Back to Journals » Clinical Interventions in Aging » Volume 9
A longitudinal cohort study of the impact of first- and both-eye cataract surgery on falls and other injuries in Vietnam
Authors To KG, Meuleners L, Bulsara M, Fraser M, Duong DV, Do DV , Huynh VN, Phi TD, Tran HH, Nguyen ND
Received 23 January 2014
Accepted for publication 4 March 2014
Published 28 April 2014 Volume 2014:9 Pages 743—751
DOI https://doi.org/10.2147/CIA.S61224
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Kien Gia To,1,2 Lynn Meuleners,1 Max Bulsara,3 Michelle L Fraser,1 Dat Van Duong,4 Dung Van Do,2 Van-Anh Ngoc Huynh,2 Tien Duy Phi,5 Hoang Huy Tran,5 Nguyen Do Nguyen5
1Curtin Monash Accident Research Centre (C-MARC), Faculty of Health Sciences, Curtin University, Perth, WA, Australia; 2University of Medicine and Pharmacy, Ho Chi Minh City, Vietnam; 3Institute for Health Research, University of Notre Dame, Fremantle, WA, Australia; 4United Nations Population Fund, Hanoi, Vietnam; 5Eye Hospital, Ho Chi Minh City, Vietnam
Aim: Little information exists on the impact of cataract surgery on falls and other injuries in Vietnam. The aim of this study was to determine the impact of first and both eye cataract surgery on the number of falls and other injuries among bilateral cataract patients in Ho Chi Minh City, Vietnam.
Materials and methods: A longitudinal cohort study was conducted involving 413 bilateral cataract patients aged 50+ years. Participants were assessed at three time points: 1 week before, 1–3 months after, and 1 year after first-eye cataract surgery. Visual measures (visual acuity, contrast sensitivity and stereopsis) were taken, and self-reported falls and injury data were collected. A multilevel longitudinal Poisson regression model was used to investigate change in the number of falls after surgery.
Results: The risk of falls decreased by 78% (incidence-rate ratio [IRR] 0.22, 95% confidence interval [CI] 0.06–0.77; P=0.018) in the year after cataract surgery for participants who had first-eye surgery only and 83% (IRR 0.17, 95% CI 0.04–0.69; P=0.012) for participants who had the second eye operated on compared to before surgery. The risk of falls was three times higher for females than males (IRR 3.13, 95% CI 1.53–6.40; P=0.002). Improved binocular contrast sensitivity was also associated with a decrease in falls (IRR 0.40, 95% CI 0.17–0.97; P=0.042). The prevalence of other injuries also decreased after cataract surgery.
Conclusion: Cataract surgery reduced the number of falls and other injuries in Vietnam. Contrast sensitivity may be important for ophthalmologists to consider when prioritizing patients for surgery and assessing their fall risk.
Keywords: falls, injuries, cataract surgery, longitudinal, older population, Vietnam
Introduction
More than 420,000 people die each year due to a fall, ranking it the second-most common cause of injury-related mortality worldwide.1 Approximately 80% of these deaths occur in developing countries, particularly in regions of Southeast Asia and the Western Pacific.1 Half of all falls result in an injury, 10% of which are serious.2–4 The older population is the most vulnerable, with the prevalence of falls reported at 35% in those aged 65 years and older, of which 50% may experience a repeat fall within a year.1,3–5 As well as causing injuries, falls can also lead to a loss of independence, reduced mobility, social isolation, and poor quality of life.4,6
Globally, there are approximately 39 million people who are blind and 246 million people with visual impairment, mostly aged 50 years and over.7 Cataract is the leading cause of visual impairment (33%) in middle- and low-income countries,7 and approximately 80% of those with untreated cataract live in developing countries.7,8
Cataract surgery is the most common ophthalmic surgical procedure performed worldwide,9,10 and has been found to bring about significant improvements in visual function, quality of life, daily activities, and depressive symptoms.6,11,12 However, research is conflicting on whether cataract surgery reduces the risk of falls. Two randomized controlled trials (RCTs) conducted in the UK reported a 34% reduction in fall rate and 40% reduction in risk of recurrent falls after first-eye cataract surgery,11 but no significant change in falls risk after second-eye surgery.6 It should be noted that these studies included only women aged over 70 years. A significant reduction in self-reported falls was also found 6 months after cataract surgery among 97 cataract patients.13 More recently, however, an Australian population-based study reported a significant increase in falls after both first- and second-eye cataract surgery compared to baseline.14 No information exists on the impact of cataract surgery on falls in developing countries, such as Vietnam, where vision is often much poorer before surgery than in developed countries and there are different cultural and lifestyle factors (such as older people living with their adult children) that may affect fall risk.15
Conflicting information also exists regarding the impact of different visual measures on fall risk for cataract patients.16,17 Several studies have reported that poor visual acuity increases the risk of falls.18–22 However, recent research in developed countries has found that reduced contrast sensitivity and stereopsis are also important visual risk factors for falls.17,19,23–25
Currently, there is little information on the impact of cataract surgery on other types of injuries. A Canadian-based retrospective case-control study found that cataract patients had a higher risk of such injuries as burns, fractures, contusions, lacerations, and sprains compared with controls before cataract surgery, but their risk decreased to that of controls following cataract surgery.26 This study also showed that the risk of an injury (including falls) increased by 3% per week of waiting for cataract surgery.26
Vietnam is a developing country with a population of 86 million people, and 17% are aged 50 years and older.27 Cataract accounts for 65% of visual impairment28 in Vietnam, and approximately 120,000 cataract surgeries are performed every year.28 The incidence rate for injuries in Vietnam is 76/1,000 person-years in the general population, and the incidence rate for falls is estimated at 32/1,000 person-years for those aged 60 years and over.29 To date, there has been no information on the impact of cataract surgery on falls and other injuries in Vietnam. Therefore, the aim of this study was to assess the impact of first- and both-eye cataract surgery on the number of falls and other injuries in a cohort of bilateral cataract patients in Ho Chi Minh City, Vietnam.
Materials and methods
Study design and participants
A longitudinal prospective cohort study was conducted on patients with bilateral cataract who were scheduled for cataract surgery at the Eye Hospital in Ho Chi Minh City, Vietnam between July 2011 and July 2013. Inclusion criteria included a diagnosis of age-related bilateral cataract, scheduled to undergo first-eye surgery, aged 50 years or older, and living independently in the community. Exclusion criteria included previous surgery for cataract, injury- or diabetes-related cataract, a diagnosis of glaucoma or any other significant ocular diseases, a diagnosis of dementia, Parkinson’s disease, schizophrenia, or being wheelchair-bound.
All cataract surgeries were undertaken by phacoemulsification and performed one eye at a time. Patients were screened for ocular comorbidities prior to surgery. Dilated funduscopy was performed by an ophthalmologist during consultation. When funduscopy was not feasible due to dense cataract, postoperative funduscopy was done only if visual outcome was less than 6/12 (0.30 logarithm of minimum angle of resolution [logMAR]) and not improved. This study was approved by the Curtin University Human Research Ethics Committee and the executive board of the Eye Hospital in Ho Chi Minh City in Vietnam.
Data collection
Consecutive bilateral cataract patients were approached by one researcher after examination of their medical records and consultation with their treating ophthalmologist(s) as to their eligibility. They were given a participant-information sheet explaining the purpose of the study, confidentiality, and their right to withdraw from the study at any time without negative impact on their medical treatment. A consent form was signed before any data were collected.
Information was collected at three time points: a week prior to first-eye cataract surgery (baseline), 1–3 months after first/both-eye cataract surgeries (second assessment), and 1 year after each participant’s first-eye cataract surgery (third assessment). The outcome of interest was a fall that was defined as “an event which results in a person coming to rest inadvertently on the ground or floor or other lower level”.30 Information was also collected about other injuries that occurred during the study period.
Questionnaire
Eligible participants were interviewed via a researcher-administered structured questionnaire at each of the three assessments. For the baseline and second assessments, the questionnaire was administered face to face, and the third assessment took place via a telephone interview. The questionnaire was translated into Vietnamese and back-translated into English by two independent translators. Information on the assessment of the test–retest repeatability of this questionnaire has been published elsewhere.31 Demographic, social, and health information collected at baseline included sex, age, ethnicity, marital status, living situation, education level, employment status, refractive management, use of prescribed medications, and presence of comorbid conditions. Comorbid conditions included hypertension, cancer, stroke, angina, rheumatoid arthritis, kidney disease, hearing loss, alcohol abuse, sleep apnea, hypertension, diabetes, and other chronic conditions. Information on changes to social and health-related circumstances was collected at the second and third assessment. Information was also collected regarding quality of life and depressive symptoms at the baseline and second assessments. These results are reported elsewhere.32,33
Self-reported falls and other injury data were collected via the questionnaire, which can be obtained from the author. At baseline, participants were asked how many times they had fallen and landed on the floor or ground in the previous 12 months. At the second and third assessments, they reported how many times they had fallen since their last interview. Participants were also asked to describe any nonfall-related injuries they received, eg, burns, fractures, contusions, sprains, lacerations, or motor vehicle-related injuries.
Objective visual measures
Three objective measures of vision were administered by the researcher at the baseline and second assessments according to the hospital protocols and under the guidance of the hospital’s ophthalmologists. As the third assessment was conducted by telephone, no visual tests were performed. However, it was expected that there would be minimal change in vision since the second assessment. Visual measures examined included visual acuity, contrast sensitivity, and stereopsis.
Participants wore their current corrective lenses for visual testing. Visual acuity (better eye, worse eye, and binocular with current lens correction) was measured using a Snellen chart provided by the Eye Hospital, calibrated at a 5 m distance.34,35 Scores were expressed on a logMAR scale. Contrast sensitivity (better eye, worse eye, and binocular with current lens correction) was measured using a Pelli–Robson chart and measured in log units.36 Due to correlation between measures, only binocular measures of visual acuity and contrast sensitivity were used for this analysis. Stereopsis was assessed by the Titmus Fly StereoTest (Stereo Optical Co. Inc. Chicago, IL, USA),37 which measured disparity from 1.602 to 3.551 log seconds of arc.
Statistical methods
Descriptive analyses for the cohort were undertaken, and the prevalence of falls and other injuries calculated for the year before and after first-eye surgery. As the number of falls was considered to be count data, a multilevel longitudinal Poisson regression model was undertaken to compare the number of falls during the year before and the year after first-eye cataract surgery. The multilevel Poisson model uses the number of falls as the outcome of interest, but accounts for those who have had more than one fall in the analysis. The longitudinal nature of the observations renders the application of standard Poisson regression analysis inappropriate. Multilevel modeling is appropriate for analyzing clustered and longitudinal data. Failure to account for this may give rise to misleading results including aggregation bias and model misspecification due to lack of independence between measurements at different times.38,39
For the multilevel model, the hierarchy was defined as level 1 (the repeated measurements), nested within the level 2 unit (the individual subject). This approach allows for the portioning of variance and covariance between each of the levels. This variation may be accounted for by explanatory variables. Multilevel modeling also allows for the use of unbalanced data.
Each variable was added to the base model as a fixed effect to explain fall variation between individuals and the change in falls within each person over time. Explanatory variables included in the model at level 2 were age, sex, education level, marital status, living situation (alone: no/yes), ethnicity, taking prescription medications (no/yes), comorbid medical conditions including other eye conditions (no/yes), binocular visual acuity, binocular contrast sensitivity, and stereopsis. Refractive management was not included in the model, due to the large number of missing values. Another three-level variable was added to specify whether a participant had first-eye cataract surgery only or both eyes operated on during the 1-year follow-up period compared to before cataract surgery. The test for linear hypothesis after model estimation was undertaken to see if there was a statistical difference between the number of falls after first-eye compared to the number of falls after second-eye surgery.
Unfortunately, the sample size was too small to undertake multivariate modeling for nonfall-related injuries. All analyses were performed using Stata 12 (StataCorp, College Station, TX, USA) at the 5% significance level.
Results
A total of 434 patients with bilateral cataract were approached by the researcher, of whom eleven patients refused to participate and ten were ineligible. The sample at baseline was 413 patients. A total of 247 participants completed the second assessment (dropout rate 40.2%), and 312 completed the third assessment (telephone interview), with 238 completing all three assessments. Of the 312 cataract patients who completed the third assessment, 119 had first-eye surgery only and 193 had both eyes operated on by the 12-month telephone follow-up. There were no statistically significant differences between those who did and did not complete all three assessments in terms of sex (P=0.18), age (P=0.09), and other variables.
Table 1 presents the demographic characteristics of the cohort. At baseline, the mean age of the 413 participants was 66.6 years (standard deviation [SD] 7.9), ranging from 50 to 88 years. The majority of participants were female (n=268, 64.9%), aged between 60 and 69 years (n=170, 41.2%), were married (n=239, 57.8%), were of Kinh ethnicity (n=401, 97.1%), lived with family (n=383, 92.7%), had junior high school level education (n=303, 73.4%), did not take any prescription medications (n=250, 60.5%), and reported at least one comorbidity (n=268, 64.9%). Demographic characteristics of the participants who completed the second and third assessments were very similar (Table 1).
  | Table 1 Demographic characteristics of bilateral cataract patients before, 1–3 months after, and 1 year after cataract surgery by fall status, Ho Chi Minh City, Vietnam |
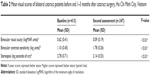
Table 2 presents participants’ visual characteristics before and after cataract surgery. Mean binocular visual acuity was 0.62 logMAR (SD 0.41) before surgery for the baseline cohort of 413 participants. After surgery, visual acuity improved to 0.09 logMAR (SD 0.19) for the 247 participants who completed the second assessment. A change of 0.1 logMAR units is commonly considered to be clinically meaningful.40
Mean binocular contrast sensitivity was 1.10 log units (SD 0.45) before surgery (n=413), and improved to 1.78 log units (SD 0.26) after surgery (n=247). A change of 0.3 log units or one line on the chart is considered to be clinically meaningful.41 Before surgery, mean stereopsis was 2.78 log seconds of arc (SD 0.71, n=413), and improved to 2.14 log seconds of arc (SD 0.53) after surgery. A change in stereopsis of 0.3 log seconds of arc is often defined as clinically meaningful.42
The prevalence of falls was 12.8% (53 of 413) in the year before first-eye cataract surgery. Forty-seven participants fell once, five fell twice, and one fell three times. Only four participants experienced a total of four falls between the baseline assessment and the second assessment. In the year after first-eye cataract surgery, the prevalence of falls was 10.9% (13 of 119) among those who had first-eye surgery only and 6.7% (13 of 193) among those who had both eyes operated on during the follow-up period. Only two participants fell more than once after surgery.
The prevalence of nonfall-related injuries was 5.6% (23 of 413) in the year before first-eye cataract surgery. Of the 23 injuries reported at baseline, 17 (73.9%) were due to motor vehicle crashes, three (13.0%) were burns, two (8.7%) contusions, and one (4.4%) sprain. In the year after first-eye cataract surgery, the prevalence of injuries was 3.4% (four of 119) among those who had first-eye surgery only, and 4.7% (nine of 193) among those who had both eyes operated on during the follow-up period. Of the 14 injuries involving 13 participants after surgery, four (28.6%) were due to motor vehicle crashes, four (28.6%) were contusions, four (28.6%) burns, and two (14.3%) fractures.
The results of the multilevel longitudinal Poisson regression model examining change in the number of falls after cataract surgery are presented in Table 3. After adjusting for potential confounding variables, the risk of falls decreased by 78% (incidence-rate ratio [IRR] 0.22, 95% confidence interval [CI] 0.06–0.77; P=0.018) in the year after cataract surgery for participants who had first-eye surgery only, and 83% (IRR 0.17, 95% CI 0.04–0.69; P=0.01) for participants who had both eyes operated on, compared to the year before surgery. The risk of falls was three times higher for females than males (IRR 3.13, 95% CI 1.53–6.40; P=0.002). In addition, for every 1-log unit increase (improvement) in binocular contrast sensitivity, the risk of falls decreased by 60% (IRR 0.40, 95% CI 0.17–0.97; P=0.04). There was no association between age, binocular visual acuity, stereopsis, education level, ethnicity, marital status, living situation, medication use, or comorbid conditions and risk of falls. An examination of the difference in the number of falls after first eye surgery and after second eye surgery revealed no significant difference (P=0.6337).
Discussion
This is the first longitudinal study to assess the impact of first- and both-eye cataract surgery on the number of falls and injuries in Vietnam. The study found a significant decrease in the number of falls 1 year after surgery of 78% for bilateral cataract patients who had first-eye surgery only and 83% for those who had both eyes operated on compared to the year before surgery.
The prevalence of falls was lower than previously reported in studies from developed countries, despite poor vision.11 However, a systematic review of 21 studies conducted in Asian countries reported the incidence of falls to be approximately half that of Caucasian populations, with a median of 18%.43 It should be noted that the participants in these studies were older than in the current study. While the reasons behind the lower prevalence of falls in the current study require further investigation, possible explanations include the younger age of participants, social environment and customs (adult children living with and caring for their older parents), better lower-limb strength, fewer high-risk behaviors, and differing activity patterns that reduce exposure to falls.43 It is also possible that the lower prevalence reported could be due to underreporting of falls and recall bias in the study questionnaire. The prevalence of nonfall-related injuries was small among this Vietnamese cohort, but also decreased following surgery. Unfortunately, the sample size was not large enough to undertake multivariate modeling for nonfall-related injuries.
Previous research has produced conflicting results on the impact of cataract surgery on falls. An RCT of expedited versus routine cataract surgery undertaken in the UK found that first-eye cataract surgery reduced the number of falls;11 however, it found no benefit for expedited second-eye cataract surgery in women aged over 70 years.6 A study by Brannan et al found that cataract surgery reduced the risk of falls;13 however, the sample size of this study was small, and only assessed the change in falls 6 months before and 6 months after surgery. Moreover, it was not specified whether the participants in this study had first- or second-eye cataract surgery. In contrast, a retrospective population-based study using administrative health-linked data found that the rate of hospital admissions due to a fall increased 1 year after surgery compared to the year before.14 However, the study was not able to control for possible confounders, including visual measurements, and only examined more severe falls. In contrast, a prospective study found that cataract surgery had no impact on falls for an independently living older population.44 However, participants who had one- and both-eye cataract surgery were combined for the analysis and the sample size was small (n=122).
The current study suggests that in Vietnam, even among a younger cohort than the UK-based RCTs, cataract surgery has significant benefits for fall prevention. The findings also suggest that for bilateral cataract patients, second-eye cataract surgery provides additional fall-prevention benefits compared to the period before surgery. However, the difference in the number of falls between first- and second-eye surgery was not statistically significant. The participants of this study had considerably poorer presurgery vision than participants of the studies described earlier, which were conducted in developed countries.11,13,44 This may have contributed to the significant reduction in falls found among this Vietnamese cohort after surgery.
This study found that the risk of falls was over three times higher for Vietnamese females than males. This elevated risk for females is consistent with previous research,45 which found that women are more likely to live on their own, possibly explaining the increased risk. The use of high-heel footwear, psychotropic drug use, and physical activity levels among women may also affect their risk for a fall; however, this information was not captured in this study.45,46 Age, comorbid conditions, and medication use have been widely reported to increase the risk of falls, but were not significantly associated with falls in the current study. This may be due to the younger age of our cohort who were aged 50+ years, with less than 1% aged 85 or older. This much older age-group has previously been found to be at a particularly elevated risk for falls.3,5,45 In addition, 65% reported a comorbid condition, and less than 40% used prescription medications at baseline. The lack of association between these variables and falls may also be due to the overall small number of falls recorded in this study.
While some previous studies have only used visual acuity when assessing the level of visual impairment, this study assessed binocular visual acuity, binocular contrast sensitivity, and stereopsis. However, only improved binocular contrast sensitivity after surgery was found to be associated with a decrease in falls. Although visual acuity is the most commonly used measure for assessing disability caused by cataract and prioritizing patients for surgery, this finding supports a growing pool of research that suggests contrast sensitivity may be a more important measure of fall risk than visual acuity.23–25 Interestingly, the current study also found no association between stereopsis and fall risk. While good evidence exists that poor stereopsis increases the risk of falls among the general older population,17 this association may not have been observed in the current study because cataract causes more impairment to contrast sensitivity than stereopsis. It should also be noted that anisometropia (a condition in which the two eyes have unequal refractive power) may have been present in participants in this study while they waited for their second-eye surgery. This difference between eyes can affect binocular vision, and may have more effect on fall risk than stereopsis. Further research is warranted.
This study has limitations. Firstly, fall and injury data were self-reported, and may have been affected by recall bias.47 The gold standard for collection of fall data involves fall diaries with frequent reporting intervals. Therefore, while the results of this study provide preliminary information on the impact of cataract surgery on falls in Vietnam, further research using more precise methods should be undertaken. In addition, the interviewer was not masked to the operative status of the patients, which may have introduced bias. While every attempt was made to confirm a fall with family members and relatives, this may have resulted in an underestimate of the number of falls. Moreover, we were not able to collect the exact date of the fall at the 1-year follow-up assessment, because the majority of the population could not recall the date. This study did not collect information on other medical interventions or lifestyle changes that may account for a change in fall risk in the 12 months after cataract surgery either. Also, we did not assess visual function at the 1-year follow-up assessment. It is possible that some people may have experienced a change in their visual function after the second assessment. A cognitive assessment was not conducted, and cognitive ability is a well-known confounder in research with an older population.44,48–52 A large number of participants (40%) were unable to return to the hospital to complete the second assessment, which may have increased the apparent effectiveness of cataract surgery. Refractive management, which is an important risk factor for a fall, was not included in the analysis either. A final limitation was the lack of a suitable comparison group to compare changes in falls. Nevertheless, the before-and-after nature of the study design, which used the same person as their own control, would have controlled for other interindividual differences that can confound studies.
In conclusion, this study provides preliminary evidence that first- and both-eye cataract surgery significantly reduce the number of falls and injuries in a Vietnamese population. These findings have implications for ophthalmologists and other health professionals, as they highlight the importance of cataract surgery for reducing the risk of falls and other injuries and the need to incorporate the contrast sensitivity measure when prioritizing patients for surgery and assessing their risk of falls. The contrast sensitivity measure may also allow health professionals to identify patients who would most benefit from other fall-prevention interventions.
Acknowledgment
This work was supported by a Curtin Strategic International Research Scholarship, Curtin University, Perth, WA, Australia.
Disclosure
The authors report no conflicts of interest in this work.
References
World Health Organization. Falls: fact sheet 344. 2012. Available from: http://www.who.int/mediacentre/factsheets/fs344/en. Accessed December 9, 2013. | ||
Meuleners LB, Lee AH, Haworth C. Emergency presentations by vulnerable road users: implications for injury prevention. Inj Prev. 2006;12(1):12–14. | ||
Masud T, Morris RO. Epidemiology of falls. Age Ageing. 2001;30 Suppl 4:3–7. | ||
Boyé ND, Van Lieshout EM, Van Beeck EF, Hartholt KA, Van der Cammen TJ, Patka P. The impact of falls in the elderly. Trauma. 2013;15(1):29–35. | ||
Yu PL, Qin ZH, Shi J, et al. Prevalence and related factors of falls among the elderly in an urban community of Beijing. Biomed Environ Sci. 2009;22(3):179–187. | ||
Foss AJ, Harwood RH, Osborn F, Gregson RM, Zaman A, Masud T. Falls and health status in elderly women following second eye cataract surgery: a randomised controlled trial. Age Ageing. 2006;35(1):66–71. | ||
World Health Organization. Visual impairment and blindness: fact sheet 282. 2013. Available from: http://www.who.int/mediacentre/factsheets/fs282/en. Accessed October 9, 2013. | ||
Wadud Z, Kuper H, Polack S, et al. Rapid assessment of avoidable blindness and needs assessment of cataract surgical services in Satkhira District, Bangladesh. Br J Ophthalmol. 2006;90(10):1225–1229. | ||
Briszi A, Prahs P, Hillenkamp J, Helbig H, Herrmann W. Complication rate and risk factors for intraoperative complications in resident-performed phacoemulsification surgery. Graefes Arch Clin Exp Ophthalmol. 2012;250(9):1315–1320. | ||
Minassian DC, Reidy A, Desai P, Farrow S, Vafidis G, Minassian A. The deficit in cataract surgery in England and Wales and the escalating problem of visual impairment: epidemiological modelling of the population dynamics of cataract. Br J Ophthalmol. 2000;84(1):4–8. | ||
Harwood RH, Foss AJ, Osborn F, Gregson RM, Zaman A, Masud T. Falls and health status in elderly women following first eye cataract surgery: a randomised controlled trial. Br J Ophthalmol. 2005;89(1):53–59. | ||
Lamoureux EL, Fenwick E, Pesudovs K, Tan D. The impact of cataract surgery on quality of life. Curr Opin Ophthalmol. 2011;22(1):19–27. | ||
Brannan S, Dewar C, Sen J, Clarke D, Marshall T, Murray PI. A prospective study of the rate of falls before and after cataract surgery. Brit J Ophthalmol. 2003;87(5):560–562. | ||
Meuleners LB, Lee AH, Ng JQ, Morlet N, Fraser ML. First eye cataract surgery and hospitalization from injuries due to a fall: a population-based study. J Am Geriatr Soc. 2012;60(9):1730–1733. | ||
Essue BM, Hackett ML, Mueller A, Hanh Duc NT, Phuc HT, Jan S. inVestIgating the pSychologIcal and ecONomic impAct of cataRact surgerY in Vietnam: the VISIONARY observational study protocol. BMC Ophthalmol. 2011;11:25. | ||
Dhital A, Pey T, Stanford MR. Visual loss and falls: a review. Eye. 2010;24(9):1437–1446. | ||
Salonen L, Kivelä SL. Eye diseases and impaired vision as possible risk factors for recurrent falls in the aged: a systematic review. Curr Gerontol Geriatr Res. 2012;2012:271481. | ||
Coleman AL, Stone K, Ewing SK, et al. Higher risk of multiple falls among elderly women who lose visual acuity. Ophthalmology. 2004;111(5):857–862. | ||
Ivers RQ, Norton R, Cumming RG, Butler M, Campbell AJ. Visual impairment and hip fracture. Am J Epidemiol. 2000;152(7):633–639. | ||
Klein BE, Klein R, Knudtson MD, et al. Associations of selected medications and visual function: the Beaver Dam Eye Study. Br J Ophthalmol. 2003;87(4):403–408. | ||
Kulmala J, Viljanen A, Sipila S, et al. Poor vision accompanied with other sensory impairments as a predictor of falls in older women. Age Ageing. 2009;38(2):162–167. | ||
Chew FL, Yong CK, Ayu SM, Tajunisah I. The association between various visual function tests and low fragility hip fractures among the elderly: a Malaysian experience. Age Ageing. 2010;39(2):239–245. | ||
de Boer MR, Pluijm SMF, Lips P, et al. Different aspects of visual impairment as risk factors for falls and fractures in older men and women. J Bone Miner Res. 2004;19(9):1539–1547. | ||
Lord SR, Dayhew J. Visual risk factors for falls in older people. J Am Geriatr Soc. 2001;49(5):508–515. | ||
Knudtson MD, Klein BE, Klein R. Biomarkers of aging and falling: the Beaver Dam eye study. Arch Gerontol Geriatr. 2009;49(1):22–26. | ||
De Coster C, Dik N, Bellan L. Health care utilization for injury in cataract surgery patients. Can J Ophthalmology. 2007;42(4):567–572. | ||
General Statistics Office of Vietnam. The 2009 Vietnam Population and Housing Census: Completed Results. Hanoi: General Statistics Office; 2010. | ||
Vietnam Vision Project. About us. 2013. Available from: http://www.vietnamvision.org.au/default.asp?fid=5&lang=en&lstID=1. Accessed May 18, 2013. | ||
Hang HM, Ekman R, Bach TT, Byass P, Svanström L. Community-based assessment of unintentional injuries: a pilot study in rural Vietnam. Scand J Public Health Suppl. 2003;62:38–44. | ||
Lamb SE, Jørstad-Stein EC, Hauer K, Becker C. Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. J Am Geriatr Soc. 2005;53(9):1618–1622. | ||
To KG, Meuleners L, Chen HY, et al. Assessing the test–retest repeatability of the Vietnamese version of the National Eye Institute 25-item Visual Function Questionnaire among bilateral cataract patients for a Vietnamese population. Australas J Ageing. Epub 2013 Dec 27. | ||
To KG, Meuleners LB, Fraser ML, et al. The impact of cataract surgery on vision-related quality of life for bilateral cataract patients in Ho Chi Minh City, Vietnam: a prospective study. Health Qual Life Outcomes. 2014;12(1):16. | ||
To KG, Meuleners LB, Fraser ML, et al. The impact of cataract surgery on depressive symptoms for bilateral cataract patients in Ho Chi Minh City, Vietnam. Int Psychogeriatr. 2014;26(2):307–313. | ||
Ferris FL 3rd, Kassoff A, Bresnick GH, Bailey I. New visual acuity charts for clinical research. Am J Ophthalmol. 1982;94(1):91–96. | ||
Holladay JT. Proper method for calculating average visual acuity. J Refract Surg. 1997;13(4):388–391. | ||
Pelli DG, Robson GJ, Wilkins AJ. The design of a new letter chart for measuring contrast sensitivity. Clin Vis Sci. 1988;2(3):187–199. | ||
Stereo Optical. Stereo Fly Test: Instructions for the StereoTests. Chicago: Stereo Optical; 2009. | ||
Heck S, Thomas S. An Introduction to Multilevel Modeling Techniques. Mahwah (NJ): Lawrence Erlbaum; 2000. | ||
Rowe K. Mutilevel Structural Equation Modeling with Mln/Mlwin and Lisrel: An Integrated Course. 3rd ed. Canberra: Australian National University; 2000. | ||
Elliott DB, Sheridan M. The use of accurate visual acuity measurements in clinical anti-cataract formulation trials. Ophthal Physiol Opt. 1988;8(4):397–401. | ||
Elliott DB, Sanderson K, Conkey A. The reliability of the Pelli–Robson contrast sensitivity chart. Ophthal Physiol Opt. 1990;10(1):21–24. | ||
Rubin GS, Bandeen-Roche K, Huang GH, et al. The association of multiple visual impairments with self-reported visual disability: SEE project. Invest Ophthalmol Vis Sci. 2001;42(1):64–72. | ||
Kwan MM, Close JC, Wong AK, Lord SR. Falls incidence, risk factors, and consequences in Chinese older people: a systematic review. J Am Geriatr Soc. 2011;59(3):536–543. | ||
McGwin G Jr, Gewant HD, Modjarrad K, Hall TA, Owsley C. Effect of cataract surgery on falls and mobility in independently living older adults. J Am Geriatr Soc. 2006;54(7):1089–1094. | ||
Deandrea S, Lucenteforte E, Bravi F, Foschi R, La Vecchia C, Negri E. Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology. 2010;21(5):658–668. | ||
Campbell AJ, Spears GF, Borrie MJ. Examination by logistic regression modelling of the variables which increase the relative risk of elderly women falling compared to elderly men. J Clin Epidemiol. 1990;43(12):1415–1420. | ||
Cummings SR, Nevitt MC, Kidd S. Forgetting falls. The limited accuracy of recall of falls in the elderly. J Am Geriatr Soc. 1988;36(7):613–616. | ||
Ishii K, Kabata T, Oshika T. The impact of cataract surgery on cognitive impairment and depressive mental status in elderly patients. Am J Ophthalmol. 2008;146(3):404–409. | ||
McGwin G, Li J, McNeal S, Owsley C. The impact of cataract surgery on depression among older adults. Ophthalmic Epidemiol. 2003;10(5):303–313. | ||
Gray CS, Karimova G, Hildreth AJ, Crabtree L, Allen D, O’Connell JE. Recovery of visual and functional disability following cataract surgery in older people: Sunderland Cataract Study. J Cataract Refract Surg. 2006;32(1):60–66. | ||
Datta S, Foss AJE, Grainge MJ, et al. The importance of acuity, stereopsis, and contrast sensitivity for health-related quality of life in elderly women with cataracts. Invest Ophthalmol Vis Sci. 2008;49(1):1–6. | ||
Walker JG, Anstey KJ, Hennessy MP, Lord SR, von Sanden C. The impact of cataract surgery on visual functioning, vision-related disability and psychological distress: a randomized controlled trial. Clin Experiment Ophthalmol. 2006;34(8):734–742. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.