guidelines recommend the adoption of aggressive revascularization procedures such as percutaneous coronary intervention (PCI) as the primary mode of treatment for patients presenting with high-risk NSTE-ACS.3–5 However, although PCI has been shown to be superior to simple antithrombotic drug therapy for the management of such patients, the GRACE study showed that only 32.5% were able to receive direct PCI.6 Thus, most patients are treated with traditional triple antithrombotic therapy that includes aspirin, clopidogrel and low-molecular-weight heparin.3–5 Issues pertaining to the administration and regulation of drug therapy for these high-risk NSTE-ACS patients who do not receive PCI in routine clinical practice due to several patient dependent factors have consistently plagued clinicians.7
ACS is mainly caused by platelet aggregation and thrombus formation leading to coronary atherosclerotic plaque rupture. Therefore, several studies indicate that drug treatment for this condition should be dominated by antiplatelet agents.8 Studies have shown that the addition of platelet receptor antagonists to traditional triple antithrombotic therapy administered to NSTE-ACS patients is associated with an effective inhibition of platelet function and a reduction in cardiovascular adverse events.9 Tirofiban is one such antiplatelet agent.10 However, balancing the effective use of active antithrombotic therapy while simultaneously reducing the risk of bleeding events in patients has proved extremely difficult and represents an important concern amongst clinicians.
We hypothesize that the addition of tirofiban to traditional triple antithrombotic therapy11 for the treatment of patients with high-risk NSTE-ACS who fail to receive PCI for various reasons can further enhance the antiplatelet function of the treatment regimen and reduce the occurrence of major adverse cardiovascular event (MACE). However, taking into account the possibility of an increased risk of bleeding, the dose of tirofiban administered as part of the quadruple therapy regimen was lowered, in addition to which the low-molecular-weight heparin dose was also halved. Thus, quadruple antithrombotic therapy comprised aspirin, clopidogrel, half-dose low-molecular-weight heparin and low-dose tirofiban.
In this work, we reviewed the adoption of quadruple antithrombotic therapy for the treatment of patients with high-risk NSTE-ACS who were unable to undergo PCI in time and to assess the efficacy and safety of an additional low dose of tirofiban for patients with high-risk NSTE-ACS compared with conventional triple anti-thrombus therapy.
Methods
Study design and participants
This was a long-term, multicenter, retrospective study to evaluate the efficacy and safety of traditional triple antithrombotic therapy (excluding low-dose tirofiban) versus quadruple antithrombotic therapy (including low-dose tirofiban) for the treatment of high-risk NSTE-ACS patients who fail to receive timely PCI. Efficacy of the two treatment regimens was evaluated by comparing the rate of occurrence of MACE, while the safety was evaluated by comparing the rate of occurrence of bleeding events (classified by the Bleeding Academic Research Consortium [BARC] standard). Data for both evaluations were collected at time points over the short-term (72 hours and 7 days) and long term (1, 3 and 6 months).
We reviewed 4,572 patient records from 3 different centers (The First Affiliated Hospital of Xinjiang Medical University and The Affiliated traditional Chinese Medicine Hospital of Xinjiang Medical University and the General Hospital of Xinjiang Military District) that indicated ACS between January 2007 and August 2016. A total of 1,895 high-risk NSTE-ACS patients who did not receive emergency PCI (within 72 hours of admission) met the inclusion criteria.
High-risk patients aged between 18 and 85 years meeting the American Heart Association (AHA) NSTE-ACS criteria3,5 who did not immediately undergo PCI for a variety of reasons were included in the study population. In addition, all patients had GRACE scores12,13 greater than or equal to 140 points, CRUSADE scores (Can Rapid risk stratification of Unstable angina patients Suppress Adverse outcomes with Early implementation of the ACC/AHA guidelines)14 less than 50 and creatinine clearance rates (calculated according to Cockcroft-Gault formula) greater than 30 mL/min, since patients who have renal impairment also have a higher risk of suffering from bleeding events.
Patients who received prior PCI therapy or who demonstrated abnormal liver function and renal function or systolic blood pressure greater than 180 mmHg and/or diastolic blood pressure greater than 110 mmHg were excluded. In addition, patients with malignant tumors and life expectancy less than 1 year or with an elevated risk of bleeding (including patients with a history of peptic ulcers, alimentary tract hemorrhage and clinically significant urogenital canal hemorrhage; previous or current platelet count less than 100,000/L; history of intracranial hemorrhage; history of cerebral infarction within 6 months; history of intracranial tumors; history of arteriovenous malformations and arteriovenous tumors; history of trauma and operation within 3 months) were also excluded.
Study conduct
Patients were divided into two groups: the triple antithrombotic therapy group (excluding tirofiban) and the quadruple antithrombotic therapy group (including low-dose tirofiban). Triple antithrombotic therapy comprised a combination of aspirin, clopidogrel and low-molecular-weight heparin. Aspirin and clopidogrel were both administered orally. Aspirin was administered at an initial dose of 300 mg followed by a long-term maintenance dose of 75–100 mg once daily. Clopidogrel was administered at an initial dose of 300 mg, followed by a long-term maintenance dose of 75 mg once daily. Low-molecular-weight heparin (enoxaparin) was injected subcutaneously at the standard recommended dose of 1 mg/kg once every 12 hours, or 0.75 mg/kg once every 12 hours for patients ≥75 years of age.
Quadruple antithrombotic therapy comprised a low dose of tirofiban hydrochloride in addition to standard triple antithrombotic therapy. Tirofiban was administered by intravenous pumping at a loading dose of 0.4 μg/kg/min for 30 minutes, followed by intravenous infusion at a maintenance dose of 0.1 μg/kg/min for 48–72 hours. The administration and dose of aspirin and clopidogrel remained the same as that of the triple antithrombotic group, while the dose of low-molecular-weight heparin was adjusted to half of what is normally recommended during the administration of tirofiban, ie, 0.5 mg/kg once every 12 hours or 0.375 mg/kg once every 12 hours for patients ≥75 years of age. Once tirofiban administration ceased, the standard dose of low-molecular-weight heparin was resumed for 2–3 days, ie, 1 mg/kg once every 12 hours or 0.75 mg/kg once every 12 hours for patients ≥75 years of age.
The study was performed in accordance with the Declaration of Helsinki, the International Conference on Harmonization/Good Clinical Practice. The study protocol was approved by the Ethics Review Committee (reference number 2011XE097) of The First Affiliated Hospital of Xinjiang Medical University and The Affiliated Traditional Chinese Medicine Hospital of Xinjiang Medical University and the General Hospital of Xinjiang Military District, and written informed consent was obtained from all participants. The study methods were conducted in accordance with approved national and international guidelines.
Study outcomes
Efficacy
The efficacy of the two treatment regimens was compared by estimating the occurrence rate of MACE defined as either all-cause mortality, recurrent angina or recurrent fatal/non-fatal myocardial infarction, ischemic stroke and transient ischemic attack in both treatment groups at 72 hours and 7 days (short term occurrence of MACE) and at 1 month, 3 months and 6 months post-treatment initiation. Since PCI was a discharge indicator for the study population, cardiac revascularization (stent or coronary artery bypass surgery) was not included in the estimation of efficacy. Only the first event of each outcome was included in the analysis.
All-cause mortality was classified as vascular unless the central adjudication committee confirmed an unequivocal non-cardiovascular cause of death. Cardiovascular death included death due to peripheral artery disease, hemorrhagic stroke, sudden death, progressive congestive heart failure and procedure-related death.
The incidence of myocardial infarction was confirmed by measuring the change in cardiac biomarker levels along with the occurrence of at least one ischemic event defined as either sustained chest pain without remission, new ECG ST-segment changes or left bundle branch block, pathological Q wave formation or iconography showing new loss of myocardial viability. If a patient died within 4 weeks of myocardial infarction or ischemic stroke, this event was recorded as fatal myocardial infarction.
Ischemic stroke was determined based on clinical manifestations and confirmed by radiological findings. Transient ischemic attack was defined according to the Classification of Cerebrovascular Diseases.
The incidence of recurrent angina pectoris was confirmed by documenting the presence of sustained chest pain for more than 5 minutes or any new change that occurred on the two adjacent leads of the ECG readout without any change in cardiac markers (enzyme levels) for myocardial infarction.
Safety
Occurrence of bleeding events (based on the BARC standard15) at 72 hours, 7 days, 1 month, 3 months and 6 months post-treatment initiation were compared between the two therapy groups. The incidence of death due to any reason was also estimated in both treatment groups.
Statistical analysis
The SPSS17.0 software package was used for statistical analysis. All data sets pertaining to the main statistical indicators of the study were subjected to a normality test. Every statistical indicator that was normally distributed is shown as mean ± standard deviation (χ-±s). An independent samples t-test was used to compare data between groups, and chi-square test was used for categorical data. The Wilcoxon rank sum test was used to estimate the rank sum test statistic (a=0.05). P≤0.05 was considered statistically significant.
Results
Baseline characteristics
Of the 1,895 patient records screened, 79 patients were treated with PCI between 3 and 180 days of admission and were therefore excluded from the study analyses. Thirty-three cases were lost to follow-up. Thus, 1,783 patients completed the study, including 882 patients treated with triple antithrombotic therapy and 901 patients treated with quadruple antithrombotic therapy. Patients were allowed to choose the treatment regimen they preferred, and administration of either triple or quadruple antithrombotic therapy was initiated based on patient preference. The population selection algorithm is presented in Figure 1.
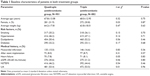
There was no statistical difference in age, sex, weight and pre-existing risk factors between the two groups of patients (Table 1). The only significant differences that existed between the two groups were pertaining to the use of tirofiban (Table 2).
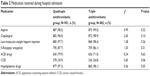  | Table 2 Medication received during hospital admission |
Study outcomes
Efficacy
There was no statistical difference in either the mortality rate or the rate of recurrent myocardial infarction between the two groups at the 72-hour, 7-day and 6-month post-treatment time points. However, the rate of occurrence of recurrent angina pectoris at the 72-hour post-treatment time point in the quadruple antithrombotic group was 2.0%, which was 45.9% lower than that of triple antithrombotic group (P<0.05). Thus, at the 72-hour time point, the rate of occurrence of MACE in the quadruple antithrombotic group was 4.6%, which was 37.0% lower than that of triple antithrombotic group P<0.05 (Table 3).
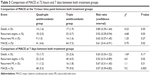  | Table 3 Comparison of MACE at 72 hours and 7 days between both treatment groups |
Similarly, at the 7-day post-treatment time point, the rate of occurrence of recurrent angina pectoris in the quadruple antithrombotic group was 46.7% lower than that of the triple antithrombotic group, P<0.05. Thus, even at the 7-day post-treatment time-point, the rate of occurrence of MACE in the quadruple antithrombotic group was 41.1% lower than that of the triple antithrombotic group, P<0.05 (Table 3).
The rate of occurrence of MACE in the quadruple antithrombotic therapy group at the 1-month and 3-month time points was 34.8% and 32.8% lower than that of the triple antithrombotic therapy group (P<0.05), respectively. Thus, there was a significant difference in the mortality rates between both groups at the 1-month and 3-month post-treatment time points (P<0.05). However, no significant differences in the 6-month mortality rate, rate of recurrent angina pectoris and rate of recurrent myocardial infarction were detected between the two groups (Table 4).
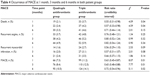  | Table 4 Occurrence of MACE at 1 month, 3 months and 6 months in both patient groups |
Survival data were analyzed using the Kaplan–Meier log rank test (Figure 2). Results showed that the survival rate of the quadruple antithrombotic therapy group was significantly higher than that of the triple antithrombotic therapy group (P=0.002).
  | Figure 2 Kaplan–Meier curve showing survival functions in both therapy groups over a 6-month follow-up period. |
In addition, a univariate analysis was conducted to assess the effect of different baseline characteristics on the occurrence of MACE. In the quadruple therapy group, characteristics such as history of MI, renal failure, high body weight, age and smoking were found to be significantly associated with the occurrence of MACE (Table 5A). In the triple therapy group, heart failure and age were also shown to have a significant effect on the occurrence of MACE in addition to those baseline characteristics found to affect MACE occurrence in the quadruple therapy group (Table 5B).
  | Table 5 Univariate analysis for MACE occurrence |
Safety
At the 72-hour time point, an equal number of Type 2, Type 3a and Type 3b bleeding events occurred in both treatment groups. All events were successfully resolved after giving symptomatic treatment. In one case, hemoglobin levels decreased to ≤3 g/dL. This was resolved after slowing down the administration tirofiban. Another patient suffered hematuresis with hemoglobin levels decreased to 3–5 g/dL. This was resolved after stopping the administration of tirofiban and low-molecular-weight heparin and blood transfusion. In another two cases, upper gastrointestinal bleeding occurred with hemoglobin levels decreased by ≥5 g/dL. The bleeding stopped after stopping the administration of tirofiban and low-molecular-weight heparin and giving blood transfusion along with an intravenous infusion of dopamine, saline, low molecular dextran, pantoprazole and other symptomatic treatment to elevate blood pressure, expand blood volume and stop bleeding. Both groups showed gingival bleeding, subcutaneous ecchymosis, epistaxis, hemoptysis, etc. (BARC Type 1 bleeding events). However, the occurrence rate of such Type 1 events in the triple antithrombotic therapy group at the 72-hour time point was 4.5%, which was significantly lower than the rate of occurrence of such events in the quadruple antithrombotic therapy group, which was 7.1%. These minor bleeding events improved in the quadruple antithrombotic therapy group after tirofiban treatment was discontinued. There was one case of Type 5b hemorrhage in the triple antithrombotic therapy group, with intracranial hemorrhage that resulted in death. No Type 5 hemorrhage occurred in the quadruple antithrombotic therapy group.
Thus, the overall occurrence of bleeding events was significantly higher in the quadruple antithrombotic therapy group than in the triple antithrombotic therapy group at all time points, mainly due to an increase in Type 1 bleeding events within 72 hours. However, there was no difference in the rate of occurrence of these various new bleeding events between the two groups after 72 hours (Table 6).
  | Table 6 Occurrence of hemorrhage at 72 hours, 7 days, 1 month, 3 months and 6 months in both patient groups |
Discussion
A number of studies have demonstrated that aggressive, invasive revascularization measures such as PCI are more effective than conservative triple antithrombotic drug therapy in the management of patients with high-risk NSTE-ACS.3–5 However, the actual number of such patients receiving direct PCI in People’s Republic of China in routine clinical practice is very low compared to the rest of the global population. This difference may be attributed to a variety of factors, the primary one being self-perceived patient risk upon opting for surgery followed by the provisions of existing health care systems.6,16 Guidelines recommend the addition of tirofiban to the standard triple therapy regimen for patients with NSTE-ACS whose condition worsens prior to surgery, with the main aim of treatment being early revascularization.3,5 However, the optimal composition of the treatment regimen remains uncertain and these guidelines have also acknowledged that there is a gap in high-quality evidence that concerns the long-term use of such medication.17
The safety and efficacy of the use of tirofiban in NSTE-ACS patients who have already received PCI or for those who are scheduled to receive PCI have also been established in previous investigations in Caucasian as well as Chinese populations.18–21 However, previous studies that assessed the efficacy of the combination of a conventional dose of tirofiban and low-molecular-weight heparin in the treatment of NSTE-ACS after PCI have shown an increased incidence of hemorrhage.15 Other studies that have halved the conventional dose of low-molecular-weight heparin and applied low-dose tirofiban as well in the treatment of medium-risk NSTE-ACS patients with diabetes have obtained better results.22 Based on the recommendations of these established guidelines and previous investigations, we reviewed and analyzed the clinical efficacy and safety of triple and quadruple antithrombotic therapy in reducing ischemic events in patients with high-risk NSTE-ACS who cannot receive PCI for a variety of reasons in routine clinical practice.
Our data show that in comparison with conventional triple antithrombotic therapy, quadruple antithrombotic treatment including a low dose of tirofiban can significantly reduce ischemic events and can also reduce the mortality rate of patients over a 3-month time period while simultaneously resulting in an absence of any increase in clinically significant bleeding events. In addition, the Kaplan–Meier log rank test also showed a significant difference in favor of quadruple treatment in survival over a 6-month time period between the two groups of patients. Our results are in accordance with previous studies that support the use of quadruple antithrombotic treatment in the management of high-risk NSTE-ACS patients.22
Thus, we demonstrate that a combination of aspirin, clopidogrel, low-dose low-molecular-weight heparin and low-dose tirofiban is more effective than traditional triple antithrombotic therapy in the management and survival of patients with high-risk NSTE-ACS who fail to receive timely PCI. Importantly, our results also indicate that the risk of clinically significant bleeding does not increase while using quadruple therapy including a low dose of tirofiban. This regimen provides an effective alternative for a particularly high-risk set of patients who cannot receive surgical intervention and who are otherwise prone to adverse cardiac outcomes.
Acknowledgment
This study was supported by grants from the Xinjiang Uygur Autonomous Region Science and Technology Department (grant number: 201554143).
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Ohira T, Iso H. Cardiovascular disease epidemiology in Asia: an overview. Circ J. 2013;77(7):1646–1652. | ||
Chan MY, Du X, Eccleston D, et al. Acute coronary syndrome in the Asia-Pacific region. Int J Cardiol. 2016;202:861–869. | ||
Anderson JL, Adams CD, Antman EM, et al. 2012 ACCF/AHA focused update incorporated into the ACCF/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61(23):e179–e347. | ||
Hillis LD, Smith PK, Anderson JL, et al; American College of Cardiology Foundation; American Heart Association Task Force on Practice Guidelines; American Association for Thoracic Surgery; Society of Cardiovascular Anesthesiologists; Society of Thoracic Surgeons. 2011 ACCF/AHA Guideline for coronary artery bypass graft surgery. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Developed in collaboration with the American Association for Thoracic Surgery, Society of Cardiovascular Anesthesiologists, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2011;58(24):e123–e210. | ||
Levine GN, Bates ER, Blankenship JC, et al; American College of Cardiology Foundation; American Heart Association Task Force on Practice Guidelines; Society for Cardiovascular Angiography and Interventions. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol. 2011;58(24):e44–e122. | ||
Fox KA, Anderson FA Jr, Dabbous OH, et al; GRACE investigators. Intervention in acute coronary syndromes: do patients undergo intervention on the basis of their risk characteristics? The Global Registry of Acute Coronary Events (GRACE). Heart. 2007;93(2):177–182. | ||
Van de Werf F. Decade in review – acute coronary syndromes: successes and future objectives in acute coronary syndrome. Nat Rev Cardiol. 2014; 11(11):624–625. | ||
Dobesh PP, Trujillo TC. Anticoagulation in the management of non-ST-segment elevation acute coronary syndrome. J Pharm Pract. 2010; 23(4):324–334. | ||
Liu N, Hou M, Ren W, Cao J, Wu H, Zhou W. Clinical research of treatment with tirofiban for high-risk non-ST-segment elevation acute coronary syndrome during peri-operative intervention operation period. Cell Biochem Biophys. 2015;71(1):43–47. | ||
King S, Short M, Harmon C. Glycoprotein IIb/IIIa inhibitors: the resurgence of tirofiban. Vascul Pharmacol. 2016;78:10–16. | ||
Valgimigli M, Minarelli M. Triple antiplatelet therapy in acute coronary syndromes. Drugs. 2011;71(13):1703–1719. | ||
Section of Interventional Cardiology of Chinese Society of Cardiology of Chinese Medical Association; Specialty Committee on Prevention and Treatment of Thrombosis of Chinese College of Cardiovascular Physicians; Editorial Board of Chinese Journal of Cardiology. [Chinese guideline for percutaneous coronary intervention (2016)]. Zhonghua Xin Xue Guan Bing Za Zhi. 2016;44(5):382–400. Chinese. | ||
Rapezzi C, Biagini E, Branzi A. Guidelines for the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes: the task force for the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes of the European Society of Cardiology. Eur Heart J. 2008;29(2):277–278. | ||
Subherwal S, Bach RG, Chen AY, et al. Baseline risk of major bleeding in non-ST-segment-elevation myocardial infarction: the CRUSADE (Can Rapid risk stratification of Unstable angina patients Suppress ADverse outcomes with Early implementation of the ACC/AHA Guidelines) Bleeding Score. Circulation. 2009;119(14):1873–1882. | ||
Mehran R, Rao SV, Bhatt DL, et al. Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the Bleeding Academic Research Consortium. Circulation. 2011;123(23):2736–2747. | ||
Chen Y, Jiang L, Zhang Q, et al. Doctor-reported hospital management of acute coronary syndrome in China: a nationwide survey of 1029 hospitals in 30 provinces. World J Cardiovasc Dis. 2012;2(3):168–176. | ||
Potpara TS, Lip GY, Dagres N, Estner HL, Larsen TB, Blomström- Lundqvist C; Conducted by the Scientific Initiatives Committee, European Heart Rhythm Association. Management of acute coronary syndrome in patients with non-valvular atrial fibrillation: results of the European Heart Rhythm Association Survey. Europace. 2014;16(2):293–298. | ||
Liu T, Xie Y, Zhou YJ, et al. Effects of upstream tirofiban versus downstream tirofiban on myocardial damage and 180-day clinical outcomes in high-risk acute coronary syndromes patients undergoing percutaneous coronary interventions. Chin Med J (Engl). 2009;122(15):1732–1737. | ||
Ferguson JJ, Califf RM, Antman EM, et al; SYNERGY Trial Investigators. Enoxaparin vs unfractionated heparin in high-risk patients with non-ST-segment elevation acute coronary syndromes managed with an intended early invasive strategy: primary results of the SYNERGY randomized trial. JAMA. 2004;292(1):45–54. | ||
Tricoci P, Newby LK, Hasselblad V, et al. Upstream use of small-molecule glycoprotein iib/iiia inhibitors in patients with non-ST-segment elevation acute coronary syndromes: a systematic overview of randomized clinical trials. Circ Cardiovasc Qual Outcomes. 2011;4(4): 448–458. | ||
Yan Z, Zhou Y, Zhao Y, et al. Efficacy and safety of tirofiban in high-risk patients with non-ST-segment elevation acute coronary syndromes. Clin Cardiol. 2009;32(9):E40–E44. | ||
Timmer JR, ten Berg J, Heestermans AA, et al. Pre-hospital administration of tirofiban in diabetic patients with ST-elevation myocardial infarction undergoing primary angioplasty: a sub-analysis of the On-Time 2 trial. EuroIntervention. 2010;Aug 6(3):336–342. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.