Back to Journals » Cancer Management and Research » Volume 10
First-line treatment strategies for newly diagnosed chronic myeloid leukemia: a network meta-analysis
Authors Chen KK, Du TF, Wu KS, Yang W
Received 18 June 2018
Accepted for publication 25 July 2018
Published 25 September 2018 Volume 2018:10 Pages 3891—3910
DOI https://doi.org/10.2147/CMAR.S177566
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Beicheng Sun
Kang-Kang Chen,1 Tai-Feng Du,1 Ku-Sheng Wu,2 Wei Yang3
1Department of Preventive Medicine and MPH Education Center, Shantou University Medical College, Shantou, Guangdong Province, China; 2Department of Preventive Medicine, Shantou University Medical College, Shantou, Guangdong Province, China; 3Department of Thoracic Surgery, Administrative Office, Shantou University Medical College Cancer Hospital, Shantou, Guangdong Province, China
Objectives: With bosutinib proven to be available for frontline treatment, there are currently four frontline treatments as well as an additional strategy with high-dose imatinib for newly diagnosed chronic myeloid leukemia (CML). Due to the lack of direct comparison of high-dose imatinib, dasatinib, nilotinib, and bosutinib, we summarized the evidence to indirectly compare the efficacy among these treatment options.
Methods: In total, 14 randomized clinical trials including 5,630 patients were analyzed by direct and mixed-treatment comparisons. Outcomes assessed were the following: complete cytogenetic response at 12 months; major molecular response at 12, 24, and 36 months; deep molecular response at 12, 24, 36, and 60 months; early molecular response at 3 months; progression-free survival (PFS); overall survival (OS); and Grade 3 or 4 adverse events (AEs).
Results: The Bayesian network meta-analysis demonstrated that high-dose imatinib was less effective than all new-generation tyrosine kinase inhibitors and had a higher probability of Grade 3 or 4 AEs. For molecular response, 300 mg of nilotinib was likely to be the preferred frontline treatment, as demonstrated by higher response rates and faster, deeper, and longer molecular response. For PFS and OS, there were high likelihoods (79% and 74%, respectively) that 400 mg of nilotinib was the preferred option. For AEs, standard-dose imatinib has the highest probability (65%) of being the most favorable toxicity profile.
Conclusion: Considering the efficacy and toxicity profile, it is not recommended to use high-dose imatinib for treatment. This analysis also showed that nilotinib has the highest probability to become the preferred frontline agents for treating CML.
Keywords: CML, tyrosine kinase inhibitor, imatinib, bosutinib, dasatinib, nilotinib
Introduction
Chronic myeloid leukemia (CML) is a myeloproliferative malignancy, accounting for about 15% of newly diagnosed leukemia in adults with 5,230 new cases in men and 3,720 in women in 2017 in USA.1 CML is characterized by the chromosomal translocation between t(9;22) (Philadelphia Chromosome-Ph), which encodes the oncoprotein BCR-ABL1 with constitutive tyrosine kinase activity.2
The earlier drug therapy for CML was conventional chemotherapy such as hydroxyurea, busulfan, and interferon-alfa. Although major advances have been made in CML treatment, these treatment strategies were limited by their modest efficacy and toxicity profile.3 Allogeneic hematopoietic cell transplantation was a curative treatment but was associated with increased morbidity and mortality and needed an appropriate donor. Fortunately, since the emergence of BCR-ABL1 tyrosine kinase inhibitors (TKIs), the life expectancy of CML patients in chronic phrase (CP) was close to that of general population, and the annual mortality rate has dropped from 10%–20% to 1%–2%.1 Imatinib was the first-generation TKI to be tested in International Randomized Study of Interferon and STI571 study. It showed that imatinib was associated with superiority compared with interferon-alfa plus cytarabine, as demonstrated by higher cytogenetic and molecular response and less CML- or treatment-related deaths after 11 years of follow-up.4,5 However, imatinib is far from perfect, with ~15%–20% CML patients failed to achieve an optimal response, and only half of the patients (48%) remained on therapy at 11-year follow-up.4–6 In addition, the high-risk CML patients treated with imatinib had a poor overall survival (OS) rate (68.6%) at 11 years of treatment as compared with low-risk CML (89.9%) patients.4 To improve the efficacy of these CML patients with imatinib resistance, several randomized controlled trials (RCTs) were conducted to explore the new strategy treatment with high-dose imatinib. Results from these RCTs showed a more faster and deeper molecular response by high-dose imatinib in patients with CML-CP.7,8 Furthermore, high-dose imatinib had a good therapeutic effect on patients with no response to standard-dose imatinib.
In addition, given the increased recognition of pathogenesis of BCR-ABL oncoprotein in CML, the new-generation TKIs with considerable activity against the oncogenic BCR-ABL1 kinase were applied to the CML treatment.9 Dasatinib, nilotinib, and bosutinib are the three types of second-generation TKIs that have been extensively studied. Dasatinib is a potent inhibitor (350 times more potent in vitro over imatinib) in inhibiting wild-type BCR-ABL kinase, as well as inhibiting the SRC kinases, platelet-derived growth factor receptor (PDGFR), and c-KIT. Nilotinib is a derivative of imatinib with 30–50 times more affinity for BCR-ABL compared with imatinib, which also inhibits the PDGFR and c-KIT receptor. Bosutinib is an oral, dual SRC/ABL kinase inhibitor with greater potency than imatinib and minimal inhibitory activity against PDGFR and c-KIT compared with other TKIs. Both dasatinib and nilotinib have been approved by the US Food and Drug Administration as the frontline treatment for CP-CML. The open-label, phase III trials (Evaluating Nilotinib Efficacy and Safety in Clinical Trials-Newly Diagnosed Patients [ENESTnd]10 and DASatinib versus Imatinib Study In treatment-Naive CML patients [DASISION]11) have demonstrated that nilotinib and dasatinib had considerable advantage of achieving molecular and cytogenetic response over imatinib in newly diagnosed CP-CML patients. In addition, for patients with high-risk CML or those who failed in imatinib treatment, switching to nilotinib or dasatinib can experience long-term benefits.6,12–14 More recently, bosutinib has been evaluated for frontline treatment for newly diagnosed CML patients.15 Considering the shortcomings of the Bosutinib Efficacy and Safety in Chronic Myeloid Leukemia (BELA), Cortes et al15 conducted a clinical trial to adjust the starting dose of bosutinib (400 mg once daily), which significantly achieved efficacy and safety, suggesting that bosutinib may be used as frontline treatment for CP-CML.15
So far, there are four frontline treatments as well as additional treatment strategy with high-dose imatinib approved for CML patients. To our knowledge, no published literature has compared the outcome of second-generation TKIs to the high-dose imatinib, except Sasaki et al16 who performed a propensity score matching to analyze the relative efficacy of these treatments and suggested that CML patients may have similar response and long-term survival between high-dose imatinib and second-generation TKIs. In addition, with bosutinib proven to be available for frontline treatment, there is currently also no direct or indirect comparison among second-generation TKIs. Therefore, to explore the relative efficacy and safety of these agents and further to determine the preferable choices as frontline treatment for CML patients, we identified all RCTs of first-line dasatinib, nilotinib, bosutinib, and high-dose imatinib and undertook this network meta-analysis (NMA) to help all stakeholders overcome the paucity of head-to-head data in making clinical decisions.
Methods
Search trials
We searched the electronic databases (EMBASE, Cochrane Central Register of Controlled Trials, and PubMed) from the inception dates to the date of search (March 17, 2018), using the terms “bosutinib,” “dasatinib,” “nilotinib,” “imatinib,” and “Leukemia, Myelogenous, Chronic, BCR-ABL Positive” to identify published RCTs evaluating the relative efficacy of second-generation TKIs, high-dose imatinib, and standard-dose imatinib. We also performed additional search which selected “systematic reviews” or “meta-analysis” as an article type, using the databases and terms described above. We exacted original RCTs included in these systematic reviews or meta-analysis, which differed from the first retrieval. There were no language and publication status restrictions.
Eligibility criteria and study selection
We selected clinical trials according to the following inclusion criteria: 1) RCTs comparing bosutinib, dasatinib, nilotinib, or high-dose imatinib (600 mg or 800 mg daily) with standard-dose imatinib (400 mg daily) as frontline therapy for newly diagnosed CP-CML; and 2) trials enrolling adults aged >18 years. Exclusion criteria were the following: 1) non-RCTs; 2) including patients with advanced stages of CML (ie, accelerated phrase or blast phase); and 3) including patients who had received other treatments before entering the study (except hydroxyurea, anagrelide, or imatinib for <2 weeks).
Study selection was performed by two independent researchers (Chen and Du) who independently reviewed the titles and abstracts based on the inclusion and exclusion criteria. For potentially relevant studies, the full text was obtained and reviewed for further investigation. Disagreements were determined by consensus or by a third reviewer (Wu).
Data extraction and risk of bias assessments
A predefined data extraction sheet was used to extract the data. Two independent reviewers (Chen and Du) abstracted data on lead author; publication year; treatments (including the type of intervention and frequency and dose of TKI); sample size; patient baseline characteristics (including gender, age, Eastern Cooperative Oncology Group performance status, the number of patients according to risk group, platelet counts, and white blood cells); and data on the complete cytogenetic response (CCyR), major molecular response (MMR), progression-free survival (PFS), OS, early molecular response (EMR), deep molecular response (DMR), and Grade 3 or 4 adverse events (AEs). In each trial, the number of outcomes was abstracted according to the intention-to-treat approach. One reviewer abstracted the data from included RCTs, and another confirmed the accuracy of the data. Any disagreements were resolved by consensus. Table 1 shows the detailed information regarding baseline characteristics.
For each included RCT, the risk of bias was independently assessed by two reviewers (Chen and Du) based on the Cochrane risk of bias criteria.17 The following seven components were used to evaluate the bias in each trial: randomization sequence generation, concealment of allocation, blinding of outcome assessors, blinding of patients and care givers, selective reporting, incomplete outcome data, and other bias. Each component was evaluated separately and graded as high risk, low risk, and unclear risk. Disagreements were determined by discussion or by a third reviewer (Wu).
Definition of outcomes
The primary outcomes were CCyR and MMR at 12 months. Secondary outcomes were MMR at 24 and 36 months; DMR at 12, 24, 36, and 60 months, EMR at 3 months; and OS, PFS, and Grade 3 or 4 AEs.
Statistical analyses
For each outcome, we used a Bayesian framework with noninformative priors to conduct an NMA to directly and indirectly compare the relative efficacy of standard-dose imatinib, high-dose imatinib, and second-generation TKIs and rank their outcomes graphically. For PFS and OS, we used HR and P-values provided by the manuscript to calculate the corresponding log HR and standard error for indirect comparison, or we used Engauge Digitizer 4.1 and excel file provided by Tierney et al,18 based on the OS curve or PFS curve, to calculate the log HR and standard error directly. For other indicators, the results were calculated as OR with 95% credible interval (CrI). For convergence, we discarded the burn-in of 5,000 initial iterations, and the results were estimated according to additional 20,000 iterations. Model fit was checked using deviance information criterion (DIC). When the DIC value of random-effects model or fixed-effects model was obtained, we chose the lower DIC model as the primary analytical model. We used the I2 statistic to assess statistical heterogeneity among the various trials, where I2 value <25% reflected mild heterogeneity, 25%–50% reflected moderate heterogeneity, and >50% reflected severe heterogeneity. The estimation of potential publication bias was investigated by funnel plot. All analyses were performed using JAGS software in R by use of gemtc (R package Version 0.8) and rjags (R package Version 4.3.0).
Results
Studies retrieved and characteristics
The initial searches yielded 1,072 relevant references. After removing duplicates, 718 references were identified from the different databases. After screening titles and abstracts, 44 full texts of these references were considered for further investigation. Then, 23 articles were excluded from 44 articles due to non-RCTs, sub-analysis of DASISION/ENESTnd, and incompatibility with our inclusion criteria. In the remaining 21 articles, 54 RCTs were identified. Among a total of 54 RCTs, further 40 RCTs were excluded, because of a repeated report; 14 studies were included in this NMA eventually. Figure 1 depicts the process of study selection.
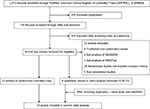  | Figure 1 Literature search and screening process. Abbreviation: RCTs, randomized controlled trials. |
In total, 14 trials including 5,630 patients were ultimately included in this NMA. Of these, imatinib was compared with high-dose imatinib in five trials,7,8,19–21 dasatinib in five trials,11,22–25 nilotinib in two trials,10,26 and bosutinib 400 mg daily and bosutinib 500 mg daily in one trial each.15,27 One trial (ie, Spirit 225) was conference abstract identified from the systematic review and meta-analysis.28 As this conference abstract did not report the baseline characteristics, we can obtain only the participant numbers and interesting outcomes. Other trials were well matched between the two groups in baseline characteristics, except two trials (S0325-1 and European Leukemia Net), which were higher in high-risk patients compared with remaining trials. Table 1 shows the detailed information.
Primary outcomes
Based on the data obtained in the original literature about CCyR, our NMA included 14 trials involving 5,410 total patients. Figure 2 shows the network configuration. Compared with imatinib, the CCyR rate at 12 months was significantly improved in all other treatments, except bosutinib 500 mg daily, which was similar to the standard-dose imatinib with an OR of 1.3 (95% CrI =0.84–1.9; Figure 2B). On the indirect comparison, all other treatments had no statistical difference in CCyR at 12 months when compared against each other. The results of surface under the cumulative ranking (SUCRA) analysis showed that bosutinib 400 mg daily (30% probability), nilotinib 400 mg daily (26% probability), and dasatinib (24% probability) had a similar probability being the first, best treatments.
For MMR at 12 months, our NMA comprised 14 trials involving 5,477 total patients, which was shown in Figure 3. The direct comparison suggested that all treatments were associated with superior efficacy compared with standard-dose imatinib (Figure 3B). On indirect comparison, nilotinib 300 mg daily had a favorable effect as compared with bosutinib 400 mg daily, dasatinib, and high-dose imatinib, but no difference with bosutinib 500 mg daily and nilotinib 400 mg daily (bosutinib 500 vs nilotinib 300: OR 0.66 [0.41–1.1] and nilotinib 300 vs nilotinib 400: OR 0.95 [0.69–1.3]; Figure 3C). The results of rank probabilities showed that nilotinib 300 mg has a 59.9% likelihood of being the preferred treatment.
In addition, we performed a subgroup analysis of CML patients with a high-risk score regarding MMR at 12 months. According to the direct comparison, imatinib had an inferior effect as compared with bosutinib 400 mg, dasatinib, nilotinib 300 mg, and nilotinib 400 mg, but no difference with bosutinib 500 mg and high-dose imatinib. On indirect comparison, only imatinib and high-dose imatinib were less effective than nilotinib 300 mg. Figure S1 shows the detailed information.
Secondary outcomes
MMR at 24 and 36 months
Compared with imatinib, all treatments had significantly superior MMR rate at long-time follow-up, except high-dose imatinib, which was similar to the standard-dose imatinib at Month 36 with an OR of 1.2 (95% CrI =0.79–1.7). On indirect comparison, nilotinib 300 mg had a significantly better MMR rate at 24 and 36 months as compared with high-dose imatinib, but no difference with dasatinib and nilotinib 400 mg. Based on the SUCRA analysis, nilotinib 300 mg daily has ranked first with 68.3% and 73.8% probabilities of providing the best MMR at 24 and 36 months.
DMR and EMR
Compared with imatinib, second-generation TKIs and high-dose imatinib had significantly higher DMR at 12, 24, 36, and 60 months, except bosutinib 500 mg, which is similar to imatinib at 24 months with an OR of 1.4 (0.82–2.3). Based on the SUCRA analysis, bosutinib 500 mg compared against all TKIs had the highest probability (67.0%) of DMR at 12 months. However, at 24, 36, and 60 months, nilotinib 300 mg may be the preferred option according to the rank probabilities. Furthermore, on indirect comparison, standard-dose imatinib and high-dose imatinib have always been worse than nilotinib 300 mg during long-time treatment. Figures S2–S5 show the detailed information.
Compared with nilotinib 300 mg, the rate of EMR at 3 months was statistically inferior to the use of bosutinib and imatinib, but no difference with dasatinib (nilotinib 300 mg vs bosutinib 400 mg: OR 2.2 [1.2–4.2], nilotinib 300 mg vs imatinib: OR 5.1 [3.2–8.4], nilotinib vs dasatinib: OR 1.6 [0.87–3.1]). Rank probabilities regarding EMR also showed that nilotinib ranked first (59.2%) among other TKIs. Figure S6 shows the detailed information.
PFS and OS
For PFS and OS, the NMA comprised five trials involving 1,972 total patients. Figure 4 shows the network configuration regarding PFS. Compared with imatinib, PFS differed in a significant manner for only patients who received nilotinib 400 mg daily with an HR of 0.30 (95% CrI =0.10–0.87; Figure 4B). When compared to nilotinib 400 mg, both standard-dose imatinib and dasatinib had significantly higher HRs of 3.4 (95% CrI: 1.1–11.0) and 3.3 (95% CrI: 1.2–9.6), respectively (Figure 4C). Based on the analysis of SUCRA, nilotinib 400 mg has a 79% likelihood of being the preferred treatment (Figure 4D).
Figure S7 shows the network configuration regarding OS. Regardless of the direct or indirect comparison, there was no statistical difference among these treatments. On a SUCRA analysis, nilotinib 400 mg has a 74% likelihood of being the preferred treatment (Figure S7D).
Safety analysis
We performed an NMA comparing Grade 3 or 4 AEs among seven treatment strategies. In this analysis, eleven trails including a total of 4,262 patients were available. Figure 5 shows the network configuration. Compared with imatinib, only nilotinib 300 mg daily was associated with a similar rate of serious AEs with an OR of 1.1 (95% CrI =0.76–1.5; Figure 5B). When compared to nilotinib 300 mg daily, all other therapies had significantly worse toxicity profile, except dasatinib (OR =1.5, 95% CrI =0.93–2.5) and standard-dose imatinib (OR =0.93, 95% CrI =0.66–1.3; Figure 5C). The results of SUCRA analysis showed that standard-dose imatinib had a 65% chance of being the most favorable toxicity profile (Figure 5D). Conversely, there was a 74.8% likelihood that high-dose imatinib had the least favorable toxicity profile (Figure 5D).
Discussion
Our NMA compiled RCTs comparing second-generation TKIs and high-dose imatinib with standard-dose imatinib 400 mg daily as frontline treatment for newly diagnosed CP-CML. It was demonstrated that nilotinib 300 mg was associated with a superiority in achieving higher response rates and faster, deeper, and longer molecular response as compared with imatinib, high-dose imatinib, dasatinib, and bosutinib. However, when we conducted subanalysis in patients with high-risk CML, we found that there was no statistical difference among second-generation TKIs. Considering the optimal efficacy and distinct toxicity profile, this finding might bring more frontline treatment options to a given patient with a high-risk score. Despite high-dose imatinib was superior to the standard-dose imatinib in terms of MMR, it paled in comparison with dasatinib and nilotinib across all Hasford risk groups. In addition, nilotinib 400 mg had the highest probability of achieving PFS and OS. Conversely, standard-dose imatinib is still the safest treatment strategy with 65% chance of being the best-tolerated regime regarding to Grade 3 or 4 adverse effects.
The major limitation in our NMA is that although our research data were extracted from RCTs, the relative efficacy among second-generation TKIs and high-dose imatinib was based on indirect comparison which suggested that the evidence level regarding relative efficacy among new-generation TKIs is limited. Another limitation is the definition of PFS among five trials as described earlier. Due to the different criteria for PFS in included articles, there may be bias in the indirect comparison of PFS. In addition, Bosutinib Trial in First-Line Chronic Myelogenous Leukemia Treatment (BFORE) trial is an ongoing phase III multinational randomized study which assessed primary and secondary outcomes up to Month 12. Due to the paucity of available data, we did not assess the comparative efficacy among three new-generation TKIs at time points beyond 12 months. Furthermore, efficacy regarding bosutinib 400 mg once daily was only reported in one trial.
In addition to CCyR and MMR, another monitoring indicator (ie, DMR) is an important factor that increases the likelihood allowing for TKI cessation, which is an emerging goal in CML treatment nowadays.29–32 Up to now, several studies have demonstrated that ~50% of the patients who achieve and sustain stable DMR for a significant period can stop TKI therapy and remain treatment-free remission (TFR) for several years.33–35 Furthermore, these patients who discontinue TKI therapy successfully remain sensitive to prior TKI and safely reestablish remission after molecular relapse.33 The DMR reported in our NMA was assessed by 12, 24, 36, and 60 months, showing that high-dose bosutinib was associated with faster and deeper molecular response, and nilotinib 300 mg was related to long-term DMR. In other words, these results may indicate that some patients who are sensitive to high-dose bosutinib will soon reach DMR during the first year, and these patients who reach DMR faster can enter the TFR phase earlier, which means that they have a great chance of achieving a higher health-related quality of life and a lower financial burden. In addition, recent evidence showed that DMR correlates significantly with long-term benefits, particularly when achieved early during treatment.36 Unfortunately, due to the high discontinuation rate caused by AEs, BELA27 (bosutinib 500 mg per day) did not meet its primary end point of CCyR at 12 months. However, with the increased experience in bosutinib treatment, Cortes et al15 conducted a clinical trial to adjust the starting dose of bosutinib (400 mg per day), which significantly achieved efficacy and safety. Therefore, it is quite important to identify the eligible patients and establish the optimal dose regimen of bosutinib that created balance to achieve both DMR and CCyR. Obviously, these findings may help us to understand that bosutinib and nilotinib seem more appropriate for younger patients who may have >30 years of remaining life expectancy or for women who wish to conceive.37 Considering that maintaining TFR is becoming an important goal in clinical care, bosutinib may have an important value in future research.
Although the emergence of TKI has substantially changed the natural history of CML and made their life expectancy close to the general population, some patients treated with TKI also failed to achieve optimal response and had poor long-term outcomes.4 Several reports have shown that EMR was strongly associated with long-term benefits in CP-CML patients.38–41 Futhermore, if patients treated with imatinib have a BCR-ABL(IS)>10% at 3 months, the prognosis was extremely poor, regardless of increasing the dose of imatinib or switching to the new-generation TKIs. It can therefore be assumed that the EMR is the important landmark that must be identified after starting TKI therapy. Our NMA revealed that all second-generation TKIs induced faster molecular response than imatinib. In addition, the results of this NMA indicated that nilotinib was related to higher EMR rate, as compared to other TKIs, in terms of relative efficacy among all TKIs and the results of rank probabilities. Due to the limitations of the original research data, we only obtained the EMR at 3 months. Several experts suggested that a single measurement of molecular response level at Month 3 cannot define failure that needs to change the treatment, and a follow-up measurement at Month 6 is necessary.6 However, recent clinical studies demonstrated that using the 3- vs 6-month landmarks to predict future outcomes was generally similar.39–41 In addition, some studies have also found that long-term outcome can be predicted accurately according to the transcript level at 3 months.42 Therefore, the EMR at Month 3 represents the credible surrogate marker for the long-term outcomes, which suggested that nilotinib may be the preferred option for CP-CML patients.
Our NMA showed that nilotinib 400 mg per day revealed a statistically significant advantage of PFS as compared to the standard-dose imatinib and dasatinib. However, our research showed no statistical significance in OS. The results of OS above may stem from the fact that the outcomes only assessed up to 5 years, and the sample size was limited. It is possible that differences will be discernible with longer follow-up. Another possible explanation for this is that patients’ comorbidities at diagnosis have a strong negative effect on OS,43 which masked the real difference in efficacy among different TKIs. However, based on the result of rank probabilities (74%), the present study may raise the trend that high-dose nilotinib has a slight advantage in OS compared with other treatment strategies. Whether this slight advantage can be expanded and further translated into long-term clinical benefit requires extended follow-up.
While multiple TKIs are available for CML patients in chronic phase, we chose a TKI as a first-line therapy depending on not only efficacy but also TKI toxicity profile and patient’s comorbidities. From the result, we only rank each TKI based on the number of Grade 3 or 4 AEs, but did not provide any specific serious side effects. Substantial research suggest that dasatinib is related to pulmonary arterial hypertension, pleural effusions, and inhibiting platelets function.11,44–46 Nilotinib has been associated with vascular events, hyperglycemia, and prolongation of QT interval.9,47 Bosutinib is a potent dual SRC/ABL kinase inhibitor evaluated for frontline treatment for CP-CML patients recently.15 Toxicities seen with bosutinib such as Grade 3 diarrhea (without Grade 4 diarrhea), which is mild and manageable, and liver function AEs (increased alanine aminotransferase and aspartate aminotransferase).15 The side effects of cardiac and vascular are not common in the treatment of bosutinib.15 Of note, the serious side effects of each TKI listed here occurred only because the incidence rate is relatively high during the treatment and does not indicate that other serious side effects will not occur with the long-term treatment. In addition, considering large majority of CML patients, current TKI treatments are lifelong, which means that they will suffer from mild or severe side effects for a long time. Pinilla-Ibarz et al48 demonstrated that even nonserious AEs are likely to significantly interfere with patient’s daily lives and compromise their health-related quality of life. Therefore, clinicians should pay close attention to the condition changes of patients with CML in real-life clinical care.
Conclusion
High-dose imatinib was more likely to cause Grade 3 or 4 AEs than other all TKIs and was associated with inferior efficacy compared with second-generation TKIs. Conversely, standard-dose imatinib has the highest probability of being the most favorable toxicity profile. In addition, nilotinib 300 mg is related to superior efficacy compared with other treatment strategies, as demonstrated by higher response rates and faster, deeper, and longer molecular response. For survival, nilotinib 400 mg has the highest probability of being the preferred treatment. Future research should 1) identify the eligible patients who are sensitive to bosutinib; 2) conduct head-to-head randomized trials to evaluate the relative efficacy among new-generation TKIs; and 3) establish the dose regimen of nilotinib that will provide long survival and good optimal efficacy.
Ethics approval
All studies that were included in this NMA stated to be in accordance with the ethical standards of the Institutional and/or National Research Committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Disclosure
The authors report no conflicts of interest in this work.
References
Siegel RL, Miller KD, Jemal A. Cancer Statistics, 2017. CA Cancer J Clin. 2017;67(1):7–30. | ||
Ren R. Mechanisms of BCR-ABL in the pathogenesis of chronic myelogenous leukaemia. Nat Rev Cancer. 2005;5(3):172–183. | ||
Silver RT, Woolf SH, Hehlmann R, et al. An evidence-based analysis of the effect of busulfan, hydroxyurea, interferon, and allogeneic bone marrow transplantation in treating the chronic phase of chronic myeloid leukemia: developed for the American Society of Hematology. Blood. 1999;94(5):1517–1536. | ||
Hochhaus A, Larson RA, Guilhot F, et al. Long-Term Outcomes of Imatinib Treatment for Chronic Myeloid Leukemia. N Engl J Med. 2017;376(10):917–927. | ||
O’Brien SG, Guilhot F, Larson RA, et al. Imatinib compared with interferon and low-dose cytarabine for newly diagnosed chronic-phase chronic myeloid leukemia. N Engl J Med. 2003;348(11):994–1004. | ||
Baccarani M, Deininger MW, Rosti G, et al. European LeukemiaNet recommendations for the management of chronic myeloid leukemia. Blood. 2013;122(6):872–884. | ||
Hehlmann R, Lauseker M, Jung-Munkwitz S, et al. Tolerability-adapted imatinib 800 mg/d versus 400 mg/d versus 400 mg/d plus interferon-α in newly diagnosed chronic myeloid leukemia. J Clin Oncol. 2011;29(12):1634–1642. | ||
Deininger MW, Kopecky KJ, Radich JP, et al. Imatinib 800 mg daily induces deeper molecular responses than imatinib 400 mg daily: results of SWOG S0325, an intergroup randomized PHASE II trial in newly diagnosed chronic phase chronic myeloid leukaemia. Br J Haematol. 2014;164(2):223–232. | ||
Mughal TI, Radich JP, Deininger MW, et al. Chronic myeloid leukemia: reminiscences and dreams. Haematologica. 2016;101(5):541–558. | ||
Saglio G, Kim DW, Issaragrisil S, et al. Nilotinib versus imatinib for newly diagnosed chronic myeloid leukemia. N Engl J Med. 2010;362(24):2251–2259. | ||
Kantarjian H, Shah NP, Hochhaus A, et al. Dasatinib versus imatinib in newly diagnosed chronic-phase chronic myeloid leukemia. N Engl J Med. 2010;362(24):2260–2270. | ||
Cortes JE, De Souza CA, Ayala M, et al. Switching to nilotinib versus imatinib dose escalation in patients with chronic myeloid leukaemia in chronic phase with suboptimal response to imatinib (LASOR): a randomised, open-label trial. Lancet Haematol. 2016;3(12):e581–e591. | ||
Yeung DT, Osborn MP, White DL, et al. TIDEL-II: first-line use of imatinib in CML with early switch to nilotinib for failure to achieve time-dependent molecular targets. Blood. 2015;125(6):915–923. | ||
Shah NP, Guilhot F, Cortes JE, et al. Long-term outcome with dasatinib after imatinib failure in chronic-phase chronic myeloid leukemia: follow-up of a phase 3 study. Blood. 2014;123(15):2317–2324. | ||
Cortes JE, Gambacorti-Passerini C, Deininger MW, et al. Bosutinib Versus Imatinib for Newly Diagnosed Chronic Myeloid Leukemia: Results From the Randomized BFORE Trial. J Clin Oncol. 2018;36(3):231–237. | ||
Sasaki K, Kantarjian H, Jabbour E, et al. Frontline therapy with high-dose imatinib versus second generation tyrosine kinase inhibitor in patients with chronic-phase chronic myeloid leukemia - a propensity score analysis. Haematologica. 2016;101(8):e324–e327. | ||
Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. | ||
Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16. | ||
Preudhomme C, Guilhot J, Nicolini FE, et al. Imatinib plus peginterferon alfa-2a in chronic myeloid leukemia. N Engl J Med. 2010;363(26):2511–2521. | ||
Cortes JE, Baccarani M, Guilhot F, et al. Phase III, randomized, open-label study of daily imatinib mesylate 400 mg versus 800 mg in patients with newly diagnosed, previously untreated chronic myeloid leukemia in chronic phase using molecular end points: tyrosine kinase inhibitor optimization and selectivity study. J Clin Oncol. 2010;28(3):424–430. | ||
Baccarani M, Rosti G, Castagnetti F, et al. Comparison of imatinib 400 mg and 800 mg daily in the front-line treatment of high-risk, Philadelphia-positive chronic myeloid leukemia: a European LeukemiaNet Study. Blood. 2009;113(19):4497–4504. | ||
Hjorth-Hansen H, Stenke L, Söderlund S, et al. Dasatinib induces fast and deep responses in newly diagnosed chronic myeloid leukaemia patients in chronic phase: clinical results from a randomised phase-2 study (NordCML006). Eur J Haematol. 2015;94(3):243–250. | ||
Radich JP, Kopecky KJ, Appelbaum FR, et al. A randomized trial of dasatinib 100 mg versus imatinib 400 mg in newly diagnosed chronic-phase chronic myeloid leukemia. Blood. 2012;120(19):3898–3905. | ||
Zhou L, Wang JX, Huang XJ, Hu JD, Shen ZX. Preliminary comparison of efficacy and safety of dasatinib and imatinib in newly diagnosed chronic myeloid leukemia. Zhonghua Xue Ye Xue Za Zhi. 2013;34(2):93–97. | ||
O’Brien S, Adams S, Foroni L, et al. Spirit 2: an NCRI randomised study comparing dasatinib with imatinib in patients with newly diagnosed CML. ASH Annual Abstracts Meetings. 2014;124:517. | ||
Shah NP. Front-Line Treatment Options for Chronic-Phase Chronic Myeloid Leukemia. J Clin Oncol. 2018;36(3):220–224. | ||
Cortes JE, Kim DW, Kantarjian HM, et al. Bosutinib versus imatinib in newly diagnosed chronic-phase chronic myeloid leukemia: results from the BELA trial. J Clin Oncol. 2012;30(28):3486–3492. | ||
Gurion R, Raanani P, Vidal L, Leader A, Gafter-Gvili A. First line treatment with newer tyrosine kinase inhibitors in chronic myeloid leukemia associated with deep and durable molecular response - systematic review and meta-analysis. Acta Oncol. 2016;55(9–10):1077–1083. | ||
Elsayed AG, Srivastava R, Jamil MO. Treatment-Free Remission: a New Therapeutic Goal in Chronic Myelogenous Leukemia. Curr Oncol Rep. 2017;19(12):77. | ||
Saußele S, Richter J, Hochhaus A, Mahon FX. The concept of treatment-free remission in chronic myeloid leukemia. Leukemia. 2016;30(8):1638–1647. | ||
Hughes TP, Ross DM. Moving treatment-free remission into mainstream clinical practice in CML. Blood. 2016;128(1):17–23. | ||
Firwana B, Sonbol MB, Diab M, et al. Tyrosine kinase inhibitors as a first-line treatment in patients with newly diagnosed chronic myeloid leukemia in chronic phase: A mixed-treatment comparison. Int J Cancer. 2016;138(6):1545–1553. | ||
Ross DM, Masszi T, Gómez Casares MT, et al. Durable treatment-free remission in patients with chronic myeloid leukemia in chronic phase following frontline nilotinib: 96-week update of the ENESTfreedom study. J Cancer Res Clin Oncol. 2018;144(5):945–954. | ||
Rea D, Nicolini FE, Tulliez M, et al. Discontinuation of dasatinib or nilotinib in chronic myeloid leukemia: interim analysis of the STOP 2G-TKI study. Blood. 2017;129(7):846–854. | ||
Hochhaus A, Masszi T, Giles FJ, et al. Treatment-free remission following frontline nilotinib in patients with chronic myeloid leukemia in chronic phase: results from the ENESTfreedom study. Leukemia. 2017;31(7):1525–1531. | ||
Mahon FX, Etienne G. Deep molecular response in chronic myeloid leukemia: the new goal of therapy? Clin Cancer Res. 2014;20(2):310–322. | ||
Cortes JE, Abruzzese E, Chelysheva E, et al. The impact of dasatinib on pregnancy outcomes. Am J Hematol. 2015;90(12):1111–1115. | ||
Hughes TP, Hochhaus A, Branford S, et al. Long-term prognostic significance of early molecular response to imatinib in newly diagnosed chronic myeloid leukemia: an analysis from the International Randomized Study of Interferon and STI571 (IRIS). Blood. 2010;116(19):3758–3765. | ||
Jabbour E, Kantarjian HM, Saglio G, et al. Early response with dasatinib or imatinib in chronic myeloid leukemia: 3-year follow-up from a randomized phase 3 trial (DASISION). Blood. 2014;123(4):494–500. | ||
Hughes TP, Saglio G, Kantarjian HM, et al. Early molecular response predicts outcomes in patients with chronic myeloid leukemia in chronic phase treated with frontline nilotinib or imatinib. Blood. 2014;123(9):1353–1360. | ||
Jain P, Kantarjian H, Nazha A, et al. Early responses predict better outcomes in patients with newly diagnosed chronic myeloid leukemia: results with four tyrosine kinase inhibitor modalities. Blood. 2013;121(24):4867–4874. | ||
Neelakantan P, Gerrard G, Lucas C, et al. Combining BCR-ABL1 transcript levels at 3 and 6 months in chronic myeloid leukemia: implications for early intervention strategies. Blood. 2013;121(14):2739–2742. | ||
Saussele S, Krauss MP, Hehlmann R, et al; Schweizerische Arbeitsgemeinschaft für Klinische Krebsforschung and the German CML Study Group. Impact of comorbidities on overall survival in patients with chronic myeloid leukemia: results of the randomized CML study IV. Blood. 2015;126(1):42–49. | ||
Valent P, Hadzijusufovic E, Schernthaner GH, Wolf D, Rea D, le Courte P. Vascular safety issues in CML patients treated with BCR/ABL1 kinase inhibitors. Blood. 2015;125(6):901–906. | ||
Montani D, Bergot E, Günther S, et al. Pulmonary arterial hypertension in patients treated by dasatinib. Circulation. 2012;125(17):2128–2137. | ||
Quintás-Cardama A, Han X, Kantarjian H, Cortes J. Tyrosine kinase inhibitor-induced platelet dysfunction in patients with chronic myeloid leukemia. Blood. 2009;114(2):261–263. | ||
Hochhaus A, Saglio G, Hughes TP, et al. Long-term benefits and risks of frontline nilotinib vs imatinib for chronic myeloid leukemia in chronic phase: 5-year update of the randomized ENESTnd trial. Leukemia. 2016;30(5):1044–1054. | ||
Pinilla-Ibarz J, Cortes J, Mauro MJ. Intolerance to tyrosine kinase inhibitors in chronic myeloid leukemia: Definitions and clinical implications. Cancer. 2011;117(4):688–697. |
Supplementary materials
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.












