Back to Journals » Open Access Rheumatology: Research and Reviews » Volume 14
From Symptoms to Diagnosis: An Observational Study of the Journey of SLE Patients in Saudi Arabia
Authors Karremah MF , Hassan RY , Faloudah AZ, Alharbi LK, Shodari AF, Rahbeeni AA, Alharazi NK, Binjabi AZ, Cheikh MM , Manasfi H, Abdulaziz S , Hussein AH, Alhazmi A, Almoallim HM
Received 17 February 2022
Accepted for publication 26 May 2022
Published 29 June 2022 Volume 2022:14 Pages 103—111
DOI https://doi.org/10.2147/OARRR.S362833
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Chuan-Ju Liu
Mishal F Karremah,1 Rola Y Hassan,2,3 Ammar Z Faloudah,1 Lujain K Alharbi,4 Albraa F Shodari,1 Ahmad A Rahbeeni,1 Nouf K Alharazi,1 Ahmad Z Binjabi,1 Mohamed M Cheikh,3,5 Hanadi Manasfi,6 Sultana Abdulaziz,7 Albadr Hamza Hussein,4 Ahmed Alhazmi,2 Hani Almoallim1,3,8
1Department of Medicine, College of Medicine, Umm Alqura University, Makkah, Saudi Arabia; 2Department of Medicine, Division of Rheumatology, King Fahad Armed Forces Hospital, Jeddah, Saudi Arabia; 3Alzaidi Chair of Research in Rheumatic Diseases, Umm Alqura University, Makkah, Saudi Arabia; 4Department of Medicine, Division of Rheumatology, King Fahad Hospital, Madinah, Saudi Arabia; 5Department of Medicine, College of Medicine, Fakeeh College for Medical Sciences, Jeddah, Saudi Arabia; 6Department of Medicine, Specialized Medical Center, Riyadh, Saudi Arabia; 7Department of Medicine, King Fahad General Hospital, Jeddah, Saudi Arabia; 8Department of Medicine, Dr. Sameer Abbas Hospital, Jeddah, Saudi Arabia
Correspondence: Hani Almoallim, Tel +966505703935, Email [email protected]
Background and Objectives: Early diagnosis and treatment is associated with improved outcomes in patients with systemic lupus erythematosus (SLE). Studying the journey of SLE patients in Saudi Arabia is essential to direct future health-care plans.
Patients and Methods: This is a cross-sectional, multicenter study. Eligibility criteria included a diagnosis of SLE that was confirmed by a rheumatologist. Patients younger than 18 at the time of interview were excluded. Primary objectives were to determine time from first symptoms to initial physician visit (Lag 1), time from initial physician visit to encounter with rheumatologist (Lag 2), time from first visit to a rheumatologist to diagnosis of SLE (Lag 3), and time from diagnosis to start of treatment (Lag 4). Secondary objectives were to determine the number and specialty of physicians seen by patients, the speciality type that confirmed the diagnosis, first symptoms experienced, and age at first diagnosis of SLE.
Results: Three hundred patients (92.3% women) with SLE were evaluated. Mean age at diagnosis was 29.92 years. Mean disease duration was 8.1 years. The majority were college educated (43.0%). The most common initial symptom was joint pain (68%), followed by skin rash (23%), and fever (3.7%). Lag 1 was less than one month in 68.2% of patients. Lag 2 was less than one month in 33.4% of patients and exceeded one year in 25.8%. Lag 3 was less than 1 month in 68.7% of patients. Lag 4 was less than one month in 94.4% of patients. The diagnosis of SLE was made most frequently by rheumatologists (80%). Evaluation by primary care, orthopedic and dermatology physicians were associated with delays in diagnosis.
Conclusion: Delay was marked in Lag 2. Causes of delay included evaluation by non-specialists and visiting higher numbers of physicians before diagnosis confirmation.
Keywords: systemic lupus erythematosus, rheumatology, delay, Saudi Arabia, physician
Introduction
Systemic lupus erythematosus (SLE) is an autoimmune disease with variable clinical presentations ranging from simple mucocutaneous manifestations to devastating life-threatening conditions. A relapsing-remitting pattern of disease symptoms is most commonly found, which contributes to difficulties in diagnosis and management.1,2 Affected patients often have multiple comorbidities, leading to adverse effects on health-related quality of life, work efficiency, and survival, more complex medical management, expanded hospitalizations, and increased health-care costs.1,2
One of the major contributors to increased survival and better quality of life with SLE is the amount of time between disease onset and diagnosis.2 Early diagnosis and treatment of SLE is essential since organ injury in patients with SLE progresses over time, leading to a 3.5-fold increased chance of mortality, compared with the general population.3 Delays in the treatment of SLE have been associated with a worse prognosis.4
More information is needed to direct future strategic health-care plans for SLE in our country. Our aim in this study is to assess delays in SLE diagnosis and identify factors that contribute to delay.
Materials and Methods
A cross-sectional, retrospective, multicenter study was performed. Patients seen at 6 hospitals in Saudi Arabia were evaluated. King Fahad Armed Forces Hospital, King Fahad General Hospital, and Dr. Soliman Fakeeh Hospital in Jeddah, King Fahad Hospital in Madinah, and Specialized Medical Center in Riyadh. This study was approved by the institutional review board at each participating hospital and was conducted in accordance with the Declaration of Helsinki.
The primary objective of this study was to evaluate the time from the first appearance of SLE symptoms to the initial physician visit (Lag 1), the time from initial physician visit to referral to a rheumatologist (Lag 2), the time from the first visit to a rheumatologist to the diagnosis of SLE (Lag 3), and the time from the diagnosis of SLE to the start of SLE treatment (Lag 4), similar to a previous report evaluating patients with rheumatoid arthritis (RA).5 A delay in diagnosis was defined as a time period greater than 1 month in each one of the Lags. The time to diagnosis (Lag 1 plus Lag 2 plus Lag 3) was also evaluated. Delays or lags have been reported in different ways in the literature.4,6–8 We chose to report our findings as time periods that seemed most clinically relevant and that best described the gaps in medical care; <1 month, 1 to 6 months, and >6 months.
Secondary objectives were the identification of factors associated with delay in the diagnosis of SLE, identification of the physician speciality of the first physician evaluating the patient, identification of the speciality of the physician making the diagnosis of SLE, characterization of the first symptoms SLE patients experience, and determination of the age at diagnosis.
Patients
A list of SLE patients was constructed from hospital databases. Patients who refused to participate, had incomplete data in their records, or were less than 18 years of age at the time of the follow-up interview were excluded. All patients had their diagnoses of SLE confirmed by an adult rheumatologist. National identification numbers were used to avoid overlapping patients across treatment centers. Three hundred patients were included in the study.
Data Acquisition
Verbal consent was obtained from patients at the beginning of each interview. Data was collected by a trained team with a medical background (medical students and physicians) using phone interviews and a standardized questionnaire. Patients were interviewed from December, 2018 to December, 2019. The questionnaire was designed to identify delays in the diagnosis and treatment of SLE.
The questionnaire consisted of two parts, patient demographics (patient age, gender, living area and education level) and factors related to disease progression (the nature of the presenting symptoms [joint pain, stiffness, body ache, fatigue, fever, other symptoms], time between first symptoms and first visit to a physician (Lag 1), specialty of the physician that first saw the patient, specialty of the doctor that made the diagnosis of SLE, time from initial physician visit to referral to a rheumatologist (Lag 2), time from the first visit to a rheumatologist to the diagnosis of SLE (Lag 3), the time from the diagnosis of SLE to the start of SLE treatment (Lag 4), specialty of the physicians who were associated with delay, and the number of doctors visited from the first medical encounter to when a diagnosis of SLE was made).
Statistical Analysis
Data entry and statistical analysis were performed utilizing the Statistical Package for Social Sciences software, version 26. The overall sample size calculated to be appropriate for the cross-sectional study that served as the basis for the current analysis was 300 patients (95% confidence interval [CI] for p = 0.100).
Categorical variables were summarized using frequency and percentage. Continuous variables were summarized using mean and standard deviation (SD). Chi-square and Fischer exact tests were used as appropriate to test for associations between categorical variables. A Student’s t-test was used to compare two groups of continuous variables. A p value less than 0.05 was considered statistically significant.
Results
Two hundred and seventy-seven women and 23 men (12:1 female/male ratio) were interviewed (Table 1). Nineteen of the 300 (6.3%) patients were less than 18 years of age at the time of diagnosis of SLE (18.8:1 adult/child ratio). Their mean age at the time of their follow-up interview was 39.3 ± 13.1 years, 8.1 years after diagnosis. The most common presenting complaints were joint pain (68%), followed by skin rash (23%), fever (3.7%), and other miscellaneous complaints (14.7%).
 |
Table 1 Demographic Characteristics |
The patients’ initial evaluation was most commonly performed by a Primary care physician (39.7%), internist (17.3%), or rheumatologist (10.3%) (Figure 1). About one-third of patients (30.3%) were seen by two physicians and 18% were seen by five or more physicians before the diagnosis of SLE was made (Figure 2). The diagnosis of SLE was most commonly made by a rheumatologist (80%) (Figure 3).
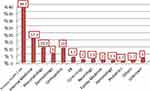 |
Figure 1 Specialty of the physician the patients first encountered. Others includes nephrology, cardiology, and ENT. Abbreviations: ER, emergency room medicine; ENT, ear, nose, and throat. |
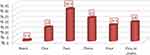 |
Figure 2 The number of physicians who assessed patients before arriving at the final diagnosis. |
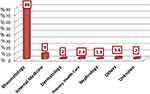 |
Figure 3 Specialty of the physician who confirmed the diagnosis of SLE. Others includes ophthalmology, hematology, ER, orthopedics and pediatrics. Abbreviation: ER, emergency room medicine. |
The time from the first appearance of symptoms to seeking initial medical care (Lag 1) was less than 1 month in about two-thirds of patients (Table 2). The time from seeking initial medical care to the first visit with a rheumatologist (Lag 2) was less than one month in 34.3% of patients, 1 to 6 months in 40.7% of patients, and more than 6 months in 25.0%. The time from the first visit with a rheumatologist to when SLE was diagnosed (Lag 3) was less than 1 month in 71.7% of patients. The time from being diagnosed with SLE to the start of treatment (Lag 4) was less than 1 month in 94.3% of patients.
 |
Table 2 Results of Lag Times and Delay Among the 300 Patients That Were Interviewed. Delay is Defined as a Time Period Greater Than 1 Month |
Delays in Lag times were evaluated (Table 2). Thirty-three percent of patients had a delay in Lag 1, 65.7% had a delay in Lag 2, 28.3% had a delay in Lag 3, and 5.7% had a delay in Lag 4. 82.3% of patients experienced a delay in the time from first symptoms of SLE to the time the correct diagnosis was made.
Factors that might affect the amount of time from first time seeking medical care to the first visit to a rheumatologist (Lag 2) were evaluated (Table 3). Differences in the specialty of the first physician seen and the number of physicians seen before making the definite diagnosis were associated with delays in Lag 2 (Table 3).
 |
Table 3 Analysis and Characteristics of Delay in Lag 2 (Time from Seeking Initial Medical Care to Visiting a Rheumatologist) |
Discussion
We have conducted a retrospective and cross-sectional analysis of the accessibility of care and speed to diagnosis and treatment that was provided to 300 SLE patients as well as the contributing factors of delays. Our main observations included a relatively short duration of access to a medical facility following appearance of symptoms (Lag 1: less than one month in two-thirds of patients), as well as the period between a visit to a rheumatologist and the confirmation of diagnosis (Lag 3: less than 1 month in 71.7% of patients) and the time between the latter’s occurrence and the start of treatment (Lag 4: less than 1 month in 94.3% of patients). The main area of delay was observed in Lag 2, which is the time from the patient’s first medical encounter to referral to a rheumatologist which was found to be less than one month in 34.3% of patients. Variables that were associated with delays in Lag 2 included the specialty of the first physician the patient encountered (orthopedics and primary care physicians were most associated with delay) and a higher number of physicians seen before making the diagnosis (Table 3).
Most patients with autoimmune disorders initially present to their local doctor, a non-specialist in a community setting. An online survey of 3022 self-reported SLE patients found that 43.6% of physicians were not sure of the diagnosis at the time of onset of SLE, 40.7% of physician made a diagnosis different from SLE, 30.5% assured the patients that nothing was wrong, and 23.6% were told it was a psychological disorder.9 72.3% of these patients saw their primary care physician to evaluate their first SLE-related complaints.9 Patients with SLE evaluated by a primary health-care physician have been reported to be misdiagnosed 75% of the time7 and rheumatologists were 3.9 times more likely to make a correct diagnosis of SLE than physicians without this specialty training.10 Only 28.3% of patients we evaluated experienced a delay in diagnosis once they were referred to a rheumatologist (Lag 3) and the majority of SLE patients (94.4%) began treatment less than 1 month after their diagnosis, when they were first seen by a rheumatologist (Lag 4).
An online survey of 827 self-reported SLE patients associated with the Lupus Foundation of America found that these patients saw a median of 3 different physicians (maximum: 10) before the correct diagnosis was made.7 Patients reported here, who were initially evaluated by primary care, orthopedic and dermatology physicians, most often had delays in obtaining a correct diagnosis. About one-third of patients we treated were seen by two physicians and 18% were seen by five or more physicians before the correct diagnosis of SLE was made. The greatest delay in patients we treated was in the time to see a rheumatologist (Lag 2), with only 33.4% of patients seen by a rheumatologist in less than one month and 25.8% not seen by a rheumatologist for more than a year after their initial clinical presentation.
The majority of SLE patients we treated sought medical advice soon after onset of their symptoms (Lag 1), with only 8.7% of patients taking more than a year to seek medical advice. This finding is of shorter duration than that of previous reports where Lag 1 varied from 13.2 to 25 months.4,7 This may be due to the easy access to medical care in urban Saudi Arabia and that there is a nationalized health-care system available for patients. The average time to diagnosis has been reported to be 15–48.2 months in Western countries, longer than that of patients we evaluated.4,8,11,12
Delays in the diagnosis of SLE are a serious health concern. Shorter times to diagnosis (less than 6 months) have been associated with significantly fewer flares, fewer hospitalizations, and lower hospital costs, compared to SLE patients with a greater than 6 month time to diagnosis.13 A longer time to diagnosis and treatment has also been associated with worse outcomes in SLE patients4,14 Earlier treatment should result in less organ damage and comorbidity accrual, mainly through quicker tapering of steroid and early use of antimalarials.3
Of 263 patients referred with a diagnosis of SLE to a rheumatology clinic, only 52.5% had their diagnosis confirmed by the specialist.10 62.8% of self-reporting SLE patients were initially misdiagnosed.7 Early correct diagnosis is associated with cost savings and lower morbidity due to the avoidance of SLE patients being misdiagnosed as not having SLE and unaffected patients being incorrectly diagnosed as having SLE.14
The frequent flares and changing disease intensity found in patients with SLE may explain why SLE patients are often misdiagnosed by primary health-care providers in Western settings.7
78.7% of physicians in this study did not make a definitive diagnosis at the first clinic visit. Every effort should be made to expedite early referrals to a rheumatologist, where the majority of our patients were diagnosed. Patients treated by a lupus specialist have less active disease, are treated with lower doses of glucocorticoids, are better treated with antimalarial agents for their SLE, have less hypertension, and have less osteoporosis, than SLE patients treated by non-specialists.3
The time from initial presentation to diagnosis in patients with SLE has decreased since the introduction of anti-nuclear antibody (ANA) testing.8 While not a specific test, ANA testing is very sensitive for SLE.1,15 Easy access to ANA testing by primary care physicians can help in the early diagnosis of SLE,1 especially when used in combination with the 2019 European League Against Rheumatism and the American College of Rheumatology criteria for SLE.16 ANA testing has been reported as positive in >90% to 95.7%6,17–19 of Saudi SLE patients.
Patients included in this study were similar in age at first clinical presentation and at the time of diagnosis as other reported Saudi SLE patients.17–19. The female:male ratio of SLE patients evaluated in this study was also similar to that of previous reports.1,18,20 It was gratifying to see that patient educational level did not relate to delay in seeing a rheumatologist.
The most common presenting symptom in our patients was joint pain (68%), consistent with other reports where arthritis and arthralgia were the most common initial symptoms.1,6,11 These findings are similar to those of previously reported Saudi SLE patients.17–19 A skin rash was found at initial presentation in 23% of our patients, less than that of other reports of Saudi SLE patients (range reported: 37. to 40.3%).6,18,19 Constitutional symptoms such as fever and fatigue were not common in our patients, in contrast to previous reports (53.1% with fatigue,6 58% with fever,18 95.7% with fever, fatigue, or malaise,17 and 50% with constitutional symptoms)11. Neuropsychiatric symptoms are noteworthy as the most common lupus-related finding leading to hospital admission, comprising 25.2% of lupus-related admissions and usually secondary to cerebrovascular events12 Neuropsychiatric symptoms at initial presentation were not common in our patients, similar to previous reports of Saudi SLE patients.17–19
Recall bias and misclassification bias are a limitation in retrospective studies like this one. Measures taken to minimize this problem included using experienced medical interviewers who referenced major national and local events to facilitate patient recollections. This type of study is also characterized by an absence of data describing potential confounding factors. Factors that could contribute to delays were identified from a literature review and previous clinical experience and reviewed in the patient interviews. The misdiagnosis rate could not be determined in these patients. The effect of patients refusing to participate in the study cannot be calculated.
Conclusion
Lag times in SLE patients in Saudi Arabia were determined. Most patients had adequate access to medical care from the time of the onset of their symptoms. The diagnosis and treatment of the majority of patients was also rapidly carried out once they were seen by a rheumatologist.
Evaluation by primary care, orthopedic and dermatology physicians as well as a higher number of physicians seen before diagnosis confirmation were the causes that were most frequently associated with delays in diagnosis. SLE specialists, rheumatologists, were the most common physician group to confirm the diagnosis of SLE. Marked delays were commonly observed in patient referral to a rheumatologist, resulting in delays in diagnosing SLE and treatment. Every effort should be made to expedite early referral to a rheumatologist in order to facilitate correct diagnosis and early treatment of SLE.
Acknowledgments
The authors would like to thank Alzaidi Chair of Research in Rheumatic Disease, Umm Alqura University, Makkah, Saudi Arabia for the support provided to have this study published.
Disclosure
The authors declare no conflict of interest. This study was funded by the Alzaidi Chair of Research Chair in Rheumatic Disease, Umm Alqura University, Makkah, Saudi Arabia.
References
1. Gergianaki I, Bertsias G. Systemic Lupus Erythematosus in primary care: an update and practical messages for the General Practitioner. Front Med. 2018;5:161. doi:10.3389/fmed.2018.00161
2. Gill JM, Quisel AM, Rocca PV, Walters DT. Diagnosis of systemic lupus erythematosus. Am Fam Physician. 2003;68(11):2179–2186.
3. Aljohani R, Gladman DD, Su J, Urowitz MB. Comparison of systemic lupus erythematosus (SLE) patients managed early after diagnosis in specialty versus community care clinics. Clin Rheumatol. 2017;36(8):1773–1778. doi:10.1007/s10067-017-3713-7
4. Kernder A, Richter JG, Fischer-Betz R, et al. Delayed diagnosis adversely affects outcome in systemic lupus erythematosus: cross sectional analysis of the LuLa cohort. Lupus. 2021;30(3):431–438. doi:10.1177/0961203320983445
5. Barhamain AS, Magliah RF, Shaheen MH, et al. The journey of rheumatoid arthritis patients: a review of reported lag times from the onset of symptoms. Open Access Rheumatol Res Rev. 2017;9:139–150. doi:10.2147/OARRR.S138830
6. Kapsala N, Flouda S, Nikolopoulos D, et al. Pos0759 the journey of patients from first symptoms to diagnosis of systemic lupus erythematosus (Sle): an observational study. Ann Rheum Dis. 2021;80(Suppl1):
7. Al Sawah S, Daly RP, Foster S, et al. SAT0423 Understanding delay in diagnosis, access to care and satisfaction with care in lupus: findings from a cross-sectional online survey in the United States. Ann Rheum Dis. 2015;74(Suppl2):812LP- 812. doi:10.1136/annrheumdis-2015-eular.1159
8. Doria A, Zen M, Canova M, et al. SLE diagnosis and treatment: when early is early. Autoimmun Rev. 2010;10(1):55–60. doi:10.1016/j.autrev.2010.08.014
9. Daly R, Partovi R, Davidson PO. Lupus diagnosis: process and patient experience [abstract]. Arthritis Rheumatol. 2017;69(Supplement 10):111.
10. Narain S, Richards HB, Satoh M, et al. Diagnostic accuracy for lupus and other systemic autoimmune diseases in the community setting. Arch Intern Med. 2004;164(22):2435–2441. doi:10.1001/archinte.164.22.2435
11. Sebastiani GD, Prevete I, Piga M, et al. Early lupus project - a multicentre Italian study on systemic lupus erythematosus of recent onset. Lupus. 2015;24(12):1276–1282. doi:10.1177/0961203315585817
12. Kapsala N, Nikolopoulos D, Flouda S, et al. Pos0757 Systemic Lupus Erythematosus (Sle) diagnosed during hospitalization: clinical phenotype and performance of the Sle Risk Probability Index (Slerpi). Ann Rheum Dis. 2021;80(Suppl1):631. doi:10.1136/annrheumdis-2021-eular.2905
13. Oglesby A, Korves C, Laliberté F, et al. Impact of early versus late systemic lupus erythematosus diagnosis on clinical and economic outcomes. Appl Health Econ Health Policy. 2014;12(2):179–190. doi:10.1007/s40258-014-0085-x
14. Clarke AE, Weinstein A, Piscitello A, et al. Evaluation of the economic benefit of earlier Systemic Lupus Erythematosus (SLE) diagnosis using a Multivariate Assay Panel (MAP). ACR Open Rheumatol. 2020;2(11):629–639. doi:10.1002/acr2.11177
15. Leuchten N, Hoyer A, Brinks R, et al. Performance of antinuclear antibodies for classifying systemic lupus erythematosus: a systematic literature review and meta-regression of diagnostic data. Arthritis Care Res. 2018;70(3):428–438. doi:10.1002/acr.23292
16. Aringer M, Costenbader K, Daikh D, et al. 2019 European League against rheumatism/American College of Rheumatology classification criteria for systemic lupus erythematosus. Arthritis Rheumatol. 2019;71(9):1400–1412. doi:10.1002/art.40930
17. Abid N, Khan AS, Otaibi A. Systemic lupus erythematosus (SLE) in the eastern region of Saudi Arabia. A comparative study. Lupus. 2013;22(14):1529–1533. doi:10.1177/0961203313500548
18. Heller T, Ahmed M, Siddiqqi A, Wallrauch C, Bahlas S. Systemic lupus erythematosus in Saudi Arabia: morbidity and mortality in a multiethnic population. Lupus. 2007;16(11):908–914. doi:10.1177/0961203307081112
19. Alballa SR. Systemic lupus erythematosus in Saudi patients. Clin Rheumatol. 1995;14(3):342–346. doi:10.1007/BF02208351
20. Rees F, Doherty M, Grainge MJ, Lanyon P, Zhang W. The worldwide incidence and prevalence of systemic lupus erythematosus: a systematic review of epidemiological studies. Rheumatol Oxf Engl. 2017;56(11):1945–1961. doi:10.1093/rheumatology/kex260
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
