Back to Journals » Journal of Blood Medicine » Volume 11
Demographical Pattern of Blood Donors and Pre-Donation Deferral Causes in Dhahran, Saudi Arabia
Authors Elsafi SH
Received 16 March 2020
Accepted for publication 17 June 2020
Published 14 July 2020 Volume 2020:11 Pages 243—249
DOI https://doi.org/10.2147/JBM.S254168
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Martin H Bluth
Salah H Elsafi
Clinical Laboratory Science Department, Prince Sultan Military College of Health Science, Dammam 31448, Kingdom of Saudi Arabia
Correspondence: Salah H Elsafi
Clinical Laboratory Science Department, Prince Sultan Military College of Health Science, P.O. Box 33048, Dammam 31448, Kingdom of Saudi Arabia
Tel +966 13 8405448
Fax + 966 13 8405577
Email [email protected]
Background: Understanding the demographic features of blood donors is important for identifying the donor structure and guiding the recruitment and retention strategies of donors. This study was aimed to determine the demographic characteristics of blood donors, the types of donation drives, and the frequency and reasons for pre-donation deferral in our population.
Methods: This cross-sectional study included data analysis of all prospective blood donors presenting themselves for donation at the Blood Bank of the King Fahad Military Medical Complex, Dhahran, Saudi Arabia between January 2010 and December 2018. Eligibility of blood donation was assessed using a standardized history questionnaire, physical examination, hemoglobin estimation, pulse rate, blood pressure, and temperature. The questionnaire included the demographic features of the donor such as age, gender, and the reason for donation and other specific risk factors that potentially affect the safety of the donor or the recipient. Data analyzed using the analysis of SPSS version 20 (SPSS Inc., Chicago, IL, USA) were used to calculate the unadjusted odds ratios (OR) and the respective 95% confidence interval for the association between the various demographic parameters.
Results: A total of 28,189 potential donations were recorded during the study period; of these, 77.4% were family replacements with females accounting for only 1.8% of all donations. Most of the donors were Saudi nationals (92.1%) of whom donors between 18 and 34 years old constituted 87.9%, while those over 40 years old represented only 7.9% of the donations. Pre-donation temporary deferral occurred in 3300 (11.7%) of all potential donation attempts. The most common causes being the recent intake of medication (24.4%) followed by low hemoglobin (14.8%), low or high blood pressure (14.6%), low or high pulse rate (13.6%), and low weight (11.6%).
Conclusion: A profile of blood donors consisting mainly of young male citizens who mostly donated for family replacement was detected. Deferral rate was found to be average when compared to other countries; the causes being similar to those detected in other developed countries. Simple descriptive statistics has shown no marked difference was noted over the 9 years of the study in neither the profile of blood donors nor the cause for temporary deferral of prospective blood donors.
Keywords: blood donation, donor’s demography, donor deferral
Introduction
Donated blood is crucial for health care in a wide range of medical services to correct losses due to surgery or massive trauma, severe anemia, hematological malignancies, and treating pregnancy-related complications.1 It is the responsibility of the blood collection services to collect blood only from donors who are at low risk for any transfusion transmissible diseases without threatening the donor’s own health.1 Thus, careful assessment of the eligibility of prospective donors is extremely important for ensuring the safety and adequacy of the blood supply and to protect the recipients as well as the donors themselves, without unnecessary deferral of suitable donors.1
Blood donation rates vary greatly between countries depending on the socioeconomic status.2 Whole blood donation rates per 1000 population per year were 32.1, 14.9, 7.8, and 4.6 donations in high-, upper-middle-, lower-, and low-income countries, respectively.2 Blood donors are generally categorized into voluntary, family replacement, remunerated, and autologous donors. The family replacement donors include those who donate for hospitalized family members, friends or associates.2 The safest donors are found among people who donate their blood voluntarily out of altruism and are self-aware of their readiness to donate blood without the slightest risk of harming the recipients.3
Understanding the characteristics and demographic features of blood donors and the types of donations are important to gain an accurate image of the donor structure, thus guiding the recruitment and retention strategies, and provide benchmarks to measure the success of these efforts.4 For example, previous studies found that in certain regions, blood donor populations are mainly of the younger age-groups.5–7 However, in other situations, older age-groups contributed to the bulk of the donations.8–11 The same diversity exists between male and female donors. Although several studies reported men to have a higher donation rate than women,7,12 other findings were reversed.13,14
Donor selection is the process of assessing the appropriateness of a person to donate blood or blood components according to predefined selection standards.1 This process consists of donor registration, pre-donation information, completion of a donor questionnaire, donor interview and pre-donation counselling, donor health and risk assessment, and finally informed consent.1 Most blood transfusion services require that the prospective donors must be at least 18 years old, have a healthy general appearance, and are feeling well on the donation day and be able to perform their routine daily activities.
In general, physical criteria for prospective donors stipulate that they should not weigh less than 50 kg, have a body temperature not exceeding 37.6 C, and their pulse rate should be between 60 and 100 beats per minute with normal blood pressure (systolic 90–180 mmHg, diastolic 50–100 mmHg). Additionally, their minimum hemoglobin level should be 13.5 g/dL and 12.5 g/dL for males and females, respectively.1 Furthermore, through a health history questionnaire, donors are screened for disease risk factors related to their medical history and travel to ensure their own as well as the recipient’s safety.1
Donors can be deferred for a variety of reasons including signs and symptoms of relevant transfusion-transmitted infections, social behaviors that increase their risk of exposure to infectious diseases, travel to certain countries where the risk of exposure to a particular infectious disease is of concern, medical procedures, intake of certain medications, and pregnancy.1 The total deferral rates vary widely among countries, from less than 1% to over 37%, with a median of 12% according to the presence or absence of donor selection criteria and different donor registration practices.2
Blood transfusion in Saudi Arabia is essentially hospital based, with the primary source of blood and blood products being a combination of a growing number of voluntary non-remunerated donations and family replacement donations. Other blood sources include blood donation campaigns, regional blood banks and the Saudi Red Crescent, a humanitarian society that provides emergency medical services in the Kingdom of Saudi Arabia.2
At present, only a few studies have been conducted concerning donor deferrals in the region and these did not include a study of the demography of the donor population. The objectives of this study were to evaluate the demographic characteristics of blood donors collected over a 9-year period in order to understand the effects of changing demographic features on the availability of blood. Better understanding the demography of the blood donor population will allow for an appropriate recruitment and retention policy and will provide baseline data for measuring the success of these efforts. The study also aimed at estimating the rate of blood donor temporary deferrals and identifying their causes with the aim of possibly reducing their numbers.
Materials and Methods
The ethical committee of Prince Sultan Military College of Health Science approved this study. It is a single-center cross-sectional study where information from all prospective donors at the King Fahad Military Medical Complex blood bank from 2010 to 2018 were retrospectively analyzed. Prospective donors who presented for blood donation were received at the reception and registered. The eligibility for blood donation was assessed using a standardized history questionnaire that investigates health, lifestyle, and disease risk factors, followed by physical examination, hemoglobin estimation, pulse rate, blood pressure, and temperature. The questionnaire included the demographic feature of the donor such as age, gender, and the reason for donation. Other information that might have revealed a specific risk such as behavior, travel history, and other factors that potentially affect the safety of the donor or the recipient were also included. The causes of pre-donation temporary deferral of prospective donors were also reported. All donors had signed an informed consent.
Data were analyzed using the analysis Woolpack in Microsoft excel version 2010. Descriptive statistics such as frequencies, percentages, and means were used to measure demographic variables. The SPSS version 20 (SPSS Inc., Chicago, IL, USA) was used to calculate the unadjusted odds ratios (OR) and the respective 95% confidence interval for the association between the various demographic parameters. The 18–25 years age-group was used as the reference group and the calculated unadjusted odds ratios and p-values were compared to this group. Non-Saudi donors, voluntary donations, and female donors were used as reference groups and the unadjusted odds ratios, and p-values were calculated compared to their analogous groups. Significance level was set at 5% (P < 0.05).
Results
Table 1 shows a multivariable analysis of demographical factors associated with the pre-donation deferral. The total number of blood donations during the study period were 28,189, of which 21,820 (77.4%) and 6369 (22.6%) were family replacement and voluntary donations, respectively (unadjusted odds ratio 3.43, P < 0.001. Most donors were Saudi citizens (92.6%, unadjusted odds ratio 12.54, P < 0.001).
 |
Table 1 Multivariable Analysis of Demographical Factors Associated with Pre-Donation Deferral (n = 28,189) |
The age-group of 18–25 years made a good contribution of 22.8% to the donation pool. This group was used as the reference group and the calculated unadjusted odds ratios and p-values of the other age-groups were compared to it. There was a significant variation in the donation contribution between all age-groups, except the age-group of 35–43 years. Donors between 26 and 34 years of age constituted the bulk of all donors (46%, unadjusted odds ratio, 2.06, P < 0.001), while those between 35 and 43 years showed a similar donation rate as the reference group with no significant variation (22.5%, unadjusted odds ratio, 0.99, P = 0.4767). Donors older than 44 years contributed only a significantly low number (7.9%) of the all donations. Another significant variation existed between genders; the males constituting 98.2% and females 1.8% (unadjusted odds ratio 53.42, P < 0.001).
Of the 28,189 potential donations during the study period, there were 3300 (11.7%) temporary deferrals (Table 2). Every blood donation deferral was based on a single reason. Recent intake of various medications was the main cause of deferral (24.4%) followed by low hemoglobin (14.8%), low or high blood pressure (14.6%), low or high pulse (13.6%), and low weight (11.6%). Other reasons for deferring prospective donors included recent illness (7.7%), recent donation of less than 56 days (4.8%), age below 18 years (4.2%), temperature exceeding 37.6° C (0.9%), and unhealthy general appearance (1.1%).
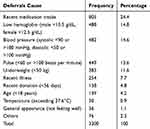 |
Table 2 Frequency and Percentage of Deferrals by Causes of Deferral (n = 3300) |
Discussion
Based on the recognition that voluntary non-remunerated blood donors are the foundation of a safe, sustainable blood supply, the WHO has set a global action plan that will enable countries to approach 100% voluntary blood donation.3 While there were no paid donors, family replacement donors in our study constituted most of the donations. They remain a critical source of non-remunerated blood that meets all classical criteria of voluntary non-remunerated donors and should be considered as legitimate and paramount at this point of time instead of being discouraged.15
Including Saudi Arabia, worldwide there was an increase in voluntary blood donation units in the reporting period between 2008 and 2013.2 However, 70 countries remained considerably dependent on family replacement and paid blood donors, with these donations accounting for more than 50% of their blood supplies in 2013.2 Nonetheless, family replacement donors continue to dominate in some regions because of the community’s belief that blood is a precious substance that should be shared only with their beloved ones and not donated to or accepted from others. Some also prefer to receive blood from a known person or family member than from a foreigner.
Although approximately one-third of Saudi Arabia’s inhabitants are immigrants, citizens make most of the donations (92.6%). As reported previously on several occasions, immigrants tend to donate less because of religious and cultural reasons or misunderstanding of the process and safety of the local system.16 Religious and other cultural behaviors represent a major motivating factor for blood donation.
A wide variation in blood donation rates among countries exists, ranging from 0.3 to 56 per 1000 population. The median whole blood donation rates were 32.1, 14.9, 7.8, and 4.6 donations per 1000 population per year in high-, upper-middle-, lower-, and low-income countries, respectively.2 However, the whole blood donation rate in Saudi Arabia was 17.8 per 1000 population in 2017.17
Donors in the 26–34 years of age constituted most of the donations (46.8%), with individuals in the 18–34 years of age contributing 69.6%, as compared to 45.2% for the 18–39 years age-group in the USA for example.8 Moreover, older people over 44 years of age contributed only 7.9% as compared to 54.8% for over 40 years of age in the USA.8 This indicates that age affects blood donor and donation rates. In this study, younger individuals in the 18–25 years age-group donated 22.8% of the total which is in agreement with studies conducted in Brazil, China, and sub-Saharan African countries,6,7,18,19 but inconsistent with a further study in which young donors only donated 9% of the units.20 The high percentage of young donors reported in our study was probably due to a strong focus on recruitment among college students.
As a large proportion of young adults are therefore able to donate blood, the prospects of recruiting young people as voluntary blood donors seem generally positive.21 On the other hand, older individuals donated less frequently than younger individuals unlike other studied in the USA and Europe.8–11 The observed decrease in donation prevalence after the age of 35 years may most likely be attributed to parenthood which seems to influence the donation frequency. Older donor’s retention should be encouraged as they may safely continue to donate even in their seventies.22
Women are usually underrepresented and donate blood less than men,21,23,24 this difference is particularly marked in this study with women contributing only 1.8% of the total donations. The poor rate of female donation in this study may be attributed to the lack of accommodation facilities at the donation suites, in addition to other social factors and beliefs, such as the fear of becoming anemic.25 This study also shows that in a situation where younger donors dominate, a lower proportion of females participate due to pregnancy and lactation.21 Previous research has shown that women experience up to 70% more deferrals from blood donation than men, due to higher rates of anemia, other health problems and adverse reactions.26 However, women play a more substantial role by donating more than 45% of the total donations in some European countries and the United States.27 Data from 118 countries on the gender profile of blood donors showed that an overall 30% of the blood donations were given by female donors; with 18 of these countries reported less than 10% of donations by women.2
The current study indicated a total pre-donation temporary deferral rate of 11.7%. The total deferral rates vary widely among countries; from less than 1% to over 37% with a median of 12%.2 Variations in deferral rates could be due to either the absence of donor selection criteria or appropriate donor selection procedures, or even different donor registration practices. Throughout Europe, the United States, and Canada, deferral rates average approximately 10%, with a considerable variation from as low as 1.4% up to as high as 25%.28
The main reason for pre-donation temporary deferral in this study was the recent intake of medications. Similar results were reported previously where the high deferral rate was due to increased use of therapeutic agents amongst the population.29 Drugs differ widely by structure and properties and include analgesics and antibiotics that result in a few days deferral to some growth hormones that result in permanent deferral. The use of drugs is widespread amongst prospective blood donors and is expected to rise due to many of them being on long-term treatment.30 Their exclusion will decrease the availability of donors dramatically. Various factors affect the final decision to defer, including concentration, pharmacologic properties, metabolites, and interactions of the drug.31
The second most common reason for pre-donation temporary deferral was a low hemoglobin level. Worldwide, approximately 10% of blood donation candidates are temporarily deferred due to low hemoglobin.32 Several studies have shown that hemoglobin-related deferrals were found to be the main cause of increased deferral rates.33,34 Female blood donors are most commonly deferred for low hemoglobin with iron deficiency being frequently detected in these donors, especially if they are premenopausal or repeat donors.
Abnormal blood pressure was the third most common deferral cause and resulted in 14.6% of the total. Whole blood donations with negative experiences were associated with a statistically significant higher pre-donation blood pressure at a subsequent visit.35 Low blood pressure was the major causes of rejection in one study at Saudi Arabia.36 A normal blood pressure is generally regarded as an indicator of good health. However, there is no evidence that raised baseline blood pressure, treated hypertension or low blood pressure were predictive of increased adverse reactions.37
Abnormal pulse rates were another very important cause for temporary deferral. First-time donors are usually nervous and anxious about donation and must be allowed to relax before taking a second pulse reading. Nevertheless, it has been postulated that pulse rate measurement in prospective donors is not warranted.38 Donors who exercised regularly with no history of heart disease and were under 55 years of age were usually not deferred for bradycardia (pulse <50 beats/minute).
Underweight resulted in 11.6% of the total deferrals; many donors being below 50 kg of body weight. Low weight was also an important reason for temporary deferral which may reflect poor nutritional status of the population. Because both anemia and low weight are curable, many temporarily deferred donors can be recruited back into the donor pool after proper management.
Other minor temporary deferral causes in this study included recent illness, previous donation, underage, body temperature, and not feeling well on the donation day.
The limitations encountered in this study are that it is based on data from a single-center and cannot be a good representation of a countrywide blood donation profile. A further limitation is that some of the information obtained was self-reported and could not be validated which may suggest a possible information bias, perhaps related to a social desirability bias.
In an attempt to study whether the reason for donating blood and the cause for temporary deferral of prospective blood donors might have changed over the period of the study (2010–2018), simple descriptive statistics has shown no marked differences in neither the demography of the donors nor the distribution of the causes for temporary deferral were noted.
Conclusion
This study showed a profile of blood donors consisting mainly of young Saudi male citizen who mostly donate for family replacement. The deferral rate is average compared to other countries and the causes are similar to those detected in other high-income developing countries.
Identification of the donor deferral pattern is an important tool for blood safety and provides a major trend for policy formulation. Indeed, the determination of the causes of donor deferral will enhance the return and retention of the temporarily deferred donors. Increased accessibility and frequent invitations are necessary for the retention of temporarily deferred donors.39
Young men also need help to integrate the blood donation habit into their lives. Most of the blood donations were given because of being a relative or friend. Greater efforts are required to increase the collection of voluntary non-remunerated blood donations to reduce the reliance on family replacement for the national blood supply.
The current findings suggest that it is important to campaign extensively to educate the public about the importance, ease, and lack of risk involved in blood donation. Previous findings suggested that social media could help to improve the blood donation practice in Saudi Arabia where there is a shortage of blood donors.40 The poor rate of female donation can be improved by providing more accommodation facilities at the donation suites and improving health awareness through repeated campaigns.
Acknowledgment
The data presented in this manuscript were generously provided by the Laboratory Medicine Department of the King Fahad Military Medical Complex to whom we are greatly indebted. Special thanks are also due to Mr Louis Greenwood for reading the manuscript.
Disclosure
The author declares no conflicts of interest in this work.
References
1. World Health Organization. Blood Donor Selection: Guidelines on Assessing Donor Suitability for Blood Donation. World Health Organization: Geneva; 2012.
2. World Health Organization. The 2016 Global Status Report on Blood Safety and Availability. Geneva: World Health Organization; 2017.
3. World Health Organization & International Federation of Red Cross and Red Crescent Societies. Towards 100% Voluntary Blood Donation: A Global Framework for Action. Geneva: World Health Organization; 2010.
4. Veldhuis IJ, Doggen CJ, Tasma F, et al. Donor profiles: demographic factors and their influence on the donor career. Vox Sang. 2009;97:129–138. doi:10.1111/j.1423-0410.2009.01201.x
5. Carneiro-Poretti AB, Sabino EC, Sampaio, et al. Demographic profile of blood donors at three major Brazilian blood centers: results from the International REDS-II study, 2007 to 2008. Transfusion. 2010;50:918–925. doi:10.1111/j.1537-2995.2009.02529.x
6. Ouk Y, Yau KK, Poon CM, et al. Donation frequency and its association with demographic characteristics a 1-year observational study. Transfus Med. 2015;25:366–373. doi:10.1111/tme.12267
7. Yang BC, Shao CP, Zhang YY, et al. Two decades of voluntary nonremunerated blood donation in Shenzhen, China. Transfusion. 2015;55:1108–1114. doi:10.1111/trf.12964
8. Goldman M, Steele WR, Di Angelantonio E, et al. Comparison of donor and general population demographics over time: a BEST Collaborative group study. Transfusion. 2017;57:
9. Ritter S, HaMoed O, Offergeld R. Demography and donation frequencies of blood and plasma donor populations in Germany. Update 2010 and 5-year comparison. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2012;55:914–922. doi:10.1007/s00103-012-1515-2
10. Atsma F, Veldhuizen I, de VF, et al. Cardiovascular and demographic characteristics in whole blood and plasma donors: results from the donor insight study. Transfusion. 2011;51:412–420. doi:10.1111/j.1537-2995.2010.02867.x
11. Notari EP, Zou S, Fang CT, et al. Age-related donor return patterns among first-time blood donors in the United States. Transfusion. 2009;49:2229–2236. doi:10.1111/j.1537-2995.2009.02288.x
12. Cimaroli K, Páez A, Newbold KB, et al. Individual and contextual determinants of blood donation frequency with a focus on clinic accessibility: a case study of Toronto, Canada. Health Place. 2012;18:424–433. doi:10.1016/j.healthplace.2011.12.005
13. Prados Madrona D, Fernández Herrera MD, Prados Jiménez D, et al. Women as whole blood donors: offers, donations and deferrals in the province of Huelva, South-western Spain. Blood Transfus. 2014;12:s1120. doi:10.2450/2012.0117-12
14. Ringwald J, Zimmermann R, Eckstein R. Keys to open the door for blood donors to return. Transfus Med Rev. 2010;24:295–304. doi:10.1016/j.tmrv.2010.05.004
15. Allain JP, Sibinga CT. Family donors are critical and legitimate in developing countries. Asian J Transfus Sci. 2016;10:5–11. doi:10.4103/0973-6247.164270
16. Weidmann C, Schneider S, Litaker D, et al. A spatial regression analysis of German community characteristics associated with voluntary non-remunerated blood donor rates. Vox Sang. 2012;102:47–54. doi:10.1111/j.1423-0410.2011.01501.x
17. Ministry of Health. Annual Statistical Book. Riyadh: Ministry of Health; 2017. https://www.moh.gov.sa/en/Ministry/Statistics/book/Pages/default.aspx.
18. Kanagasabai U, Chevalier MS, Drammeh B, et al. Trends and gaps in national blood transfusion services 14 sub-Saharan African countries, 2014–2016. MMWR Morb Mortal Wkly Rep. 2018;67:1392–1396. doi:10.15585/mmwr.mm6750a4
19. Valerian DM, Mauka WI, Kajeguka DC, et al. Prevalence and causes of blood donor deferrals among clients presenting for blood donation in northern Tanzania. PLoS One. 2018;13:e0206487. doi:10.1371/journal.pone.0206487
20. Zou S, Musavi F, Notari EP, et al. Changing age distribution of the blood donor population in the United States. Transfusion. 2008;48:251–257. doi:10.1111/j.1537-2995.2007.01517.x
21. Zito E, Alfieri S, Marconi M, et al. Adolescents and blood donation: motivations, hurdles and possible recruitment strategies. Blood Transfus. 2012;10:45–58. doi:10.2450/2011.0090-10
22. Kalargirou AA, Beloukas AI, Kosma AG, et al. Attitudes and behaviours of Greeks concerning blood donation: recruitment and retention campaigns should be focused on need rather than altruism. Blood Transfus. 2014;12:320–329. doi:10.2450/2014.0203-13
23. Ferdández-Montoya A, López-Berrio A, Luna del Castillo JD. How some attitudes, beliefs and motivations of Spanish blood donors evolve over time. Vox Sang. 1998;74:140–147. doi:10.1046/j.1423-0410.1998.7430140.x
24. Ringwald J, Lange N, Rabe C, et al. Why do some apheresis donors donate blood just once. Vox Sang. 2007;93:354–362. doi:10.1111/j.1423-0410.2007.00977.x
25. Elsafi SH, Al Zahrani MJ, Al Zahrani EM. Awareness and practice of blood donation by college students in Dhahran, Saudi Arabia. ISBT Sci Ser. 2015;10:11–17. doi:10.1111/voxs.12172
26. Newman BH, Newman DT, Ahmad R, et al. The effect of whole-blood donor adverse events on blood donor return rates. Transfusion. 2007;46:1374–1379. doi:10.1111/j.1537-2995.2006.00905.x
27. Bani M, Giussani B. Gender differences in giving blood: a review of the literature. Blood Transfus. 2010;8:278–287. doi:10.2450/2010.0156-09
28. De Kort W, Mayr W, Jungbauer C, et al. Blood donor selection in European Union directives: room for improvement. Blood Transfus. 2016;14:101–108. doi:10.2450/2015.0148-15
29. Jamal S, Shaikh I, Sohail S, et al. Frequency and causes of deferral amongst voluntary non‐remunerated blood donors from Pakistan – a single centre study. ISBT Sci Ser. 2018;13:136–140. doi:10.1111/voxs.12411
30. Melanson SEF, Stowell CP, Flood JG, et al. Does blood donor history accurately reflect the use of prescription medications? A comparison of donor history and serum toxicologic analysis. Transfusion. 2006;46:1402–1407. doi:10.1111/j.1537-2995.2006.00909.x
31. Becker CD, Stichtenoth DO, Wichmann MG, et al. Blood donors on medication an approach to minimize drug burden for recipients of blood products and to limit deferral of donors. Transfus Med Hemother. 2009;36:107–113. doi:10.1159/000203355
32. Annen K, Delaney M, Leitch D, et al. The health implications of low hemoglobin deferral in infrequent blood donors. Transfusion. 2015;55:86–90. doi:10.1111/trf.12801
33. de Groot R, Prinsze FJ, Broekman-Piets R, et al. On-site deferral of whole blood and plasma donors in the Netherlands between 2006 and 2013. ISBT Sci Ser. 2015;10(2):73–81. doi:10.1111/voxs.12207
34. Al Shaer L, Sharma R, AbdulRahman M. Analysis of blood donor pre-donation deferral in Dubai: characteristics and reasons. J Blood Med. 2017;2017(8):55–60. doi:10.2147/JBM.S135191
35. Hoogerwerf MD, Veldhuizen IJ, van den Hurk K, et al. Negative experiences and predonation blood pressure at the subsequent donation in blood donors. Vox Sang. 2016;110:107–115. doi:10.1111/vox.12319
36. AlNouri AK, Maghrabi LA, Hamdi SS, et al. Analysis of the most common causes of blood donor deferral in northern Jeddah: a single-center study. J Blood Med. 2019;10:47–51. doi:10.2147/JBM.S178822
37. Stainsby D, Brunskill S, Chapman CE, et al. Safety of blood donation from individuals with treated hypertension or non-insulin dependent type 2 diabetes a systematic review. Vox Sang. 2010;98:431–440. doi:10.1111/j.1423-0410.2009.01275.x
38. Germain M, Delage G, Grégoire Y, et al. Donation by donors with an atypical pulse rate does not increase the risk of cardiac ischaemic events. Vox Sang. 2013;104:309–316. doi:10.1111/vox.12002
39. Kasraian L, Tavassoli A. Relationship between first-year blood donation, return rate for subsequent donation and demographic characteristics. Blood Transfus. 2012;10:448–452. doi:10.2450/2012.0097-11
40. Alanzi T, Alsaeed B. Use of social media in the blood donation process in Saudi Arabia. J Blood Med. 2019;10:417–423. doi:10.2147/JBM.S217950
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
