Back to Journals » Clinical Ophthalmology » Volume 10
Femtosecond laser-assisted in situ keratomileusis multifocal ablation profile using a mini-monovision approach for presbyopic patients with hyperopia
Authors Vastardis I, Pajic-Eggspuehler B, Müller J, Cvejic Z, Pajic B
Received 7 December 2015
Accepted for publication 22 April 2016
Published 14 July 2016 Volume 2016:10 Pages 1245—1256
DOI https://doi.org/10.2147/OPTH.S102008
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Iraklis Vastardis,1 Brigitte Pajic-Eggspühler,1 Jörg Müller,1,2 Zeljka Cvejic,2 Bojan Pajic,1–4
1Swiss Eye Research Foundation, Orasis Eye Clinic, Aargau, Reinach, Switzerland; 2Faculty of Physics, University of Novi Sad, Novi Sad, Serbia; 3Department of Ophthalmology, Geneva University Hospitals, Geneva, Switzerland; 4Medical Faculty, Military Medical Academy, University of Defence, Belgrade, Serbia
Purpose: To report the visual outcomes of the femtosecond laser-assisted multifocal aspheric corneal ablation profile using a mini-monovision approach and to evaluate if corneal multifocality was effective, and to report the relative benefits of this approach.
Patients and methods: Bilateral femtosecond laser-assisted in situ keratomileusis using a multifocal aspheric corneal ablation profile was performed on 19 hyperopic patients (38 eyes). They were divided into two groups based on eye dominance: dominant eye (DE) group targeting emmetropia and the nondominant eye (NDE) group targeting -0.5 D slight myopia. The uncorrected distance visual acuity (UDVA), uncorrected intermediate visual acuity (UIVA), uncorrected near visual acuity (UNVA), and retreatment rates were reported from baseline to 6 months.
Results: The UNVA, UIVA, and UDVA improved significantly in both groups (Kruskal–Wallis test, DE and NDE: P<0.00001, P<0.000005, and P=0.00001, respectively). Corrected distance visual acuity (CDVA) baseline was better in both groups in comparison to UDVA at 6 months (Wilcoxon test, DE: P<0.001, 95% confidence interval (CI) of the median 0.0–0.0 LogMAR and 0.1000–0.1218 LogMAR and NDE: P=0.010, 95% CI of the median 0.0–0.0 LogMAR and 0.00–0.10 LogMAR). There was a significant loss of lines between CDVA baseline and UDVA at 6 months in both groups (DE group: 68% of eyes lost one line or more; NDE group: 58% of eyes lost one line or more). The corrected near visual acuity baseline compared to UNVA at 6 months was not statistically important (Wilcoxon test, DE: P=0.8125, 95% CI of the median 0.0–0.0 LogMAR and 0.0–0.0 LogMAR and NDE: P=0.82, 95% CI of the median 0.0–0.0 LogMAR and 0.0–0.0 LogMAR). The comparison among the UDVA, UIVA, and UNVA between the two groups at baseline and during all follow-ups was not statistically important. Two cases from the DE group were retreated (6%).
Conclusion: Use of this multifocal aspheric corneal ablation profile in patients with hyperopic presbyopia significantly improved UDVA, UIVA, and UNVA. This improvement was due to created multifocality of the cornea. The mini-monovision seems not to affect UDVA, UIVA, and UNVA between the two groups. The retreatment rates at the 6-month evaluation were significantly less in our study when compared with other studies. This method seems to improve UDVA, UIVA, and UNVA but could result in a significant statistical difference between CDVA baseline and UDVA at 6 months that leads to loss of lines in distance vision. Despite promising results, this is a preliminary evaluation of this new profile, and a larger number of eyes are needed to verify visual outcomes, retreatment rates, and safety.
Keywords: presbyopia, hyperopia, Femto LASIK, presbyLasik, visual acuity
Introduction
Presbyopia correction techniques are improving, although they remain an active area of research in the field of refractive surgery. Two major surgical approaches exist today, which attempt to give presbyopes good vision at distance, intermediate and near viewing distances: the static and the dynamic approaches.1 Static methods broadly adopt the same optical techniques as those used in presbyopic contact lens correction and aim to satisfy the needs of the presbyope by increasing binocular depth of focus, often using monovision as well as simultaneous imagery. Dynamic methods generally attempt to make use of at least some of the still-active elements of the accommodation system. They include procedures that are supposed to modify the relative geometry of the ciliary muscle and lens or reduce the stiffness of the presbyopic lens either by replacing it with other natural or man-made material or by subjecting it to femtosecond laser treatment. Alternatively, the natural lens may be replaced by some form of intraocular lens (IOL), which changes power as a result of forces derived from the still-active ciliary muscle, zonule and capsule, or other sources.1
Based on these approaches, techniques used to mimic accommodation include surgical removal of the lens followed by implantation of pseudoaccommodative intraocular lenses, the use of multifocal corneal treatments, or creation of asphericity of the cornea with an excimer laser, or as recently described, by inducing central corneal steepening and asphericity through a customized collagen cross-linking (CXL) method.2–7 Same principles have led to the development of premium IOLs, corneal inlays, and presbyLasik profiles.1,7–14 Corneal approaches could offer the chance to provide a reliable treatment of presbyopia. Despite some promising initial results, current techniques are far from clinically optimal, and as such, more investigation is needed.2–4,14–17
We evaluated a recently developed European Conformity marked multifocal aspheric corneal ablation profile. This new presbyLasik algorithm is an aspheric treatment that differs from previous central or peripheral presbyLasik profiles because no transitional zones are created. Near vision is facilitated by creating an elevation within the 3 mm zone. This modification provides the necessary additional refractive power for near vision, at the expense of increased spherical aberration. This multifocality (central 3 mm for near vision and 3–6 mm for distance vision) may also be perceived as increasing the depth of field. In this kind of method, the major argument is that a better UNVA and UIVA are created through a mini-monovision effect or through an induced myopia because a hyperpositive elevation in the 3 mm zone is created. Should this be true, the treatment would result in an insufficient UDVA at 6 months postoperative and possibly high retreatment rates. Assuming that our null hypothesis is correct and a multifocal cornea is indeed created, then we should expect also an equal improvement on the UDVA on both groups equal and no different results between the groups. Should the hypothesis be rejected, then the dominant eye (DE) group should have a better UDVA and worse UIVA and UNVA, while the nondominant eye (NDE) group should have the opposite effect. The alternative hypothesis would be that a monovision effect was created. We evaluated the refractive outcomes of this new algorithm in a preliminary evaluation with the DE group targeting emmetropia and NDE group targeting −0.5 D over a follow-up period of 6 months.
Patients and methods
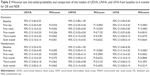
This preliminary evaluation of this new profile included 19 hyperopic patients (12 males) with presbyopia who underwent a same session of bilateral femtosecond laser-assisted in situ keratomileusis (LASIK) multifocal aspheric corneal ablation treatment. All procedures were carried out by the same surgeon (BP) minimizing the effect of surgical variability by the operator at Orasis Eye Clinic in Switzerland. All patients provided written informed consent; the local ethics committee (Kantonale Ethikkommission Nordwest, Aargau, Switzerland) approved all procedures in advance. Demographic data and clinical settings are demonstrated in Table 1.
  | Table 1 Clinical settings and demographic data of the patients in this study |
Table 2 lists the inclusion and exclusion criteria used in participant selection.
  | Table 2 Inclusion and exclusion criteria of the study |
DE and NDE groups were determined with the Dolman method (hole in the card test) during the ophthalmological evaluation. Eleven right and eight left DE targeted emmetropia, while 19 NDE targeted −0.5 D of myopia.
The following initial nomogram was used on the DE group as recommended:
- If up to +1 D manifest refraction spherical equivalent (MRSE), then we treated +0.25 D less sphere.
- If +1.5–+2.0 D MRSE, then we treated +0.5 D less sphere.
- If +2.5 D or more MRSE, then we treated +0.75 D less sphere.
On the NDE, the initial recommended nomogram was tweaked and overcorrection targeting −0.5 D myopia was performed.
Our null hypothesis is that a better UDVA, UNVA, and UIVA were created through induced multifocality on the cornea in both groups. Should this be true, then the visual outcomes between the groups should not be different to each other.
All patients received a full anterior and posterior segment evaluation prior to surgery. Scheduled eye exams took place 1 week prior to surgery, on the first day, first week, first month, third month, and sixth month after surgery. Corneal reflection scanning slit topography was performed prior to surgery and at each scheduled follow-up and wavefront Hartmann–Schack aberrometry prior to surgery and at 6 months. The pupils were measured during mesopic and skotopic conditions prior to surgery and the induced spherical aberrations at baseline and 6 months under mesopic and skotopic conditions with wavefront Hartmann–Schack aberrometry. Monocular UDVA and CDVA were measured and recorded at baseline and at each follow-up visit with Snellen charts and then converted to LogMAR for statistical purposes. The gain or loss of lines between baseline and 6 months was also calculated through the visual acuity conversion chart.18 Monocular corrected near visual acuity (CNVA) and UNVA were measured and recorded at baseline and at each follow-up visit at a 40 cm distance and the monocular UIVA at 80 cm, both using the Logarithmic Visual Acuity Chart 2000 “New ETDRS”. All visual acuity results were reported in the LogMAR scale.
The MRSE was analyzed and evaluated for both groups for stability purposes. Visual acuity outcomes and the total induced spherical aberrations (Z400) were analyzed and evaluated for both groups for efficiency purposes. The graph results are demonstrated in the Waring tables.19
The percentages in Waring tables were calculated with Excel 2010 through cross-multiplication. Statistical analysis was performed with Datagraph 2.70 and Medcalc 14.0. Parametric or nonparametric tests were used according to data distribution. Statistical significance was defined as P<0.05.
Results
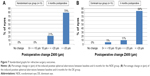
UNDA, UIVA, and UNVA improved significantly on both groups (Kruskal–Wallis test, DE: P=0.000001, P<0.000005, and P<0.000005; NDE: P<0.00001, P<0.000005, and P<0.000001, respectively) (Figure 1A–F).
On the DE group, the difference between the UDVA at baseline and after 6 months was P=0.0001 (Wilcoxon test, 95% confidence interval (CI) for the median 0.4–0.52 LogMAR at baseline and 95% CI for the median 0.1–0.18 LogMAR at 6 months). That corresponded to 16% of eyes that showed loss of one or more lines and 84% that gained more than one line (Figure 2). For the NDE group, the difference between the UDVA at baseline and after 6 months was P=0.0002 (Wilcoxon test, 95% CI for the median 0.25–0.52 LogMAR at baseline and 95% CI for the median 0.0–0.1 LogMAR at 6 months). This result corresponded to 16% of eyes that showed no gain or loss of lines, 11% that lost one line, and 73% that gained more than one line (Figure 2).
Wilcoxon test performed for UNVA at baseline and at 6 months showed a two-tailed probability P<0.0001, respectively, for the DE group, 95% CI for the median 0.8–1.0 LogMAR at baseline and 95% CI for the median 0.0–0.0 LogMAR at 6 months and for the NDE group, 95% CI for the median 0.65–1.0 LogMAR at baseline and 95% CI for the median 0.0–0.0 LogMAR at 6 months, respectively. All eyes on DE and NDE groups gained over three lines or more (Figure 3). The UIVA on both DE and NDE groups between baseline and 6 months postoperative showed similar results (Wilcoxon test P<0.0001, 95% CI for the median 0.4–0.5 LogMAR at baseline and 95% CI for the median 0.0–0.0 LogMAR at 6 months, respectively). All eyes on DE group gained one line or more and on the NDE group two lines or more (Figure 4).
Table 3 lists all Wilcoxon results in terms of UDVA, UIVA, and UNVA for the DE and NDE groups, respectively. The cumulative visual acuity results for both groups between UDVA, UNVA, and UIVA at baseline and UDVA, UNVA, and UIVA at 6 months are demonstrated in Figures 4, 5, and 6.
In comparison to UDVA and UNVA from baseline and during all follow-up in both groups, the CDVA and CNVA were always better. Table 4 lists all Wilcoxon test comparison results. However, the CDVA baseline was better for both groups in comparison to UDVA at 6 months (Wilcoxon test, DE: P<0.001, 95% CI of the median 0.0–0.0 LogMAR and 0.1000–0.1218 LogMAR, and NDE: P=0.010, 95% CI of the median 0.0–0.0 LogMAR and 0.00–0.10 LogMAR). In terms of lines, the DE group showed 68% of eyes that lost one line or more, 26% with no change, and 5% that gained one line. For the NDE group, the equivalent result was 58% of eyes that lost one line or more, 32% no change, and 11% that gained one line (Figure 2). On the other hand, the CNVA baseline compared to UNVA at 6 months was not statistically important (Wilcoxon test, DE: P=0.8125, 95% CI of the median 0.0–0.0 LogMAR and 0.0–0.0 LogMAR, and NDE: P=0.82, 95% CI of the median 0.0–0.0 LogMAR and 0.0–0.0 LogMAR). This result in terms of lines showed in the DE group 16% loss of one line, 74% of eyes with no change, and 11% gain of one line. For the NDE group, the equivalent result was 10% of eyes that lost one line or more, 74% with no change, and 16% gain of one line or more (Figure 3). The cumulative visual acuity results for both groups between CDVA and CNVA baseline and UDVA and UNVA at 6 months are demonstrated in Figures 5 and 6.
The comparison between the UDVA, UIVA, and UNVA between the two groups at baseline and during all follow-up was not statistically important. Table 5 lists all Wilcoxon results in terms of UDVA, UIVA, and UNVA between the DE and NDE groups, respectively.
Regarding the induced total spherical aberrations (Z400), there was a shift from negative to positive spherical aberrations in all eyes in both groups (Figure 7A and B).
Regarding the MRSE, 19 eyes (DE) targeted emmetropia. The NDE group was overcorrected, targeting −0.5 D of myopia. The attempted over achieved MRSE showed an overcorrection in the DE group (Figures 8 and 9A).
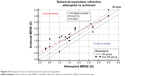  | Figure 8 Attempted versus achieved refraction spherical equivalent. |
On the NDE group, two eyes were retreated due to overcorrection (6%). Three eyes were undercorrected (7.89%), but no retreatment was made since the UDVA was not negatively affected. The NDE group showed greater MRSE stability over the follow-up period (Figure 9B).
Discussion
Presbyopia treatment is an area of enthusiastic research in refractive surgery, since the number and expectations of patients with presbyopia are increasing. During the past decades, there has been substantial effort devoted to improving surgical methods.4,14–26 Current treatment strategies to correct presbyopia, based on static or dynamic surgical approaches, include lens-based treatments, intracorneal inlays, corneal multifocality or modification of corneal asphericity, and combination approaches. All methods possess not only specific advantages, but also disadvantages: whereas corneal inlays show distinct improvement on UDVA and may carry an increased risk of scarring and haze formation, bifocal lens-based approaches improve UDVA and UNVA but may lead to glare halos and blurred vision.7,22,26–29 Corneal approaches using an excimer laser include monovision, modification of corneal asphericity, and methods inducing corneal multifocality.2,3,30–36
Recently, Kanellopoulos et al also reported a new treatment method using variable fluence and topographically customized CXL. Kanellopoulos et al described the principles and initial clinical findings regarding a novel application of topographically customized CXL method aiming to achieve a modest, nevertheless predictable, hyperopic and presbyopic refractive change. CXL was implemented in a specific, annular section mid-peripherally, employing differential response and biomechanical change, inducing central corneal steepening and asphericity changes.2,3
Our study was based on a new central presbyLasik profile. This new algorithm creates a multifocal cornea without transition zones through an elevation in the 3 mm zone. This modification provides the necessary additional refractive power for near vision, at the expense of increased spherical aberration. An aspheric treatment between 3 mm and 6 mm corrects residual refractive errors and improves far vision. This multifocality (central 3 mm for near vision and 3–6 mm for distance vision) may also be perceived as increasing the depth of field. In this kind of method, the major argument is that a better UNVA and UIVA are created through a mini-monovision effect or through an induced myopia because a hyperpositive elevation in the 3 mm zone is created. Should this be true, the treatment would result in an insufficient UDVA at 6 months postoperative with possible high retreatment rates. Our results demonstrated a significant improvement of UDVA, UIVA, and UNVA in both groups. In terms of UDVA on the DE group 6 months postoperative, 84% of eyes gained more than one line, and on the NDE group, 73% of eyes. In terms of UNVA, all eyes on the DE and the NDE groups gained over three lines or more. The UIVA at 6 months postoperative showed similar results, and all eyes on the DE group gained one line or more and on the NDE group two lines or more. A direct comparison of UIVA with other studies using PresbyLasik profiles was not possible. Studies using trifocal IOL implantation showed similar results and adequate contrast sensitivity.23–25
Although the mini-monovision effect seems to facilitate positively the UNVA and UIVA on the NDE, the comparison between the UDVA, UIVA, and UNVA between the two groups at baseline and during all follow-up was not statistically important. We believe that this new presbyLasik algorithm indeed created a multifocal corneal effect and that it provides spectacle independence.
In two recent publications, both Cosar and Sener31 and Ryan and O’Keefe32 also concluded that this procedure not only provides spectacle independence but also results in a loss of lines of CDVA at 6 months after surgery. We found a statistical difference and loss of lines in both DE and NDE groups, when the CDVA baseline was compared to UDVA at 6 months after surgery. The DE group showed 68% of eyes that lost one line or more and 58% of eyes on the NDE group with same results. We believe this result is crucial, since most of the presbyope patients anticipate having distance vision after surgery as good as spectacle distance vision before. On the other hand, the CNVA baseline compared to UNVA at 6 months after surgery was not statistically important, and in terms of lines, both groups showed 74% of eyes with no change at all.
Cosar and Sener31 treated 68 hyperopic patients (128 eyes) and reported a rate of J1 UNVA of 77.2%, while 89.4% of eyes achieved J2 or better.
Ryan and O’Keefe32 reported that 91% of patients scored an N8 or better.32 We found similar results in our study. All patients in both the DE and NDE groups, 6 months after surgery, achieved an UNVA 0.10 LogMAR (95% CI for the median 0.0000–0.0000 LogMAR) or better and were extremely satisfied with their vision during reading. Similar results were observed regarding the presbyopic correction of patients with multifocal corneal profiles or enhancement of corneal asphericity.31–36
In terms of UDVA, Cosar and Sener31 reported that 22% of eyes reached a 0.0 LogMar and 36.6% 0.1 LogMar by 6 months after surgery.
In our study, UDVA increased significantly, ranging from 0.1–0.0 LogMar (95% CI for the median 0.1000–0.1218 LogMAR) on the DE group and from 0.3–0.0 LogMar (95% CI for the median 0.00–0.10 LogMAR) for the NDE group.
Two eyes on the NDE group achieved 0.3 LogMAR due to overcorrection and were retreated (6%). In the other studies, high retreatment rates (22%) were reported suggesting that optimal UDVA results may require nomogram adjustments or an asymmetric treatment.31,32
In our eyes, this method leads to an interesting mix of results. The UNVA and UIVA results were remarkable on both DE and NDE during the entire follow-up period. We did not find statistical difference in terms of UDVA between both the groups, although optimal results in distance vision are expected when the MRSE is between −0.25 D and 0.25 D. Moreover, since distance vision correction occurs between the 3 mm and 6 mm zones, this correctional approach is also highly pupillary-dependent, especially in photopic conditions.
In our study, the retreatment rate with this approach (6%) was less when compared to 22% in previous studies,32 but we also had a smaller number of eyes tested. Spectacle independence was achieved for near and intermediate vision. All patients were satisfied with near vision the day after surgery. The overall effect of this procedure on UDVA was mediocre, but there was a gradual improvement in the UDVA until the last follow-up at 6 months. Nevertheless, the loss of one line or more after 6 months clearly demonstrates that corneal treatment approach is inferior to other presbyopia treatment methods with regard to UDVA.15,20–26
Surgeons must explain these complex outcomes to patients before surgery. Further investigation of contrast sensitivity and its role in the quality of vision after multifocal corneal ablation is needed. Also, larger studies could provide answers in terms of safety, retreatment rates, and the possible connection between the loss of lines and pupillary dependency.
Conclusion
A correction using this algorithm, with the DE targeting emmetropia and the NDE targeting slight myopia up to −0.5 D, could ensure good results for near and intermediate vision. This technique provided spectacle independence, showing that it could confer certain advantages in presbyopia treatment. However, the statistically and clinically important difference between CDVA and UDVA and the loss of lines are major disadvantages, especially when the approach is compared to other presbyopia correction technologies.7,21,23–25
Disclosure
The authors report no conflicts of interest in this work.
References
Charman WN. Developments in the correction of presbyopia II: surgical approaches. Ophthalmic Physiol Opt. 2014;34(4):397–426. | ||
Kanellopoulos AJ, Asimellis G. Hyperopic correction: clinical validation with epithelium-on and epithelium-off protocols, using variable fluence and topographically customized collagen corneal crosslinking. Clin Ophthalmol. 2014;8:2425–2433. | ||
Kanellopoulos AJ, Asimellis G. Presbyopic PiXL cross-linking. Curr Ophthalmol Rep. 2015;3(1):1–8. | ||
Uy E, Go R. Pseudoaccommodative cornea treatment using the NIDEK EC-5000 CXIII excimer laser in myopic and hyperopic presbyopes. J Refract Surg. 2009;25(1 suppl):S148–S155. | ||
Telandro A. The pseudoaccommodative cornea multifocal ablation with a center-distance pattern: a review. J Refract Surg. 2009;25(1 suppl):S156–S159. | ||
Cillino S, Casuccio A, Di Pace F, et al. One-year outcomes with new-generation multifocal intraocular lenses. Ophthalmology. 2008;115(9):1508–1516. | ||
Agresta B, Knorz MC, Kohnen T, Donatti C, Jackson D. Distance and near visual acuity improvement after implantation of multifocal intraocular lenses in cataract patients with presbyopia: a systematic review. J Refract Surg. 2012;28(6):426–435. | ||
Cillino G, Casuccio A, Pasti M, Bono V, Mencucci R, Cillino S. Working-age cataract patients: visual results, reading performance, and quality of life with three diffractive multifocal intraocular lenses. Ophthalmology. 2014;121(1):34–44. | ||
Lindstrom RL, Macrae SM, Pepose JS, Hoopes PC. Corneal inlays for presbyopia correction. Curr Opin Ophthalmol. 2013;24(4):281–287. | ||
Yilmaz OF, Bayraktar S, Agca A, Yilmaz B, McDonald MB, van de Pol C. Intracorneal inlay for the surgical correction of presbyopia. J Cataract Refract Surg. 2008;34(11):1921–1927. | ||
Bouzoukis DI, Kymionis GD, Limnopoulou AN, Kounis GA, Pallikaris IG. Femtosecond laser-assisted corneal pocket creation using a mask for inlay implantation. J Refract Surg. 2011;27(11): 818–820. | ||
Baudu P, Penin F, Arba Mosquera S. Uncorrected binocular performance after biaspheric ablation profile for presbyopic corneal treatment using AMARIS with the PresbyMAX module. Am J Ophthalmol. 2013;155(4):636–647. | ||
Luger MH, Ewering T, Arba-Mosquera S. One-year experience in presbyopia correction with biaspheric multifocal central presbyopia laser in situ keratomileusis. Cornea. 2013;32(5):644–652. | ||
Telandro A. Pseudo-accommodative cornea: a new concept for correction of presbyopia. J Refract Surg. 2004;20(5 suppl):S714–S717. | ||
Patel S, Alió JL, Feinbaum C. Comparison of Acri Smart multifocal IOL, crystalens AT-45 accommodative IOL, and Technovision presbyLASIK for correcting presbyopia. J Refract Surg. 2008;24(3):294–299. | ||
Pinelli R, Ortiz D, Simonetto A, Bacchi C, Sala E, Alió JL. Correction of presbyopia in hyperopia with a center-distance, paracentral-near technique using the Technolas 217z platform. J Refract Surg. 2008;24(5):494–500. | ||
Epstein RL, Gurgos MA. Presbyopia treatment by monocular peripheral presbyLASIK. J Refract Surg. 2009;25(6):516–523. | ||
Holladay JT. Visual acuity measurements. J Cataract Refract Surg. 2004;30(2):287–290. | ||
Waring GO 3rd, Reinstein DZ, Dupps WJ, et al. Standardized graphs and terms for refractive surgery results. J Refract Surg. 2011;27(1):7–9. Erratum in J Refract Surg. 2011;27(2):88. | ||
Tomita M, Huseynova T. Evaluating the short-term results of KAMRA inlay implantation using real-time optical coherence tomography-guided femtosecond laser technology. J Refract Surg. 2014;30(5):326–329. | ||
Huseynova T, Kanamori T, Waring GO 4th, Tomita M. Outcomes of small aperture corneal inlay implantation in patients with pseudophakia. J Refract Surg. 2014;30(2):110–116. | ||
Mulet ME, Alio JL, Knorz MC. Hydrogel intracorneal inlays for the correction of hyperopia: outcomes and complications after 5 years of follow-up. Ophthalmology. 2009;116(8):1455–1460. | ||
Mojzis P, Kukuckova L, Majerova K, Liehneova K, Piñero DP. Comparative analysis of the visual performance after cataract surgery with implantation of a bifocal or trifocal diffractive IOL. J Refract Surg. 2014;30(10):666–672. | ||
Mojzis P, Peña-García P, Liehneova I, Ziak P, Alió JL. Outcomes of a new diffractive trifocal intraocular lens. J Cataract Refract Surg. 2014;40(1):60–69. | ||
Alió JL, Montalbán R, Peña-García P, Soria FA, Vega-Estrada A. Visual outcomes of a trifocal aspheric diffractive intraocular lens with microincision cataract surgery. J Refract Surg. 2013;29(11):756–761. | ||
Chang JS, Ng JC, Lau SY. Visual outcomes and patient satisfaction after presbyopic lens exchange with a diffractive multifocal intraocular lens. J Refract Surg. 2012;28(7):468–474. | ||
Zheleznyak L, Kim MJ, MacRae S, Yoon G. Impact of corneal aberrations on through-focus image quality of presbyopia-correcting intraocular lenses using an adaptive optics bench system. J Cataract Refract Surg. 2012;38(10):1724–1733. | ||
Braga-Mele R, Chang D, Dewey S, et al; ASCRS Cataract Clinical Committee. Multifocal intraocular lenses: relative indications and contraindications for implantation. J Cataract Refract Surg. 2014;40(2):313–322. | ||
Woodward MA, Randleman JB, Stulting RD. Dissatisfaction after multifocal intraocular lens implantation. J Cataract Refract Surg. 2009;35(6):992–997. | ||
Alió JL, Amparo F, Ortiz D, Moreno L. Corneal multifocality with excimer laser for presbyopia correction. Curr Opin Ophthalmol. 2009;20(4):264–271. | ||
Cosar CB, Sener AB. Supracor hyperopia and presbyopia correction: 6-month results. Eur J Ophthalmol. 2014;24(3):325–329. | ||
Ryan A, O’Keefe M. Corneal approach to hyperopic presbyopia treatment: six-month outcomes of a new multifocal excimer laser in situ keratomileusis procedure. J Cataract Refract Surg. 2013;39(8): 1226–1233. | ||
Alió JL, Chaubard JJ, Caliz A, Sala E, Patel S. Correction of presbyopia by technovision central multifocal LASIK (presbyLASIK). J Refract Surg. 2006;22(5):453–460. | ||
Jackson WB, Tuan KM, Mintsioulis G. Aspheric wavefront-guided LASIK to treat hyperopic presbyopia: 12-month results with the VISX platform. J Refract Surg. 2011;27(7):519–529. | ||
Reinstein DZ, Carp GI, Archer TJ, Gobbe M. LASIK for presbyopia correction in emmetropic patients using aspheric ablation profiles and a micro-monovision protocol with the Carl Zeiss Meditec MEL 80 and VisuMax. J Refract Surg. 2012;28(8):531–541. | ||
Gordon M. Presbyopia corrections with the WaveLight ALLEGRETTO: 3-month results. J Refract Surg. 2010;26(10):S824–S826. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.