Back to Journals » Infection and Drug Resistance » Volume 15
Follow-Up of Surgical or Nonsurgical Patients with Pulmonary Cryptococcosis: A Real-World Study
Authors Li H , Ma Y, Zeng Z, Luo L, Li T, Zeng H, Chen Y
Received 17 December 2021
Accepted for publication 30 May 2022
Published 11 July 2022 Volume 2022:15 Pages 3669—3681
DOI https://doi.org/10.2147/IDR.S352966
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Herui Li,* Yiming Ma,* Zihang Zeng, Lijuan Luo, Tiao Li, Huihui Zeng, Yan Chen
Department of Respiratory and Critical Care Medicine, the Second Xiangya Hospital, Central South University, Changsha, Hunan, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yan Chen; Huihui Zeng, Department of Respiratory and Critical Care Medicine, the Second Xiangya Hospital, Central South University, 139 Renmin Road, Changsha, 410011, Hunan, People’s Republic of China, Email [email protected]; [email protected]
Background: Surgical and medical treatments are applied to pulmonary cryptococcosis (PC) in the real world, while the prognosis of different therapies is uncertain. This study investigated diagnosis, real-world therapy, follow-up outcomes, and prognosis factors, aiming to deepen our understanding of PC.
Methods: Patients pathologically diagnosed with PC were retrospectively reviewed and followed up. Further comparisons and subgroup analyses were conducted in surgical and nonsurgical treatment individuals. Univariable and multivariable logistic regression methods were used to explore the risk factors associated with treatment failure.
Results: One hundred and sixty-three patients were included in this study, of whom 92 underwent surgical removal of VATS or open lung surgery (68 of them received postoperative antifungal treatment) and 71 got antifungal drugs only. Compared with nonsurgical patients, surgical patients were more immunocompetent (73 [79.3%] cases vs 33 [46.5%]), showed milder symptoms and more limited pulmonary lesions. Although they had instant treatment response owing to lesions resection, there is no significant advantage in the rate of treatment failure. Multivariable regression showed independent predictive factors associated with treatment failure were polymorphonuclear (PMN)> 6.30*109/L, albumin (Alb) < 40g/L and antifungal dosage < 400mg/d. Further analysis among patients with different immune statuses or symptoms demonstrated that sufficient antifungal dosage could reduce the rate of treatment failure.
Conclusion: PC showed variable and nonspecific clinical features. PC patients with limited nodules/masses and mild symptoms often led to misdiagnosis and unnecessary lung resections. The potential risk factors including higher PMN and hypoalbuminemia could help clinicians to identify PC patients with poor treatment efficiency at an early stage. To note, sufficient antifungal dosage may improve the treatment outcomes.
Keywords: pulmonary cryptococcosis, diagnosis, antifungal treatment, clinical features, surgery
Introduction
Cryptococcus, an omnipresent budding yeast-like basidiomycete in the environment,1 causes human diseases by Cryptococcus neoformans and Cryptococcusgattii.2 Although Cryptococcus is more likely to invade the central nervous system,3 the lung is always the first stop via inhalation that triggers pulmonary cryptococcosis (PC).4 PC shows a gradually increased incidence over the past 20 years,5 to the extent that it has become one of the most common opportunistic invasive fungal infections in China.6 It is well known that PC mainly affects immunocompromised individuals;7 however, more than half of Chinese patients were immunocompetent.3,8,9 PC presents as nonspecific clinical and radiological features, perpetuating a knowledge deficit and resulting in a high misdiagnosis rate.10
The treatment of PC tends to follow the guidelines published by the Infectious Diseases Society of America in 2000, updated in 2010: step-wise graded antifungal treatment based on immune status, severity, and presence of extrapulmonary.11 Fluconazole has been the most commonly used drug, although itraconazole, voriconazole and posaconazole are also available.11 However, evidence regarding the management of PC is mainly from retrospective surveys and anecdotal reports, while specific therapies and optimal duration of treatment have not been precisely elucidated,11 leading to inconsistent treatments.12
Surgery is considered for diagnosis or salvage treatment after ineffective antifungal therapy; however, the efficiency of single surgery without drug treatment in PC has not reached a consensus.11,13 Furthermore, the information about the dosage and duration of postoperative or nonsurgical antifungal treatment is limited. To discuss the efficiency of different treatment approaches, this study enrolled 163 surgical and nonsurgical PC cases with pathological evidence, reviewed their clinical and radiological features, and followed up these cases for more than 6 months.
Materials and Methods
Patients and Data
One hundred and sixty-three patients with tissue-proven PC were analyzed, and all patients were diagnosed during hospitalization in the Second Xiangya Hospital of Central South University from November 2009 to December 2020 (Figure 1). The inclusion criteria included: 1) biopsy-confirmed PC; 2) clinical data and CT imaging information were available. Exclusion criteria were: 1) medical record missing; 2) HIV positive; 2) complicated with extrapulmonary involvement; 3) concomitant with other pulmonary infiltrating diseases, which may influence the assessment of PC; 4) loss to follow-up. Data about clinical characteristics, diagnosis, treatment and follow-up outcomes of the patients were collected and analyzed. Subjects were grouped as surgical and nonsurgical individuals, and immunocompromised individuals were defined as at least one of the predisposing conditions: diabetes mellitus, malignancy, solid organ transplantation, cirrhosis, respiratory disorder, immunosuppressive drug therapy (such as immunosuppressor and glucocorticoid) and other defined immunosuppressive diseases. In addition, the stratification of antifungal therapeutic dose was classified into <200 mg/d, 200–400 mg/d and ≥400 mg/d, and duration was classified into referred to <2 months, 2–6 months and 6 months, referring to clinical practice guidelines for cryptococcal disease11 and expert consensus on diagnosis and treatment of pulmonary cryptococcosis.14 The study protocol was approved by the institutional ethics committee of the Second Xiangya Hospital of Central South University (No. 2018-023) and complied with the Declaration of Helsinki. Informed consents were obtained from all involved patients.
 |
Figure 1 Flowchart diagram of eligible study population. |
The demographics, history of illness, laboratory and radiological features, diagnosis and treatments were collected from the medical records without intervention. The information of follow-up studies was obtained through regular clinical assessments and telephone calls. All patients had CT scans, and the image findings were divided into three patterns, including nodules/masses (isolated or multiple), pneumonic infiltrates or mixed.10 Two experienced radiologists assessed all image findings independently.
Follow-Up and Outcomes
All patients were followed up to 1st August, 2021 (at least 6 months). The definition of outcomes referred to studies by Zhang et al,10 Yang et al,13 Wei et al15 with summarization and modification. Recovery was defined as the disappearance of clinical imaging abnormalities, and improvement was the partial improvement of clinical or imaging findings. Persistence meant no change of symptoms or radiology after at least two-months-antifungal therapy, and progression was defined as symptoms/images aggravation or recurrence (after lesions were removed). Furthermore, recovery and improvement groups were defined as treatment response group, while the other two were merged into the treatment failure group.
Statistical Analysis
All information was entered and verified by three researchers independently, with SPSS 18.0 software (SPSS Inc., Chicago, IL, USA) for the data processing. Continuous variables were presented as mean ± SD or median (interquartile range, IQR); categorical variables were presented as count (percentage). Comparisons between surgical and nonsurgical subjects were analyzed by two-sample t-test or Wilcoxon rank-sum test for continuous variables, by chi-square or Fisher’s exact test for categorical variables. To explore the risk factors associated with treatment failure, univariable and multivariable logistic regression models were used, in which variables with P value of <0.10 in univariate analysis were included in multivariate regression. A significant difference was approved with P < 0.05.
Results
Demographic and Clinical Information
Figure 2 demonstrates the accumulative numbers of cases with tissue-proven PC from 2009 to 2020, suggesting a general upward trend. Our study identified 163 patients, of whom 92 (56.4%) underwent surgical removal by VATS or open lung surgery, followed by clinical observation or postoperative antifungal treatment; 71 received PNLB or TNLB for diagnosis and antifungal therapy. Except for the 2020 (COVID-19 epidemic), the rate of surgery presented a decreasing trend.
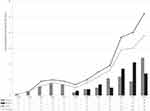 |
Figure 2 Dynamics of pulmonary cryptococcosis diagnosed in patients from 2009 to 2020. |
Table 1 summarizes the clinical data of the 163 PC patients. They age from 15 to 82 years, including 106 males, 47.9% of them lived in the village. Fourteen cases had specific histories environmental exposure, including pigeons (eight cases), wet environments (three cases), dust (two cases) and fowl (two cases). Comorbidities were present in 35.6% of patients, with diabetes being the most common (19 [11.7%] cases), followed by immunosuppressive therapy associated diseases (16 [9.8%] cases) and malignancy (16 [9.8%] cases). Besides 64 asymptomatic cases, the most common symptoms were cough and expectoration, followed by chest discomfort and bloody phlegm. Forty-seven patients underwent serum cryptococcal antigen (CrAg) test and 57.4% of them had positive results. The lesions are mainly located unilaterally in the single lobe, 87.7% of which manifested as isolated or multiple nodules/masses, most commonly accompanied by spiculation, pleural involvement, patchy shadow and mediastinal lymphadenopathy. Histologically (Supplement Figure 1), the lesions mostly performed as granuloma (62.6%), followed by necrosis (7.4%), dispersed pathogen (18.4%) and mixed lesions (11.7%). Specific stains were used to find the pathogen, of which the positive rates were 94.1%, 89.2% and 92.3% in PAS (101 cases), GMS (74 cases) and AP (52 cases) staining.
 |
Table 1 Clinical Features of 163 Patients with PC |
Diagnosis and Treatment
Diagnosis, treatment and follow-up data are shown in Table 2. Of all 163 cases, the median illness course was 30 days (IQR 15–60 days), suggesting subacute or chronic onset. Cryptococcal infection was rarely considered during the initial visits, and most cases were diagnosed with uncertainty (42.9%), followed by lung cancer (28.2%) and pneumonia (25.8%). Seventy-one patients received antifungal drugs only, with a median fluconazole dose of 375mg/d (IQR 300–450 mg/d) and a median duration of 6 months (IQR 3–8 months).
 |
Table 2 Diagnosis and Treatment Outcomes of 163 Patients with PC |
Surgery and Non-Surgery
As shown in Table 1, there was no significant difference in age, sex, and the area between surgical and nonsurgical patients. However, the immunocompromised frequency (including immunosuppressive drug therapy and renal transplantation) was significantly higher in nonsurgical patients. Compared with surgical patients, nonsurgical cases had more symptoms (such as cough, expectoration, dyspnea and fever), wilder pulmonary involvement accompanied with patchy shadow and cavity. In surgical individuals, spiculation was more common, which may heighten the suspicion of lung cancer. There were significant differences in blood routines and serum albumin examination, of which nonsurgical cases showed decreased hemoglobin (HBG) and albumin (Alb), higher count of white blood cell (WBC) and polymorphonuclear (PMN), but they were mostly in the normal range. Among patients receiving serum C-reactive protein (CRP), erythrocyte sedimentation rate (ESR) and cryptococcal antigen (CrAg) test, the positive rates in nonsurgical subjects were higher than those in surgical patients.
Among 92 surgical patients, 68 received postoperative antifungal treatment with a median dose of 300 mg/d (IQR 150–300 mg/d) for a median of 2 months (IQR 1–3 months). The clinical characteristics between patients who underwent simple surgery and postoperative antifungal treatment had no difference (Supplement Table 1). In total, 88.1% of the 163 patients had completely recovered or partly improved (Supplement Figure 2), and the rate of treatment failure (Supplement Figure 3) was 12.9%.
As shown in Table 2, surgical patients were mostly diagnosed with lung cancer on the initial visits, which led to surgical resection of benign lesions. After lesion resection, the surgical patients took antifungal drugs in a lower dose [300 (IQR 150–300) mg/d vs 375 (IQR 300–450) mg/d] and for a shorter duration [2 (IQR 1–3) months vs 6 (IQR 3–8) months] than patients in the nonsurgical group, while the progressive rate of these two groups had no obvious difference.
Since the guidelines recommend antifungal treatment as a primary therapy, of which medication regimen was determined by the severity of disease and immune status of patients, we showed therapeutic dosage, duration and efficiency among different people simply using the histogram. Significantly, higher dosages and longer duration of antifungal drugs were observed in symptomatic patients than those in asymptomatic cases. In different people, sufficient antifungal doses may reduce the rate of treatment failure. Treatment and follow-up outcomes among different populations are demonstrated in Figure 3.
Prognostic Factors
Univariate and multivariate analyses were performed in patients with different treatment efficiency (Table 3). Univariate analysis revealed that treatment failures occurred mostly in patients from the village (P=0.026), with HGB <130g/L (P=0.019), PMN >6.30*109/L (P<0.001), Alb <40g/L (P=0.001), and mixed lesions (P=0.004). Multivariate analysis was constructed using the following variables: male, village, immunocompromised, HGB <130g/L, PMN >6.30*109/L, Alb <40g/L, lesion patterns, only antifungal drug and antifungal dosage. Independent predictive factors associated with treatment failure in patients with PC were PMN >6.30*109/L (OR 18.079, 95% CI 3.539–92.352, P = 0.001), Alb <40g/L (OR 7.781, 95% CI 1.947–31.089, P=0.004) and antifungal dosage <400mg/d [200–400mg/d (OR 13.141, 95% CI 1.777–97.196, P=0.012); <200mg/d (OR 19.317, 95% CI 2.067–180.524, P=0.009).
 |
Table 3 Univariate and Multivariate Analysis of Factors Associated with Treatment Failure in 163 Patients with PC |
To identify prognostic factors in patients with different therapies, univariate and multivariate analyses were, respectively, executed in surgical or nonsurgical groups. In the nonsurgical group (Table 4), univariate analysis indicated that treatment failure might be related to male (P=0.046), PMN >6.30*109/L (P=0.005), and antifungal dosage (P=0.013). Multivariate analysis was constructed using the following variables: male, PMN >6.30*109/L, lesion patterns, and antifungal dosage. Independent predictive factors associated with treatment failure in nonsurgical patients with PC were PMN >6.30*109/L (OR 11.663, 95% CI 2.272–59.879, P=0.003) and antifungal dosage <400mg/d [200–400mg/d (OR 9.576, 95% CI 1.521–60.290, P = 0.016); <200mg/d (OR 20.268, 95% CI 1.651–248.895, P=0.019). In surgical patients (Table 5), treatment failure was probably related to living in the village (P=0.041), Alb <40g/L (P=0.010) and hilar lymphadenopathy (P=0.031). Independent predictive factors associated with treatment failure in surgical patients with PC were living in the village (OR 12.067, 95% CI 1.306–111.517, P=0.028) and Alb <40g/L (OR 20.317, 95% CI 2.237–184.525, P=0.007).
 |
Table 4 Univariate and Multivariate Analysis of Factors Associated with Treatment Failure in 71 Nonsurgical Patients with PC |
 |
Table 5 Univariate and Multivariate Analysis of Factors Associated with Treatment Failure in 92 Surgical Patients with PC |
Discussion
In the current study, 56.4% of enrolled patients underwent lesions resection. Due to local lesion removal and decreased loads of pathogens in the lung, surgery showed instant effects on PC treatment. However, results showed a certain probability of recurrence in single surgical patients without enough antifungal treatment. Furthermore, treatment failure may relate to higher PMN, insufficient antifungal dose, living area and lower Alb. Enough antifungal drug dose and duration might prevent patients from treatment failure, which should be further verified in large prospective studies.
Pulmonary cryptococcosis is an invasive fungal infection caused by inhalation of cryptococci spores, mainly affecting the immunocompromised population.16–18 Recently, the prevalence of PC has been on the rise, and patients are mainly distributed among non-HIV people in China.5,19 The rising prevalence may be caused by two aspects: 1) the increased detection rates of PC as a consequence of the development of medical technology and improvement of people’s health awareness;20 2) the increased rates of PC infection, which may be associated with the aging of the population and the burden of chronic diseases.20–22 In our study, three of 190 cases co-infected HIV and Cryptococcus were excluded, 35.6% of 163 enrolled patients had complications, with diabetes, immunosuppressive therapy and carcinoma being the most common, suggesting that the increasing number of patients was related to the above two reasons. Only two of 190 patients merged extrapulmonary involvement, indicating that systemic spread of primary PC might be rare, supported by Chen et al (34/1142).3
Surgery always occurs in misdiagnosing or excluding malignancy, and it is essential to avoid unnecessary lung resection by further differential diagnosis. The main diagnostic method of our cohort is surgery in the earlier years, and these patients manifested asymptomatic or mild symptoms, accompanied with more limited solitary or multiple nodules/masses in radiology, which heightened the rate of misdiagnosis and following surgical resection.13 The environmental exposures that are acknowledged to be associated with PC, were atypical in our data and more commonly ignored in surgical patients, suggesting that clinicians should pay more attention to patient’s exposure history.10 Moreover, we found that laboratory examinations of ESR, CRP and sCRAG may help distinguish PC and malignancy. There are a large number of capsular polysaccharides released into the blood during Cryptococcus infection; therefore, detection of CrAg in serum samples has emerged as an invaluable tool for the diagnosis of cryptococcal disease.23 In our study, 47 cases received sCRAG tests with a lower positive rate (57.4%, 27/47) compared with most reports,10 which could be due to limited lesions and mild symptoms. Baddley et al24 found that the positive sCRAG test showed a reduced rate in patients with merely pulmonary involvement, which has been further proven by Zhu et al.25 Significantly, positive sCRAG was mostly found in nonsurgical cases, avoiding misdiagnosis and unnecessary lung resection.
The efficiency of surgery for patients with PC may be limited, but it might be helpful for persistent lesions. In a study by Yang et al,13 surgery was thought to effectively treat PC with no need for additional antifungals after complete resection. On the contrary, some scholars found that surgical patients without antifungals showed a higher rate of recurrence or cryptococcal meningitis incidence, inferring that antifungal treatment is indeed necessary.15,26 However, in consideration of the limited sample size in previous studies, the definitive therapy of PC is still controversial. In our study, surgical patients take a shorter time to reach improvement or recovery, and it could be explained by the local lesion removement and decreased loads of pathogens in the lung. Although the surgical patients present better baseline conditions than the nonsurgical group (eg, milder symptoms, limited lesions and good immune status), the rate of progression shows no significant difference between the two groups. Thus, we suspect that the role of single surgery may be limited, but it might decrease loads of Cryptococcus for intractable or persistent lesions after 4 weeks of therapy.27 Moreover, surgery always has high costs and increases risks of surgical morbidities,10 so we hold the opinion that surgery may be unnecessary as the initial therapy of PC.
As the recommended primary therapy, adequate antifungal treatment is crucially important. Some reports10,28 suggest that clinical observation can be justified for asymptomatic immunocompetent individuals, which was thought to be debated by Liu et al.26 Guidelines11 recommend administering fluconazole (400 mg per day orally) for 6–12 months to patients with mild-to-moderate symptoms, while the other expert consensus in China14 recommends administering fluconazole 200–400 mg per day orally for 6 months to asymptomatic cases. Moreover, long-term antifungal therapy has been reported to lead to side effects29,30 and may hinder patient compliance, inducing wild ranges of the antifungal dose and duration in the real world. Our data show that more than half of subjects received fluconazole less than 400 mg per day, which is an independent risk factor of treatment failure of PC, especially for nonsurgical patients. Conversely, sufficient antifungal dose may prevent treatment failure of PC, which can be proved again in the analysis of treatment regimen and outcomes between symptomatic and asymptomatic, immunocompromised and immunocompetent groups. Nevertheless, there is insufficient evidence to indicate whether a duration of more than 6 months is required. Wild range of duration was also observed in the study by Zhang et al10 (2 weeks to 2 years, with a mean of 4.8 months and a median of 3 months) and Liu et al26 (2 weeks to 1.5 years), which showed overall efficiency of 98.68% and 86%, indicating that shorter duration might be available, which should be further verified by large prospective studies. Furthermore, postoperative antifungal treatment was necessary to prevent systemic dissemination when immunocompromised factors persist, lesions rupture during the surgery, the symptoms and signs relapse26 and at least 2 months of antifungal treatment was recommended by the expert consensus in China.14 However, Wei et al15 found that there was no significant difference in the rates of PC recurrence and cryptococcal meningitis occurrence between groups with 2 months’ and more than 2 months’ antifungal treatment. The specific dosage and duration of postoperative antifungal therapy need to be further clarified.
Besides the antifungal dosage discussed above, some risk factors of treatment failure should be paid attention early to improve the prognosis of PC. A high level of PMN is also found as an independent risk factor in the majority of nonsurgical cases, indicating that a higher inflammation level may cause treatment failure. Moreover, a lower level of Alb infers poor baseline condition of patients to prevent Cryptococcus infection, which is independently associated with treatment failure. Furthermore, it could be explained that the poorer prognosis of rural people is due to larger lesions and lower antifungal dosage than that of the citizens. Taken together, we assume that PC patients with poor baseline conditions should be paid more attention. Meanwhile, sufficient antifungal therapy may prevent treatment failure, to some extent filling up the gaps in the previous studies.
There are several limitations in the current study that deserve to be acknowledged. First, the natural limitations of retrospective analysis may introduce the possibility of unrecognized biases. Second, since most cases were admitted in surgery to rule out malignancy, our data consisting of laboratory examinations are not comprehensive, such as sCRAG tests, quantitative immune status, microbiological culture and molecular subtype. Furthermore, the specific regimen of postoperative antifungal drugs needs to be investigated in prospective studies with larger samples.
Conclusion
Pulmonary cryptococcosis showed varied and nonspecific manifestations, leading to a high rate of misdiagnosis and unnecessary lung resection. Serum cryptococcal antigen, which correlated with the extent of the lesions and symptoms, may be instructive for further diagnosis and treatment. Single surgery in PC treatment has limited efficiency and might be used for intractable lesions resection after enough antifungal treatment. Antifungal treatments should not only be considered as primary therapy, but also as necessary postoperatively to prevent recurrence.
Acknowledgments
The authors thank Y. Wu and J. Chen (Department of Radiology, the Second Xiangya Hospital of Central South University, China) for reviewing the radiological images. We appreciate help to review the histological section by D. Li, X. She and Y. Li (Department of Pathology, the Second Xiangya Hospital of Central South University, China).
Funding
This study was supported by the National Natural Science Foundation of China [grant numbers 81873410 and 82070049], the National Key R&D Program of China [grant number 2016YFC1304700], and the Fundamental Research Funds for the Central Universities of Central South University [grant number 2018zzts046].
Disclosure
The authors report no conflicts of interest in relation to this work.
References
1. Chang C, Sorrell T, Chen S. Pulmonary cryptococcosis. Semin Resp Crit Care. 2015;36(05):681–691. doi:10.1055/s-0035-1562895
2. Maliehe M, Ntoi MA, Lahiri S, et al.Cryptococcus neoformans environmental factors that contribute to the maintenance of pathogenesis. Microorganisms. 2020;8(2):180.
3. Yuchong C, Fubin C, Jianghan C, et al. Cryptococcosis in China (1985–2010): review of cases from Chinese database. Mycopathologia. 2012;173(5–6):329–335. doi:10.1007/s11046-011-9471-1
4. Denham S, Brown J. Mechanisms of pulmonary escape and dissemination by Cryptococcus neoformans. J Fungi. 2018;4(1):25. doi:10.3390/jof4010025
5. Wu SX, Guo NR, Li XF. Human pathogenic fungi in China – emerging trends from ongoing national survey for 1986, 1996, and 2006. Mycopathologia. 2011;171(6):387–393. doi:10.1007/s11046-011-9398-6
6. Liu YN, She DY, Sun TY, et al. [A multicentre retrospective study of pulmonary mycosis clinically proven from 1998 to 2007]. Zhonghua Jie He He Hu XI Za Zhi. 2011;34(2):86–90. Chinese.
7. Li SS, Mody CH. Cryptococcus. Proc Am Thorac Soc. 2010;7(3):186–196. doi:10.1513/pats.200907-063AL
8. Liao Y, Chen M, Hartmann T, Yang RY, Liao WQ. Epidemiology of opportunistic invasive fungal infections in China: review of literature. Chin Med J. 2013;126(2):361–368.
9. Ye F, Xie J-X, Zeng Q-S, Chen G-Q, Zhong S-Q, Zhong N-S. Retrospective analysis of 76 immunocompetent patients with primary pulmonary cryptococcosis. Lung. 2012;190(3):339–346. doi:10.1007/s00408-011-9362-8
10. Zhang Y, Li N, Zhang Y. Clinical analysis of 76 patients pathologically diagnosed with pulmonary cryptococcosis. Eur Respir J. 2012;40(5):1191–1200. doi:10.1183/09031936.00168011
11. Perfect JR, Dismukes WE, Dromer F, et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis. 2010;50(3):291–322. doi:10.1086/649858
12. Taniwaki M, Yamasaki M, Ishikawa N, Kawamoto K, Hattori N. Pulmonary cryptococcosis mimicking lung cancer. Lancet Infect Dis. 2019;19(9):1033. doi:10.1016/S1473-3099(19)30278-6
13. Yang B, Lee H, Lee T, et al. The use of surgery in a real-world clinic to diagnose and treat pulmonary cryptococcosis in immunocompetent patients. J Thorac Dis. 2019;11(4):1251–1260. doi:10.21037/jtd.2019.04.17
14. Diseases ZMAS. Expert consensus on diagnosis and treatment of pulmonary cryptococcosis. Chin J Clin Infect Dis. 2017;10(5):321–326.
15. Wei S, Su X, Pan YH, et al.Postoperative antifungal treatment of pulmonary cryptococcosis in non-HIV-infected and non-transplant-recipient patients: a report of 110 cases and literature review. Open Forum Infect Dis. 2020;7(1):a4.
16. Kiertiburanakul S, Wirojtananugoon S, Pracharktam R, Sungkanuparph S. Cryptococcosis in human immunodeficiency virus-negative patients. IJID. 2006;10(1):72–78. doi:10.1016/j.ijid.2004.12.004
17. Marr KA, Sun Y, Spec A. A multicenter, longitudinal cohort study of cryptococcosis in human immunodeficiency virus-negative people in the United States. Clin Infect Dis. 2020;70(2):252–261. doi:10.1093/cid/ciz193
18. Bandalizadeh Z, Javidnia J, Hosseini SA. Cryptococcus and cryptococcosis in Iran during 1969–2019: a systematic review and meta-analysis. J Mycol Med. 2020;30(1):100917. doi:10.1016/j.mycmed.2019.100917
19. Chen J, Varma A, Diaz MR, Litvintseva AP, Wollenberg KK, Kwon-Chung KJ. Cryptococcus neoformans strains and infection in apparently immunocompetent patients, China. Emerg Infect Dis. 2008;14(5):755–762. doi:10.3201/eid1405.071312
20. Roth GA, Abate D, Abate KH, et al.Global, regional, and national age-sex-specific mortality and life expectancy, 1950–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1684–1735. doi:10.1016/S0140-6736(18)31891-9
21. Zhou M, Wang H, Zeng X. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;394(10204):1145–1158. doi:10.1016/S0140-6736(19)30427-1
22. Roberts NL, Mountjoy-Venning WC, Anjomshoa M, Banoub JA, Yasin YJ. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–1858. doi:10.1016/S0140-6736(18)32279-7
23. McFadden D, Zaragoza O, Casadevall A. The capsular dynamics of Cryptococcus neoformans. Trends Microbiol. 2006;14(11):497–505. doi:10.1016/j.tim.2006.09.003
24. Baddley JW, Perfect JR, Oster RA, et al. Pulmonary cryptococcosis in patients without HIV infection: factors associated with disseminated disease. Eur J Clin Microbiol. 2008;27(10):937–943. doi:10.1007/s10096-008-0529-z
25. Zhu T, Luo WT, Chen GH, et al. Extent of lung involvement and serum cryptococcal antigen test in non-human immunodeficiency virus adult patients with pulmonary cryptococcosis. Chin Med J. 2018;131(18):2210–2215. doi:10.4103/0366-6999.240815
26. Liu K, Ding H, Xu B. Clinical analysis of non-AIDS patients pathologically diagnosed with pulmonary cryptococcosis. J Thorac Dis. 2016;8(10):2813–2821. doi:10.21037/jtd.2016.10.36
27. La Hoz RM, Pappas PG. Cryptococcal infections: changing epidemiology and implications for therapy. Drugs. 2013;73(6):495–504. doi:10.1007/s40265-013-0037-z
28. Aberg JA, Mundy LM, Powderly WG. Pulmonary cryptococcosis in patients without HIV infection. Chest. 1999;115(3):734–740. doi:10.1378/chest.115.3.734
29. Davis MR, Nguyen MH, Donnelley MA, Thompson GR. Tolerability of long-term fluconazole therapy. J Antimicrob Chemoth. 2019;74(3):768–771. doi:10.1093/jac/dky501
30. Xu SX, Shen JL, Tang XF, Feng B, Xu HQ. Newer antifungal agents micafungin and voriconazole for fungal infection prevention during hematopoietic cell transplantation: a meta-analysis. Eur Rev Med Pharma. 2016;20(2):381–390.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

