Back to Journals » Drug Design, Development and Therapy » Volume 12
Efficacy and safety of nicorandil on perioperative myocardial injury in patients undergoing elective percutaneous coronary intervention: results of the PENMIPCI trial
Authors Ye Z, Lu H, Su Q, Long M , Li L
Received 12 May 2018
Accepted for publication 27 June 2018
Published 22 August 2018 Volume 2018:12 Pages 2591—2599
DOI https://doi.org/10.2147/DDDT.S173931
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Anastasios Lymperopoulos
Ziliang Ye,1 Haili Lu,2 Qiang Su,1 Manyun Long,1 Lang Li1
On behalf of the PENMIPCI investigators
1Department of Cardiology, The First Affiliated Hospital of Guangxi Medical University, Nanning, Guangxi, People’s Republic of China; 2Department of Orthodontics, The Affiliated Dental Hospital of Guangxi Medical University, Nanning, Guangxi, People’s Republic of China
Background: Previous studies have indicated that nicorandil can reduce perioperative myocardial injury (PMI) in patients undergoing elective percutaneous coronary intervention (ePCI), but this conclusion is still controversial. Additionally, studies reporting on the safety of nicorandil are lacking. Therefore, we performed this prospective study to evaluate the efficacy and safety of nicorandil on PMI in patients undergoing ePCI.
Methods: One hundred and forty-six patients with coronary heart disease (CHD) scheduled to undergo ePCI were randomly assigned to the nicorandil group (n=74) or control group (n=72). The primary outcomes were the change in cardiac troponin T (cTnT) and creatine kinase-MB (CK-MB) at 12 and 24 hours after surgery. The secondary outcome was the incidence of major adverse cardiac events (MACE), which was a composite of cardiac death, nonfatal myocardial infarction, new heart failure or coronary revascularization.
Results: There was no difference in age (54.76±5.93 vs 56.35±5.22) between the nicorandil group and the control group. In addition, no differences were observed in the cTnT and CK-MB levels between the two groups at admission (all P>0.05). Compared with those in the control group, the cTnT (0.15±0.12 vs 0.12±0.10 at 12 hours and 0.17±0.12 vs 0.13±0.10 at 24 hours) and CK-MB (15.35±8.23 vs 12.31±7.93 at 12 hours and 13.63±8.87 vs 11.13±5.71 at 24 hours) levels in the nicorandil group were significantly decreased after surgery (all P<0.05). Furthermore, nicorandil did not increase the incidence of MACE in the nicorandil group compared with the control group (12.16% vs 12.50%).
Conclusions: Nicorandil can reduce PMI in patients undergoing ePCI and does not increase the incidence of MACE.
Clinical Trial Registration: URL: http://www.chictr.org.cn/. Unique Identifier: ChiCTR-IOR-17012056.
Keywords: nicorandil, perioperative myocardial injury, elective percutaneous coronary intervention
Introduction
With the continuous development of the social economy, people’s way of life has undergone profound changes.1 In addition, due to the aging of the population and the accelerated process of urbanization, the prevalence of cardiovascular disease risk factors is increasing year by year, which leads to an increasing number of cardiovascular diseases.2–4 According to some research reports, cardiovascular disease is the leading cause of death among urban and rural residents in China.5–7 Coronary heart disease (CHD) is one of the most common cardiovascular diseases, and its mortality has also been on the rise in recent years.8–10 In general, the increasing burden of cardiovascular diseases has become a major public health problem all over the world.11–13
The results of a clinical study showed that percutaneous coronary intervention (PCI) is an effective way to treat CHD.14 However, periprocedural myocardial injury (PMI)15,16 is a common complication of elective PCI. Previous studies have shown that PMI can directly reduce myocardial cell viability and cardiac function.17 Furthermore, PMI can lead to various serious events.18,19 Therefore, preventing PMI during elective PCI is a key concern of clinicians.
Nicorandil, an N-nicotinoyl nitrate drug, which can lead to diastolic coronary artery dilation, antagonizes platelet activation and eliminates inflammatory mediators, is used to treat various ischemic and cardiovascular diseases.16,20 Previous studies have shown that nicorandil used in PCI can improve myocardial perfusion and reduce the incidence of PMI.16,21,22 However, this conclusion is still controversial. Some scholars have noted that nicorandil can significantly prevent myocardial injury during PCI,21,23,24 while other scholars have indicated that nicorandil has no protective effect on myocardial injury.22 For example, Miyoshi et al25 found that intravenous use of nicorandil did not reduce the incidence of perioperative myocardial injury. In contrast, Isono et al26 noted that nicorandil significantly reduced the incidence of perioperative myocardial injury and improved left ventricular wall motion. Interestingly, our previous meta-analysis indicated that nicorandil reduced PMI and reduced the incidence of adverse reactions in Chinese patients following elective PCI, but this phenomenon was not obvious for non-Chinese patients.16 Therefore, we performed the PENMIPCI (Protective Effects of Nicorandil on Myocardial Injury after Percutaneous Coronary Intervention) trial to evaluate the efficacy and safety of nicorandil on PMI in patients undergoing elective PCI.
Methods
The data, analytic methods, and study materials will not be made immediately available to other researchers for the purposes of reproducing the results or replicating the procedure. Requests for these materials can be sent to the corresponding author (LL), and if the applicant is approved as qualified for access to the data, we will provide the data as well as information regarding the analytic methods and study materials.
Study design
The PENMIPCI trial is a single-center, randomized, open-label trial conducted at the First Affiliated Hospital of Guangxi Medical University, Nanning, Guangxi, China. The detailed design of the study has been described at http://www.chictr.org.cn/. The flow chart for this study is shown in Figure 1. In summary, a total of 164 patients who underwent elective PCI were included in this study. Ultimately, 146 patients who underwent elective PCI were randomly assigned to two groups after providing informed consent: the control group (who received aspirin 100 mg daily + clopidogrel 75 mg daily) and the nicorandil group (who received aspirin 100 mg daily + clopidogrel 75 mg daily + nicorandil 5 mg, three times a day). The use of nicorandil was as follows: 5 mg of nicorandil was taken orally for 3 days before PCI and 7 days after PCI. All patients were given beta-blockers, angiotensin-converting enzyme inhibitors, or angiotensin II receptor blockers and statins according to the current guidelines. Data analysis was carried out independently by the researchers. The corresponding authors (Lang Li and Qiang Su) had the right to access all study data and bore the ultimate responsibility for the decision to submit the data for publication. This study was approved by the ethical committee of the First Affiliated Hospital of Guangxi Medical University (approval number: 2017 (KY-E-026; http://www.chictr.org.cn/). All participants were informed of the study and provided written informed consent. In addition, this study was conducted in accordance with the tenets of the Declaration of Helsinki.
  | Figure 1 Study flow chart. |
Study patients
The inclusion criteria were as follows: patients with CHD scheduled for elective PCI at the First Affiliated Hospital of Guangxi Medical University; aged 18 to 75 years old; male or non-pregnant females; coronary blood flow of more than TIMI2 (thrombolysis in myocardial infarction, TIMI) after PCI; and no potassium channel openers within 1 month before enrollment. The exclusion criteria were as follows: acute coronary syndrome (including unstable angina, ST-segment elevation myocardial infarction and non-ST-segment elevation myocardial infarction); severe cardiac insufficiency (New York Heart Association [NYHA] ≥ III class or left ventricular ejection fraction [LVEF] less than 40% as measured by echocardiography); severe liver and renal insufficiency (estimated glomerular filtration rate ≤30%); bleeding tendency; gastrointestinal bleeding; history of a malignant tumor, such as lung cancer, primary liver cancer and digestive tract malignant tumors; allergy to antiplatelet drugs or anticoagulant drugs; scheduled coronary artery bypass grafting treatment; severe valvular heart diseases; autoimmune diseases; and potassium channel medication use within 1 month of enrollment. Other detailed descriptions can be found at http://www.chictr.org.cn/.
Randomization
Patients who met the inclusion criteria and exclusion criteria mentioned above were randomly assigned in a 1:1 fashion to the control group and nicorandil group using a random number table. This process was entirely conducted by the researchers, and no pharmacist or pharmaceutical company were involved in this process.
Study endpoints and follow-up
The primary outcomes were the change in cardiac troponin T (cTnT) and creatine kinase-MB (CK-MB) at 12 and 24 hours after surgery. The secondary outcome was the incident of major adverse cardiac events (MACE) 30 days after the operation, which was a composite of cardiac death, nonfatal myocardial infarction, new heart failure or coronary revascularization. The serious adverse events mentioned above were checked and confirmed by two cardiovascular specialists according to the guidelines that were formulated. All patients were followed-up by telephone at 30 days after the operation.
Covariant variables
We used the electronic medical records of the First Affiliated Hospital of Guangxi Medical University to collect the demographic characteristics, comorbidities and cardiac medications of all patients. The patient information included age, sex, diabetes, hypertension, dyslipidemia, smoking status, weight, height, body mass index (BMI), estimated glomerular filtration rate (eGFR), glutamic-oxaloacetic transaminase, alanine aminotransferase, low-density lipoprotein, high-density lipoprotein, total cholesterol, triglycerides, uric acid, fasting blood glucose, hemoglobin A1C, brain natriuretic peptide, left ventricular end diastolic diameter (LVDD) and LVEF. The variables mentioned above were measured within 24 hours after admission. Echocardiography was usually performed within 24 hours after admission by two echocardiography experts.
Treatment and procedure
The drugs used before and after PCI were given in accordance with the accepted guidelines and practice standards. The PCI procedure and perioperative anticoagulant therapy were carried out in accordance with the accepted guidelines.
Statistical analysis
The hypothesis of this study is that nicorandil can reduce the incidence of PMI in patients undergoing ePCI compared with the control group. In our preliminary experiment, the incidence of PMI in the control group was 43.6%, while the incidence of PMI in the nicorandil group was 27.4%. With a two-sided alpha level of 5% and beta error of 20%, each group needed to recruit 66 participants. In addition, supposing that 10% of the participants in each group would be lost or withdraw from the study, each group ultimately needed to include 73 participants.
In this study, the analysis was based on intention-to-treat principles, and all patients involved in the study were included in the final analysis. The results are presented as the mean ± standard deviation or number + percent. Categorical variables were compared using the chi-squared test. We compared the mean values of continuous variables between the two groups by unpaired Student’s t-test. Differences in the mean values of cTnT and CK-MB between baseline and 12 and 24 hours after operation were compared using repeated-measures analysis of variance.
The incidence of MACE events between the two groups was compared by multivariate logistic regression analyses with hazard ratios (HRs) and 95% confidence intervals (CIs). In addition, the Kaplan–Meier curve method and log-rank test were used in this study to compare the survival time of the two groups. We used the Cox proportional hazards model to estimate HRs between the two groups while adjusting for potential confounding factors, including age, sex, diabetes, hypertension, dyslipidemia, smoking status, weight, height, BMI, eGFR, glutamic-oxaloacetic transaminase, alanine aminotransferase, low-density lipoprotein, high-density lipoprotein, total cholesterol, triglycerides, uric acid, fasting blood glucose, hemoglobin A1C, brain natriuretic peptide, LVDD and LVEF.
Furthermore, we also carried out a subgroup analysis. All patients were stratified into six groups according to age (age >65 years or age <65 years), sex (female or male), diabetes (yes or no), hypertension (yes or no), dyslipidemia (yes or no) and smoking status (yes or no). All reported probability values were two-sided with a P-value <0.05 considered to be statistically significant. Data analysis was performed using IBM SPSS Statistics for Windows, version 22.0 (IBM Corporation, Armonk, NY, USA), R statistical software version 3.3.2 (available at: www.r-project.org) and SAS software (SAS Institute Inc., Cary, NC, USA), version 9.2.
Results
Study flow chart
From October 2017 through April 2018, 164 patients were recruited in the present study; 82 patients were assigned to the nicorandil group and 82 patients were assigned to the control group. During this study, four patients declined to participate, three patients discontinued the study, and one patient was lost to follow-up in the nicorandil group; five patients declined to participate, four patients discontinued the study, and one patient was lost to follow-up in the control group. Ultimately, 74 patients were included in the full analysis set in the nicorandil group and 72 patients were included in the full analysis set in the control group. The flowchart is shown in Figure 1.
Baseline characteristics of study participants
There was no significant difference in the baseline characteristics between the two groups (Table 1). The average age of the control group was 56.35±5.22 years, while the average age of the nicorandil group was 54.76±5.93 years (P=0.088). Females accounted for 25% of the control group and 24.32% of the nicorandil group (P=0.925). Additionally, no significant differences were observed between the two groups in terms of drug application and criminal vessel (Table 1).
Primary outcome
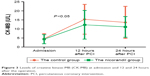
The primary outcomes of this study were the changes in cTnT and CK-MB at 12 and 24 hours after surgery. There was no significant difference in cTnT (0.032±0.018 for the control group and 0.030±0.022 for the nicorandil group, P=0.549) or CK-MB (4.64±2.78 for the control group and 4.35±2.48 for the nicorandil group, P=0.501) between the two groups at admission (Table 2). The levels of cTnT in the nicorandil group decreased significantly compared with those of the control group at both 12 hours (0.12±0.10 vs 0.15±0.12, P=0.012) and 24 hours (0.13±0.10 vs 0.17±0.12, P=0.030) after surgery (Table 2 and Figure 2). Similarly, the levels of CK-MB in the nicorandil group also decreased significantly compared with those of the control group at both 12 hours (12.31±7.93 vs 15.35±8.23, P=0.024) and 24 hours (11.13±5.71 vs 13.63±8.87, P=0.022) after surgery (Table 2 and Figure 3).
  | Table 2 The levels of cardiac troponin T and creatine kinase-MB (CK-MB) at admission, 12 hours and 24 hours after operation |
  | Figure 2 Levels of cardiac troponin T (cTnT) at admission and 12 hours and 24 hours after the operation. |
  | Figure 3 Levels of creatine kinase-MB (CK-MB) at admission and 12 and 24 hours after the operation. |
Secondary outcome
During a mean follow-up of 24.12±3.00 days, nine patients (9/72, 12.50%) had MACE events in the control group and nine patients (9/74, 12.16%) had MACE events in the nicorandil group. A Cox proportional hazards model showed that no significant difference was observed in MACE events between the two groups (HR =0.99, 95% CI: 0.39–2.55, P=0.98) (Figure 4).
Subgroup analyses of the secondary outcome among the two groups
In subgroup analyses, we found that nicorandil did not increase the incidence of MACE events, regardless of age (age >65 years: HR: –0.49, 95% CI: –2.21 to 1.17; age <65 years; HR: 0.03, 95% CI: –1.12 to 1.28), sex (female: HR: 0.11, 95% CI: –2.04 to 1.03; male: HR: −0.04, 95% CI: −1.17 to 1.08), diabetes (with diabetes; HR: −0.17, 95% CI: −1.43 to 1.07; without diabetes; HR: 0.09, 95% CI: −1.56 to 1.76), hypertension (with hypertension: HR: −0.58, 95% CI: −1.71 to 0.57; without hypertension: HR: −0.14, 95% CI: −0.62 to 0.49), dyslipidemia (with dyslipidemia: HR: 0.15, 95% CI: −1.11 to 1.39; without dyslipidemia: HR: −0.29, 95% CI: −1.97 to 1.43) and smoking status (current smoker: HR: −0.14, 95% CI: −1.27 to 1.03; non-smoker: HR: 0.11, 95% CI: −1.90 to 2.14) (Figure 5).
  | Figure 5 Incidence of MACE events between the control group and nicorandil group in subgroup analyses. |
Discussion
Main findings
In this single-center, randomized, open-label trial, we found that nicorandil significantly reduced the incidence of PMI, mainly the levels of cTnT and CK-MB at 12 and 24 hours after ePCI surgery. In addition, our results also indicated that nicorandil did not increase the incidence of MACE (a composite of cardiac death, nonfatal myocardial infarction, new heart failure or coronary revascularization) within 30 days (12.16% in the nicorandil group and 12.50% in the control group). Furthermore, this result remained consistent in subgroup analysis. Our findings support the hypothesis that nicorandil can reduce PMI in patients undergoing ePCI and does not increase the incidence of MACE.
Comparison with previous studies
Previously, a large number of studies have reported the relationship between nicorandil and PMI in patients undergoing ePCI. However, there is controversy regarding this conclusion. Some scholars support the hypothesis that nicorandil can reduce the incidence of myocardial injury, while the results of other scholars do not support this conclusion. For instance, Hwang et al23 carried out a clinical study including 41 patients in the nicorandil group and 40 patients in the control group and found that nicorandil did not reduce the incidence of PMI in patients with stable or unstable angina. In addition, another study observed the clinical effect of intravenous nicorandil in preventing perioperative myocardial injury in the Japanese population. The results also support the hypothesis that nicorandil can prevent perioperative myocardial injury.27 Similarly, another subgroup analysis conducted in diabetic patients demonstrated that nicorandil reduced perioperative myocardial injury in patients undergoing ePCI.24 Interestingly, the findings also suggested that nicorandil improved left ventricular ejection fraction after 6 months (63.5%±7.7% vs 56.5%±8.3%). By contrast, some scholars hold the opposite opinion. A study conducted in South Korea found that an intracoronary injection of nicorandil did not reduce the levels of CK-MB and troponin I, regardless of whether patients had stable or unstable angina. Interestingly, another study conducted in the same country (Republic of Korea) found the opposite result.22 Since the issue of whether nicorandil can prevent perioperative myocardial injury is controversial, we previously conducted a systematic review and meta-analysis;16 16 studies were included in our meta-analysis. Surprisingly, our findings showed that nicorandil was effective for the Chinese population, but not for the non-Chinese population.
In general, it remains controversial as to whether nicorandil can prevent perioperative myocardial injury in patients undergoing ePCI. Therefore, we performed this randomized controlled trial to explore the preventive effect of nicorandil on myocardial injury. The PENMIPCI trial is a single-center, randomized, open-label trial conducted in Guangxi, China. The result of the PENMIPCI trial found that the cTnT and CK-MB levels at 12 and 24 hours were significantly decreased in the nicorandil group compared with those of the control group (Table 2) following ePCI surgery. In addition, our results indicated that nicorandil did not increase the incidence of adverse cardiovascular events within 30 days (Figure 3). Similarly, no significant change was found in subgroup analyses (Figure 4).
The results of the PENMIPCI trial are partly contradictory to previous studies, and the possible explanations are as follows. First, there is a great variety in the drug delivery methods used for nicorandil. Some studies have used intracoronary injections of nicorandil,22,25 while others have been carried out using oral administration.28 The different administration methods of nicorandil may lead to different results. Second, the difference in dosage is a possible reason leading to the different results. In some studies, the dosage of nicorandil was 4 mg once daily,21,23 while in other studies, the dosage of nicorandil was 20 mg once daily.24 Third, there are also significant differences in the follow-up period over which major adverse cardiovascular events were observed. The observation time for some studies was 1 month, 6 months, or even 1 year. Fourth, some previous studies did not describe the grouping method in detail, which is one of the reasons leading to a mixed bias. In the PENMIPCI trial, all patients were randomly assigned to the control group and nicorandil group according to the random number table method. Fifth, differences in the research populations may be an important reason leading to inconsistent results, and this hypothesis can be confirmed by our previous meta-analysis. As is known, the adaptability and metabolic rate of drugs vary among different populations.
Strength and weakness
Our study has several strengths. First, the analysis of the PENMIPCI trial was based on intention-to-treat principles, which is notably different from previous studies. In clinical practice, patients have the right to choose suitable treatment methods, and intention-to-treat analysis is more in line with the real world. In this case, we can minimize the confounding bias and reach a conclusion that is more consistent with the real world. Second, as a randomized controlled trial, the baseline information of the PENMIPCI trial was well balanced, with no significant differences between the groups. Under these circumstances, we were able to control the confounding factors to the minimum, thus increasing the reliability of the results. Third, subgroup analyses were also performed in the PENMIPCI trial according to age (age >65 years or age <65 years), sex, diabetes, hypertension, dyslipidemia and smoking status. The results of the subgroup analyses did not change our conclusions, thus indicating the robustness of the PENMIPCI trial.
Our study also has several limitations. First, as a single-center study, whether the results of the PENMIPCI trial can be applied to other regions or countries still needs to be confirmed in further research. Second, nicorandil was administered orally in the PENMIPCI trial. Thus, it should be noted that the results of this study only indicate that oral nicorandil can significantly reduce the incidence of myocardial injury during the perioperative period and cannot represent the effect of intracoronary nicorandil. It is possible that the route of administration of nicorandil might affect the research results.
Conclusion
Our results suggest that nicorandil can reduce PMI in patients undergoing ePCI without increasing the incidence of MACE. The results are consistent in the subgroup analyses. Considering the difference in dosage and route of administration, this result still requires further confirmation.
Acknowledgments
This study was supported by grants from the National Natural Science Foundation of China (grant number 81600283) and the Guangxi Natural Science Foundation (grant number 2016GXNSFBA380022).
Disclosure
The authors report no conflicts of interest in this work.
References
Fuenmayor A, Granell R, Tortosa MA Ángeles. Caring for older people: an analysis of the small business sector. The Service Industries Journal. 2012;32(15):2347–2363. | ||
Lam NN, Kim SJ, Knoll GA, et al. The risk of cardiovascular disease is not increasing over time despite aging and higher comorbidity burden of kidney transplant recipients. Transplantation. 2016;101(3):588–596. | ||
Gada H, Kirtane AJ, Newman W, et al. 5-year results of a randomized comparison of XIENCE V everolimus-eluting and TAXUS paclitaxel-eluting stents: final results from the SPIRIT III trial (clinical evaluation of the XIENCE V everolimus eluting coronary stent system in the treatment of patients with de novo native coronary artery lesions). JACC Cardiovasc Interv. 2013;6(12):1263–1266. | ||
Meng M, Gao B, Wang X, Bai ZG, Sa RN, Ge B. Long-term clinical outcomes of everolimus-eluting stent versus paclitaxel-eluting stent in patients undergoing percutaneous coronary interventions: a meta-analysis. BMC Cardiovasc Disord. 2016;16:34. | ||
Zhou B, Wu Y, Yang J, Li Y, Zhang H, Zhao L. Overweight is an independent risk factor for cardiovascular disease in Chinese populations. Obes Rev. 2002;3(3):147–156. | ||
He Y, Jiang B, Wang J, et al. BMI versus the metabolic syndrome in relation to cardiovascular risk in elderly Chinese individuals. Diabetes Care. 2007;30(8):2128–2134. | ||
Hou F, Jiang J, Chen J, et al. China collaborative study on dialysis: a multi-centers cohort study on cardiovascular diseases in patients on maintenance dialysis. BMC Nephrol. 2012;13:94. | ||
Marenberg ME, Risch N, Berkman LF, Floderus B, de Faire U. Genetic susceptibility to death from coronary heart disease in a study of twins. N Engl J Med Overseas Ed. 1994;330(15):1041–1046. | ||
Bendinelli B, Masala G, Saieva C, et al. Fruit, vegetables, and olive oil and risk of coronary heart disease in Italian women: the EPICOR Study. Am J Clin Nutr. 2011;93(2):275–283. | ||
Rachas A, Raffaitin C, Barberger-Gateau P, et al. Clinical usefulness of the metabolic syndrome for the risk of coronary heart disease does not exceed the sum of its individual components in older men and women. The Three-City (3C) Study. Heart. 2012;98(8):650–655. | ||
Mensah GA, Moran AE, Roth GA, Narula J. The global burden of cardiovascular diseases, 1990–2010. Glob Heart. 2014;9(1):183–184. | ||
Roth GA, Johnson C, Abajobir A, et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. 2017;70(1):1–25. | ||
Smith SC Jr, Chen D, Collins A, et al. Moving from political declaration to action on reducing the global burden of cardiovascular diseases: a statement from the global cardiovascular disease taskforce. Circulation. 2013;128:2546–2548. Erratum: e450. | ||
Fortuna D, Nicolini F, Guastaroba P, et al. Coronary artery bypass grafting vs percutaneous coronary intervention in a ‘real-world’ setting: a comparative effectiveness study based on propensity score-matched cohorts. Eur J Cardio-Thoracic Surg. 2013;44(1):e16–e24. | ||
Cuculi F, Lim CC, Banning AP. Periprocedural myocardial injury during elective percutaneous coronary intervention: is it important and how can it be prevented? Heart. 2010;96(10):736–740. | ||
Ye Z, Su Q, Li L. The clinical effect of nicorandil on perioperative myocardial protection in patients undergoing elective PCI: A systematic review and meta-analysis. Sci Rep. 2017;7:45117. | ||
Nagele P, Liggett SB. Genetic variation, β-blockers, and perioperative myocardial infarction. Anesthesiology. 2011;115(6):1316–1327. | ||
Kim SE, Park DG, Lee JH, Han KR, Oh DJ. Utility of B-type natriuretic peptide for predicting perioperative cardiovascular events in patients without history of cardiovascular disease undergoing major non-cardiac surgery. Korean Circ J. 2011;41(1):11–15. | ||
Cuthbertson BH, McKeown A, Croal BL, Mutch WJ, Hillis GS. Utility of B-type natriuretic peptide in predicting the level of peri- and postoperative cardiovascular support required after coronary artery bypass grafting. Crit Care Med. 2005;33(2):437–442. | ||
Horinaka S. Use of nicorandil in cardiovascular disease and its optimization. Drugs. 2011;71(9):1105–1119. | ||
Kim JH, Jeong MH, Yun KH, et al. Myocardial protective effects of nicorandil during percutaneous coronary intervention in patients with unstable angina. Circ J. 2005;69(3):306–310. | ||
Kim SJ, Kim W, Woo JS, et al. Effect of myocardial protection of intracoronary adenosine and nicorandil injection in patients undergoing non-urgent percutaneous coronary intervention: a randomized controlled trial. Int J Cardiol. 2012;158(1):88–92. | ||
Hwang J, Lee HC, Kim BW, et al. Effect on periprocedural myocardial infarction of intra-coronary nicorandil prior to percutaneous coronary intervention in stable and unstable angina. J Cardiol. 2013;62(2):77–81. | ||
Shehata M. Cardioprotective effects of oral nicorandil use in diabetic patients undergoing elective percutaneous coronary intervention. J Interven Cardiol. 2014;27:472–481. | ||
Miyoshi T, Ejiri K, Kohno K, et al. Effect of remote ischemia or nicorandil on myocardial injury following percutaneous coronary intervention in patients with stable coronary artery disease: A randomized controlled trial. Int J Cardiol. 2017;236:36–42. | ||
Isono T, Kamihata H, Sutani Y, et al. Nicorandil suppressed myocardial injury after percutaneous coronary intervention. Int J Cardiol. 2008;123(2):123–128. | ||
Murakami M, Iwasaki K, Kusachi S, et al. Nicorandil reduces the incidence of minor cardiac marker elevation after coronary stenting. Int J Cardiol. 2006;107(1):48–53. | ||
Pei WN, Xie RQ, Cui W, et al. Cardiology DO: comparative study for trimetazidine and nicorandil in patients with PCI related myocardial injure. Chinese Circulation J. 2014;29:256–260. Chinese. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


