Back to Journals » International Journal of General Medicine » Volume 15
Flexible Bronchoscope versus Video Laryngoscope for Orotracheal Intubation During Upper Gastrointestinal Endoscopic Surgery in Left Lateral Position: A Randomized Controlled Trial
Authors Shen W, Cai X, Liu X, Zhang Z , Wang X, Yu A
Received 16 March 2022
Accepted for publication 28 June 2022
Published 8 July 2022 Volume 2022:15 Pages 6097—6104
DOI https://doi.org/10.2147/IJGM.S366020
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Wenlong Shen, Xingzhi Cai, Xiaohui Liu, Zongwang Zhang, Xuxiang Wang, Ailan Yu
Department of Anesthesiology, Liaocheng People’s Hospital, Liaocheng, Liaocheng, Shandong, People’s Republic of China
Correspondence: Ailan Yu; Xingzhi Cai, Department of Anesthesiology, Liaocheng People’s Hospital, Liaocheng, Shandong, 252000, People’s Republic of China, Tel +86 13563530309, Email [email protected]; [email protected]
Purpose: Endoscopic submucosal dissection (ESD) has become the primary treatment for early upper gastrointestinal tract lesions. During endoscopic surgery, endotracheal intubation is generally performed in the patients’ supine position, and patients are shifted to the left lateral position for endoscopic surgery. This study compared the efficacy of flexible bronchoscope-guided intubation with that of video laryngoscope-guided intubation in the left lateral position.
Patients and Methods: Forty-eight patients receiving ESD were randomly divided into the flexible bronchoscope group (group F) or the video laryngoscope group (group V). Tracheal intubation was performed by a trained anesthetist with a flexible bronchoscope (group F) or unchanneled video laryngoscope (group V) in the left lateral position. Primary outcomes included the intubation duration and success rate. Secondary outcomes included the ease of intubation technique and the occurrence of complications.
Results: Twenty-four (100%) patients in group F and twenty-three (95.8%) in group V were successfully intubated (P = 1.000). The median intubation time in group F was 37s (interquartile range, 33.0, 44.5), which was significantly shorter compared to group V (53s [45.5, 66.5]; P < 0.001). The flexible bronchoscope was significantly easier to manage than the video laryngoscope, as reflected by the users scoring system (9 [9, 10] vs 8 [7, 8]; P < 0.001). The presence of perioperative adverse events and complications were comparable between the two groups.
Conclusion: Both flexible bronchoscope- and video laryngoscope-guided intubation in patients’ left lateral position achieved high success rates and comparable complication rates. However, intubation with the flexible bronchoscope was completed more quickly.
Keywords: intubation, bronchoscope, laryngoscope, endoscopic submucosal dissection, left lateral position
Introduction
The advances in endoscopic equipment have propelled endoscopic techniques in disease diagnosis and treatment. As a result, endoscopic submucosal dissection (ESD) is widely used as the primary approach for gastrointestinal disorders. Compared with traditional surgery, ESD is superior in preserving native organs, minor trauma, quick recoveries, short hospital stays, and lower complication rates.1–3 General anesthesia with endotracheal intubation is the preferred anesthetic method for ESD, as it can maintain the airway patency, reduce gastric reflux and pulmonary aspiration risk, and provide good operative conditions for endoscopists.3
During endoscopic surgery, endotracheal intubation is generally performed on patients in the supine position, and then they are shifted to the left lateral position, which is required for endoscopic surgery. However, it is unsafe to change the patient’s position after the induction of anesthesia. Intubation in the left lateral position avoids the need to change the patients’ position, decreases the stress reaction and physiological interference caused by the patient’s position shift, and reduces the required time and workforce.4 Furthermore, endotracheal intubation may also be necessary in many emergency circumstances, such as accidental extubation during surgery when the patient is already in the lateral position, which is potentially hazardous.5
The poor glottic view and uncomfortable intubation position in the left lateral position increase the difficulty of endotracheal intubation by Macintosh laryngoscope and reduce the successful intubation rate.6 With the implementation of many intubation-assisting optical devices, such as intubating laryngeal mask airway,7 lightwand,8 and video laryngoscope,9,10 endotracheal intubation in the lateral position has become more feasible.7,8,11,12 The flexible bronchoscope, with the flexibility of the insertion tube and the ability to look around the corner during intubation, can flexibly guide the tracheal tube into the airway. Therefore, the flexible bronchoscope was recommended as the gold standard during anticipated complex airway management.13 Furthermore, for patients already under anesthesia, orotracheal intubation with the flexible bronchoscope in the lateral position was more effective and time-saving than in the supine position.14 Thus, it was hypothesized that flexible bronchoscope-guided endotracheal intubation is advantageous over the video laryngoscope for patients in the lateral position. Therefore, this work explored the safety and effectiveness of intubation with flexible bronchoscopes for ESD surgery with patients in the left lateral position and evaluated the potential advantages of the flexible bronchoscope over the video laryngoscope.
Patients and Methods
Trial Design
This investigation was a prospective, randomized controlled study conducted in Liaocheng People’s Hospital between June 2020 and August 2020. The study was approved by the Ethics Committee of Liaocheng People’s Hospital (2020018) and was registered at the Chinese Clinical Trial Register (ChiCTR 2000033840). In addition, written informed consent was obtained from all participants. The same skilled anesthesiologist performed all endotracheal intubations with the flexible bronchoscope and video laryngoscope with patients in the lateral position.
Participants
The study population comprised all patients receiving ESD surgery in the left lateral position. The exclusion criteria included: age > 80 years; American Society of Anesthesiologists (ASA) physical status score > III; high-risk airway (such as Mallampati score > III, mouth opening < 3 cm, BMI > 30 kg/m2, cervical spine abnormality, severe maxillofacial deformity.); and presence of an acute respiratory infection.
Randomization and Blinding
A total of 48 patients were included in this study. The patients were randomly allocated into the video laryngoscope group (group V) or the flexible bronchoscope group (group F) in a 1:1 ratio using the sealed envelope method. The random sequence was generated by a computer. All patients were blinded to their grouping, and the intubation operator was not involved in observations, documentation, and evaluations of outcome events.
General Anesthesia and Endotracheal Intubation
None of the patients received preoperative medication. Before intubation, the patients were supine on the operating table, and their heart rate, noninvasive blood pressure, oxygen saturation (SpO2), and bispectral index (BIS) were monitored. Next, the patients were asked to shift to the left lateral position. A pillow was used to support the head and neck to maintain the natural horizontal position of the patients’ spines during anesthesia induction and intubation. A disposable mouthpiece was placed between the incisor teeth to keep the mouth open before anesthesia induction in group F. After preoxygenation, general anesthesia was induced by intravenous administration of midazolam (0.03 mg/kg), propofol (1.5–2.0 mg/kg), fentanyl (2 μg/kg), and cisatracurium (0.15–0.2 mg/kg). Then, manual ventilation was maintained for approximately 3 min with 100% oxygen through a face mask, followed by intubation. In group V, the anesthetist performed the oral endotracheal intubation using the unchanneled video laryngoscope (E.An-II; Tianjin Median Medical Electronic Technology Co. Ltd., Tianjin, China) with the assistance of an intubation stylet. The position of the patient’s head and neck was adjusted as necessary. In group F, the oral endotracheal intubation was performed using the flexible bronchoscope (TIC-SD-Ш; Zhejiang UE Medical Instrument Co., LTD, Zhejiang, China). The assistant applied the jaw-thrust maneuver if necessary. Reinforced tracheal tubes (7.0 mm internal diameter for men and 6.5 mm for women) were used for all patients.
During endotracheal intubation, if the patient’s SpO2 dropped below 90%, the intubation was paused immediately, and face mask-assisted ventilation was performed to raise the SpO2 to 100%. Meanwhile, the intubation was considered a failure and repeated with the patient in the lateral position. If two intubation attempt failures occurred, the patient was placed in a supine position to complete the endotracheal intubation, which was recorded as an intubation failure. The duration of the first and second (if applicable) and the overall intubation process were recorded by the assistant using a timer. Intubation time was defined as the time from the mask leaving the patient’s face to the exit of the flexible bronchoscope or video laryngoscope after the catheter was successfully inserted into the trachea. After intubation, anesthesia was maintained with sevoflurane (2–3%) and remifentanil (0.1–0.3 μg/kg/min). The respiratory frequency was set to 12–15 breaths/min, and the tidal volume to 6–8 mL/kg. The BIS was maintained at 40–60, and the end-tidal CO2 (PETCO2) at 35–40 mmHg.
Study Outcomes
The primary outcomes included the overall intubation duration and the success rates of the first attempt, the second attempt, and the overall intubation. The secondary outcomes included the ease of the intubation technique (10 grades: 1 = very poor, 10 = excellent), and the presence of intubation-dependent complications (oral mucosal injury, dental injury, hypoxemia [SpO2 < 90%], and esophageal intubation).
Sample Size Prediction
The minimum sample size was estimated based on intubation time. In the pilot study of 15 patients, the mean and standard deviation (SD) of intubation durations were 46.0 ± 8.53 sec and 65.22 ± 12.64 sec in groups F and V, respectively. The estimated sample size was calculated using a two-group chi-square test with a statistical power of 80% and a two-sided significance of 0.05. Based on an estimated 10% dropout rate, 24 patients were required in each group.
Statistical Analysis
SPSS software (version 23.0, IBM Corp., Armonk, NY, USA) was used for data analysis. The Shapiro–Wilk test was used to test the normality of continuous variables. Continuous variables were expressed as the mean ± SD and compared using the Student’s t-test if they were normally distributed or described as median (interquartile range [IQR]) or the Mann–Whitney U-test if they were non-normally distributed. Categorical variables are presented as counts (percentage, %) and were compared using the Chi-squared test or Fisher’s exact test as appropriate. All statistical tests were two-sided. A value of P less than 0.05 was considered statistically significant.
Results
Study Population
Among the 53 patients enrolled in the trial, five patients were excluded due to the following reasons: patients over 80 years of age (one case), acute upper respiratory tract infection (one case), and refused to join the trial (three cases). Consequently, 48 patients were included for data analysis, with 24 in each group (Figure 1).
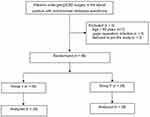 |
Figure 1 Flow diagram of the study. Group F: flexible bronchoscope group; Group V: video laryngoscope group. Abbreviation: ESD, endoscopic submucosal dissection. |
Demographic and Clinical Characteristics
No significant differences were observed between groups V and F regarding demographic and patient clinical characteristics, including age, height, body weight, ASA grade, and Mallampati score (Table 1).
 |
Table 1 Demographic and Clinical Assessment Data |
Intubation Status
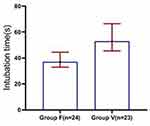
A total of 24 (100%) patients in group F and 23 (95.8%) in group V were successfully intubated. The overall success rates between the two groups were comparable (P = 1.000; Table 2). Notably, the results showed that the median intubation time in group F was 37s (IQR: 33.0, 44.5), which was significantly shorter than that in group V (53 s [IQR: 45.5, 66.5]; P < 0.01; Figure 2). Moreover, in group V, one patient (4.2%) was successfully intubated during the second attempt by adjusting the tracheal tube molding after the initial failure. Furthermore, one patient (4.2%) was successfully intubated in the supine position after two failed intubation attempts in the lateral position. Therefore, the success rate of the first intubation was 100% in group F and 91.7% in group V (P = 0.234; Table 2). In addition, the user’s evaluation revealed that the flexible bronchoscope was significantly more manageable than the video laryngoscope (9 [9, 10] vs 8 [7, 8]; P < 0.001; Table 2).
 |
Table 2 Success Rates and the User’s Evaluation in Both Groups |
Complications and Adverse Events
During the trial, two (8.3%) cases of intubation-related oral mucosal injury were reported in group V, but no cases were noted in group F. No dental injury cases were found in either group. In addition, at the first intubation attempt, hypoxemia occurred in the two failed intubation cases, and oxygen saturation was recovered upon its immediate supply. Moreover, the analysis revealed no significant difference in perioperative adverse events or complications between the two groups (P > 0.05; Table 3).
 |
Table 3 Complications and Adverse Events |
Discussion
This study investigated the advantage of endotracheal intubation under the guidance of a flexible bronchoscope over that of a video laryngoscope for patients in the left lateral position for ESD surgery. This study did not find significant differences in complications or adverse events caused by endotracheal intubation guided by either of the two intubation tools. The results also suggested that flexible bronchoscope- and video laryngoscope-guided intubation achieved more than 95% success rates. However, it should not be omitted that the duration of flexible bronchoscope-assisted intubation was significantly less than that of the video laryngoscope. More importantly, this study further revealed that endotracheal intubation guided by a flexible bronchoscope is safer and easier to use.
Although unconventional in clinical practice, endotracheal intubation in the lateral position is particularly valuable for perioperative airway management, such as establishing artificial airways for patients in restricted positions, sudden respiratory depression, and accidental loss of the tracheal tube during an operation.5,15–17 Meanwhile, endotracheal intubation in the lateral position is safer for patients with a full stomach since the peak inspiratory pressure of mask ventilation in the lateral decubitus position is lower than in the supine position,12,17,18 and oropharyngeal secretions are easier to clear. In addition, endotracheal intubation in the lateral decubitus position may avoid related complications caused by position change and save time and the workforce needed to move patients.
In this trial, performing endotracheal intubation with the flexible bronchoscope (37.0 s [33.0, 44.5]) was faster compared to the video laryngoscope (53.0 s [45.5, 66.5]) in the left lateral position. On the other hand, Wahdan et al19 compared elective endotracheal intubation in the lateral position using the laryngoscopic-assisted video stylet with the fiberoptic bronchoscope. They found that the average time taken for intubation was significantly less in the video stylet group (39.5 ± 10.0 s) than in the fiberoptic bronchoscope group (75.6 ± 16.2 s). Two considerations may explain these contradictory results. First, the video stylet was different from the laryngoscope; during intubation with the video stylet, the endotracheal tube could be placed over the stylet before the timer started, which might shorten the time. Second, a mouthpiece rather than an assistant was used in this study to keep the patient’s mouth open. Single-person intubation (no assistant was needed in group F) saved communication time between operators and likely made the operation more convenient.
Of note, previous studies have demonstrated that the video laryngoscope could provide a better laryngoscopic view, a high success rate, and a shorter intubation time in a lateral position than the Macintosh laryngoscope.9,11 As the most widely used intubation-assisting tool in clinical practice, a video laryngoscope can significantly reduce the airway grading since its visual technology makes the laryngoscope blade more consistent with the physiological curvature of the pharynx. Some scholars have even proposed video laryngoscopy as the standard tool for intubation.20 However, in this study, the success rate of video laryngoscope-guided intubation in the lateral decubitus position was 91.7% at the first attempt, which is lower than that of a recent study, where the first intubation success rate was 96.72%.12 The lower success rate could be caused by improper shaping of the endotracheal tube, which is considered an independent risk factor for intubation failure.21 In addition, the tube used in video laryngoscope-guided endotracheal intubation in a lateral position needs to be adjusted to align with the glottis, and an assistant is needed to remove guide wires. This might explain why video laryngoscope-assisted intubation has a lower success rate and longer duration.
It should be noted that tracheal intubation is an empirical procedure. Each operator’s clinical experience and personal habits vary with different intubation tools. In this study, the tracheal intubation operator had the clinical experience of more than 200 cases of intubation with the flexible bronchoscope with patients in both the supine and lateral positions. The endotracheal intubation operator in this study preferred the flexible bronchoscope compared with the video laryngoscope. The user’s satisfaction with a flexible bronchoscope (9 [9, 10]) was higher than with the video laryngoscope (8 [7, 8]). Of course, it cannot be denied that some anesthesiologists may prefer a video laryngoscope over a flexible bronchoscope.
There was no significant difference in intubation complications between the two groups. There was no injury to the oral mucosal during intubation in group F because the flexible bronchoscope’s body is softer than the laryngoscope blade. The two cases with oral mucosa injury in group V were healed before discharge. It was also noted that three patients from group F and four from group V experienced irritation during tracheal intubation. The stimulation caused by endotracheal intubation can primarily be attributed to glottis exposure and tube placement. Although the flexible bronchoscope’s flexibility reduces stimulation during glottis exposure, it cannot be completely avoided. In addition, since all ESD patients need to drink Dyclonine prior to surgery to remove the foam in the digestive tract, its anesthetic effect, and surgical operations would affect the analysis of a sore throat. Therefore, this study did not analyze sore throat, a common adverse reaction to tracheal intubation.
This study has several limitations. Firstly, this study included a relatively small sample size. Clinical studies involving a larger population and multiple centers are required to confirm the findings of this study. Secondly, to avoid any bias from lack of proficiency, the procedures in this study were only performed by a single trained resident. The results might differ if the operator were a senior or consultant anesthesiologist. Thirdly, only single models of the flexible bronchoscope and video laryngoscope were used in this study. The performance and comfort of different brands and models of flexible bronchoscopes and laryngoscopes are known to differ, and anesthesiologists’ preferences for intubation instruments may also affect the results. Last but not least, during our clinical management, patients with high airway risk, such as obese patients or patients with BMIs over 30, were managed in their supine position throughout the treatment. Therefore, those patients were excluded from our current study. Thus, our findings may not apply to this group of patients. In future studies, we will try to investigate the airway management for these patients.
Conclusion
Both intubation methods achieved high intubation success rates. Meanwhile, no significant differences in complications of intubation were observed between the two groups. Importantly, in this study, it took less time to guide endotracheal intubation in the left lateral position with a flexible bronchoscope than with a video laryngoscope. Therefore, flexible bronchoscope-guided endotracheal intubation in the left lateral position may be an effective and safe approach for ESD patients.
Data Sharing Statement
The data sets analyzed and/or used during the present study are available from the Ailan Yu and Xingzhi Cai author upon reasonable request after the article was published.
Ethics Approval and Informed Consent
The study was conducted in accordance with the Declaration of Helsinki and approved by the Medical Ethics Committee of Liaocheng People’s Hospital (2020018). All participants provided written informed consent.
Acknowledgments
We would like to thank the digestive endoscopy team for their cooperation.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Chiu PW, Teoh AY, To KF, et al. Endoscopic submucosal dissection (ESD) compared with gastrectomy for treatment of early gastric neoplasia: a retrospective cohort study. Surg Endosc. 2012;26(12):3584–3591. doi:10.1007/s00464-012-2371-8
2. Purchiaroni F, Costamagna G, Hassan C. Quality in upper gastrointestinal endoscopic submucosal dissection. Ann Transl Med. 2018;6(13):261. doi:10.21037/atm.2018.02.27
3. Sharp CD, Tayler E, Ginsberg GG. Anesthesia for routine and advanced upper gastrointestinal endoscopic procedures. Anesthesiol Clin. 2017;35(4):669–677. doi:10.1016/j.anclin.2017.08.006
4. Edgcombe H, Carter K, Yarrow S. Anaesthesia in the prone position. Br J Anaesth. 2008;100(2):165–183. doi:10.1093/bja/aem380
5. Brahma R, Singla R, Pandia MP, Dube SK. Securing endotracheal tube in a bearded patient undergoing surgery for cerebellopontine angle tumor in lateral position-A different approach. J Neurosurg Anesthesiol. 2020;32(3):280–281. doi:10.1097/ANA.0000000000000599
6. Nathanson MH, Gajraj NM, Newson CD. Tracheal intubation in a manikin: comparison of supine and left lateral positions. Br J Anaesth. 1994;73(5):690–691. doi:10.1093/bja/73.5.690
7. Komatsu R, Nagata O, Sessler DI, Ozaki M. The intubating laryngeal mask airway facilitates tracheal intubation in the lateral position. Anesth Analg. 2004;98(3):858–861. doi:10.1213/01.ANE.0000100741.46539.6B
8. Cheng KI, Chu KS, Chau SW, et al. Lightwand-assisted intubation of patients in the lateral decubitus position. Anesth Analg. 2004;99(1):279–283. doi:10.1213/01.ANE.0000118103.78553.06
9. Jain D, Mehta S, Gandhi K, Arora S, Parikh B, Abas M. Comparison of intubation conditions with CMAC Miller videolaryngoscope and conventional Miller laryngoscope in lateral position in infants: a prospective randomized trial. Paediatr Anaesth. 2018;28(3):226–230. doi:10.1111/pan.13316
10. Komatsu R, Kamata K, You J, Sessler DI, Kasuya Y. Airway scope for tracheal intubation in the lateral position. Anesth Analg. 2011;112(4):868–874. doi:10.1213/ANE.0b013e31820c7cdf
11. Takenaka I, Aoyama K, Iwagaki T, Kadoya T. Efficacy of the airway scope on tracheal intubation in the lateral position: comparison with the Macintosh laryngoscope. Eur J Anaesthesiol. 2011;28(3):164–168. doi:10.1097/EJA.0b013e328340c368
12. Jin Y, Ying J, Zhang K, Fang X. Endotracheal intubation under video laryngoscopic guidance during upper gastrointestinal endoscopic surgery in the left lateral position: a randomized controlled trial. Medicine. 2017;96(52):e9461. doi:10.1097/MD.0000000000009461
13. Irwin MG. Difficult Airway Society guidelines for awake tracheal intubation in adults. Anaesthesia. 2020;75(5):688. doi:10.1111/anae.14969
14. Li H, Wang W, Lu YP, et al. Evaluation of endotracheal intubation with a flexible fiberoptic bronchoscope in lateral patient positioning: a prospective randomized controlled trial. Chin Med J. 2016;129(17):2045–2049. doi:10.4103/0366-6999.189069
15. Wen TT, Liu ZL, Zeng M, Zhang Y, Cheng BL, Fang XM. Lateral position intubation followed by endoscopic ultrasound-guided angiotherapy in acute esophageal variceal rupture: a case report. World J Clin Cases. 2021;9(2):372–378. doi:10.12998/wjcc.v9.i2.372
16. Singh N, Rao PB, Samal RL. TruView video laryngoscope for lateral position intubation in a patient with giant presacral neurofibroma. J Emerg Med. 2019;57(3):380–382. doi:10.1016/j.jemermed.2019.05.028
17. Nakao K, Komasawa N, Kusaka Y, Minami T. Rapid-sequence intubation in the left-lateral tilt position in a pregnant woman with premature placental abruption utilizing a videolaryngoscope. AJP Rep. 2015;5(1):e30–2. doi:10.1055/s-0034-1544109
18. Moro ET, Módolo NS. [Tracheal intubation and the patient with a full stomach]. Rev Assoc Med Bras. 2009;55(2):201–206. Portuguese. doi:10.1590/S0104-42302009000200027
19. Wahdan AS, El-Refai N, Omar SH, Abdel Moneem SA, Mohamed MM, Hussien MM. Endotracheal intubation in patients undergoing open abdominal surgery in the lateral position: a comparison between the intubating video stylet and fiberoptic intubating bronchoscopy. Korean J Anesthesiol. 2021;74(3):234–241. doi:10.4097/kja.20384
20. Zaouter C, Calderon J, Hemmerling TM. Videolaryngoscopy as a new standard of care. Br J Anaesth. 2015;114(2):181–183. doi:10.1093/bja/aeu266
21. Liu DX, Ye Y, Zhu YH, et al. Intubation of non-difficult airways using video laryngoscope versus direct laryngoscope: a randomized, parallel-group study. BMC Anesthesiol. 2019;19(1):75. doi:10.1186/s12871-019-0737-3
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.