Back to Journals » Research Reports in Clinical Cardiology » Volume 5
Fluctuant tonus of the coronary arteries possibly documented by repeated multidetector row computed tomography
Authors Anan I, Hongo K, Kawai M, Ogawa K, Sakuma T, Fukuda K, Taniguchi I, Yoshimura M
Received 8 August 2014
Accepted for publication 2 September 2014
Published 26 November 2014 Volume 2014:5 Pages 327—337
DOI https://doi.org/10.2147/RRCC.S72464
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Kones
Ikuko Anan,1 Kenichi Hongo,1 Makoto Kawai,1 Kazuo Ogawa,1 Toru Sakuma,2 Kunihiko Fukuda,2 Ikuo Taniguchi,1 Michihiro Yoshimura1
1Division of Cardiology, Department of Internal Medicine, 2Department of Radiology, The Jikei University School of Medicine, Tokyo, Japan
Objective: Recent advances in multidetector row computed tomography (MDCT) have made it possible to diagnose coronary stenosis with high sensitivity. However, coronary arterial tonus has not been considered when reading MDCT. We hypothesized that MDCT can document fluctuant tonus of the coronary arteries.
Methods: The study population consisted of 39 consecutive patients who underwent MDCT twice in our institution with 64-row dual-source MDCT. Measurements were performed with stretched multiplanar reconstruction images using the full width at half maximum method. The coronary arteries were measured at each segment, and the same measurement was performed in the ascending aorta and the left internal thoracic artery (ITA). The percent diameter changes between the first and second measurements were examined in each segment of the coronary arteries and compared with those in the aorta or the ITA.
Results: The average percent diameter changes were statistically equivalent between the coronary arteries and the aorta or the ITA. On the other hand, the percent diameter changes in distribution were significantly larger in the coronary arteries than those in the aorta or the ITA. This suggests that the diameter of the coronary arteries is liable to show variation compared to that of other arteries.
Conclusion: This study confirmed for the first time that coronary arteries can fluctuate substantially and that these changes can be documented by MDCT. Changes in coronary arterial tonus should therefore be considered when reading MDCT.
Keywords: coronary spastic angina, coronary arterial tonus, false positive study
Introduction
For the diagnosis of organic stenosis in the coronary arteries, coronary angiography is the gold standard because it allows for the accurate detection of narrowing in each coronary arterial segment. Recent advances in multidetector row computed tomography (MDCT) have made it possible to use it for the diagnosis of coronary stenosis for the same purpose, with high sensitivity and specificity, nearly equivalent to that of the invasive coronary angiography, although there have sometimes been discrepancies in the findings between coronary angiography and MDCT examinations.1–8 MDCT is also used to estimate anatomical changes or tissue volumes in various organs.9–11
Coronary spasm is an important cause of ischemic heart disease in general, and is especially common in Asian countries, including Japan.12–14 Coronary artery spasm is difficult to detect by MDCT examination because of its special characteristics.13 For example, coronary spasm transiently occurs most often from midnight to the early morning, and least often in the afternoon, due to the circadian variation of the tone of the large coronary artery in most patients with coronary spastic angina. However, we recently found two cases that showed severe coronary spasm detected by chance with MDCT examination.15,16 After these reports, we found similar cases during usual clinical practice, and hypothesized that these cases might not be so rare. We further hypothesized that the coronary artery tonus might be dynamically changed or fluctuate in patients with ischemic heart disease in general, and that these changes may not be limited to patients with coronary spasm definitely diagnosed by the intracoronary acetylcholine infusion test and other methods.
MDCT has recently become a very sensitive modality for detecting the coronary arterial diameter, and it could possibly detect the coronary artery tonus to some extent, although it has been considered that the MDCT examination is not a suitable method for evaluating the coronary tonus.16 In order to define whether fluctuation of the coronary artery tonus can be detected by MDCT examination, we retrospectively compared the changes in the coronary artery diameter with those in other arterial diameters by serial measurements with MDCT examinations.
Methods
Study population
Among 2,940 patients who underwent MDCT examinations between June 2007 and February 2009 at Jikei University Hospital using the following modality, this study retrospectively evaluated 39 consecutive patients who were examined twice at different times by chance. MDCT was performed in these patients because of a suspicion of angina pectoris due to clinical symptoms, electrocardiogram (ECG) changes, blood biochemical findings, and other reasons, and because of the follow-up analyses needed after percutaneous coronary intervention. The timing of the MDCT examination was decided by each attending physician for individual patients. Patients with coronary bypass surgery, acute coronary syndrome, Kawasaki disease, renal dysfunction (serum creatinine ≥1.5 mg/dL), allergies to contrast medium, or in unstable hemodynamic condition were excluded from this study. For the diagnosis by MDCT examination, written informed consent was provided by all of the patients studied. This study conformed to the ethical guidelines of the 1975 Declaration of Helsinki, as reflected in the a priori approval by the institution’s human research committee (approval number: 22-192 6369).
Protocol for MDCT examination
We used a 64-row dual-source MDCT (Somatom Definition; Siemens Healthcare, Erlangen, Germany) for the evaluation of coronary arteries in the present study.3,4,17 This MDCT was equipped with two X-ray tubes and two corresponding detectors, which were mounted onto a rotating gantry with an angular offset of 90°, and which provides high temporal and spatial resolutions. The patients were centrally placed in the scanner to ensure that the entire heart was covered by the smaller field of view of the second tube detector array. Coronary computed tomography (CT) angiography was performed with a collimation of 32 mm×0.6 mm, a slice acquisition of 64 mm×0.6 mm by means of a Z-flying focal spot, a gantry rotation time of 330 ms, a helical pitch of 0.20–0.39 adapted to the heart rate (from 38 to 95 bpm [64.2±11.4 bpm]), tube current of 80 mAs per rotation, and tube potential of 120 kV. For the contrast-enhanced scan, 0.7 mL/kg of contrast media (iopamidol, 370 mg/mL; Bayer AG, Leverkusen, Germany) was injected at 0.07 mL/kg/second (the lower limit was 3.5 mL/second and the upper limit was 5.0 mL/second), followed by 30 mL of normal saline. Nitroglycerin inhalation was used for all patients, except for those who had systolic blood pressure <100 mmHg (four patients). We did not newly initiate the use of a beta-blocker for MDCT examination, irrespective of the patients’ heart rate. The start timing was automatically defined using a bolus tracking program, and the image acquisition began when the CT density reached the threshold value (120 Hounsfield units) at the base of the aorta. All scans were performed during a single breath hold. The scanned data were reconstructed using algorithms optimized for retrograde ECG-gated reconstruction in diastole. The reconstructed image data were transferred to a commercially available workstation (Aquarius NetStation iNtuition Edition; TeraRecon, Inc., San Mateo, CA, USA) for further analysis.
Estimation of the arterial diameters with MDCT
In individual patients, coronary artery segments were defined according to the 15-segments model widely accepted for the American Heart Association classification.18 We then evaluated two segments in the right coronary artery (#1, ostium lesion; and #3, just before the branching posterolateral artery), left main trunk (#5, prior to the left descending artery), four segments in the left anterior descending artery (#6, just after the circumflex artery; #7, just after the branching of the first diagonal artery; #8, just after the branching of the second diagonal artery; and #9, the first diagonal artery just after the branching from the left descending artery), and two segments in the left circumflex artery (#11, just after the branching the left descending artery; and #13, just after the branching of the obtuse marginal). Measurements were performed with stretched multiplanar reconstruction cross-section images in each segment using the full width at half maximum (FWHM) method, which was validated previously.17,19 In brief, along the central line of the cross-section images, the profile of the CT density was constructed, and the FWHM of the profile was automatically determined as the diameter (Figure 1).
Coronary arterial segments with stent implantation, marked plaque formation, and calcification were excluded from the measurement. The diameters of the left internal thoracic artery (ITA) (almost the same height as the left main trunk) and the aorta (almost at the sinotubular junction) were also measured using the same method as was used for the coronary arteries. Careful attention was paid to measure the diameter of exactly the same portion of the coronary artery in the two MDCT examinations. In individual patients, the changes in the diameter of the arteries between the first and the second MDCT examinations were calculated for each coronary artery segment. For the aorta and ITA, the diameter was calculated in the same way.
The change in the arterial diameter (%) was calculated according to Equation 1:
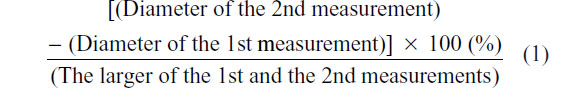
Similarly, the absolute value of the diameter change (%) in each segment of the coronary artery was calculated using the value obtained from Equation 1.
Statistical analysis
All the data were expressed as the means ± standard error of the mean. Continuous variables were analyzed using Student’s t-test, and the frequency distributions of these values were compared using the F-test in the statistical analyses. Categorical data were analyzed using the chi-square test, with the significance level set at P<0.05. All of the statistical analyses were performed using the IBM SPSS software program, version 22 (IBM Corporation, Armonk, NY, USA).
Results
Patient characteristics
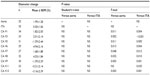
The baseline characteristics of the 39 study patients are summarized in Table 1. The average time elapsed between the first and the second MDCT examinations was 318±121 days (74–610 days). Table 2 shows the medications that the patients were receiving at the first and second MDCT examinations (see Table S1, which demonstrated the details of the medications being administered to each patient).
  | Table 1 The patient characteristics |
Representative images of coronary artery and ITA from the first and the second MDCT examinations
Figure 2A shows the typical findings of representative coronary diameter changes. Figure 2Aa and Ab show the longitudinal and cross-sectional images of the coronary (circumflex) artery from the first MDCT examination. The cross-sectional image was constructed at the portion indicated by a white bar. Figure 2Ac and Ad show the longitudinal and cross-sectional images of the coronary artery from the second MDCT examination in the same patient. The coronary diameters were clearly changed between the first and second examinations in this patient.
Figure 2B shows the representative images of the ITA diameter in the same patient as Figure 2A. Figure 2Ba and Bb show the longitudinal and cross-sectional images of the ITA from the first MDCT examination, and Figure 2Bc and Bd show the longitudinal and cross-sectional images from the second MDCT examination. The ITA diameter was similar between the first and second examinations.
Raw data of the changes in coronary artery diameter among all patients
Figure 3 shows the average changes in coronary artery diameter for all 39 patients. The percent diameter changes in the aorta, the ITA, and the coronary arteries (#1, 3, 5, 6, 7, 8, 9, 11, 13) are presented (see Figure S1, which demonstrates the raw data for all patients).
Comparison of the average and distribution of the arterial diameter changes among the aorta, ITA, and coronary arteries
Table 3 shows a summary of the changes in the diameters of the aorta, ITA, and coronary arteries between the first and second MDCT examinations. There were no significant differences in the averages evaluated between the aorta and the coronary arteries, or between the ITA and the coronary arteries, as evaluated by Student’s t-test. On the other hand, there was a significant difference in the distribution between the aorta and the coronary arteries, and between the ITA and the coronary arteries in most of the segments, as determined by the F-test. There were only two exceptions at coronary artery #7 and #11 versus the aorta. This result suggests that the diameter of the coronary arteries is more liable to show variation when compared to that of the aorta or the ITA.
Absolute changes in each coronary artery segment
To make the findings easier to understand, Figure 4 shows the absolute changes in the diameter of the aorta, ITA, and coronary arteries. These analyses showed that the absolute change of the diameter was significantly larger in the coronary arteries than in the aorta or in the ITA in most of the segments of the coronary arteries.
Discussion
The main findings of the present study are: 1) that MDCT could detect the changes in the coronary artery diameter; and 2) that the changes in the coronary arteries were significantly larger than those in the aorta or the ITA, suggesting that the coronary arteries would be expected to show large fluctuations.
The study population included consecutive patients who underwent MDCT examinations twice because of suspected angina pectoris or as a follow-up examination after percutaneous coronary intervention, including only two patients with a definite diagnosis of coronary spasm (patient numbers 26 and 32). Therefore, the present results suggest that coronary artery tonus is liable to exhibit variation in patients with ischemic heart disease in general. This result may support the idea that coronary spasm widely contributes to the pathogenesis of many kinds of ischemic heart disease in the Japanese population, which may be different from what is found in Western countries.13
MDCT examination can currently be used for the diagnosis of atherosclerotic organic stenosis. In previous studies, there was a relatively high rate of “false positive” detection of organic stenosis with MDCT examination when compared to that observed by coronary angiography.4,20–23 The reasons were thought to be due to the high sensitivity of the MDCT examination to calcification, atherosclerotic changes, movement artifacts, or other types of artifacts. However, the current study shows that organic stenosis examined with MDCT would be overestimated if it was not taken into account that the coronary tonus was enhanced, which might be another reason for the “false positive” results of the MDCT examinations.
In the study patients, the attending physicians of the individual patients carefully selected the drugs and changed them according to the patients’ condition, such as based on the patients’ clinical symptoms, blood pressure, heart rate, side effects, and other findings. The drugs being taken were thus naturally diverse among the study patients, and between the first and second MDCT examinations. All arteries in the body, including the aorta, the ITA, and the coronary arteries, would be simultaneously exposed to the drugs. Thus, the main finding of the present study that the coronary artery fluctuates more when compared to the other arteries is not due to drug effects. We found that six patients were taking different potentially relevant drugs between the first and second MDCT examinations. We therefore reanalyzed the data after excluding these patients, but reached a similar conclusion as had been obtained with the original analysis, especially when comparing the ITA (Table S2). Nitroglycerin inhalation was used for coronary dilation before the MDCT examination in all patients, except for those who had systolic blood pressure <100 mmHg (four patients). We also reanalyzed the data without these patients, and these data were also similar to those for all patients (Table S3). Therefore, coronary tonus changes could be detected in this study even in the presence of various drugs.
The changes in coronary artery diameter estimated by MDCT examination cannot be thought to be a result of atherosclerotic progression or regression because the elapsed time between the first and second measurements was relatively short (318±121 days), and because positive and negative changes in values were mixed in individual patients (Figure S1). Therefore, it is reasonable to conclude that the present results indicate that the changes in diameter were due to differences in the coronary arterial tonus.
Limitations of the study
Although we excluded arterial segments with marked plaque formation and calcification from the measurement, the present results might have been affected by the changes in coronary atherosclerosis between the first and second measurements. This study was performed with a retrospective analysis, involving a limited number of patients diagnosed with or suspected to have ischemic heart disease, and we included patients with previous myocardial infarction, in whom atherosclerosis might have been progressive. This could have led to some selection bias in the study population.
Conclusion
The coronary artery diameter was dynamically changed and had fluctuated in patients with ischemic heart disease in general. MDCT can detect these changes. Coronary arterial tonus changes should therefore be taken into consideration when examining MDCT findings in patients with ischemic heart disease.
Disclosure
The authors report no conflicts of interest in this work.
References
Ohnuki K, Yoshida S, Ohta M, et al. New diagnostic technique in multi-slice computed tomography for in-stent restenosis: pixel count method. Int J Cardiol. 2006;108(2):251–258. | |
Hamon M, Morello R, Riddell JW, Hamon M. Coronary arteries: diagnostic performance of 16- versus 64-section spiral CT compared with invasive coronary angiography – meta-analysis. Radiology. 2007;245(3):720–731. | |
Leber AW, Johnson T, Becker A, et al. Diagnostic accuracy of dual-source multi-slice CT-coronary angiography in patients with an intermediate pretest likelihood for coronary artery disease. Eur Heart J. 2007;28(19):2354–2360. | |
Piers LH, Dikkers R, Willems TP, et al. Computed tomographic angiography or conventional coronary angiography in therapeutic decision-making. Eur Heart J. 2008;29(23):2902–2907. | |
Budoff MJ, Dowe D, Jollis JG, et al. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J Am Coll Cardiol. 2008;52(21):1724–1732. | |
Motoyama S, Sarai M, Harigaya H, et al. Computed tomographic angiography characteristics of atherosclerotic plaques subsequently resulting in acute coronary syndrome. J Am Coll Cardiol. 2009; 54(1):49–57. | |
Hassan A, Nazir SA, Alkadhi H. Technical challenges of coronary CT angiography: today and tomorrow. Eur J Radiol. 2011;79(2):161–171. | |
Bischoff B, Meinel FG, Del Prete A, Reiser MF, Becker HC. High-pitch coronary CT angiography in dual-source CT during free breathing vs breath holding in patients with low heart rates. Eur J Radiol. 2013;82(12):2217–2221. | |
Cao K, Ding K, Christensen GE, Reinhardt JM. Tissue volume and vesselness measure preserving nonrigid registration of lung CT images. Proc SPIE. 2010;7623:762309. | |
Tozaki M, Kobayashi T, Uno S, et al. Breast-conserving surgery after chemotherapy: value of MDCT for determining tumor distribution and shrinkage pattern. AJR Am J Roentgenol. 2006;186(2):431–439. | |
Takao H, Murayama Y, Otsuka S, et al. Hemodynamic differences between unruptured and ruptured intracranial aneurysms during observation. Stroke. 2012;43(5):1436–1439. | |
Yasue H, Horio Y, Nakamura N, et al. Induction of coronary artery spasm by acetylcholine in patients with variant angina: possible role of the parasympathetic nervous system in the pathogenesis of coronary artery spasm. Circulation. 1986;74(5):955–963. | |
Yasue H, Nakagawa H, Itoh T, Harada E, Mizuno Y. Coronary artery spasm – clinical features, diagnosis, pathogenesis, and treatment. J Cardiol. 2008;51(1):2–17. | |
Beltrame JF, Sasayama S, Maseri A. Racial heterogeneity in coronary artery vasomotor reactivity: differences between Japanese and Caucasian patients. J Am Coll Cardiol. 1999;33(6):1442–1452. | |
Ito K, Ogawa T, Yoshimura M. Severe coronary spasm occasionally detected by coronary computed tomography. Eur Heart J. 2009;30(22):2768. | |
Ota M, Anan I, Morimoto S, et al. Severe lasting coronary spasm detected by multi-detector row computed tomography. Int J Cardiol. 2011;153(3):e62–e64. | |
Flohr TG, McCollough CH, Bruder H, et al. First performance evaluation of a dual-source CT (DSCT) system. Eur Radiol. 2006;16(2):256–268. | |
Austen WG, Edwards JE, Frye RL, et al. A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation. 1975; 51(Suppl 4):5–40. | |
Steen H, André F, Korosoglou G, et al. In vitro evaluation of 56 coronary artery stents by 256-slice multi-detector coronary CT. Eur J Radiol. 2011;80(1):143–150. | |
Mowatt G, Cook JA, Hillis GS, et al. 64-Slice computed tomography angiography in the diagnosis and assessment of coronary artery disease: systematic review and meta-analysis. Heart. 2008;94(11):1386–1393. | |
Tsiflikas I, Brodoefel H, Reimann AJ, et al. Coronary CT angiography with dual source computed tomography in 170 patients. Eur J Radiol. 2010;74(1):161–165. | |
Soon K, Wong C. Coronary computed tomography angiography: a new wave of cardiac imaging. Intern Med J. 2012;42 Suppl 5:22–29. | |
Yan RT, Miller JM, Rochitte CE, et al. Predictors of inaccurate coronary arterial stenosis assessment by CT angiography. JACC Cardiovasc Imaging. 2013;6(9):963–972. |
Supplementary materials
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.