Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 13
Fertility Desire, Knowledge of Prevention of MCT of HIV and Associated Factors Among Men and Women Attending ART Clinic at Public Health Institutions of West Shoa Zone, Oromia, Ethiopia, 2020
Authors Dina GD, Debelo BT , Belema D, Danusa KT , Muleta R
Received 13 July 2021
Accepted for publication 13 September 2021
Published 24 September 2021 Volume 2021:13 Pages 927—938
DOI https://doi.org/10.2147/HIV.S328565
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Bassel Sawaya
Gurmesa Daba Dina, Bikila Tefera Debelo, Daniel Belema, Kababa Temesgen Danusa, Rebuma Muleta
Midwifery Department, College of Medicine and Health Science, Ambo University, Ambo, Ethiopia
Correspondence: Bikila Tefera Debelo Email [email protected]
Background: Globally, the human immunodeficiency virus (HIV) affects young people in their reproductive years. Most of the studies conducted in Ethiopia focus on the fertility desire of women of reproductive age and did not give due consideration to the men’s fertility perspective. Thus, this study aimed to assess the fertility desire, knowledge of prevention of mother to child of HIV (PMTCT), and associated factors among HIV-positive men and women attending ART clinic at west Shewa zone, Oromia region, Ethiopia, 2020.
Methods: Facility-based cross-sectional study design was applied to identify fertility desire, PMTCT knowledge, and associated factors among 590 HIV-positive reproductive age group men and women attending ART clinics at public health institutions of West Shewa zone. Data were collected by pre-tested structured questionnaires and analyzed using SPSS version 22. Binary logistic regression analysis was used to examine the association of predictors on fertility desire and knowledge about PMTCT. Odds ratio, 95% CI, and P value 0.05 were used to measure the statistical association.
Results: The prevalence of fertility desire and knowledge of PMTCT in the study area were 58.8% and 30.7%, respectively. The odds of fertility desire were higher among the respondents aged > 25 years [AOR=4.64, 95% CI (2.75– 7.85)], housewives [AOR=3.14, 95% CI (1.90– 5.21)], merchants [AOR=5.31, 95% CI (2.55– 11.05)], ART use for ≤ 5 years [AOR=5.13, 95% CI (2.37– 11.12)] and among those voluntarily tested to know their HIV status [AOR=2.16, 95% CI (1.30– 3.58)]. Besides, the odds of fertility desire were low among husband who cannot read and write [AOR=0.07, 95% CI (0.02– 0.23)], primary education [AOR=0.22, 95% CI (0.09– 0.56)], and secondary education [AOR= 0.32, 95% CI (0.14– 0.73)] when compared with husband education of college and above. Likewise, the odds of PMTCT knowledge were higher among the respondents aged less than 25 years [AOR=2.53, 95% CI (1.32– 4.86)] who undergone voluntary testing during HIV diagnosis reasons [AOR=1.55, 95% CI (1.03– 2.35)], and ART use for more than five years [AOR=1.94, 95% CI (1.26– 2.98)].
Conclusion: Younger age, husband education, occupation, recent HIV test, and voluntary testing were significantly associated with fertility desire. Likewise, the younger age group, voluntary testing and counseling, and those on ART for more than five years had higher odds of PMTCT knowledge. Therefore, strengthening voluntary testing and counseling strong counseling on PMTCT throughout the follow-up care and involvement partners is of paramount importance should be insured to decrease MTCT.
Keywords: PMTCT knowledge, fertility desire, west Shewa, Ethiopia
Introduction
Globally in 2020, 37.7 million people are living with HIV, including 10.2 million who were not on treatment, 1.5 million new HIV infections, and 680 thousand people died of AIDS-related illnesses.1 The WHO global HIV AIDS progress report showed an average of 150,000 new infections of HIV in children from age 0–14 years despite the target of zero new infection target among children in 2020.1 Adolescent girls and young women of sub-Saharan countries account for 25% of all new HIV infections.2 New infections in children are mainly through mother-to-child transmission of HIV AIDS during pregnancy, childbirth, or breastfeeding which can be decreased by adequate access to HIV prevention, care, and treatment services.1,3 In Ethiopia, the national HIV prevalence among aged 15–49 years was 0.9%, 1.2% among women, and 0.6 among men.4
Physiological, social vulnerability, and gender inequalities make women particularly vulnerable to HIV/AIDS.5 In Africa, the desire to have uninfected children remains a great challenge for HIV-positive women.6 The use of highly active antiretroviral treatment has decreased transmission from mother to child.7
In Ethiopia, the prevalence of fertility desire among those attending ART clinic was 33.4% in Finote Selam,8 40.3% in Northwest Ethiopia,9 44% in Addis Ababa,10 45.5% in Tigray Region,11 and 46.8% in Jimma Town.12 The fertility desire of HIV-positive women is affected by the fear of transmitting the infection to the child.13 Younger age,3,10,11,14–16 lower educational status,9,12,17 years on ART,8 current health status,18 number of alive children,3,11,16 knowledge on PMTCT,16,19 and disclosure to a partner11 were some of the factors reported to be associated with fertility desire.
There is evidence indicating the use of ART during early pregnancy can decrease the risk of HIV transmission from mother to child to less than 2%.20 However, in countries like Ethiopia, access to HIV treatment and awareness of PMCT services remains low.
Despite the progress, poor knowledge and awareness of PMTCT is a major hindrance to the success of the program.21 In Ethiopia, the level of knowledge on the MTCT is very low during the three-timing of transmission (pregnancy, childbirth, and breastfeeding),4,22 a study conducted in Northwest Ethiopia showed that 57.5% of the respondents had full knowledge about those modes of transmission but only 17.4% knew the possible prevention method.23
In line with the UNAIDS Strategic Plan, the government of Ethiopia has adopted the 90-90-90 targets.24 In Ethiopia, 79%, 71%, and 87% knew their status, are on ART, and attained viral suppression, respectively.24
According to the 2019 Ethiopian Demographic health survey, 50% of women still deliver at home without a skilled birth attendant.25 Assessing factors associated with fertility desire and PMTCT knowledge among HIV-positive men and women are useful for policymakers and program implementers to design evidence-based intervention strategies to tackle the problem. Furthermore, evidence-based estimation of the magnitude of fertility desire and knowledge of PMCT is a cornerstone for tracking progress towards the prevention of mother-to-child transmission of HIV.
Despite WHO’s zero HIV infection target among children aged 0–14 years by the year 2020, there still exists a significant mother-to-child transmission of HIV in Ethiopia. Adequate access to HIV prevention, care, and treatment services for women is proven to decrease MTCT of HIV. This could be ensured by understanding fertility desire and prevention knowledge of men and women. Even though studies have been conducted in Ethiopia concerning fertility desire and PMTCT knowledge male partners’ fertility desire and PMTCT knowledge gained little attention. Thus, this study addresses both men’s and women’s fertility desire and PMTCT knowledge and attempts to improve current knowledge and notify the stakeholders to put efforts to improve the health of men and women living with HIV/AIDS in the study area.
Methods and Materials
Study Area
The study was conducted in west Shewa zone public hospitals, according to a 2007 population survey the Zone has a total population of more than 2 million, of whom more than half were women. Currently, there are about 495,753 women of reproductive age in this zone. There are around 100,283 mothers who give birth per year. West Shewa zone has 22 woredas with over 526 rural kebeles and 58 urban kebele with 8 hospitals and 91 health centers. Currently, according to the zone’s health department, 24 health facilities are providing ART services for a total population of 8785 people in the west Shewa zone.
Study Design and Period
A facility-based cross-sectional study design was conducted from September to October 2019.
Source and Study Population
All HIV-positive men and women of reproductive age group attending ART clinic in west Shewa zone were included in the source population. All HIV-positive men and women of reproductive age group attending ART clinic at ten randomly selected health facilities in the zone were included in the study population. Men and women attending ART clinic and were already pregnant were excluded from the study.
Sample Size Determination
The sample size was determined for the four objectives of the study, and the highest sample size was taken as the final sample size. Accordingly, the sample for the first objective (prevalence of fertility desire) size was determined by using a single proportion formula with the assumption of fertility intention among HIV-positive women 39.1%,3 5% of marginal error, and 95% confidence level. Ie 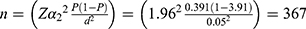 . The sample size for the second objective (knowledge of PMTCT) was determined similarly by using prevalence of PMTCT 34.9% from study conducted in Ethiopia22 with a sample size of 349. For the third and fourth objectives, the sample size was calculated by using epi info version 7.2.4.0 by using the parameters from the studies conducted in Fitche hospital3 and Ethiopia22 for the fertility desire and PMTCT knowledge, respectively (Table 1). Finally, by taking the highest sample size amongst the four objectives and adding a 10% non-response rate, and design effect of 1.5, the final calculated sample size was 606.
. The sample size for the second objective (knowledge of PMTCT) was determined similarly by using prevalence of PMTCT 34.9% from study conducted in Ethiopia22 with a sample size of 349. For the third and fourth objectives, the sample size was calculated by using epi info version 7.2.4.0 by using the parameters from the studies conducted in Fitche hospital3 and Ethiopia22 for the fertility desire and PMTCT knowledge, respectively (Table 1). Finally, by taking the highest sample size amongst the four objectives and adding a 10% non-response rate, and design effect of 1.5, the final calculated sample size was 606.
 |
Table 1 Sample Size Calculation for Factors Associated with Fertility Desire and Knowledge of PMTCT |
Sampling Technique
A multistage sampling technique was employed to select the study participants. Seven woredas among 22 woredas of the West Shewa zone (Bako-Tibe, Dandi woreda, Ada’a Berga, Ambo woreda, Caliya woreda, Jibat woreda, Toke Kutaye woreda) were selected by simple random sampling using a lottery method. In this study, 10 public health institutions that provide ART services were included from the selected woredas. The final sample size was obtained by proportionally allocating to these selected public health institutions by considering their monthly ART patient flows. Lastly, subjects were selected by systematic random sampling, based on an assessment of each health facility’s three-month patient flow, ie Kth= N/n (7448/606 ≈ 12). HIV-positive women attending ART services were recruited as study units in each health facility until the total sample size for this study was obtained (Figure 1).
 |
Figure 1 Schematic presentation of sampling frame of fertility desire and knowledge level on PMTCT among HIV positive women, west shoe Oromia Region, Ethiopia 2020. |
Study Variables
Dependent Variables
Fertility desire and PMTCT knowledge.
Independent Variables
Sociodemographic factors (age, education, sex, residence, marital status, occupation, and income), obstetric factors (history of abortion, number of pregnancies, number of alive children), HIV/AIDS-related characteristics (a year since diagnosis, voluntary HIV testing, status disclosure, years on ART) and knowledge of HIV transmission during pregnancy, childbirth, and breastfeeding were independent variables of the study.
Operational Definitions
Fertility Desires
Investigated using the question “Would you like to have children in the future?” and the variable was dichotomized into “had no desire” if a participant answered “No”, and “had fertility desire” if they answered “Yes”.3
PMTCT Knowledge
Knowledge index was built from the answers to a total of five questions, which are categorized under three main timings of HIV prevention from mother to child (three questions under antiretroviral therapy (ART) drugs use during pregnancy, one question during the time of delivery, and one question during exclusive breastfeeding up to 6 months); then, the index was categorized as not full knowledge (score,3) and full knowledge (score =3).23
Data Collection Instruments and Procedures
The data collection tool was adopted from previous similar studies3,9,23,26 and adapted to the local context. The data collection instrument was prepared in English and translated into the local language (Afaan Oromoo) by an expert and translated back to English by another expert to ensure consistency and accuracy. An interviewer-administered structured questionnaire was used as a data collection instrument by 15 trained data collectors with a BSc degree in health science and a supervisor for each study institution with an MSc degree.
Data Analysis
The pre-coded responses were double entered into EPI data version 4.6 software; then, it was exported to SPSS version 26 for statistical analysis. Percentage, frequency, table, and charts were employed to describe the variables. Bivariate and multivariable logistic regression was fitted to identify a statistical association between dependent and independent variables. Variables with a p-value of less than 0.2 at the bivariate level were included in the multivariable logistic regression model. Finally, adjusted odds ratios with 95% confidence interval were employed to declare strength, directions of association between dependent and independent variables, and a P-value of <0.05 was used to declare statistical significance.
Data Quality Assurance
Pretest was conducted on 5% of the sample in Holota health center. Supervision by nine supervisors and the principal investigator of how data collectors administer the questions to the respondents. On spot, the questionnaire was reviewed by supervisors and the Principal investigators to check for completeness and further edition. The necessary feedback was offered to data collectors.
Ethical Consideration
Before the data collection process, ethical clearance was obtained from the Research and Ethical Review Committee of the college of medicine and health science, Ambo University. A supportive letter was obtained from the Midwifery department to the West Shewa zone health office and from the West Shewa zone health department permission letter for data collection to each institution was obtained. Verbal consent was taken from each respondent on the confidentiality of their response after being approved by the Research and Ethical Review Committee of Ambo University. The participants were informed about the purpose of the study, per the Declaration of Helsinki.
Result
Sociodemographic Characteristics of the Study Participants
In this study, a total of 590 participants responded making the response rate of 97.4%. The mean age of the respondents was 35.64 with a standard deviation of 7.84. The majority 381 (64.6%) of the participants were female and more than half 314 (53.2%) of them were rural residents. More than one-third 221 (37.5%) of the wives were unable to read and write, whereas the majority 254 (43.1%) of the husbands had a completed secondary education (Table 2).
 |
Table 2 Sociodemographic Characteristics of the Study Participants Attending ART Clinic in West Shewa Zone Public Health Facilities, 2020 |
HIV/AIDS and Related Characteristics
More than two-third 396 (67.1%) of the respondents had voluntarily undergone HIV test when they received their HIV status and 276 (46.8%) of them underwent the test to know their HIV status (Figure 2). Majority 340 (57.6%) of the respondents were on ART for five and fewer years. Among the female respondents, 20 (3.4%) of them were currently pregnant, 241 (40.8%) had 2–4 pregnancies and 251 (42.5%) of them had 2–4 live births (Table 3).
 |
Table 3 HIV/AIDS and Related Characteristics of the Study Participants Attending ART Clinic in West Shewa Zone Public Health Facilities, 2020 |
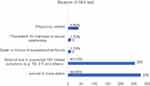 |
Figure 2 Reason of HIV test of the study participants attending ART clinic in west Shewa zone public health facilities, 2020. |
Fertility Desire and PMTCT Knowledge
The majority 324 (54.9%) of the participants responded that HIV is not transmitted during pregnancy and 440 (74.6%) believe that ART can reduce the risk of transmission of HIV/AIDS from mother to child. The majority 429 (72.7%) of the respondents recognize that ART can decrease HIV transmission during breastfeeding and 409 (69.3%) of them distinguish ART can decrease HIV transmission during delivery from mother to child (Table 4). The majority 347 (58.8%) of the respondents wanted to have at least one child with a 95% CI (54.7–62.9) and 181 (30.7%) of them had good knowledge of the prevention of transmission of HIV from mother to child, 95 CI (26.9–34.2) (Figures 3 and 4).
 |
Table 4 Knowledge of Prevention of HIV Transmission from Mother to Child of the Study Participants Attending ART Clinic in West Shewa Zone Public Health Facilities, 2020 |
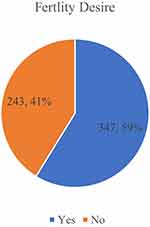 |
Figure 3 Prevalence of fertility desire of the study participants attending ART clinic in west Shewa zone public health facilities, 2020. |
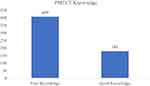 |
Figure 4 Level of knowledge of the study participants attending ART clinic in west Shewa zone public health facilities, 2020. |
Factors Associated with Fertility Desire
The odds of fertility desire among the respondents aged 26–35 years were 4.6 times higher than those aged greater than 35 years [AOR=4.64, 95% CI (2.75–7.85)]. Households with a husband who was unable to read and write, primary and secondary education were 93% [AOR=0.07, 95% CI (0.02–0.23)], 77.7% [AOR=0.22, 95% CI (0.09–0.56)], and 68.2% [AOR= 0.32, 95% CI (0.14–0.73)] less likely to desire at least one child, respectively. The odds of fertility desire among Housewives were 3.14 times higher than other occupations [AOR=3.14, 95% CI (1.90–5.21)]. Likewise, merchants had more than five times the odds of fertility desire than other occupations [AOR=5.31, 95% CI (2.55–11.05)] (Table 5).
 |
Table 5 Factors Associated with Fertility Desire Among Participants Attending ART Clinic in West Shewa Zone Public Health Facilities, 2020 |
Respondents who received their test result 1–4 years were 67.4% less likely to desire fertility than those who have known their status for 9–12 years [AOR=0.33, 95% CI (0.12-0.86)]. The odds of fertility desire among participants who have been on ART for ≤5 years were more than five times higher than those who were on ART for more than five years [AOR=5.13, 95% CI (2.37–11.12)]. Those voluntarily tested to know their HIV status had the odds of fertility desire more than two times higher than those tested for other indications [AOR=2.16, 95% CI (1.30–3.58)] (Table 5).
Factors Associated with Knowledge of PMTCT
The odds of PMTCT knowledge among the respondents aged less than 25 years were two and a half higher than those aged greater than 35 years [AOR=2.53, 95% CI (1.32–4.86)]. Likewise, respondents who underwent voluntary testing during HIV diagnosis had 55% higher odds of PMTCT knowledge than those tested by an indication during health facility visit for other reasons [AOR=1.55, 95% CI (1.03–2.35)].
Also, the odds of PMTCT knowledge were about twice higher for the respondents who were on ART for more than five years when compared with those who had been on ART for less than five years [AOR=1.94, 95% CI (1.26–2.98)] (Table 6).
 |
Table 6 Factors Associated with Knowledge of PMTCT Among Study Participants Attending ART Clinic in West Shewa Zone Public Health Facilities, 2020 |
Discussion
Prevention of mother-to-child transmission of HIV during pregnancy, childbirth, and breastfeeding is a key component of the UNAIDS Strategic Plan on HIV/AIDS. This study assessed the prevalence and factors associated with fertility desire and PMTCT knowledge. Accordingly, the prevalence of fertility desire and knowledge of PMTCT in the study area were 58.8% and 30.7%, respectively. Younger age, husband education, occupation, recent HIV test, and voluntary testing were significantly associated with fertility desire. Likewise, the younger age group, voluntary testing, and those on ART for more than five years had higher odds of PMTCT knowledge.
The prevalence of fertility desire in the study area was 58.8%. This finding is higher than the prevalence reported in Finote Selam hospital, Northwest Ethiopia (33.4%),8 Addis Ababa, Ethiopia (44%),10 Northwest Ethiopia (40.3%),9 Tigray region, Ethiopia (45.5%),11 and Jimma town, South West Ethiopia (46.8%).12 This might be due to the difference in the study population, the current study used both men and women as study participants. The results of this study are consistent with the studies done among 15- to 49-year-old people living with HIV/AIDS in Addis Ababa, Ethiopia (54.6%)18 and Harari region of Ethiopia (56.2%).15
According to this study, 30.7% of the study participants had good knowledge of the prevention of transmission of HIV from mother to child. This result is lower than the study Hawassa Referral hospital (82.3%)27 and East Gojjam, Northern Ethiopia (52%).28 This finding is also lower than the knowledge of PMTCT nationally, 57% and Oromia region (51.7%),4 but higher than the studies reported in Assosa town, Northwest Ethiopia (17.4%)23 and Mecha district, Northwest Ethiopia (22.4%).29 This might be due to the inadequate counseling of transmission mechanisms of HIV from mother to child during pregnancy, childbirth, and postnatal periods, especially a gap in involving a male partner.
The odds of fertility desire among the younger age were higher when compared with the older age group. This finding is consistent with a study done in Southern India,14 Addis Ababa Ethiopia,10 Fitche Ethiopia,3 and Harari region, Ethiopia.15 The younger age group might want a large family size, and the fertility rate is contrary to the older age group, which might have reached the family size they desire.
According to this study, lower educational status is negatively associated with fertility desire. This is consistent with studies done in Northwest Ethiopia9 and Jimma Town, South West Ethiopia12 but inconsistent with the study done in Western Ethiopia.17 Educational status is directly associated with knowledge of PMTCT during pregnancy, childbirth, and breastfeeding, which decreases the fear of transmission from mother to child, making fertility desire more likely. They also educated people to have access to media through which they get the mode of transmission and prevention mechanisms of HIV from mother to child.
The study results showed that the fertility desire among housewives and merchants was higher when compared with students, daily laborers, and private employees. This could be due to students; daily laborers are economically dependent to make their fertility choice and also time constraints to care for the child can their desire.
Respondents who received their test results in recent times had higher fertility desires than their counterparts. The difference could be due to the advancement in HIV treatment and prevention from mother to child in recent times. Also, the incidence of HIV infection is higher among the younger age group in which group fertility desire is higher.
The odds of fertility desire among participants who have been on ART for less than five years were more than six times higher than those who were on ART for more than five years. The result was consistent with the study conducted at Finote Selam hospital Northwest Ethiopia.8 This could be due to ART immediately improving their health status in the early years of medication. Those voluntarily tested to know their HIV status had the odds of fertility desire more than twice higher than those tested for other indications. This might be due to voluntary testing being associated with good adherence, contrary to those tested for other indications like opportunistic infections.
The odds of PMTCT knowledge among the younger respondents were two and a half higher than those aged greater than 35 years. Increasing social media to use share and get information about HIV among younger age groups (18–40 years) might have played a role.30 Likewise, respondents who underwent voluntary testing during HIV diagnosis had 55% higher odds of PMTCT knowledge than those tested for other indications during health facility visits for other reasons.
Also, the odds of PMTCT knowledge were about twice times higher for the respondents who were on ART for more than five years when compared with those who had been on ART for less than five years. This could be due to those who had been on ART for a longer period having vigorous service counseling when receiving the follow-up with health professionals.
Limitation and Strength of the Study
The limitation of the study is that since the study was a facility-based cross-sectional study, the findings may not represent the general HIV-positive women and men. Also, the respondents were asked about their history, and a recall bias could not be avoided. The strength of the study was both male and female fertility, and PMTCT perspective was assessed.
Conclusion
The prevalence of fertility desire in the study area was higher than studies conducted in other parts of the country. Knowledge of PMTCT in the study area was lower than the national survey reported in 2016. Younger age, husband education, occupation, recent HIV test, and voluntary testing and counseling were significantly associated with fertility desire. Likewise, the younger age group, voluntary testing and counseling, and those on ART for more than five years had higher odds of PMTCT knowledge. Therefore, strengthening voluntary testing and counseling throughout the follow-up care is of paramount importance to decrease MTCT.
Data Sharing Statement
All the datasets used and/or analyzed during the current study are available from the corresponding author’s reasonable request.
Acknowledgment
The authors are indebted to Ambo University for the financial support, West Shewa Zone health office for the permission letter to the health institutions, study participants, and data collectors for their information and time.
Author Contributions
All authors have made considerable contributions to the conception, design, analysis, and interpretation of the data. The authors have also read and agreed to the final manuscript and to which journal it is submitted. All authors have also agreed to be accountable for all aspects of the work.
Funding
The financial support for the study was obtained from Ambo University, the office of the research, and community services. The university has no role in the design of the study, collection, analysis, and interpretation of the data.
Disclosure
The authors declare that they have no competing interests.
References
1. World Health Organization. Global Progress Report on HIV, Viral Hepatitis and Sexually Transmitted Infections, 2021: Accountability for the Global Health Sector Strategies 2016–2021: Actions for Impact; 2021.
2. Karim SSA, Baxter C. HIV incidence rates in adolescent girls and young women in sub-Saharan Africa. Lancet Glob Health. 2019;7:e1470–e1471. doi:10.1016/S2214-109X(19)30404-8
3. Demissie DB, Tebeje B, Tesfaye T. Fertility desire and associated factors among people living with HIV attending antiretroviral therapy clinic in Ethiopia. BMC Pregnancy Childbirth. 2014;14(1):1–10. doi:10.1186/s12884-014-0382-2
4. Demographic I. Health Survey 2016: Key Indicators Report. Addis Ababa, Ethiopia, and Rockville, Maryland, USA; 2016.
5. Mojola SA, Wamoyi J. Contextual drivers of HIV risk among young African women. J Int AIDS Soc. 2019;22(S4):e25302. doi:10.1002/jia2.25302
6. Kuete M, Yuan H, He Q, et al. Sexual practices, fertility intentions, and awareness to prevent mother-to-child transmission of HIV among infected pregnant women at the Yaounde central hospital. Sex Med. 2016;4:e97–e105. doi:10.1016/j.esxm.2016.01.004
7. Moretton MA, Bertera F, Lagomarsino E, Riedel J, Chiappetta DA, Höcht C. Advances in therapy for the prevention of HIV transmission from mother to child. Expert Opin Pharmacother. 2017;18(7):657–666. doi:10.1080/14656566.2017.1316369
8. Abbawa F, Awoke W, Alemu Y. Fertility desire and associated factors among clients on highly active antiretroviral treatment at finoFinote Selam hospital Northwest Ethiopia: a cross-sectional study. Reprod Health. 2015;12:1–7. doi:10.1186/s12978-015-0063-2
9. Mekonnen B, Minyihun A. Fertility desire and associated factors among HIV positive women attending ART clinics in Amhara Region referral hospitals in Northwest Ethiopia, 2017. HIV/AIDS. 2019;11:247.
10. Asfaw HM, Gashe FE. Fertility intentions among HIV positive women aged 18–49 years in Addis Ababa Ethiopia: a cross-sectional study. Reprod Health. 2014;11:1–8. doi:10.1186/1742-4755-11-36
11. Melaku YA, Zeleke EG, Kinsman J, Abraha AK. Fertility desire among HIV-positive women in Tigray region, Ethiopia: implications for the provision of reproductive health and prevention of mother-to-child HIV transmission services. BMC Womens Health. 2014;14:1–10. doi:10.1186/s12905-014-0137-2
12. Shiferaw T, Kiros G, Birhanu Z, Gebreyesus H, Berhe T, Teweldemedhin M. Fertility desire and associated factors among women on the reproductive age group of antiretroviral treatment users in Jimma Town, South West Ethiopia. BMC Res Notes. 2019;12:1–8. doi:10.1186/s13104-019-4190-7
13. Mokwena K, Bogale YR. Fertility intention and use of contraception among women living with the human immunodeficiency virus in Oromia Region, Ethiopia. S Afr Fam Pract. 2017;59:46–51. doi:10.1080/20786190.2016.1254931
14. Jose H, Madi D, Chowta N, et al. Fertility desires and intentions among people living with HIV/AIDS (PLWHA) in Southern India. J Clin Diagn Res. 2016;10:OC19.
15. Haile F, Isahak N, Dessie A. Fertility desire and associated factors among people living with HIV on ART in Harari Regional State, Eastern Ethiopia. J Trop Dis. 2014;2:3.
16. Jones DL, Cook R, Potter JE, et al. Fertility desires among women living with HIV. PLoS One. 2016;11(9):e0160190. doi:10.1371/journal.pone.0160190
17. Melka AS, Wordofa MA, Wossen BA. Determinants of fertility intention among women living with HIV in western Ethiopia: implications for service delivery. Afr J Reprod Health. 2014;18:54–60.
18. Adilo TM, Wordofa HM. Prevalence of fertility desire and its associated factors among 15-to 49-year-old people living with HIV/AIDS in Addis Ababa, Ethiopia: a cross-sectional study design. HIV/AIDS. 2017;9:167.
19. Getachew M, Alemseged F, Abera M, Deribew A. Factors affecting fertility decisions of married men and women living with HIV in South Wollo Zone, Northeast Ethiopia. Ethiop J Health Dev. 2010;24. doi:10.4314/ejhd.v24i3.68388
20. Nygren-krug H. The joint United Nations programme on HIV/AIDS: With communities for human rights. In Human Rights in Global Health: Oxford University press. 2018:281.
21. Ramoshaba R, Sithole SL. Knowledge and awareness of MTCT and PMTCT post-natal follow-up services among HIV infected mothers in the Mankweng Region, South Africa. Open AIDS J. 2017;11(1):36–44. doi:10.2174/1874613601711010036
22. Luba TR, Feng Z, Gebremedhin SA, et al. Knowledge about mother–to–child transmission of HIV, its prevention and associated factors among Ethiopian women. J Glob Health. 2017;7:020414.
23. Abtew S, Awoke W, Asrat A. Knowledge of pregnant women on mother-to-child transmission of HIV, its prevention, and associated factors in Assosa town, Northwest Ethiopia. HIV/AIDS. 2016;8:101.
24. Office FHAPaC. HIV Prevention in Ethiopia. Addis Ababa: National Road Map; 2018.
25. Mini E; Demographic E. Health Survey 2019: Key Indicators Report. The DHS Program ICF; 2019.
26. Adal M. Systematic review on HIV situation in Addis Ababa, Ethiopia. BMC Public Health. 2019;19(1):1544. doi:10.1186/s12889-019-7885-8
27. Abajobir AA, Zeleke AB. Knowledge, attitude, practice, and factors associated with prevention of mother-to-child transmission of HIV/AIDS among pregnant mothers attending antenatal clinic in Hawassa referral hospital, South Ethiopia. J AIDS Clin Res. 2013;4:2–7. doi:10.4172/2155-6113.1000215
28. Alemu YM, Habtewold TD, Alemu SM. Mother’s knowledge on prevention of mother-to-child transmission of HIV, Ethiopia: a cross-sectional study. PLoS One. 2018;13:e0203043. doi:10.1371/journal.pone.0203043
29. Liyeh TM, Cherkose EA, Limenih MA, Yimer TS, Tebeje HD. Knowledge of prevention of mother to child transmission of HIV among women of reproductive age group and associated factors at Mecha district, Northwest Ethiopia. BMC Res Notes. 2020;13(1):1–6. doi:10.1186/s13104-020-05005-5
30. Taggart T, Grewe ME, Conserve DF, Gliwa C, Isler MR. Social media and HIV: a systematic review of uses of social media in HIV communication. J Med Internet Res. 2015;17(11):e248. doi:10.2196/jmir.4387
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
