Back to Journals » Clinical, Cosmetic and Investigational Dentistry » Volume 10
Force degradation trend of latex and nonlatex orthodontic elastics after 48 hours stretching
Authors Ardani IGAW, Susanti B, Djaharu’ddin I
Received 14 May 2018
Accepted for publication 18 July 2018
Published 11 October 2018 Volume 2018:10 Pages 211—220
DOI https://doi.org/10.2147/CCIDE.S173648
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Christopher E. Okunseri
I Gusti Aju Wahju Ardani,1 Bintiana Susanti,2 Irwadi Djaharu’ddin1
1Department of Orthodontics, Faculty of Dental Medicine, Universitas Airlangga, Surabaya, Indonesia; 2Department of Orthodontics, Faculty of Dental Medicine, Universitas Airlangga, Surabaya, Indonesia
Background: Two types of orthodontic elastics exist based on their material, latex and nonlatex, each of which has different properties in clinical use. Some of the differences include their initial force and force degradation over time. This study was conducted to compare the force changes in both materials.
Aim: To evaluate the force degradation of latex and nonlatex elastics under moderate stretching over time.
Methods: Medium-force orthodontic latex and nonlatex elastics from American Orthodontics (AO) and Ortho Technology (OT) of lumen size 1/4 inches and 3/16 inches (total sample 110 elastics) were submerged in artificial saliva (pH 6.7) and incubated for 48 hours. Then, the elastic force was measured at the following time intervals: initial, 1, 3, 6, 12, 24, and 48 hours. Orthodontic latex and nonlatex elastics from AO and OT were analyzed using Fourier-Transform Infrared Spectroscopy and energy-dispersive X-ray to know the chemical bond structure and elements.
Results: There was a statistically significant difference between latex and nonlatex force degradation over a period of 0–24 hours (P<0.05), while no significant difference existed between 24–48 hours (P>0.05). Force degradation of latex elastics was higher than that of nonlatex elastics. Energy-dispersive X-ray results on nonlatex elastic bands from OT and AO showed higher C element in the latex elastic band from OT, while the latex elastic band from AO had higher Al element.
Conclusion: Medium-force latex and nonlatex elastics 1/4 inches and 3/16 inches in size both showed force degradation at 1, 3, 6, 12, and 24-hour intervals under 30 mm stretching when kept in artificial saliva (pH 6.7) and incubated at 37°C for 48 hours.
Keywords: force degradation, orthodontic elastics, latex, nonlatex, medium force
Introduction
Elastics, as highlighted by Case et al,1 have long been used in orthodontics. According to Wang et al,2 from a cost perspective, elastics are relatively cheap and can be easily removed and installed by patients.
Alavi and Monoghan3 stated that natural latex is an isoprene polymer consisting mainly of heavy molecules and small quantities of protein and fatty acids. Although natural latex is nonallergenic, it possesses weak mechanical properties which require reinforcement. One additive used to improve the mechanical properties of latex is ammonia, despite the fact that its addition produces allergens. Another process, vulcanization, which involves the addition of accelerants and antioxidants, also generates allergens.3
According to the American Dental Association Council on Scientific Affairs, approximately 0.12%–6% of the general population and 6.2% of dental health professionals are hypersensitive to latex. According to Russell et al,4 the effects of hypersensitivity vary from dermatitis to anaphylactic shock.
Since the early 1990s, nonlatex elastics have been synthesized for patients who are allergic to latex. However, latex and nonlatex elastics posses contrasting mechanical properties in clinical use, specifically in terms of their initial force and force degradation, which thus merit further investigation. Russel at al4 previously compared the properties of latex and nonlatex elastics and reported the different mechanical properties of the 2 according to the material and manufacturing processes.
Kersey et al5 evaluated the initial force and force degradation of 4 different nonlatex elastic brands over 24 hours and found that with equal traction force, the initial force generated by the various brands differed significantly. In addition, Kersey et al5 also reported that elastics lost 50% of their initial force within 24 hours of the postdynamic test.
López et al,6 conducted a study on latex and nonlatex elastics under wet conditions, which resulted in greater force degradation in the nonlatex elastics than latex elastics.6 Although, to date, studies on latex elastics have been widely conducted, those on nonlatex elastics remain limited with controversial results, mainly due to the varying experimental methods applied within different studies.
Materials and methods
This study was a laboratory experimental research using medium-force latex and nonlatex orthodontic elastics of size 1/4 inches and 3/16 inches from American Orthodontics (AO) and Ortho Technology (OT). Sampling size was determined using a Lemeshow formula and totaled 110 samples, which were divided into 11 groups according to brand, size, and elastic material. Meanwhile, Fourier-Transform Infrared Spectroscopy (FTIR) (Thermo Nicolet Nexus 670, Thermo Fisher Scientific, Waltham, MA, USA) and energy-dispersive X-ray (EDX) (AMETEK, EDAX, Mahwah, NJ, USA) analyses were carried out at the Laboratory of FTI Institut Teknologi Sepuluh Nopember, Surabaya, Indonesia.
Data collection was performed using a Tension gauge/Dontrix gauge, which measured the tensile force of the elastics when stretched diagonally between its 2 pins with 30 mm extension and 20° angulation. The initial force of the elastics was measured in grams. The elastics were then submerged in a plastic container containing artificial saliva (pH 6.7) and incubated at 37°C for 48 hours. After that period had elapsed, the tensile force of the elastics was measured repeatedly by removing them from one of the pins with mosquito pliers and then pulling them back to their original position to embrace both pins. At the end of 1 hour of stretching, the tensile force of the elastics was then read on the scale of the gauge. Consecutive measurements were taken after 1, 3, 6, 12, 24, and 48 hours using exactly the same method.
Results
The changes in the tensile force averages and standard deviations for both latex and nonlatex elastics over time are shown in Figure 1 and Table 1.
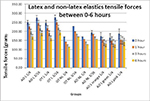  | Figure 1 Average and SD of latex and nonlatex elastics tensile force 0–6 hours. Abbreviations: AO, American Orthodontics; L, latex; NL, nonlatex; OT, Ortho Technology. |
  | Table 1 Average and SD of latex and nonlatex elastics tensile forces 12–48 hours Abbreviations: AO, American Orthodontics; L, latex; NL, nonlatex; OT, Ortho Technology. |
Based on the calculated average values in Figure 1 and Table 1, Shapiro–Wilk tests were used to check the normal distribution of data. The Shapiro–Wilk tests showed that the data in every group was not normally distributed (P<0.05). Consequently, a Wilcoxon singed-rank test was utilized to check the differences between time intervals within each group, as shown in Tables 2–5.
  | Table 3 Level of significance for 1/4 inch OT latex and nonlatex elastics at different time intervals Note: aStatistically significant. Abbreviations: L, latex; NL, nonlatex; OT, Ortho Technology. |
  | Table 5 Level of significance for 3/16 inch OT latex and nonlatex elastics at different time intervals Note: aStatistically significant. Abbreviations: L, latex; NL, nonlatex; OT, Ortho Technology. |
The Wilcoxon Signed-Rank results in Table 2 show there were statistically significant differences in tensile force changes for the AO latex 1/4 inch (AO L 1/4) group between 0–1, 1–3, 3–6 and 6–12 hours (P<0.05), but not for the 12–24 and 24–48 hours immersion intervals (P>0.05). Significant changes in tensile forces were also exhibited by the AO L 1/4 orange, AO L 1/4 green, and AO L 1/4 pink groups for 5 consecutive intervals (P<0.05). However, for the 24–48 hours intervals, these groups showed P-values >0.05, indicating that no significant changes were found during this time period.
OT latex 1/4 inch (OT L 1/4) group (Table 3) showed statistically significant differences in tensile force changes during the first 24 hours (P<0.05): 0.008 during 0–1 hour and 0.002 during 1–3, 3–6, 6–12, and 12–24 hours. During the 24–48 hours interval, no significant change was found (P>0.05) within the same group.
As can be seen in Table 4, statistical analysis revealed significant changes in tensile forces (P<0.05) for 5 consecutive intervals for the AO latex 3/6 inch (AO L 3/16) group and AO nonlatex 3/6 inch (AO NL 3/16). Nevertheless, for the 24–48 hours interval, there were no significant changes exhibited by either group (P>0.05).
The OT latex 3/16 inch (OT L 3/16) group showed statistically significant changes during the 0–1, 1–3, 3–6, and 12–24 hours intervals with respective P-values of 0.011, 0.020, 0.019, and 0.005 (Table 5). For the 6–12 and 12–24 hours intervals, statistical analysis revealed no significant changes since P-values were found to be 0.063 and 1.000, respectively. On the contrary, the OT nonlatex 3/16 inch (OT NL 3/16) group only showed significant changes for the 0–1 and 6–12 hours intervals with the same P-values of 0.004, while no significant changes were obtained for the other intervals (1–3, 3–6, 12–24, and 24–48 hours).
A comparison of the reduction in tensile forces over time (force degradation) for latex and nonlatex elastics are shown in Figures 2–5.
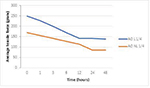  | Figure 2 Force degradation trend for 1/4 inch AO latex and nonlatex elastics over time. Abbreviations: AO, American Orthodontics; L, latex; NL, nonlatex. |
  | Figure 3 Force degradation trend for 1/4 inch OT latex and nonlatex elastics over time. Abbreviations: L, latex; NL, nonlatex; OT, Ortho Technology. |
  | Figure 4 Force degradation trend for 3/16 inch AO latex and nonlatex elastics over time. Abbreviations: AO, American Orthodontics; L, latex; NL, nonlatex. |
  | Figure 5 Force degradation trend for 3/16 inch OT latex and nonlatex elastics over time. Abbreviations: L, latex; NL, nonlatex; OT, Ortho Technology. |
Figure 2 above depicts the force degradation trend of the AO L 1/4 group and AO NL 1/4 group over time. The AO L 1/4 graph shows a declining trend of tensile force for the first 12 hours, yet an almost flat trend for the 12–48 hours interval as the changes in tensile force after 12 hours time were found to be not significant (P>0.05). Although the same pattern can be seen for the AO NL 1/4 group, in which the graph appears to be continuously declining within the 12 hours period, unlike the AO L 1/4 group the force degradation during 12–24 hours interval for AO NL 1/4 shows a steep decline before becoming stable during the 24–48 hours interval.
The graphs in Figure 3 compare the force degradation of OT L 1/4 and OT NL 1/4. Both graphs contain a steeply declining gradient during the first 24 hours (significant force degradations) before leveling off between 24 and 48 hours (nonsignificant force degradations).
In Figures 4 and 5, the trend for AO L 3/16, AO NL 3/16, OT L 3/16, and OT NL 3/16 graphs shows a similar pattern: a steep reduction in tensile force during the first 24 hours, followed by a small force reduction toward 48 hours for OT NL 3/16 (P=0.317) or no reduction for the other graphs (P=1.000).
Results of the FTIR analysis showed the composition and functional structure of the latex and nonlatex elastic bands. OT nonlatex has vinyl ether bonds with a peak 1,013.52 wavelength, while OT latex has alkene bonds with a peak of 697.00 wavelength (Figures 6 and 7). AO latex has halo compound bonds with a peak 841.32 wavelength, while AO nonlatex has alkene bonds with a peak 841.32 wavelength (Figures 8 and 9).
  | Figure 6 Results of the FTIR analysis on OT nonlatex elastic band. Abbreviations: FTIR, Fourier-Transform Infrared Spectroscopy; OT, Ortho Technology. |
  | Figure 7 Results of the FTIR analysis on OT latex elastic band. Abbreviations: FTIR, Fourier-Transform Infrared Spectroscopy; OT, Ortho Technology. |
  | Figure 8 Results of the FTIR analysis on AO latex elastic band. Abbreviations: AO, American Orthodontics; FTIR, Fourier-Transform Infrared Spectroscopy. |
  | Figure 9 Results of the FTIR analysis on AO nonlatex elastic band. Abbreviations: AO, American Orthodontics; FTIR, Fourier-Transform Infrared Spectroscopy. |
EDX results on nonlatex elastic band OT showed higher C element 58.78 and O element 25.51, while nonlatex elastic band AO higher C element 55.62 and O element 44.38 (Figures 10 and 11).
  | Figure 10 Results of the EDX analysis on OT nonlatex elastic band. Abbreviations: EDX, energy-dispersive X-ray; OT, Ortho Technology; KCnt, thermal conductivity carbon nano tubes. |
  | Figure 11 Results of the EDX analysis on AO nonlatex elastic band. Abbreviations: AO, American Orthodontics; EDX, energy-dispersive X-ray; KCnt, thermal conductivity carbon nano tubes. |
EDX results on latex elastic band OT showed higher C element 48.93 and O element 31.23, while latex elastic band AO higher Al element 53.25 and O element 26.13 (Figures 12 and 13).
  | Figure 12 Results of the EDX analysis on OT latex elastic band. Abbreviations: EDX, energy-dispersive X-ray; OT, Ortho Technology; KCnt, thermal conductivity carbon nano tubes. |
  | Figure 13 Results of the EDX analysis on AO latex elastic band. Abbreviations: AO, American Orthodontics; EDX, energy-dispersive X-ray; KCnt, thermal conductivity carbon nano tubes. |
Discussion
Tooth movement that occurs in orthodontics is the result of the forces applied. The use of both intraoral and extraoral elastics in orthodontics has produced significant results. The use of elastics along with effective cooperation from the patients can correct anteroposterior or vertical discrepancies.7,8
Force degradation is a major problem affecting the clinical use of latex or nonlatex elastics. Continuous loss of tensile force over time makes it difficult for clinicians to determine the actual force applied to the teeth, despite such applications being expected to generate constant and optimal tension for a specified time period. In this study, force degradation of latex and nonlatex elastics was investigated to aid in its clinical use.7,9
Similar to a study conducted by López et al,6 this research was an in vitro investigation involving an artificially fabricated environment simulating the oral environment. Elastics were submerged in an artificial saliva medium of pH 6.7 and incubated at 37°C.6
The samples in this study utilized two different elastic brands: AO and OT. The decision to use more than 1 elastic brand was based on their different formulations and manufacturing processes. Thus, the results of this research can provide additional information for elastic users.
This study measured tensile forces generated by the elastics at 1, 3, 6, 12, 24, and 48 hours of stretching. In several previous studies, the first 3 periods (1, 3, and 6 hours) were reported as representing the greatest loss of tensile force. A number of investigations found that the largest force reduction occurred between 3 and 5 hours of stretching, while others asserted that it occurred within the first 1 hour.2,10,11 Three other subsequent periods (12, 24, and 48 hours) showed a much slower rate of force degradation.2,6 In several studies, including one conducted by Pithon et al, a 24-hour period was chosen since it generally constituted the time for elastic users to replace their elastics, while a 12-hour period represented the median time between initial use and replacement.14
Results gathered form this study showed that almost all types of latex and nonlatex elastics experienced force degradation at all time intervals (0–1, 1–3, 3–6, 6–12, 12–24, and 24–48 hours) when compared to their initial forces. These results are consistent with those of other studies by Alavi and Monoghan.3 A study conducted by López et al6 on 1/4 inch medium-force latex and nonlatex elastics from GAC and Lancer at 5 seconds and 8- and 24-hour periods after immersion in artificial saliva showed that force degradation was significant at 8 and 24 hours for GAC latex, GAC nonlatex, and Lancer latex, yet not significant for Lancer nonlatex. Alavi and Monoghan3 in their study explained that the force degradation for nonlatex elastics from Forestadent (Pforzheim, Germany), Dentaurum (Ispringen, Germany) and OT was statistically significant for the first 1 hour (4%–7.5%) and reached 19%–38% at the 24-hour point. Similarly, Gioka et al,11 who studied latex elastics, found 25% force degradation within a 24-hour period.3
In this study, the significance of force degradation between 3 and 48 hours varied. At 3 hours of stretching, OT NL 3/16 did not show significant reduction in tensile force, as was also the case with OT NL 1/4 and OT NL 3/16 at 6 hours of stretching, OT L 3/16 and OT NL 1/4 at 12 hours of stretching, and AO L 1/4 and OT NL 3/16 after 24 hours of stretching. Insignificant reduction in tensile force indicated relatively stable tension was produced by the elastics within the time period. The observed variations between groups may have been influenced by the different elastic brands used and the lumen diameter sizes.
In keeping with Wang et al,2 during the 24 hours after stretching, all groups exhibited very low force reduction as shown by the nonsignificant force degradations (0%–1%) during 24–48 hours interval. Liu et al12 stated that structural changes of the elastics after repeated stretching are not cumulative. Therefore, after a certain period of time, the tensile force of the elastics will be stable despite increased repeated stretching. Another study by Bishara13 even suggests that elastics not be replaced frequently as, after an initial large application of tensile force, the remaining force remains constant over time. Nevertheless, for reasons of hygiene, elastics are to be replaced after 24 hours as they also tend to break due to activities in the mouth.12,13
Comparisons between latex and nonlatex elastics showed significant differences. AO L 1/4 and AO NL 1/4 showed force degradation of 9.1% and 8.3% at the 0–1 hour interval, 12.5% and 9.1% at the 1–3 hours interval, 14.3% and 10.0% at the 3–6-hour interval, 16.7% and 11.1% at the 6–12 hours interval, and 2% and 0% at the 24–48 hours interval. The same pattern was observed for the OT brand, in which force degradation of latex elastics at all intervals were greater than nonlatex elastics. These results are comparable to a previous in vivo study of Pithon et al14 in which latex and nonlatex elastics 1/8, 1/4, and 5/16 inches in diameter were placed intermaxillary and observed at 0, 12, and 24 hours for stretching. Pithon et al14 reported that nonlatex elastics 1/4 and 5/16 inches in size were able to maintain initial force for between 0 and 12 hours, implying the changes in the tensile force of the elastics were relatively small for the time period. Conflicting results were found by Russel et al4 and López et al,6 showing greater force degradation for nonlatex elastics than latex elastics. These differences may due to the different brands of elastics used, methods, and research environments of the studies. On the other hand, according to Kersey et al, there was no a significant difference between latex and nonlatex elastics during static testing, yet a significant difference was found during dynamic testing.5
Force degradation of latex and nonlatex elastics is multifactoral. One of the factors, as stated by Case et al,1 is fluid absorption during the period of immersion. Elastics in this study were extended to 30 mm in accordance with the study of Bales et al.15 It was stated that the normal range of retraction distance during clinical use in the mouth is between 20 and 40 mm. Other studies proposed a retraction distance corresponding to the force index (Kersey et al5; Russell et al4). However, as concluded by Kersey et al,5 force index does not represent the actual tensile force of the elastics. Russel et al4 observed that the initial forces of elastics stretched according to the force index was greater than those specified by the manufacturers as seen in this study. For AO L 1/4 and AO L 3/16, the measured initial forces were 249 and 274.9 g, respectively, despite the force index listed on the package being 125 g. For OT L 1/4 and OT L 3/16, the measured initial forces were 120 and 151 g higher than the given force index of 128 g. Correspondingly, for AO and OT nonlatex elastics, a similar pattern applied.
Information on elastic force degradation is very important for users as it will give an objective evaluation in determining the appropriate type of elastic and duration of use necessary for optimal results. Furthermore, this information is also useful for manufacturers to include data regarding the force degradation of their respective elastics in their packaging.
Conclusion
Significant force degradations were observed in medium-force 1/4 and 3/6 inch latex and nonlatex elastics between 0 and 12 hours after 30 mm extension at 20°, yet no significant force degradations were observed between 24 and 48 hours. Force degradations of medium-force 1/4 and 3/16 inch latex elastics between 0 and 24 hours were higher than those of nonlatex elastics; yet between 24 and 48 hours, force degradations were shown to be the opposite. Generally, as time increases, the tensile force of the elastics decreases. Both latex and nonlatex elastics showed a similar degradation trend of tensile force, except that for latex elastics insignificant reductions were observed in the 12–48 hours period, while for the nonlatex variety these occurred during the 24–48 hours period.
Acknowledgment
The authors thank the Faculty of Dental Medicine, Universitas Airlangga, Surabaya, East Java, Indonesia, and Institute Technology Sepuluh November Faculty of Industrial Engineering, for helping in the research.
Disclosure
The authors report no conflicts of interest in this work.
References
Case W, Fernandes G, Artese F. Force extension relaxation of medium force orthodontic latex elastics. Angle Orthod. 2011;81(5):812–819. | ||
Wang T, Zhou G, Tan X, Dong Y. Evaluation of Force Degradation Characteristics of Orthodontic Latex Elastics in Vitro and In Vivo. Angle Orthod. 2007;77(4):688–693. | ||
Alavi K, Monoghan P. An in vitro study simulating effect of daily diet and patient elastic band change compliance on orthodontic latex elastic. Angle Orthod. 2014;7(2):234–239. | ||
Russell KA, Milne AD, Khanna RA, Lee JM. In vitro assessment of the mechanical properties of latex and non-latex orthodontic elastics. Am J Orthod Dentofacial Orthop. 2001;120(1):36–44. | ||
Kersey M, Glover K, Heo G. A comparison of dynamic and static testing of latex and non latex orthodontic elastic. Angle Orthod. 2003;73(2):181–186. | ||
López N, Vicente A, Bravo LA, Calvo Guirado JL, Canteras M, Lopez, Vicente B. In vitro study of force decay of latex and non-latex orthodontic elastics. Eur J Orthod. 2012;34(2):202–207. | ||
Kamisetty SK, Nimagadda C, Begam MP, Nalamotu R, Srivastav T, Gs S. Elasticity in Elastics-An in-vitro study. J Int Oral Health. 2014;6(2):96–105. | ||
Wong AK. Orthodontic Elastis Material. Angle Orthod. 1976;46:198–205. | ||
Langlade HM, Lobner D. In vitro neuron cytotoxicity of latex and nonlatex orthodontic elastics. Am J Orthod Dentofacial Ortho. 2004;122(1):65–70. | ||
El-Hassanein, H., Orthodontic elastics, Al-Azhar University Faculty of Dental Medicine Orthodontic Department, Cairo. Modul Book. 2007. 1–30. Available on https://www.scribd.com/doc/49649457/elastics-in-orthodontics-Hassanein. | ||
Gioka SP, Stewart K, Katona T. The effect of pH levels on latex vs latex interach elastic. Angle Orthod. 2011;81(6):1070–1074. | ||
Liu CC, Wataha JC, Craig RG. The effect of repeated stretching on the force decay and compliance of vulcanized cis-polyisoprene orthodontic elastics. Dent Mater. 1993;9(1):37–40. | ||
Bishara SE. Texbook of Orthodontics. 2nd ed. New Delhi; WB Saunders Company; 2001:452–455. | ||
Pithon MM, Santana DA, Sousa KH, Farias IM, Sousa F. Does chlorhexidine in different formulations interfere with the force of orthodontic elastics? Angle Orthod. 2013;83(2):313–318. | ||
Bales TR, Chaconas SJ, Caputo AA. Force-extension characteristics of orthodontic elastics. Am J Orthod. 1977;72(3):296–302. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


