Back to Journals » Clinical Interventions in Aging » Volume 11
Effect of pedometer use and goal setting on walking and functional status in overweight adults with multimorbidity: a crossover clinical trial
Authors Takahashi P, Quigg S, Croghan I, Schroeder D, Ebbert J
Received 2 March 2016
Accepted for publication 28 April 2016
Published 1 September 2016 Volume 2016:11 Pages 1099—1106
DOI https://doi.org/10.2147/CIA.S107626
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Walker
Paul Y Takahashi,1 Stephanie M Quigg,1 Ivana T Croghan,1 Darrell R Schroeder,2 Jon O Ebbert1
1Division of Primary Care Internal Medicine, 2Division of Biomedical Statistics and Informatics, Mayo Clinic, Rochester, MN, USA
Background: Walking can improve functional status, and a pedometer and goal setting can increase walking and, potentially, gait speed. The efficacy of pedometer use and goal setting for increasing step counts among overweight and obese adults with multiple comorbid conditions has not been evaluated.
Methods: We recruited and randomly assigned obese or overweight adults with multimorbidity to immediate pedometer use with goal setting or delayed pedometer use, using a crossover design. The primary outcome of interest was step count, with secondary outcomes of gait speed and grip strength, with comparison between the intervention and delayed pedometer groups.
Results: Mean (standard deviation [SD]) age of the 130 participants was 63.4 (15.0) years. At 2 months, mean (SD) steps for the immediate pedometer use group (n=64) was 5,337 (3,096), compared with 4,446 (2,422) steps in the delayed pedometer group (n=66) (P=0.08). Within-group step count increased nonsignificantly, by 179 steps in the immediate pedometer group and 212 steps in the delayed pedometer group after 2 months of intervention, with no significant difference between the groups. Gait speed significantly increased by 0.08 m/s (P<0.05) and grip strength significantly increased by 1.6 kg (P<0.05) in the immediate pedometer group.
Conclusion: Pedometer use and goal setting did not significantly increase step count among overweight and obese adults with multimorbidity. The absolute step count was lower than many reported averages. Gait speed and grip strength increased with immediate pedometer use. The use of pedometers and goal setting may have an attenuated response in this population.
Clinical Trials number: NCT01833507.
Keywords: chronic disease, muscle strength, obesity, physical activity, pedometer, gait speed, grip strength
Introduction
Walking is important for all people, but is particularly important for older adults. Understanding the importance of gait speed, walking, and exercise in general, primary care providers routinely encourage increased physical activity. One such method to increase activity involves the use of a pedometer. Pedometers provide step count for the day and may record these steps for a week. Pedometers provide feedback that uses theoretical modeling of social cognitive theory. Patients set goals by trying to reach a target for steps and improve self-efficacy by setting and reaching daily goals. In some workplace studies, 70% of people will increase their activity with a 4-week pedometer program.1 In a 2007 meta-analysis of 27 studies – both randomized controlled trials and observational studies – participants in clinical trials increased their physical activity by 2,183 steps compared with a control group.2 Other meta-analyses have evaluated step count in patients with specific illnesses. An analysis of seven randomized trials in patients with musculoskeletal disorders showed an average increase in step count of 1,950 steps.3 In a recent Cochrane analysis of workplace pedometer use in 1,809 employees, only one of four studies showed increased pedometer steps and two studies showed no difference.4 In younger populations, the use of pedometer may provide health benefits.2,5
Both the speed of walking and the absolute number of steps are important. Gait speed is an established biological marker for frailty and a potential predictor of mortality.6 Gait speed is calculated using traveled distance in meters by the time required to travel that distance in seconds (m/s). Consensus statements and systematic reviews have outlined the deleterious effects of low gait speed. The International Academy on Nutrition and Aging concluded that low gait speed was a risk factor for disability, falls, institutionalization, and mortality.7 A timed gait speed slower than 1.0 m/s is considered to indicate deficient muscle functional strength.8 Gait speed in people older than 70 years averages 0.74 m/s (95% confidence interval 0.65–0.83 m/s) in the outpatient clinic9 and 0.475 m/s in nursing homes.10 On average, most adults older than 70 years have a gait speed that places them at risk for adverse outcomes.
An increasing proportion of our patient population is overweight or obese and has multimorbidity. These patients are at increased risk for hospitalization and adverse health events.11 No data exist on whether a pedometer coupled with a goal-setting program will improve step count or gait speed in this population. Obesity or multimorbidity may influence step count. In this study, we aimed to determine the effect of pedometer use and behavioral goal setting, compared with usual care, on walking steps, gait speed, and grip strength in overweight and obese adults with multimorbidity.
Methods
Trial setting and design
The study was approved by the Mayo Clinic Institutional Review Board. We conducted a randomized controlled trial with a crossover design at Mayo Clinic, Rochester, MN, USA. The study participants and staff were not masked to assignment because the intervention group wore the pedometer and the usual care group did not. Randomization was completed with a computerized randomization scheme with blocks of four and given to patients in sealed envelopes. There were no changes to the design or execution of the trial after initiation. Study enrollment occurred from May 1, 2013, through September 10, 2014.
Participants were assigned to pedometer and behavioral goal setting or usual care in a 1:1 ratio. All participants had a baseline visit. Those in the immediate pedometer group then had three intervention visits at Months 1, 2, and 3 and a follow-up visit at Month 4; those in the delayed pedometer group had a follow-up visit at Month 1, with the intervention in Months 2 and 3, and a final follow-up at Month 4. Continuing the intervention in the immediate pedometer group allowed for a longer within-group comparison.
Participants
Patients were eligible for enrollment if they were at least 18 years old, community dwelling, overweight or obese, and had multiple medical comorbid conditions. Overweight was defined as a body mass index (BMI) between 25 and 29.9 kg/m2 and obese as a BMI of ≥30.0 kg/m2. Potential participants were screened for BMI using the electronic medical record, sampling the previous 12 months of clinical data.
We used Minnesota medical tiering as the basis for determining medical complexity. Minnesota medical tiering is based on the Ambulatory Care Group risk stratification method, which counts both number and severity of illnesses.12 Trained medical staff not involved with the study calculated Minnesota tiering scores for the medical practice based on medical record billing codes. The International Classification of Diseases-9 codes for the previous year were used and were counted and placed into expanded disease clusters. These clusters were further categorized into 22 major expanded disease clusters, which were then counted, for each patient to be placed into medical tiers. Tiering placed patients into five categories: 0, low (0 medical conditions); 1, basic (one to three conditions); 2, intermediate (four to six conditions); 3, extended (seven to nine conditions); and 4, complex (ten or more conditions). Patients with extended and complex tiering (seven or more conditions or Tiers 3 or 4) were eligible for this study.
Participants were excluded if they were in Tier 2 or lower, had clinically documented dementia, were wheelchair bound, had uncontrolled depression (Patient Health Questionnaire-9 score >10),13 or were in hospice. They were also excluded if they lived in a skilled nursing facility or were in a correctional facility. Patients who refused medical record review were also excluded.14
Study enrollment
Identification numbers for potentially eligible patients were placed in random order, and letters were sent to potential participants. Before distribution of the letters, tiering scores within the week were checked to ensure continued eligibility. Participants telephoned a study coordinator who used an institutional review board-approved script to discuss the study. Participants met in person with the study coordinator to obtain informed consent and conduct screening procedures.
Age, sex, and race information were obtained at baseline. The study coordinator measured weight (kg), height (cm), blood pressure (mmHg), and pulse rate at baseline and at follow-up visits. The study coordinator measured cognitive status using the Short Test of Mental Status,15,16 which is scored on a 38-point scale, with 29 points or less considered as possible dementia. The reported sensitivity ranges from 86% to 92% and specificity from 91% to 93%. The study coordinator administered the Patient Health Questionnaire-9;13 the nine questions are based on the standard criteria for depression and have rankings from 0 to 3, for a total possible score of 27. A score of ≥10 has a sensitivity and specificity for depression of 88%.13 All data were collected and managed using REDCap electronic data capture tools at Mayo Clinic.17
Intervention
The intervention emphasized exercise through pedometer use, as well as SMART (Specific, Meaningful, Action-based, Realistic, and Timely) goal setting.18 SMART goals follow a transtheoretical model of change in which participants are in contemplation stages of change.19 This method of goal setting has the participant set realistic goals that are obtainable and helpful at each stage. Participants in the immediate pedometer group received the pedometer, a digital versatile disc on exercise, exercise literature, nutrition literature, and a journal for activity self-entry. The pedometer was an Omron HJ-112 (Omron Healthcare, Inc, Lake Forest, IL, USA), with 7-day recording capability. Omron pedometers have been validated as accurate measures of step count.20–25 Patients were instructed to wear the pedometer whenever they were up and walking. The participants set their own step goal, which was based on their baseline steps and the SMART goals they set. The pedometer served as the measure of adherence to the walking program.
Each intervention visit (baseline, 1-, 2-, and 3-month) involved brief behavioral goal setting to encourage and outline an increase in walking steps or healthy lifestyle. The initial visit averaged 90 minutes in length, and the follow-up visits were 30 minutes long. The digital versatile disc encouraged patients to start an exercise program in a 43-minute overview, including sample exercises. The exercise booklet emphasized SMART goals and included strengthening and stretching exercises. The nutritional material emphasized the food pyramid and reducing cholesterol and salt intake. The daily journal had a section to record exercise and a food log. The front of the booklet had a section on SMART goals, with a space for the participant to write down their goals. The study coordinator helped participants set goals, with physical activity and nutritional goal setting, as directed by the patient.
Delayed pedometer group
Participants enrolled in the delayed pedometer group received entrance screening tests with no goal setting or pedometer use. Participants had full access to the video, journal, and education materials; however, this was not given to them at the baseline visit. Participants were given entry into the intervention at the 2-month visit and received the pedometer, educational materials, and behavioral goal setting at that point.
Outcomes
Walking steps were the primary outcome of interest, with comparison between the immediate pedometer group and the delayed pedometer group. Walking steps and functional status were obtained at baseline and at follow-up visits. For baseline steps, the study coordinator called the patient after 1 week to obtain an average number of steps for the initial week using the pedometer. Steps per day were averaged over the first 7 days of intervention and the 7 days before visits at 1, 2, 3, and 4 months.
Grip strength was measured using a Baseline (Medline Industries, Inc, Mundelein, IL, USA) hydraulic hand dynamometer and recorded in kilograms. The study coordinator had the participant tightly squeeze the dynamometer in the dominant hand with an outstretched arm. The study coordinator measured gait speed using a stopwatch, instructing the participant to walk at a normal speed over 4 m, which was measured in seconds and reported as m/s. The 4-m test is used as a standard gait measure.26 To assess safety, we recorded the total number of adverse events (AEs), defined as any concerns from the participant (such as unplanned doctor visits or injury), and serious AEs (SAEs), defined as death, life-threatening events, hospitalization, and emergency room visits. AEs and SAEs were adjudicated for relationship to the study intervention.27
Data analysis
To compare groups at baseline, we used the χ2 test for dichotomous characteristics and t-tests for continuous variables. For the primary outcome of walking steps, we used matched t-tests to compare the differences between baseline and 2- and 4-month visits for within-group comparisons in both the immediate pedometer and delayed pedometer groups. We also compared between the immediate pedometer and delayed pedometer groups for walking steps at 2 months using a t-test. On the basis of step counts, we categorized patients as sedentary (<5,000 steps) or nonsedentary (≥5,000 steps) based on previously published categories for step count for the overall population.28 For the secondary outcomes of gait speed and grip strength, both outcomes were compared within assigned group at baseline, 2 months, and 4 months and between groups at 1 and 2 months.
We analyzed the data using an intention-to-treat analysis. For patients with incomplete or missing step information, we used the average daily steps from the available data or last observation carried forward. For patients with other types of missing data, we carried forward the last available information using the last observation carried forward method of imputing the data. We performed analysis of covariance for between-group (immediate pedometer vs delayed pedometer group) evaluation. Significance was determined using a two-tailed test, with P<0.05 being considered significant. All analyses were conducted using SAS software version 9.3 (SAS Institute Inc., Cary, NC, USA).
The study power calculation was based on 100 participants to be randomly assigned into the immediate pedometer group (n=50) and delayed pedometer group (n=50). The power calculations were based on the primary outcome of walking steps. The basis for sample size calculations was 7,500 steps on average, with an expected change of 26%. These baseline assumptions were derived from a meta-analysis of clinical trials and observational studies using pedometers.2 Using these assumptions, we had an 80% power to detect a 30% difference with 90 participants. We did not perform an interim analysis.
Results
Participants
In this study, 130 participants were enrolled, provided consent, and were randomly assigned: 64 participants to the immediate pedometer group and 66 to the delayed pedometer group (Figure 1). The first patient was enrolled on May 1, 2013, and the study finished on January 9, 2015. The mean (standard deviation [SD]) age for the cohort overall was 63.4 (15.0) years; 72% were women, and 98% were white. Participant characteristics were similar between groups at baseline (Table 1).
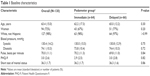  | Table 1 Baseline characteristics |
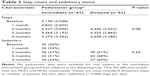
Step count
The mean (SD) number of baseline steps was 5,158 (3,048) steps in the immediate pedometer group. At 2 months, the number was 5,337 (3,096) steps in the immediate pedometer group and 4,446 steps (2,422) in the delayed pedometer group (P=0.08). After 2 months of pedometer use and behavioral goal setting, step count increased nonsignificantly in the immediate pedometer group by 179 steps from baseline. In the delayed pedometer group, the step count also increased nonsignificantly (212 steps) from Months 2 to 4. The proportion of sedentary adults in the immediate pedometer group was 56% at baseline and 57% at 2 months, compared with 61% at baseline vs 60% at 2 months in the delayed pedometer group (Table 2).
Gait speed and grip strength
The mean measured time to walk 4 m at baseline in the immediate pedometer group was 4.31 seconds; meter time was significantly lower (faster gait speed) than baseline at Months 1, 2, and 4 (paired t-test: P=0.02, P=0.02, and P=0.002, respectively) (Table 3). Calculated gait speed was 0.93 m/s vs 1.02 m/s after 4 months (P=0.002). For the delayed pedometer group, meter time was significantly lower than baseline at all follow-up months (all P<0.001). The delayed pedometer group also showed improvement in gait speed from baseline to 4 months (P<0.001). For the immediate pedometer group, grip strength was significantly greater than baseline at Months 2, 3, and 4 (P=0.02, P=0.04, and P=0.01, respectively). Grip strength did not change from baseline at any follow-up in the delayed pedometer group (Table 3).
Safety
Participants in the immediate pedometer group reported 51 AEs and 22 SAEs: 11 hospitalizations and 11 emergency department visits. None of the SAEs were adjudicated as being study related. In the delayed pedometer group, 56 AEs and 26 SAEs (22 emergency department visits and 4 hospitalizations) were reported. None of the SAEs were adjudicated as being study related.
Discussion
In this randomized trial of obese, multimorbid adults, the use of a pedometer with goal setting did not increase step counts at 2 months in the immediate pedometer group compared with the delayed pedometer group. Comparing change from before to after intervention, participants had an increased number of steps, but the change was nonsignificant. There was no change in sedentary status in either the immediate pedometer or delayed pedometer group after starting the pedometer and goal-setting program. Our study reflected an effectiveness intervention with a pedometer and available patient education with monthly follow-up.
Our findings contrast with those in the available literature. Several studies have confirmed the utility of pedometers for increasing step count in different populations. In a study from Qatar, 970 adults used a pedometer and online goal setting, with 45% of participants reaching 10,000 steps, compared with 19% at baseline.29 In 102 older adults with obstructive lung disease, patients randomly assigned to use a pedometer had an increase of 3,080 steps, compared with a 140-step increase in the usual care group (P<0.001).30 A study from Hong Kong of 205 older adults who used a pedometer for 10 weeks found an increase in mean step count from 6,591 to 8,934.31 In a systematic review of seven articles with 484 total participants with musculoskeletal problems, the use of a pedometer increased the number of steps by an average of 1,950.3 Finally, a study using intensive counseling and educational intervention and a pedometer in 18 obese women aged >60 years showed an increase of 1,856 steps from baseline to 3 months and a decrease in weight.32 Our findings may differ from these previous studies because of the multimorbidity and obesity in our population, which may affect mobility. Climate may also have a role in walking steps, with cold weather, ice, and snow potentially changing walking patterns. In survey studies, people who were younger and had a lower BMI had higher step counts.33
We observed an increase in gait speed with the immediate pedometer group from baseline to the 4th month. This is an encouraging finding because gait speed is a primary marker for frailty. Other studies with an emphasis on pedometer use and ensuing gait speed showed some differing findings. In a pilot study of eleven patients after stroke who used a step activity monitor, step count increased by 1,100 steps, but gait speed did not change over the 3-month trial.34 Definition of a clinically meaningful change in gait speed varies; however, in stroke patients, an increase of 0.16 m/s resulted in less disability.35 It is unclear whether the 0.08 m/s increased gait speed in our study population has any clinical relevance.
We observed a small within-group increase in grip strength in the immediate pedometer group compared from baseline to the 2nd, 3rd, and 4th month. The strength increased by approximately 1 kg, although the clinical significance of a 1 kg change has not been determined. It is possible that patients in the immediate pedometer group undertook further activity that increased their grip strength; however, the difference we identified may represent random chance. In patients with wrist fracture, a change of 6.5 kg of grip strength is noticeable by self-report.36 Improvement in grip strength with a pedometer program has not been well documented. In a previous study of 36 ambulatory patients in assisted living, the use of a pedometer increased step count by 670 steps, which was significant; however, the investigators did not find a difference in grip strength.37 Our findings that grip strength improved in addition to gait speed within group is encouraging but not expected given the nonsignificant change in step count. The findings of improved strength and gait speed may reflect a greater emphasis on physical activity that was not reflected by the step count.
Our study has several limitations. The mean number of steps and the effect of the pedometer on improving step count were lower than expected, and the study was underpowered to detect such a small difference. The study was not masked for practical reasons; however, the observation bias should favor increased steps in the immediate pedometer group, which was not seen. Adherence to the intervention (ie, increased activity and wearing the pedometer) was the primary challenge, and measuring adherence was difficult. However, adherence is the primary challenge in clinical practice, and this study attempts to reflect a practical approach that can be used in a clinical setting. A more intensive intervention may have had a greater effect on step count. The completion rates in both the immediate pedometer group and the delayed pedometer group were 80% and 90%, respectively, with slightly more attrition in the immediate pedometer group. We imputed the data using last observation carried forward, which might introduce bias into the analysis. The generalizability of the study may be restricted because our regional population is predominantly white and highly educated,38 and our sample was predominantly white.
Conclusion
We did not observe a significant difference in step count between participants with immediate or delayed use of a pedometer with a goal-setting program. We also did not find within-group changes in step count from before to after starting the program in either group. We did note an increase in gait speed and grip strength, but the clinical utility of these findings will have to be determined. The clinical implications involve the recommendations of pedometer use in this population. Pedometers may have much less or no utility in this group. Different interventions may be required to increase activity and step count in this population. Ultimately, patients will continue to use pedometers in the general community, because it is an inexpensive intervention; however, for this overweight, multimorbid population, the effectiveness of this intervention was not demonstrated by our study. Future work may involve a more intensive pedometer regimen with a potential online goal-setting program and potentially a longer period of intervention. Future work may also focus on identifying the population that most benefits from the intervention.
Acknowledgments
This publication was supported by Grant Number UL1 TR000135 from the National Center for Advancing Translational Sciences (NCATS). Its contents are solely the responsibility of the authors, and do not necessarily represent the official views of the National Institutes of Health. We also acknowledge the Department of Medicine for support.
Disclosure
The authors report no conflicts of interest in this work.
References
Thomas L, Williams M. Promoting physical activity in the workplace: using pedometers to increase daily activity levels. Health Promot J Austr. 2006;17(2):97–102. | ||
Bravata DM, Smith-Spangler C, Sundaram V, et al. Using pedometers to increase physical activity and improve health: a systematic review. JAMA. 2007;298(19):2296–2304. | ||
Mansi S, Milosavljevic S, Baxter GD, Tumilty S, Hendrick P. A systematic review of studies using pedometers as an intervention for musculoskeletal diseases. BMC Musculoskelet Disord. 2014;15:231. | ||
Freak-Poli RL, Cumpston M, Peeters A, Clemes SA. Workplace pedometer interventions for increasing physical activity. Cochrane Database Syst Rev. 2013;4:CD009209. | ||
Lubans DR, Morgan PJ, Tudor-Locke C. A systematic review of studies using pedometers to promote physical activity among youth. Prev Med. 2009;48(4):307–315. | ||
Hardy SE, Perera S, Roumani YF, Chandler JM, Studenski SA. Improvement in usual gait speed predicts better survival in older adults. J Am Geriatr Soc. 2007;55(11):1727–1734. | ||
Abellan van Kan G, Rolland Y, Andrieu S, et al. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J Nutr Health Aging. 2009;13(10):881–889. | ||
Fielding RA, Vellas B, Evans WJ, et al. Sarcopenia: an undiagnosed condition in older adults: current consensus definition: prevalence, etiology, and consequences. International Working Group on Sarcopenia. J Am Med Dir Assoc. 2011;12(4):249–256. | ||
Peel NM, Kuys SS, Klein K. Gait speed as a measure in geriatric assessment in clinical settings: a systematic review. J Gerontol A Biol Sci Med Sci. 2013;68(1):39–46. | ||
Kuys SS, Peel NM, Klein K, Slater A, Hubbard RE. Gait speed in ambulant older people in long term care: a systematic review and meta-analysis. J Am Med Dir Assoc. 2014;15(3):194–200. | ||
Haas LR, Takahashi PY, Shah ND, et al. Risk-stratification methods for identifying patients for care coordination. Am J Manag Care. 2013;19(9):725–732. | ||
Weiner JP, Starfield BH, Steinwachs DM, Mumford LM. Development and application of a population-oriented measure of ambulatory care case-mix. Med Care. 1991;29(5):452–472. | ||
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. | ||
Rocca WA, Yawn BP, St Sauver JL, Grossardt BR, Melton LJ 3rd. History of the Rochester Epidemiology Project: half a century of medical records linkage in a US population. Mayo Clin Proc. 2012;87(12):1202–1213. | ||
Kokmen E, Smith GE, Petersen RC, Tangalos E, Ivnik RC. The short test of mental status: correlations with standardized psychometric testing. Arch Neurol. 1991;48(7):725–728. | ||
Kokmen E, Naessens JM, Offord KP. A short test of mental status: description and preliminary results. Mayo Clin Proc. 1987;62(4):281–288. | ||
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. | ||
Bovend’Eerdt TJ, Botell RE, Wade DT. Writing SMART rehabilitation goals and achieving goal attainment scaling: a practical guide. Clin Rehabil. 2009;23(4):352–361. Erratum in: Clin Rehabil. 2010;24(4):382. | ||
White ND, Lenz TL, Smith K. Tool guide for lifestyle behavior change in a cardiovascular risk reduction program. Psychol Res Behav Manag. 2013;6:55–63. | ||
Barreira TV, Bennett JP, Kang M. Validity of pedometers to measure step counts during dance. J Phys Act Health. 2015;12(10):1430–1435. | ||
Giannakidou DM, Kambas A, Ageloussis N, et al. The validity of two Omron pedometers during treadmill walking is speed dependent. Eur J Appl Physiol. 2012;112(1):49–57. | ||
Steeves JA, Tyo BM, Connolly CP, Gregory DA, Stark NA, Bassett DR. Validity and reliability of the Omron HJ-303 tri-axial accelerometer-based pedometer. J Phys Act Health. 2011;8(7):1014–1020. | ||
Holbrook EA, Barreira TV, Kang M. Validity and reliability of Omron pedometers for prescribed and self-paced walking. Med Sci Sports Exerc. 2009;41(3):670–674. | ||
Schneider PL, Crouter SE, Lukajic O, Bassett DR Jr. Accuracy and reliability of 10 pedometers for measuring steps over a 400-m walk. Med Sci Sports Exerc. 2003;35(10):1779–1784. | ||
Crouter SE, Schneider PL, Karabulut M, Bassett DR Jr. Validity of 10 electronic pedometers for measuring steps, distance, and energy cost. Med Sci Sports Exerc. 2003;35(8):1455–1460. | ||
National Institutes of Health [database on the Internet]. NIH Toolbox 4-meter Walk Gait Speed Test. Bethesda, MD: National Institutes of Health; 2006–2012. Available from: http://www.nihtoolbox.org/WhatAndWhy/Motor/Locomotion/Pages/NIH-Toolbox-4--Meter-Walk-Gait-Speed-Test.aspx. Accessed May 21, 2015. | ||
US Food and Drug Administration [database on the Internet]. What is a Serious Adverse Event? Silver Spring, MD: US Food and Drug Administration; 2014 [January 10]. Available from: http://www.fda.gov/Safety/MedWatch/HowToReport/ucm053087.htm. Accessed May 21, 2015. | ||
Tudor-Locke C, Hatano Y, Pangrazi RP, Kang M. Revisiting “how many steps are enough?” Med Sci Sports Exerc. 2008;40(7 Suppl):S537–S543. | ||
Al-Kuwari MG, Al-Mohannadi AS, El-Jack II, Almudahka FA. Effect of online pedometer program on physical activity in Qatar. J Sports Med Phys Fitness. 2016;56(3):275–280. | ||
Mendoza L, Horta P, Espinoza J, et al. Pedometers to enhance physical activity in COPD: a randomised controlled trial. Eur Respir J. 2015;45(2):347–354. | ||
Leung AY, Cheung MK, Tse MA, Shum WC, Lancaster BJ, Lam CL. Walking in the high-rise city: a Health Enhancement and Pedometer-determined Ambulatory (HEPA) program in Hong Kong. Clin Interv Aging. 2014;9:1343–1352. | ||
Jensen GL, Roy MA, Buchanan AE, Berg MB. Weight loss intervention for obese older women: improvements in performance and function. Obes Res. 2004;12(11):1814–1820. | ||
Bassett DR Jr, Wyatt HR, Thompson H, Peters JC, Hill JO. Pedometer-measured physical activity and health behaviors in US adults. Med Sci Sports Exerc. 2010;42(10):1819–1825. | ||
Shaughnessy M, Michael KM, Sorkin JD, Macko RF. Steps after stroke: capturing ambulatory recovery. Stroke. 2005;36(6):1305–1307. | ||
Tilson JK, Sullivan KJ, Cen SY, et al; Locomotor Experience Applied Post Stroke (LEAPS) Investigative Team. Meaningful gait speed improvement during the first 60 days poststroke: minimal clinically important difference. Phys Ther. 2010;90(2):196–208. | ||
Kim JK, Park MG, Shin SJ. What is the minimum clinically important difference in grip strength? Clin Orthop Relat Res. 2014;472(8):2536–2541. | ||
Snyder A, Colvin B, Gammack JK. Pedometer use increases daily steps and functional status in older adults. J Am Med Dir Assoc. 2011;12(8):590–594. | ||
St Sauver JL, Grossardt BR, Leibson CL, Yawn BP, Melton LJ 3rd, Rocca WA. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin Proc. 2012;87(2):151–160. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.