Back to Journals » Drug Design, Development and Therapy » Volume 9
Comparison of peginterferon alfa-2a and alfa-2b for treatment of patients with chronic hepatitis C:a retrospective study using the Japanese Interferon Database
Authors Sato I, Shimbo T, Kawasaki Y, Masaki N
Received 4 August 2014
Accepted for publication 26 August 2014
Published 30 December 2014 Volume 2015:9 Pages 283—290
DOI https://doi.org/10.2147/DDDT.S72245
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Shu-Feng Zhou
Izumi Sato,1 Takuro Shimbo,2 Yohei Kawasaki,3 Naohiko Masaki4
1Department of Clinical Study and Informatics, Center for Clinical Sciences, National Center for Global Health and Medicine, Tokyo, Japan; 2Ohta Nishinouchi Hospital, Fukushima, Japan; 3Department of Mathematics, Tokyo University of Science, Tokyo, Japan; 4The Research Center for Hepatitis and Immunology, National Center for Global Health and Medicine, Chiba, Japan
Purpose: We aimed to compare the rates of sustained virologic response (SVR) achieved with peginterferon (PEG-IFN) alfa-2a and alfa-2b in combination with ribavinin (RBV) for chronic hepatitis C, using a large database of hepatitis cases to improve the generalizability of these results.
Methods: We identified patients with chronic hepatitis C who were treated with PEG-IFN alfa-2a or alfa-2b and RBV, from the Japanese Interferon Database, between December 2009 and April 2013. This database contains the medical records of IFN treatment collected from 36 prefectures in Japan. Multivariable logistic regression analysis was used to compare SVR rates obtained with PEG-IFN alfa-2a and alfa-2b, in combination with RBV.
Results: A total of 16,349 patients were recorded in the Japanese Interferon Database. After application of the exclusion criteria, 12,706 patients (3,578 [1,710 males, 1,868 females] on PEG-IFN alfa-2a; and 9,128 [4,652 males, 4,476 females] on PEG-IFN alfa-2b) were included in this analysis. The SVR rate in the PEG-IFN alfa-2b group was 62.0%, as compared with a rate of 55.1% in the PEG-IFN alfa-2a group (crude odds ratio =1.31; 95% confidence interval [CI]: 1.23 to 1.44). There was no significant difference in the adjusted SVR rates between the two groups (adjusted odds ratio =0.96; 95% CI: 0.88 to 1.05). Similar proportions of adverse events were observed in the two groups, with the exception of thrombocytopenia, retinopathy, and anemia.
Conclusion: There was no significant difference in the SVR rates and safety profile between chronic hepatitis C patients treated with the PEG-IFN alfa-2a and alfa-2b.
Keywords: sustained virologic response, HCV genotype, sustained virologic response, adverse events
Introduction
More than 170 million persons worldwide are infected with the hepatitis C virus (HCV), and the number of deaths caused by HCV-related liver diseases is more than 35 thousand per year.1 In addition, HCV infection is associated with an increased incidence of hepatocellular carcinoma.2 To reduce the risk of developing hepatocellular carcinoma and HCV-related liver diseases, a treatment based on interferon (IFN) is commonly used for patients with chronic hepatitis C.3 Two types of pegylated interferon (PEG-IFNs) (alfa-2a and alfa-2b) are used, which are pegylated to improve their pharmacokinetic effects and pharmacodynamic actions, and which have a higher rate of sustained virologic response (SVR) and lower frequency of incidence of adverse reactions than IFN.4 Thus far, the general recommendation for the treatment of patients with chronic hepatitis C involves combination therapy with PEG-IFN (alfa-2a or alfa-2b) and ribavirin (RBV).3 However, previous studies that have compared the effectiveness and safety of treatment with PEG-IFN alfa-2a and alfa-2b for patients with chronic hepatitis C have yielded conflicting results.5–8
The largest randomized controlled trial (RCT) to date was a comparison in 2009 of SVR and safety in the treatment of 3,070 patients with chronic HCV genotype 1 among three groups (low-dose PEG-IFN alfa-2b plus RBV; standard-dose PEG-IFN alfa-2b plus RBV; and PEG-IFN alfa-2a plus RBV).9 That study excluded patients with hepatitis B virus (HBV) or human immunodeficiency virus (HIV) infection, as well as other liver diseases, and found that the rates of SVR and adverse event profiles among the three groups were similar. On the other hand, some meta-analyses of RCTs comparing PEG-IFN alfa-2a and alfa-2b suggested a higher SVR rate in the alfa-2a group than in the alfa-2b group.5,6 However, several limitations involving the study quality were pointed out, including a small sample size as well as inadequate blinding and randomization.5 A large retrospective cohort study was conducted to compare the SVR rate obtained with PEG-IFN alfa-2a and alfa-2b for the treatment of patients with chronic hepatitis C in Germany.10 A total of 3,414 patients were identified as a study cohort from the database. This study allowed the inclusion of patients who had a comorbid HBV or HIV infection and any HCV genotype, and used matched pair analysis, using the baseline patient characteristics to compare the rates of SVR with PEG-IFN alfa-2a and alfa-2b. Although a higher SVR rate was found for alfa-2a than for alfa-2b, the possibility of residual uncontrolled confounding was acknowledged, such as details of the therapeutic profiles, for eg, the duration of therapy in the two groups were different, even after subject matching.10 Thus far, a definitive conclusion has yet to be reached regarding the superiority of one PEG-IFN over the other.
In this study, we aimed to compare the rates of SVR with PEG-IFN alfa-2a and alfa-2b in combination with RBV for chronic hepatitis C, using a large database of hepatitis cases to improve the generalizability of these results.
Methods
The Japanese Interferon Database
Because hepatitis is becoming one of the most prevalent major infectious diseases, the Basic Act on Measures against Hepatitis in Japan was established to conquer hepatitis, by providing high quality medical care for patients with a hepatitis viral infection.11 As part of this measure, the Japanese Interferon Database, which is comprised of more than 16,000 patient records regarding IFN treatment for chronic hepatitis and/or cirrhosis, collected retrospectively from throughout Japan, was developed. This database contains diagnosis, IFN treatment data (type of IFN, with or without RBV), results of laboratory tests (date of test, HCV RNA, type of HCV genotype, aspartate aminotransferase, alanine aminotransferase [ALT], and platelet count), adverse drug reactions, and outcomes (SVR, and completed or discontinued treatment), which have been recorded in a standardized report form by practitioners. Serum HCV RNA levels were quantitated by Cobas® Amplicor HCV Monitor v2.0 (Roche Molecular Systems, Pleasanton, CA, USA) or Cobas® TaqMan HCV Test (Roche Molecular Systems).
This study was approved by the Institutional Review Board of the National Center for Global Health and Medicine.
Study population
We identified all of the patients with chronic hepatitis C from the Japanese Interferon Database who had received a combination treatment of PEG-IFN (alfa-2a or alfa-2b) and RBV between December 2009 and April 2013.
Patients meeting any of the following criteria were excluded from this study: comorbid cirrhosis or HBV infection; without RBV use; dual therapy with PEG-IFN alfa-2a and alfa-2b; any missing data items (sex, age, diagnosis, and/or comorbid condition, ie, liver diseases); and age under 16 years.
Statistical analysis
Descriptive statistics were calculated as absolute numbers, percentages, and means (± standard deviation [SD]) for each group. Patient baseline characteristics were compared between PEG-IFN alfa-2a and alfa-2b, using a t-test for age, the Wilcoxon rank-sum test for duration of therapy, the Mantel–Haenszel chi-square statistic for genotype, and the chi-square test for the other categorical variables. We also compared adverse events in the patients withdrawn from study, according to HCV genotype, using the Fisher’s exact test. To explore the association of patient SVR with chronic hepatitis C, we used multivariate logistic regression to calculate the adjusted odds ratio (OR) and the associated 95% confidence intervals (CIs). We included covariates to adjust for age, sex, platelet counts, ALT level, HCV viral load, genotype, and frequency of treatment. Interaction analyses were performed with the logistic regression model, to test for interactions between PEG-IFN and level of treatment experience or HCV genotype. The results indicated that there were no significant interactions (between type of PEG-IFN and treatment experience [P=0.229] or between type of PEG-IFN and HCV genotype [P=0.069]). The fit of the logistic model was assessed using Hosmer–Lemeshow tests. Subgroup analyses were performed according to treatment experience and genotype. The SAS software, version 9.3 (SAS Institute, Inc., Cary, NC, USA) was used for all analyses.
Results
Study population
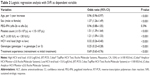
Between December 2009 and April 2013, a total of 16,349 patients were recorded in the Japanese Interferon Database. Of these, 3,643 subjects were excluded for the following reasons: comorbid condition of cirrhosis in 569 subjects and HBV infection in 300 subjects; without RBV use in 2,414 subjects; dual therapy of PEG-IFN alfa-2a and alfa-2b in 225 subjects; missing data (any of sex, age, diagnose, and/or comorbid condition [liver diseases]) in 261 subjects; and under 16 years of age in three subjects (Figure 1). The remaining 12,706 patients were included in this study. Of these, 3,578 subjects (1,710 [48%] males; 1,868 [52%] females) were taking PEG-IFN alfa-2a, with a mean age (SD) of 59.1 (10.0) years; and 9,128 subjects (4,652 [51%] males; 4,476 [49%] females) were taking PEG-IFN alfa-2b, with a mean age (± standard deviation) of 57.2 (±10.9) years (Table 1). Several differences were found between the two groups, as follows: the mean age was higher in the alfa-2a group than in the alfa-2b group; the proportion of male patients was higher in the alfa-2b group; the proportion of patients with an HCV genotype1 infection in the PEG-IFN alfa-2a group (2,874 [83%]) was higher than in alfa-2b group (5,564 [62%]); and, a higher proportion of initial treatment patients was obtained in the alfa-2b group (2,181 [62%]) than in the alfa-2a (7,086 [79%]).
Outcomes
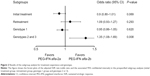
The SVR rate in patients receiving PEG-IFN alfa-2b was higher than that in patients receiving alfa-2a (crude OR=1.31; 95% CI: 1.23 to 1.44). After adjustment for potential confounders (including age, sex, platelet count, alanine aminotransferase [ALT] level, HCV viral load, genotype, and treatment experience), no significant difference was found in SVR rates between the PEG-IFN alfa-2a group and the PEG-IFN alfa-2b group (adjusted OR=0.96; 95% CI: 0.88 to 1.05) (Table 2).
We also performed subgroup analyses, according to treatment experience and genotype. No significant differences were found between the PEG-IFN alfa-2b and alfa-2a groups, in terms of adjusted SVR rate, in patients receiving their initial treatment (crude OR=1.27; 95% CI: 1.14 to 1.40; adjusted OR=0.90; 95% CI: 0.80 to 1.01), patients receiving retreatment (crude OR=1.15; 95% CI: 1.00 to 1.33; adjusted OR=1.09; 95% CI: 0.93 to 1.27), and patients with HCV genotype 1 infections (crude OR=1.00; 95% CI: 0.91 to 1.09; adjusted OR=0.95; 95% CI: 0.86 to 1.05). The adjusted SVR rate for PEG-IFN alfa-2b in patients with HCV genotype 2 or 3 was superior to that of PEG-IFN alfa-2a (crude OR=1.36; 95% CI: 1.10 to 1.69; adjusted OR=1.35; 95% CI, 1.08 to 1.69) (Figure 2).
Adverse events
During the study, significant differences between the two treatments were observed in patients with HCV genotype 1. Ninety-six patients withdrew from treatment due to thrombocytopenia (46 [1.6%] in the PEG-IFN alfa-2a group and 50 [0.9%] in the alfa-2b group [P=0.005]), and 57 patients withdrew due to retinopathy (13 [0.5%] in the alfa-2a group and 44 [0.8%] in alfa-2b group [P=0.091]) (Table 3). In contrast were the patients with genotype 2 or 3, who displayed anemia (ten [1.6%] in the alfa-2a group and 25 [0.7%] in the alfa-2b group [P=0.034]), thrombocytopenia (eight [1.3%] in the alfa-2a group and 14 [0.4%] in alfa-2b group [P=0.012]), and retinopathy (five [0.8%] in the alfa-2a group and five [0.1%] in the alfa-2b group [P=0.010]) (Table 4). No other significant differences were observed between the study groups.
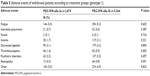  | Table 3 Adverse events of withdrawal patients according to treatment groups (genotype 1) |
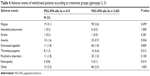  | Table 4 Adverse events of withdrawal patients according to treatment groups (genotype 2, 3) |
Discussion
We conducted a retrospective cohort study to compare the SVR rate in patients with chronic hepatitis C treated with PEG-IFN alfa-2a and alfa-2b in combination with RBV, using data from the large Japanese Interferon Database to improve the generalizability of the results. We employed multivariate logistic regression analysis to adjust for potential confounders, as the demographic characteristics at baseline differed between the two groups. We found similar SVR rates in patients with chronic hepatitis C who received either PEG-IFN alfa-2a or alfa-2b in combination with RBV.
Our findings were consistent with previous results from the largest reported RCT, which involved 3,070 patients.9,12,13 On the other hand, some other previous studies,10,14 including the largest retrospective cohort study, which involved 3,414 subjects, presented results that conflicted with our findings. As mentioned above, several limitations of these previous studies have been pointed out (eg, small sample size, inadequate blinding or randomization, difference in treatment regimen, and different study populations).5,15 To enhance generalizability, we conducted a study with a larger sample size (12,706 subjects) than used in previous studies.5–7,9,10 We found no difference in the adjusted SVR rate between the two treatment groups, even though the sample size was large enough to detect such a difference. In addition, our results were obtained from a realistic medical setting, using data recorded according to the actual treatments applied to patients with hepatitis, by practitioners. Previously, few studies had been performed that reflected a realistic medical setting for treatment of patients with chronic hepatitis C because most of the previous studies were RCTs.5–7 We also performed two subgroup analyses, according to treatment experience and genotype, because the largest reported RCT9 had included only patients receiving their initial treatment and patients with HCV genotype 1. Similar to our other results, we also found no difference in the adjusted SVR rate between treatment with PEG-IFN alfa-2a and alfa-2b from the subgroup analyses, except for the subgroup of genotypes 2 and 3. In this subgroup, alfa-2b had higher a SVR rate, although the interaction was not significant.
While the present study suggests that PEG-IFN alfa-2b may be the preferable treatment for patients with HCV genotypes 2 and 3, the results of several RCTs9,16,17 showed no difference between treatment with PEG-IFN alfa-2a or alfa-2b in patients with genotype 1 or with genotypes 1–4.
In a study comparing the pharmacokinetics and pharmacodynamics of the two drugs,18 PEG-IFN alfa-2b displayed a greater effect of biological activity by reducing HCV-RNA and upregulating IFN-related response genes. However, the duration of this effect may be affected by the time period between dosing because the volume of distribution of PEG-IFN alfa-2b is large, and it is metabolized faster than PEG-IFN alfa-2a.8 Due to its higher molecular weight and branched pegylation, the extravascular volume of distribution of PEG-IFN alfa-2a is smaller. Thus, its duration in the body is longer than that of PEG-IFN alfa-2b. In general, the amount of a drug in the body tends to decrease as body weight increases; however, in this study, the amount of PEG-IFN alfa-2b in the body was constant regardless of body weight because the dosage was adjusted for body weight.18 In the present study, PEG-IFN alfa-2b was more effective than PEG-IFN alfa-2a for the treatment of patients with genotypes 2 and 3. This may be because the patients treated with PEG-IFN alfa-2b received a dosage based on body weight, whereas patients treated with PEG-IFN alfa-2a were treated with a fixed dosing regimen, without accounting for weight. However, information regarding the patients’ body weight and dosage of PEG-IFN was not included in this database.
We found that proportions of adverse events, such as thrombocytopenia, retinopathy, and anemia, were higher in patients treated with PEG-IFN alfa-2a. In a previous study comparing pharmacokinetics and pharmacodynamics,18 both leukocytes and neutrophils were significantly decreased in patients receiving PEG-IFN alfa-2a versus those receiving PEG-IFN alfa-2b. Additionally, the incidences of hematological abnormalities tend to be higher in PEG-IFN alfa-2a–treated patients.18 In contrast, RCTs comparing PEG-IFN alfa-2a and alfa-2b, including a Japanese study19 and the largest study ever conducted,9 showed no difference in hematological abnormalities following termination of treatment. In the RCTs, the subjects may have been selected from patients in good condition or from those who were expected to adhere to the study treatment. Our data suggests that hematological abnormalities, such as thrombocytopenia, may develop in actual medical care situations, because we used data obtained from the database of medical records from patients receiving IFN treatment. Further, our results are consistent with the previous study18 evaluating pharmacokinetics and pharmacodynamics.
The strengths of our study include the large sample size, the use of data collected from actual medical settings, and the inclusion of patients with all types of HCV genotype infections and patients with or without previous treatment experience.
Our study also has several limitations. First, there were residual confounders, which could persist due to unmeasured or imprecisely measured potential confounding factors. To adjust for potential confounders, we used multivariable logistic regression. Secondly, there was a reporting bias because the data were recorded by practitioners using a standardized report form. Additional studies are needed to validate the data, using an alternative existing database source (eg, electronic medical records database or claims database). Thirdly, the viral load levels might have been misclassified because the measurement methods for HCV RNA in this database differed depending on the time of therapy. Finally, further studies are required to assess the rate of SVR between the two medications in combination with simeprevir, a new agent for the treatment of chronic hepatitis C, because the current standard therapy for chronic hepatitis C is triple therapy with PEG-IFN (alfa-2a or alfa-2b), RBV, and simeprevir.20,21
Conclusion
There was no significant difference in the SVR rates and safety profile between chronic hepatitis C patients treated with the PEG-IFN alfa-2a and alfa-2b.
Acknowledgments
Financial support was provided by a Grant-in-Aid from the Ministry of Health, Labour and Welfare of Japan (Research on Hepatitis: 2009–2014) to NM.
The authors wish to thank Ms Mikako Kajio and Ms Asako Horihata for technical assistance during the data analysis. The great contributions of the 36 prefectural members and all of the medical staff engaged in long-term IFN treatment and data collection are particularly acknowledged.
Disclosure
The authors report no conflicts of interest in this work.
References
who.int [homepage on the Internet]. Hepatitis C. Fact sheet N°164. World Health Organization; 2014 [updated April 2014; cited June 26, 2014]. Available from: http://who.int/mediacentre/factsheets/fs164/en/index.html. Accessed Sept 13, 2014. | ||
Shepard CW, Finelli L, Alter MJ. Global epidemiology of hepatitis C virus infection. Lancet Infect Dis. 2005;5(9):558–567. | ||
Editors of the Drafting Committee for Hepatitis Management Guidelines, The Japan Society of Hepatology. Guidelines for the management of hepatitis C virus infection: First edition, May 2012, The Japan Society of Hepatology. Hepatol Res. 2013;43(1):1–34. | ||
Shiffman ML. Pegylated interferons: what role will they play in the treatment of chronic hepatitis C? Curr Gastroenterol Rep. 2001;3(1):30–37. | ||
Zhao S, Liu E, Chen P, et al. A comparison of peginterferon α-2a and α-2b for treatment-naive patients with chronic hepatitis C virus: A meta-analysis of randomized trials. Clin Ther. 2010;32(9):1565–1577. | ||
Singal AK, Jampana SC, Anand BS. Peginterferon alfa-2a is superior to peginterferon alfa-2b in the treatment of naïve patients with hepatitis C virus infection: meta-analysis of randomized controlled trials. Dig Dis Sci. 2011;56(8):2221–2226. | ||
Awad T, Thorlund K, Hauser G, Stimac D, Mabrouk M, Gluud C. Peginterferon alpha-2a is associated with higher sustained virological response than peginterferon alfa-2b in chronic hepatitis C: systematic review of randomized trials. Hepatology. 2010;51(4):1176–1184. | ||
Brochot E, Nguyen-Khac E, Duverlie G. Equal efficacy between the two types of peginterferon on HCV: a matter of relapse? Antiviral Res. 2013;98(1):1–3. | ||
McHutchison JG, Lawitz EJ, Shiffman ML, et al; IDEAL Study Team. Peginterferon alfa-2b or alfa-2a with ribavirin for treatment of hepatitis C infection. N Engl J Med. 2009;361(6):580–593. | ||
Witthoeft T, Hueppe D, John C, et al. Efficacy and tolerability of peginterferon alfa-2a or alfa-2b plus ribavirin in the daily routine treatment of patients with chronic hepatitis C in Germany: the PRACTICE study. J Viral Hepat. 2010;17(7):459–468. | ||
Ministry of Health, Labour and Welfare. Measures against Hepatitis. Tokyo: Ministry of Health, Labour and Welfare; 2010. Available from: http://www.mhlw.go.jp/english/wp/wp-hw5/dl/23010219e.pdf. Accessed April 8, 2014. | ||
Yenice N, Mehtap O, Gümrah M, Arican N. The efficacy of pegylated interferon alpha 2a or 2b plus ribavirin in chronic hepatitis C patients. Turk J Gastroenterol. 2006;17(2)97–98. | ||
Scotto G, Fazio V, Fornabaio C, et al. Peg-interferon alpha-2a versus Peg-interferon alpha-2b in nonresponders with HCV active chronic hepatitis: a pilot study. J Interferon Cytokine Res. 2008;28(10):623–629. | ||
Mach TH, Cieśla A, Warunek W, et al. Efficacy of pegylated interferon alfa-2a or alfa-2b in combination with ribavirin in the treatment of chronic hepatitis caused by hepatitis C virus genotype 1b. Pol Arch Med Wewn. 2011;121(12):434–439. | ||
Tsubota A, Fujise K, Namiki Y, Tada N. Peginterferon and ribavirin treatment for hepatitis C virus infection. World J Gastroenterol. 2011;17(4):419–432. | ||
Rumi MG, Aghemo A, Prati GM, et al. Randomized study of peginterferon-alpha2a plus ribavirin vs peginterferon-alpha2b plus ribavirin in chronic hepatitis C. Gastroenterology. 2010;138(1):108–115. | ||
Laguno M, Cifuentes C, Murillas J, et al. Randomized trial comparing pegylated interferon alpha-2b versus pegylated interferon alpha-2a, both plus ribavirin, to treat chronic hepatitis C in human immunodeficiency virus patients. Hepatology. 2009;49(1):22–31. | ||
Silva M, Poo J, Wagner F, et al. A randomised trial to compare the pharmacokinetic, pharmacodynamic, and antiviral effects of peginterferon alfa-2b and peginterferon alfa-2a in patients with chronic hepatitis C (COMPARE). J Hepatol. 2006;45(2):204–213. | ||
Miyase S, Haraoka K, Ouchida Y, Morishita Y, Fujiyama S. Randomized trial of peginterferon α-2a plus ribavirin versus peginterferon α-2b plus ribavirin for chronic hepatitis C in Japanese patients. J Gastroenterol. 2012;47(9):1014–1021. | ||
Hayashi N, Izumi N, Kumada H, et al. Simeprevir with peginterferon/ribavirin for treatment-naïve hepatitis C genotype 1 patients in Japan: CONCERTO-1, a phase III trial. J Hepatol. 2014;61(2):219–227. | ||
Izumi N, Hayashi N, Kumada H, et al. Once-daily simeprevir with peginterferon and ribavirin for treatment-experienced HCV genotype 1-infected patients in Japan: the CONCERTO-2 and CONCERTO-3 studies. J Gastroenterol. 2014;49(5):941–953. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.