Back to Journals » Clinical Interventions in Aging » Volume 15
A Simple Bedside Screening Tool for Spasticity Referral
Authors Hacker ML , Ploucher S, Naik AG , Turchan M, Meystedt JC, Harper K, Hedera P, Pirtle CJ , Stubblefield K, Charles D
Received 7 February 2020
Accepted for publication 11 April 2020
Published 13 May 2020 Volume 2020:15 Pages 655—662
DOI https://doi.org/10.2147/CIA.S248602
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Walker
Mallory L Hacker,1,2 Shelby Ploucher,1,3 Aaditi G Naik,1,4 Maxim Turchan,1 Jacqueline C Meystedt,1 Kelly Harper,1 Peter Hedera,1 Claude J Pirtle,5 Kassandra Stubblefield,1 David Charles1
1Department of Neurology, Vanderbilt University Medical Center, Nashville, TN, USA; 2Department of Physical Medicine and Rehabilitation, Vanderbilt University Medical Center, Nashville, TN, USA; 3Florida State University College of Medicine, Tallahassee, FL, USA; 4Pritzker School of Medicine, The University of Chicago, Chicago, IL, USA; 5Department of Biomedical Informatics, Vanderbilt University Medical Center, Nashville, TN, USA
Correspondence: Mallory L Hacker
Neurology and Physical Medicine & Rehabilitation, Vanderbilt University Medical Center, 440 Crystal Terrace, 3319 West End Ave, Nashville, TN 37203, USA
Email [email protected]
Background and Objectives: Spasticity is common in long-term care facilities; however, this often-disabling condition is largely underdiagnosed in this setting and therefore left untreated. This study aimed to test the ability of a three-question flowchart used at the bedside by primary care providers in the long-term care setting to identify residents in need of referral to a specialist for spasticity consultation.
Methods: All residents of a single long-term care facility were approached for participation in this cross-sectional, observational study. Spasticity diagnostic evaluations by a movement disorders specialist neurologist (reference standard) were compared with referral determinations made by two primary care providers [a primary care physician (PCP) and a nurse practitioner (NP)] using the simple flowchart.
Results: The analysis included 49 residents (80% male, age 78.2± 9.0 years) who were evaluated by the reference standard neurologist and at least one primary care provider. The bedside referral tool demonstrated high sensitivity and moderate specificity when used by the PCP (92% and 78%, respectively; AUC=0.84) and NP (80% and 53%, respectively; AUC=0.67).
Conclusion: This simple tool may be useful for primary care providers to identify residents to be referred to a specialist for evaluation and treatment of spasticity. These results warrant further investigation of the potential utility of this screening tool across multiple long-term care facilities and various types of care providers.
Keywords: spasticity, neurological disease, long-term care, screening, primary care
Introduction
Spasticity is common in the long-term care setting (up to 35% of residents) but is unfortunately underdiagnosed and, therefore, often left untreated.1–3 This condition, which can arise following disease or injury to the central nervous system (CNS), is currently defined as “a disordered sensorimotor control, resulting from an upper motor neuron lesion, presenting as intermittent or sustained involuntary activation of muscles”.4 Failure to treat spasticity using available efficacious, FDA-approved therapies can result in complications such as pain, loss of function, and deformity, which can also negatively affect the quality of life and activities of daily living3,5,6 and impose a significant burden on caregivers.7
The underdiagnosis and subsequent lack of treatment for spasticity in the long-term care setting are likely due to the fact that primary care providers at these facilities are often stretched thin to see many residents suffering from a range of medical conditions and have not received specialized training in the recognition, diagnosis, and treatment of spasticity. Diagnosis of spasticity relies on a clinical conclusion informed by the patient’s medical history and findings from a physical and neurological examination.8 This type of evaluation is often performed by a physiatrist or neurologist specializing in movement disorders, which typically requires a referral for an outpatient consultation. The growing population of older adults and number of patients with long-lived neurological impairment,9,10 coupled with the underdiagnosis of spasticity and paucity of spasticity-trained practitioners,11 underscore the urgent medical need for improved methods to assist primary care providers in identifying long-term care residents who may have spasticity and may also benefit from available treatments.12 The utility of such a screening method will hinge not only on its performance but also on its ease of use by healthcare providers caring for this population.
In this study, a simple three-question referral tool was developed as part of a broader initiative to improve the screening, diagnosis, and treatment of spasticity in long-term care facilities. Adapted from a previous diagnostic assessment,13 this flowchart was designed to be used at the bedside by primary care providers to screen residents in the long-term care setting to identify those who likely have spasticity. This study’s objective was to test the ability of this simple bedside flowchart to be used by primary care providers without spasticity training to identify residents in need of referral to a specialist (physiatrist or movement disorders neurologist) for consultation.
Methods
Study Population
This cross-sectional, observational study (Vanderbilt University IRB #162074) was conducted in a 140-bed long-term care facility offering intermediate and skilled levels of nursing care for veterans and their spouses in the Southeast United States (NCT03209960). All 129 inpatient residents of the facility at the time of enrollment (December 2017 to February 2018) were approached for recruitment. The study neurologist and nursing staff at the facility made the determination whether each resident was cognitively capable of providing informed consent. A total of 59 residents were determined to be cognitively capable of providing informed consent and were approached for participation in-person by the principal investigator and study staff at the facility. A total of 70 residents were determined to be cognitively incapable of providing informed consent, and informational packets with informed consent forms were mailed to their medical decision makers. Study personnel also approached available medical decision makers at the facility and, if agreeable to participation, acquired proxy consent onsite. Written informed consent was obtained for all study participants, either directly by participants or their medical decision makers. This study was conducted in accordance with the Declaration of Helsinki.
Diagnosis, History, and Treatment of Spasticity
Subjects who enrolled in the study received a neurological examination from a neurologist specializing in movement disorders not affiliated with the long-term care facility to determine if spasticity was present. Diagnosis of spasticity by the movement disorders specialist (reference standard) was based on a clinical impression, including assessment of increased muscle tone, exaggerated tendon jerks, stretch reflex spread to extensors, repetitive stretch reflex discharges, clonus, Babinski response, mass synergy pattern, loss of dexterity, inadequate force generation, slow movements, and loss of selective control of muscles and limb segments. The neurologist also rated the severity of stiffness for the worst-affected limb for subjects diagnosed with spasticity using the Modified Ashworth Scale14,15 and determined whether treatment should be recommended. Medical records of enrolled participants were reviewed by study staff to extract information related to diagnoses of spasticity (most often identified in Section I of the Minimum Data Set (MDS) 3.0, “hemiplegia/hemiparesis”) or related ICD 9/10 codes, spasticity treatment history, and demographic information. History of CNS illness or injury known to be associated with spasticity was recorded from ICD 9/10 codes to document potential etiology (stroke, multiple sclerosis, cerebral palsy, traumatic brain injury, spinal cord injury, and spinal stenosis).
Bedside Referral Tool Examination
A bedside tool was developed as part of a broader initiative to improve the screening, diagnosis, and treatment of spasticity in long-term care facilities. The goal of this assessment was to guide the determination of whether spasticity may be present and warrant referral to a specialist (physiatrist or movement disorders neurologist) for a spasticity consultation. The referral tool was adapted from a previously piloted diagnostic tool13 and consisted of a simple one-page, paper-based screening flowchart, with three yes/no questions (Figure 1). Unlike the prior diagnostic assessment that was tested, this referral tool was designed to be completed by primary care physicians, nurse practitioners, or physician assistants who may be less familiar with spasticity and who may not conduct these elements in their typical exam.
Two primary care providers, one primary care physician (PCP) and one nurse practitioner (NP), not affiliated with the long-term care facility were each asked to evaluate subjects using the referral tool. Both providers were previously unfamiliar with the referral tool and study population, and neither provider received any training regarding spasticity or the use of the referral tool. Each provider was guided by the three-question flowchart to perform elements of a physical exam leading to a yes or no determination of whether the subject should be referred to a specialist for a spasticity consultation. Primary care providers were blind to subjects’ medical history, each other’s determination, and the reference standard neurologist’s decision. All subject examinations were completed between January 2018 and March 2018. After the conclusion of the study, the PCP, NP, and three members of the study staff were independently asked to estimate the shortest, longest, and mean times to complete the examination using the referral tool.
Statistical Analysis
Demographics, consent rates, prevalence of spasticity, history of neurological condition associated with spasticity, prior evidence of spasticity in the medical record, and prior spasticity treatment are reported for all subjects evaluated by the reference standard neurologist using descriptive statistics (n=49). Chi-square tests were used to compare self-consent versus proxy-acquired consent. True positives, false positives, true negatives, and false negatives were tabulated for both the PCP and NP in subjects who were also evaluated by the reference standard (n=43 and n=45, respectively). Sensitivity, specificity, and the area under the curve (AUC) in receiver operating characteristics (ROC) were calculated. Internal validation was performed using a bootstrapping resampling procedure (1000 replications; seed: 2019), and optimism-corrected AUCs are presented alongside uncorrected AUCs.16 The positive likelihood ratio (sensitivity/1-specificity) and negative likelihood ratio (1-sensitivity/specificity) were also calculated17 and used to estimate the probability of spasticity presence after administration of the referral tool (post-test probability). Analyses were performed using STATA 15.1 (StataCorp LP, College Station, TX) and the R statistical package (version 3.2.3). All P values are two-sided, and the ROC Curve and Fagan’s nomogram were generated using R ggplot2 package.
Results
Study Population
Sixty residents enrolled in this study, with 54 subjects evaluated by the reference standard neurologist, primary care physician, and/or nurse practitioner. Eleven enrolled subjects were unable to receive an evaluation by the reference standard neurologist: seven did not complete any study procedures (one withdrew from the study, five were discharged from the facility, one was deceased), and four were evaluated by the primary care physician and/or the nurse practitioner for signs of spasticity but not by the reference standard neurologist in order to receive an official determination of spasticity. Therefore, the total number of subjects evaluated for the presence or absence of spasticity in this study was 49. The majority of subjects in this study were male (80%, 39/49), and the mean age of this cohort was 78.2±9.0 years (Table 1).
 |
Table 1 Subject Characteristics |
Self-Consent versus Proxy-Acquired Consent in a Long-Term Care Facility
The majority of cognitively capable residents enrolled in this study (69%, 41/59), compared to only 27% of residents consented by their medical decision maker (19/70). Self-consent rates were significantly higher than proxy-acquired consent rates (χ2=23.08, P<0.0001).
Spasticity Prevalence, History and Prior Treatment
The reference standard neurologist determined that spasticity was present in 35% of the study population (17/49; Table 1). Subjects with spasticity had Modified Ashworth Scale ratings of 1+ (4/17), 2 (6/17), 3 (2/17), and 4 (5/17; Table 2). Among the subjects diagnosed with spasticity in this study, 53% had prior evidence of spasticity in the medical record (9/17), but only one out of four subjects with a known diagnosis of spasticity was receiving any treatment (4/17). Three subjects were prescribed baclofen and one was receiving physical and occupational therapy. The reference standard neurologist recommended treatment for 65% of subjects with spasticity (11/17; Table 2), but only half of those subjects (6/11) had prior evidence of spasticity in the medical record and only two were actively being treated. Overall, the majority of subjects diagnosed with spasticity in this study who would be expected to benefit from treatment were not actively being treated (82%, 9/11).
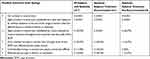 |
Table 2 Modified Ashworth Scale Ratings |
History of Central Nervous System Illness or Injury
Nearly half of all long-term care residents studied had a history of a CNS process that may be associated with spasticity (24/49, spasticity absent n=7; spasticity present n=17). Twenty-one percent of residents without spasticity had a history of CNS conditions: stroke (5/32), TBI (1/32), spinal stenosis (1/32), and both spinal cord injury and stroke (1/32). As expected, the majority of residents with spasticity had a history of CNS conditions associated with spasticity (11/17, 65%): stroke (11/17) and both spinal stenosis and stroke (1/17). Six participants who received a spasticity diagnosis had no documented neurological conditions in the medical record that were likely to have caused spasticity (6/17; 35%). Nearly half of subjects recommended to receive spasticity treatment had no prior history of a neurological condition likely to have caused spasticity (5/11; 45%).
Bedside Referral Tool
Estimates of sensitivity, specificity, AUC, pre-test probability, post-test probability, positive likelihood ratio, and negative likelihood ratio for each primary care provider who used the referral tool are shown in Table 3. Receiver operating characteristic curves of the referral tool used by the PCP and NP are shown in Figure 2. Fagan’s nomograms shown in Supplementary Figure 1 illustrate the post-test probabilities of using this bedside tool for spasticity referral.
 |
Table 3 Spasticity Referral Tool Performance |
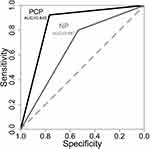 |
Figure 2 Receiver operating characteristic curves for the bedside spasticity referral tool. PCP optimism-corrected AUC=0.844; NP optimism-corrected AUC=0.660. |
Primary Care Physician
The spasticity prevalence among subjects evaluated by both the reference standard and the primary care physician was 30% (pre-test probability). When used by the PCP, the bedside tool had 92% sensitivity and 78% specificity (Figure 2; Table 3; AUC=0.845, optimism-corrected AUC=0.844). After receiving a recommendation for referral by the primary care physician using the bedside tool, subjects with spasticity were 4 times more likely to be referred than subjects without spasticity (Table 3; Supplementary Figure 1). This corresponds to a 63% prevalence of spasticity among those referred (post-test probability). Similarly, subjects with spasticity were 0.1 times as likely to be missed for referral, which translates to only a 4% chance of having spasticity if not determined to need a referral.
Nurse Practitioner
Spasticity was present in 33% of subjects evaluated by both the nurse practitioner and reference standard (pre-test probability). Sensitivity and specificity were 80% and 53%, respectively, when the NP used the referral tool (Figure 2; Table 3; AUC=0.667, optimism-corrected AUC=0.660). A referral for spasticity consultation after using the bedside tool was 1.7 times more likely in subjects with spasticity than subjects without, which corresponds to a spasticity prevalence among those referred by the NP of 46% (post-test probability; Supplementary Figure 1). Subjects with spasticity were 0.4 times as likely to be missed for referral, corresponding to a spasticity prevalence in subjects not referred by the NP of 16%.
Time to Complete the Bedside Spasticity Referral Tool Examination
Mean time estimated to complete the bedside exam using the referral tool was 3 mins (3.1±1.2 mins). The shortest examination was estimated to be 1.5 mins (1.5 ± 0.6 mins), and the longest examination was estimated to be 6 mins (6.0 ± 2.6 mins).
Missed Referrals
There were four missed referrals between the two primary care providers who used the bedside tool. The PCP missed one referral for a subject who was recommended for spasticity treatment and had a Modified Ashworth Rating of 4. The NP missed three referrals: two subjects were not recommended for spasticity treatment who had Modified Ashworth Ratings of 1+ and one subject was recommended for treatment who had a Modified Ashworth Rating of 2.
There will be no further data shared, results can be seen by visiting ClinicalTrials.gov Identifier: NCT03209960.
Discussion
To address the critical need for improved spasticity screening, diagnosis, and treatment in the long-term care setting, a simple bedside screening tool was developed to be used by primary care providers to initiate a referral for more specialized evaluation. This one-page flowchart guided a brief physical examination at the bedside and demonstrated high sensitivity to correctly identify residents that would benefit from spasticity referral to a specialist for further evaluation. Furthermore, the specificity of this referral tool is consistent with screening assessments for other diseases,18,19 and spasticity prevalence was extremely low in subjects not recommended for referral using this bedside tool.
Clinical scales currently used for spasticity assessment are not well suited for screening in the primary care setting, as they must be administered by subspecialty-trained clinicians.14,20 Likewise, biomechanical and electrophysiological methods of spasticity measurement have limited clinical usefulness20 and are not suitable for use as screening tools. At present, there are no instruments available specifically designed to screen for the presence of spasticity in patients who have not yet received a diagnosis.21 Our results further establish the urgent need for a simple assessment like the one used in this study: half of the subjects with spasticity had no prior evidence of a diagnosis in the medical record, and four out of five subjects who would likely benefit from available therapies were not receiving any treatment. This finding is in line with prior research, which indicates that spasticity is under-diagnosed in the long-term care setting,1–3 despite the availability of multiple scales for spasticity measurement.14,15,22
Developing better screening assessments for spasticity is an area of active investigation, with a patient-reported tool recently introduced.21 The screening referral tool presented in this study fits before such a patient-reported treatment needs assessment, such that long-term care providers without subspecialty training in spasticity could implement this simple exam to identify at-risk residents. This referral tool is, therefore, only an initial part of the diagnostic algorithm, with subsequent multidisciplinary collaboration with physiatrists or movement disorders experts remaining critical to successful diagnosis and treatment. While treatment is not recommended for all people with spasticity8 and spasticity can actually improve functional abilities (ie, standing transfers) for some affected individuals,8,23,24 many people with spasticity are likely to benefit from available treatments.21 Importantly, more than one-third of subjects determined to have spasticity in this study did not have a recorded history of CNS illness or injury likely to have caused spasticity. This finding highlights the importance of screening all long-term care residents for the presence of spasticity, not only those with a well-documented history of a neurological condition associated with spasticity.
This study’s high sensitivity and moderate specificity are consistent with other screening assessments.18,19 Unlike diagnostic tests that require high specificity to minimize false positives, screening tests strive for high sensitivity to ensure as few cases of the condition are missed as possible.25 In this study, pre- and post-test probabilities estimated were derived from the true prevalence of spasticity in the cohort which was determined by the reference standard examination as part of the study protocol. Therefore, it is important to note that the true value of this bedside referral tool is likely underestimated using these metrics, because nearly half of subjects determined to have spasticity by the reference standard as part of this research study had no prior evidence of the condition in their medical record.
Study Limitations
This pilot study was conducted at a single long-term care facility, which reduces the generalizability of these results in other settings. The brief physical exam guided by this referral tool has the potential to identify signs of spasticity in other populations, but future studies are needed to understand the utility of this screening assessment in different health care settings. Performance varied between providers, with the primary care physician making the correct referral decision for more subjects than the nurse practitioner. It is unclear whether this is due to differences in clinical training or simply a result of the variability of performance of this bedside tool across providers. A larger study with multiple primary care providers is needed to understand potential differences between primary care physicians and nurse practitioners using this referral tool. This screening tool was designed to identify people who may have spasticity. It is, therefore, unable to discern between spasticity versus contractures, a determination that would be provided at a subsequent specialist evaluation. Without a biomarker or objective diagnostic method available, this study relied on the current diagnostic criteria for spasticity to serve as the reference standard: a clinical conclusion by a movement disorders expert after a physical and neurological examination.
Spasticity affects long-term care residents of all cognitive abilities, and all residents at the facility were therefore approached to participate in this study. However, similar to a prior study in the long-term care setting,2 there was a significantly lower proportion of subjects who enrolled when a medical decision maker was required for informed consent compared to subjects who provided self-consent. This selection bias is noted as a limitation of this study. Efforts were made in this investigation to improve proxy-acquired consent rates by also approaching medical decision makers available at the facility, in addition to mailing study information and informed consent packets. This additional effort nearly doubled the proportion of proxy-acquired consent for this study (27%) compared to the prior investigation (14%).2 Nevertheless, clinical research enrollment remains challenging in the long-term care setting,26 and additional research is needed to further enhance the inclusion of cognitively impaired residents to adequately represent this population and show the full impact of this referral tool as a screening assessment in long-term care settings.
This referral tool was developed to be used by primary care providers without prior knowledge of spasticity and without requiring extensive training of personnel using the three-question flowchart. In this study, the referral tool was used without providing any training to the primary care providers, which yielded very encouraging referral results after only minutes of use. Future studies could, therefore, explore whether the addition of a brief written introduction on the flowchart improves performance.
Conclusions
This simple bedside screening tool demonstrated high sensitivity for primary care providers to correctly refer residents of a long-term care facility with spasticity for further diagnostic evaluation. These data suggest that a brief physical exam guided by a simple, one-page flowchart could be used in the long-term care setting to identify residents who would likely benefit from referral to a physiatrist or a movement disorders specialist for evaluation and subsequent treatment of spasticity. Given the critical need to improve the diagnosis of spasticity, these results strongly warrant a validation study to understand the utility and impact of this bedside referral tool across multiple long-term care facilities and various types of care providers in this setting.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
This work was supported by Ipsen Biopharmaceuticals, Inc. Ipsen had no input into study design, data collection, analysis, or interpretation or writing of the manuscript.
Disclosure
Vanderbilt University receives income from grants or contracts Allergan, Ipsen, Medtronic, Merz, Pharma Two B, and Voyager for research or educational programs led by Dr. David Charles. Dr. Charles receives income from Allergan, Ipsen, Revance, and USWorldMeds for consulting services. Dr David Charles also reports grants from Medtronic, Merz, Pharma Two B, and Voyager, grants, personal fees from Revance, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Pfister AA, Roberts AG, Taylor HM, Noel-Spaudling S, Damian MM, Charles PD. Spasticity in adults living in a developmental center. Arch Phys Med Rehabil. 2003;84(12):1808. doi:10.1016/s0003-9993(03)00368-x.
2. Turchan M, Hudson TS, Gill CE, et al. The prevalence of spasticity in veterans living in a long-term care facility. Int J Neurol Neurother. 2017;3(5):2–5. doi:10.23937/2378-3001/3/5/1056
3. Gill CE, Hacker ML, Meystedt J, et al. Prevalence of spasticity in nursing home residents. J Am Med Dir Assoc. 2020;In Press. doi:10.1016/j.jamda.2020.01.005
4. Pandyan AD, Gregoric M, Barnes MP, et al. Spasticity: clinical perceptions, neurological realities and meaningful measurement. Disabil Rehabil. 2005;27(1–2):2–6. doi:10.1080/09638280400014576
5. Pattuwage L, Olver J, Martin C, et al. Management of spasticity in moderate and severe traumatic brain injury. J Head Trauma Rehabil. 2017;32(2):E1–E12. doi:10.1097/HTR.0000000000000234
6. Sommerfeld DK, Eek EU-B, Svensson A-K, Holmqvist LW, von Arbin MH. Spasticity after stroke. Stroke. 2004;35(1):134–140. doi:10.2165/00002512-199609050-00004
7. Ganapathy V, Graham GD, Dibonaventura MD, Gillard PJ, Goren A, Zorowitz RD. Caregiver burden, productivity loss, and indirect costs associated with caring for patients with poststroke spasticity. Clin Interv Aging. 2015. doi:10.2147/CIA.S91123
8. Milligan J, Ryan K, Lee J. Demystifying spasticity in primary care. Can Fam Physician. 2019;65(10):697–703.
9. Harris-Kojetin L, Sengupta M, Park-Lee E, et al. Long-Term Care Providers and Services Users in the United States: Data from the National Study of Long-Term Care Providers, 2013–2014. Vital Health Stat. 2016;3:1–105. Available from : https://permanent.access.gpo.gov/gpo116380/sr03_038.pdf.
10. Oliver M, Inaba K, Tang A, et al. The changing epidemiology of spinal trauma: a 13-year review from a level i trauma centre. Injury. 2012;43(8):1296–1300. doi:10.1016/j.injury.2012.04.021
11. Shih LC, Tarsy D, Okun MS. The current state and needs of north american movement disorders fellowship programs. Parkinsons Dis. 2013;2013. doi: 10.1155/2013/701426.
12. Sayce L, Hudson T, Heusinkveld LE, Currie AD, Hacker ML, Charles D. Spasticity diagnosis and treatment in the United States-a priority for our aging population. Int J Neurorehabilitation. 2016;3(3). doi:10.4172/2376-0281.1000216
13. Hudson T, Turchan M, Gill C, et al. Inter-rater reliability of a novel spasticity diagnostic algorithm. Tennessee Med E J. 2018;3(3).
14. Johnson GR. Outcome measures of spasticity. Eur J Neurol Suppl. 2002;9(1):10–16. doi:10.1046/j.1468-1331.2002.0090s1010.x
15. Hsieh JTC, Wolfe DL, Miller WC, Curt A. Spasticity outcome measures in spinal cord injury: psychometric properties and clinical utility. Spinal Cord. 2008;46(2):86–95. doi:10.1038/sj.sc.3102125
16. Moons KGM, Donders ART, Steyerberg EW, Harrell FE. Penalized maximum likelihood estimation to directly adjust diagnostic and prognostic prediction models for overoptimism: a clinical example. J Clin Epidemiol. 2004;57(12):1262–1270. doi:10.1016/j.jclinepi.2004.01.020
17. Akobeng AK. Understanding diagnostic tests 2: likelihood ratios, pre- and post-test probabilities and their use in clinical practice. Acta Paediatr Int J Paediatr. 2007;96(4):487–491. doi:10.1111/j.1651-2227.2006.00179.x
18. Ashton-Prolla P, Giacomazzi J, Schmidt AV, et al. Development and validation of a simple questionnaire for the identification of hereditary breast cancer in primary care. BMC Cancer. 2009;9(1):283. doi:10.1186/1471-2407-9-283
19. Sieper J, Srinivasan S, Zamani O, et al. Comparison of two referral strategies for diagnosis of axial spondyloarthritis: the Recognising and Diagnosing Ankylosing Spondylitis Reliably (RADAR) study. Ann Rheum Dis. 2013;72(10):1621–1627. doi:10.1136/annrheumdis-2012-201777
20. Biering-Sørensen F, Nielsen JB, Klinge K. Spasticity-assessment: A review. Spinal Cord. 2006;44(12):708–722. doi:10.1038/sj.sc.3101928
21. Zorowitz RD, Wein TH, Dunning K, et al. A screening tool to identify Spasticity in need of treatment. Am J Phys Med Rehabil. 2017;96(5):315–320. doi:10.1097/PHM.0000000000000605
22. Pierson SH. Outcome measures in spasticity management. Muscle Nerve Suppl. 1997;6:36–60. doi:10.1002/(sici)1097-4598(1997)6+<36::aid-mus5>3.3.co;2-e
23. Satkunam LE. Rehabilitation medicine: 3. Management of adult spasticity. CMAJ. 2003;169(11):1173–9.
24. Thompson AJ. Clinical management of spasticity. J Neurol Neurosurg Psychiatry. 2005;76(4):459. doi:10.1136/jnnp.2004.035972.
25. Goetzinger KR, Tuuli MG, Odibo AO. Statistical analysis and interpretation of prenatal diagnostic imaging studies, part 3: approach to study design. J Ultrasound Med. 2011;30(10):1415–1423. doi:10.7863/jum.2011.30.10.1415
26. Magaziner J, German P, Zimmerman SI, et al. The prevalence of dementia in a statewide sample of new nursing home admissions aged 65 and older: diagnosis by expert panel. Gerontologist. 2000;40(6):663–672. doi:10.1093/geront/40.6.663
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

