Back to Journals » Journal of Multidisciplinary Healthcare » Volume 11
Frequency of vital sign measurement among intubated patients in the general ward and nurses’ attitudes toward vital sign measurement
Authors Kamio T, Kajiwara A , Iizuka Y, Shiotsuka J, Sanui M
Received 3 July 2018
Accepted for publication 3 September 2018
Published 15 October 2018 Volume 2018:11 Pages 575—581
DOI https://doi.org/10.2147/JMDH.S179033
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Tadashi Kamio,1 Ayako Kajiwara,2 Yusuke Iizuka,1 Junji Shiotsuka,1 Masamitsu Sanui1
1Department of Anesthesiology and Critical Care Medicine, Jichi Medical University Saitama Medical Center, Saitama, Japan; 2Department of Nursing, Jichi Medical University Saitama Medical Center, Saitama, Japan
Purpose: The lack of recognition of respiratory distress may result in emergency tracheal intubation in the general ward. However, few studies have examined the differences in the frequency of vital sign measurement between patients with and without emergency tracheal intubation in the general ward. Thus, this study aimed to investigate the differences in the frequency of vital sign measurements between patients with and without emergency tracheal intubation.
Patients and methods: This is a single-center, retrospective, observational study of unplanned intensive care unit (ICU) admissions from the general wards between December 2015 and February 2017. This study included patients with emergency medical intubations in the general ward who were then transferred to the ICU. Vital signs measured within 24 hours prior to ICU admission were compared between patients who did and did not require emergency tracheal intubation in the general ward. A survey was also conducted to explore the nurses’ attitudes toward vital sign measurements.
Results: Compared with other vital signs, the respiratory rate was significantly less frequently measured. Moreover, the frequency of respiratory rate measurement was lower in the 38 patients who were intubated than in the 102 patients who were not intubated in the general ward (P=0.07). The survey revealed that 54% of the participating nurses considered assessment of the respiratory rate as the most troublesome nursing task and ~15% of nurses did not routinely measure respiratory rates.
Conclusion: Respiratory rate was less frequently assessed in deteriorating patients in the general ward, possibly because it was considered a troublesome task.
Keywords: emergency intubation, vital sign measurements, general ward, nurse’s attitudes toward vital signs, respiratory rate
Plain language summary
Few studies have examined the frequency of vital sign measurement in the general wards for deteriorating patients, who often require emergency intubation to prevent respiratory and cardiac arrest, before they are unexpectedly transferred to the intensive care unit (ICU). This study aimed to investigate the differences in the frequency of vital sign measurement between patients with and without emergency tracheal intubation in the general wards. Moreover, we conducted a survey of nurses using a questionnaire to explore their attitudes toward vital sign measurement. We found that patients who had an emergency tracheal intubation in the general ward tended to receive less frequent assessment of all vital signs within 24 hours prior to unplanned ICU admission. Moreover, our survey revealed the poor understanding of nurses on the importance of respiratory rate assessment in the hospital studied. Our results are important as they reveal the frequency of vital sign measurement in the general ward prior to ICU transfer and provide additional evidence on the general attitude of nurses toward vital sign measurement.
Introduction
Delayed recognition of patient deterioration in the general ward may lead to unplanned intensive care unit (ICU) admissions.1 Furthermore, delayed ICU transfers are associated with poor patient outcomes.2 The lack of recognition of the importance of respiratory status and a delay in intervention for its deterioration may lead to emergency tracheal intubation in the general wards. Respiratory insufficiency is a major preventable cause of in-hospital cardiac arrest in the general ward.3 This suggests that early recognition of respiratory deterioration is key to survival. Among the vital signs measured at the bedside, the respiratory rate is the earliest clinical sign of patient deterioration and has been shown to be an important predictor of fatal events.4–6
As vital sign assessment is an important nursing function that allows the nurse to identify deteriorating patients at an early stage, whether nurses appropriately interpret and respond to abnormal vital sign measurements before the patient’s condition deteriorates is an important issue. Nevertheless, several studies have indicated that vital signs are not consistently measured, recorded, or reported.7–9 Poor clinical monitoring has been shown to be the most dominant cause of preventable deaths in acute hospitals.10 However, few studies have examined the frequency of vital sign measurement in the general wards for deteriorating patients, who often require emergency intubation to prevent respiratory and cardiac arrest, before they are unexpectedly transferred to the ICU.
We, therefore, hypothesized that the vital signs of patients who underwent emergency tracheal intubation in the general ward prior to ICU admission were less monitored compared with patients who did not require emergency tracheal intubation. This study aimed to investigate the differences in the frequency of vital sign measurement between patients with and without emergency tracheal intubation in the general wards. Moreover, as no studies have examined how nurses’ attitudes toward vital sign measurement were reflected on their behaviors in clinical practice, we conducted a survey of nurses using a questionnaire to explore their attitudes toward vital sign measurement.
Patients and methods
Patient selection
We conducted a retrospective, observational study of all unplanned transfers to the ICU from the general wards between December 2015 and February 2017. We examined the frequency of measuring vital signs (body temperature, pulse rate, respiratory rate, and blood pressure) that was documented in the electronic health records of each patient within 24 hours prior to transfer to the ICU. At each measurement, nurses in all adult inpatient areas entered the patients’ vital signs into hand-held, personal digital assistant software at the bedside. The following data were also collected: patient characteristics, type of wards, main reasons for ICU admission, the time and place of intubations, and the presence or absence of continuous monitoring (ie, pulse oximetry and electrocardiogram).
Patients with the following conditions were excluded: planned ICU admissions, transferred to the ICU within 24 hours of hospital admission, already intubated and mechanically ventilated in the general wards before deterioration, and readmissions within 24 hours of ICU discharge.
The study institution has a 608-bed capacity and admits ~19,000 patients annually. Of the 608 beds, 20 were in the ICU including the cardiac care unit and managed by full-time staff of the critical care division. Although we introduced a rapid response system into our hospital in 2014, we have not implemented an Early Warning Scoring System11 in the general wards.
This study was approved by the Institutional Review Board of the Jichi Medical University Saitama Medical Center. Because this was a retrospective study using patients’ data obtained from the electronic health records, the institutional review board and medical ethics committee waived the need for written informed consent from the participants. All data were de-identified prior to entry into the spreadsheet.
Questionnaire
Among the nursing staff, an anonymous survey was conducted. A prerequisite for completion of the questionnaire was that all participants gave informed consent to participate in the present study and the study design was approved by the institutional review board. The objective of this questionnaire was to explore nurses’ attitudes and behaviors toward vital sign measurement. We asked the following questions:
- Q1: “When measuring vital signs (body temperature, pulse rate, respiratory rate, blood pressure, level of consciousness, and urine output), which is the most troublesome one? Explain”
- Q2: “How do you measure respiratory rate for patients?”
We also asked the following questions to explore which physiological change nurses perceive as the first sign of deterioration:
- Q3: “Assuming that you cannot find some other abnormal findings, please choose one from the list below that would be of concern to you as early signs of deterioration in a patient.”
- Systolic blood pressure changes from 130 to 200 mmHg
- Heart rate changes from 60 to 120 bpm
- Respiratory rate changes from 18/min to 26/min
- Oxygen saturation changes from 98% to 94% (on room air)
- Temperature changes from 36.2°C to 39.0°C
This question was generated based on the National Early Warning Score (NEWS). Early warning score systems known as “track-and-trigger systems” are aimed at directing or guiding patient care.12 The National Early Warning Score Development and Implementation Group recommends three trigger levels for a clinical alert requiring clinician assessment based on the NEWS: 1) a low score: an aggregate NEWS of 1–4; 2) a medium score: a NEWS aggregate of 5 or more, or a red score, that is, an extreme variation in an individual physiological parameter; and 3) a high score: an aggregate NEWS of 7 or more.13 These triggers help determine the urgency of the clinical response and the competency of the responders. Therefore, the National Early Warning Score Development and Implementation Group recommends that an extreme score in any one physiological parameter should trigger a medium-level alert. NEWS has a greater capability to discriminate patients at risk of the combined outcome of cardiac arrest, unanticipated ICU admission, or death.14 Among the above questions, only abnormal recording for respiratory rate obtained an extreme score at NEWS. The other abnormal recordings were all low or medium scores.
Statistical analysis and frequency calculations
The frequency of measuring vital signs was calculated by dividing the number of vital sign recordings by 24 hours. Numerical data are presented as medians and IQRs, and categorical data as counts and percentages. As Shapiro–Wilks normality test showed that the frequencies of measuring vital signs were not normal in distribution, Wilcoxon test or Kruskal–Wallis test with Dunn’s post hoc was used accordingly. Similarly, Mann–Whitney U test was used to compare observed frequencies between patients with and without emergency tracheal intubation in the general ward. Group comparisons for categorical variables were performed using chi-squared test. All tests were two sided, and P-values of <0.05 were considered statistically significant. Data were analyzed using JMP Pro12 (SAS Institute Inc., Cary, NC, USA).
Results
Case series
During the study period, a total of 1,822 ICU admissions were recorded. Of them, 140 were unplanned. Demographic characteristics, the main reasons for the admission, intubation status, and ward type before admission to the ICU are described in Table 1. The main reasons for ICU admission documented by physicians were respiratory failure in 67 patients (48%) and sepsis in 33 (24%). A total of 53% of all patients were transferred to the ICU from the surgical wards and 47% were from the medical wards. Among the patients who deteriorated, 13 (9%) needed cardiopulmonary resuscitation in the general ward. Moreover, 38 patients (27%) underwent emergency tracheal intubation in the general ward before ICU admission.
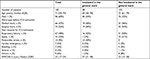  | Table 1 Patient characteristics Abbreviations: APACHE, Acute Physiology And Chronic Health Evaluation; ICU, intensive care unit. |
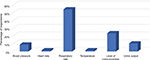
Table 2 and Figure 1 show the frequency of recording of each vital sign for patients who were transferred to the ICU unplanned. The median monitoring frequency 24 hours before ICU admission from the ward was 4 (IQR: 2–5) for respiratory rate, 4 (IQR: 3–6) for temperature, 6 (IQR: 4–9) for blood pressure, and 6 (IQR: 4–10) for pulse. The respiratory rate was significantly less frequently recorded than the other vital signs (P<0.05).
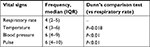  | Table 2 Frequency of vital sign measurement 24 hours before unplanned ICU admission Abbreviation: ICU, intensive care unit. |
  | Figure 1 Frequency of recording of each vital sign in the general ward among patients who were transferred to the ICU unplanned. Abbreviation: ICU, intensive care unit. |
Table 3 shows the comparison of the frequency of recording of each vital sign between patients with and without intubation in the general ward before they were transferred to the ICU. Although the frequency of respiratory rate recording was not significantly different between patients with and without emergency tracheal intubation in the general ward, patients who had emergency tracheal intubation in the general ward tended to receive less frequent assessment of all vital signs within 24 hours prior to the unplanned transfer to the ICU. However, the percentage of patients with continuous monitoring systems in the general ward was similar across the groups.
  | Table 3 Comparison of the frequency of recording of each vital sign between patients with and without intubation in the general ward |
A total of 68 nurses, which accounted for ~10% of the total nursing staff, completed the survey and provided demographic information. The median length of experience was 3.9 years (range, 1–25 years). Of them, 25 (37%) nurses worked in the surgical wards, 35 (51%) in the general ward, and 8 (12%) in the ICU (data not shown).
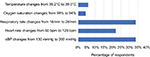
The results of the survey exploring the nurses’ attitudes toward vital sign measurement are shown in Figure 2. More than 50% of the nurses reported that assessment of the respiratory rate is the most troublesome task primarily because it is more time consuming than the measurement of the other vital signs (data not shown in the figure).
Figure 3 shows the percentage of nurses who measured the respiratory rate according to different methods. More than 50% of the nurses counted the respirations for 15 seconds and then multiplied it by 4, while >20% of them recorded the respiratory rate measured by the telemetry machine. Moreover, ~15% of nurses did not routinely count respirations and only recorded the respiratory rate as displayed on the bedside monitor.
  | Figure 3 Nurses’ behaviors regarding respiratory rate measurement. Note: Survey question: “How do you measure respiratory rate?” |
Figure 4 shows the results of a case-scenario-based questionnaire. When the nurses encountered the above situations, systolic blood pressure change and respiratory change were similarly judged as an early sign of deterioration. However, the percentage of nurses who considered respiratory change as the most serious sign of deterioration was only 34%, while >20% of nurses considered heart rate change to be the most serious indicator of deterioration.
Discussion
In this study, we investigated the frequency of vital sign measurement in the general wards within 24 hours prior to an unplanned ICU transfer and the nurses’ attitudes toward vital sign measurement. We found that the respiratory rate was significantly less frequently assessed than blood pressure and pulse. Moreover, patients who had an emergency tracheal intubation in the general ward tended to receive less frequent assessment of all vital signs within 24 hours prior to unplanned ICU admission; however, the rate of using continuous monitoring systems in the general ward was similar across both groups. More than 50% of the participating nurses considered assessment of the respiratory rate to be the most taxing work, and ~15% of them did not routinely count the respirations and only recorded the respiratory rate displayed on the bedside monitor.
Our study has several notable strengths. First, to our knowledge, this is the first report to examine the frequency of vital sign measurement in the general ward prior to ICU transfer for patients with emergency tracheal intubation in the general ward. Second, we showed supporting evidence that nurses consider respiratory rate assessment to be a troublesome task. Our results are important as they provide additional evidence on the general attitude of nurses toward vital sign measurement.
We found that the respiratory rate was less frequently recorded compared with other vital signs, and this finding is consistent with that of previous studies.15–17 Jonsson et al demonstrated that respiratory failure was the primary cause of emergency ICU admission of inpatients, with respiratory rate as the least documented vital sign.16 Moreover, Boerma et al reported that the respiratory rate was poorly documented in patients presenting to the emergency department.17 However, in these studies, information on whether the patients’ vital signs were continuously monitored or not was lacking. Continuous monitoring of patients’ vital signs can alert nurses about any developing clinical events, thus allowing early detection of deterioration and may improve patient outcomes.18 Therefore, if patients were deemed to be stable, their vital signs were less likely to be monitored. The frequency of measuring vital signs is important. However, in the present study, the rate of using continuous monitoring systems in the general ward was similar across the groups. We found that among those who had emergency tracheal intubation in the general ward, 79% were on continuous monitoring equipment (electrocardiogram or pulse oximetry), but tended to have fewer vital sign measurements prior to ICU transfer. This means that nurses recognized that most of these patients were at high risk of deterioration beforehand, and that insufficient patient monitoring might lead to emergency tracheal intubation in the general ward.
Although an increasing respiratory rate is widely recognized as the earliest clinical sign of deterioration, Philip et al showed that the clinical staff are not confident in the accuracy of respiratory rate measurements not assessed using recommended methods.19 Moreover, a recent study revealed that the respiratory rate is inaccurately recorded, even among those with cardiopulmonary compromise.20 The present study also showed that >20% of nurses recorded the respiratory rate measured by the telemetry machine, and ~15% of nurses did not routinely count respirations and only recorded the respiratory rate displayed on the bedside monitor. Our results showed that >50% of the participating nurses considered assessment of the respiratory rate to be the most taxing work. Although there were some reasons for this, the commonest reason was consistent with a recent report that measuring respiratory rate in a clinical setting takes more time than measuring other vital signs.9
Since the lack of understanding of the importance of respiratory rate is an important issue that needs to be addressed,7,19 we attempted to determine the nurses’ perception toward patients’ deterioration using a case-scenario questionnaire, based on NEWS. We found that only 34% of nurses considered respiratory change as the most serious sign of deterioration, although an abnormal respiratory rate was only an extreme score based on the NEWS. This result suggests poor understanding of the importance of respiratory rate assessment. One of the reasons why nurses place less importance on the respiratory rate is because they may lack the knowledge of the key indicators of deterioration and the importance of respiratory rate as a key predictor of a potentially serious clinical event.9 Nurses should be educated regarding the importance of early identification of clinical deterioration to help them understand the significance of accurate and timely respiratory rate assessment.
Limitations
Our study has several limitations. First, this was not a prospective study. All data were obtained from a retrospective review of medical records. However, we carefully evaluated all the patients who were admitted to the ICU and were enrolled in the study. Second, this study was performed in only one ICU, and thus, the number of patients included in the analysis was relatively small. However, this may also be a strength because many confounding factors were controlled (eg, patient characteristics, policy, and Rapid Response Team call strategy). Third, the patients who had emergency tracheal intubation in the general ward might have deteriorated rapidly. Therefore, nurses might have been unable to identify the antecedents, even though they understood the clinical importance of respiratory rate. Patients with severe metabolic acidosis, which may lead to sudden deterioration, may have an increased respiratory rate to maintain a normal hydrogen ion concentration; however, it is unknown whether frequent respiratory rate measurements can prevent emergency tracheal intubation in the general ward and unplanned ICU admissions. Fourth, because of the small sample size, we used non-parametric test to compare differences between patients with and without emergency tracheal intubation in the general ward. As parametric tests have more statistical power than non-parametric tests, increasing our sample size might also give us greater power to detect differences.
Conclusion
We showed that the respiratory rate was significantly less frequently recorded than the other vital signs in patients who were transferred to the ICU unplanned. We also demonstrated that the vital signs were less frequently assessed in the general ward among patients with emergency tracheal intubation. Moreover, our survey revealed the poor understanding of nurses on the importance of respiratory rate assessment in the hospital studied.
Author contributions
TK and MS designed the study. TK and AK collected the data and administered the survey. TK interpreted the data and drafted the manuscript. YI, JS, and MS reviewed the manuscript. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
van Galen LS, Struik PW, Driesen BE, et al. Delayed recognition of deterioration of patients in general wards is mostly caused by human related monitoring failures: a root cause analysis of unplanned ICU admissions. PLoS One. 2016;11(8):e0161393. | ||
Cardoso LT, Grion CM, Matsuo T, et al. Impact of delayed admission to intensive care units on mortality of critically ill patients: a cohort study. Crit Care. 2011;15(1):R28. | ||
Chon GR, Lee J, Shin Y, et al. Clinical outcomes of witnessed and monitored cases of in-hospital cardiac arrest in the general ward of a university hospital in Korea. Respir Care. 2013;58(11):1937–1944. | ||
Buist MD, Moore GE, Bernard SA, Waxman BP, Anderson JN, Nguyen TV. Effects of a medical emergency team on reduction of incidence of and mortality from unexpected cardiac arrests in hospital: preliminary study. BMJ. 2002;324(7334):387–390. | ||
Jones D, Bellomo R, Bates S, et al. Long term effect of a medical emergency team on cardiac arrests in a teaching hospital. Crit Care. 2005;9(6):R808–815. | ||
Kenzaka T, Okayama M, Kuroki S, et al. Importance of vital signs to the early diagnosis and severity of sepsis: association between vital signs and sequential organ failure assessment score in patients with sepsis. Intern Med. 2012;51(8):871–876. | ||
Hodgetts TJ, Kenward G, Vlachonikolis IG, Payne S, Castle N. The identification of risk factors for cardiac arrest and formulation of activation criteria to alert a medical emergency team. Resuscitation. 2002;54(2):125–131. | ||
Goldhill DR, McNarry AF, Mandersloot G, McGinley A. A physiologically-based early warning score for ward patients: the association between score and outcome. Anaesthesia. 2005;60(6):547–553. | ||
Ansell H, Meyer A, Thompson S. Why don’t nurses consistently take patient respiratory rates? Br J Nurs. 2014;3(8):414–4182. | ||
Bianchi W, Dugas AF, Hsieh YH, et al. Revitalizing a vital sign: improving detection of tachypnea at primary triage. Ann Emerg Med. 2013;61(1):37–43. | ||
Chen J, Hillman K, Bellomo R, et al. The impact of introducing medical emergency team system on the documentations of vital signs. Resuscitation. 2009;80(1):35–43. | ||
Smith GB, Prytherch DR, Schmidt PE, Featherstone PI. Review and performance evaluation of aggregate weighted ‘track and trigger’ systems. Resuscitation. 2008;77(2):170–179. | ||
National Early Warning Score (NEWS). Standardising the assessment of acute-illness severity in the NHS. Report of a working party. London: Royal College of Physicians; 2012. | ||
Smith GB, Prytherch DR, Meredith P, Schmidt PE, Featherstone PI. The ability of the National Early Warning Score (NEWS) to discriminate patients at risk of early cardiac arrest, unanticipated intensive care unit admission, and death. Resuscitation. 2013;84(4):465–470. | ||
Cretikos MA, Bellomo R, Hillman K, Chen J, Finfer S, Flabouris A. Respiratory rate: the neglected vital sign. Med J Aust. 2008;188(11):657–659. | ||
Jonsson T, Jonsdottir H, Möller AD, Baldursdottir L. Nursing documentation prior to emergency admissions to the intensive care unit. Nurs Crit Care. 2011;16(4):164–169. | ||
Boerma LM, Reijners EPJ, Hessels RAPA, V Hooft MAA. Risk factors for unplanned transfer to the intensive care unit after emergency department admission. Am J Emerg Med. 2017;35(8):1154–1158. | ||
Brown H, Terrence J, Vasquez P, Bates DW, Zimlichman E. Continuous monitoring in an inpatient medical-surgical unit: a controlled clinical trial. Am J Med. 2014;127(3):226–232. | ||
Philip K, Richardson R, Cohen M. Staff perceptions of respiratory rate measurement in a general hospital. Br J Nurs. 2013;22(10):570–574. | ||
Badawy J, Nguyen OK, Clark C, Halm EA, Makam AN. Is everyone really breathing 20 times a minute? Assessing epidemiology and variation in recorded respiratory rate in hospitalised adults. BMJ Qual Saf. 2017;26(10):832–836. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.