Back to Journals » Patient Preference and Adherence » Volume 12
Feasibility and willingness to pay for dengue vaccine in the threat of dengue fever outbreaks in Vietnam
Authors Nguyen LH , Tran BX, Do CD, Hoang CL, Nguyen TP, Dang TT, Thu Vu G, Tran TT , Latkin CA , Ho CS , Ho RCM
Received 27 June 2018
Accepted for publication 26 July 2018
Published 26 September 2018 Volume 2018:12 Pages 1917—1926
DOI https://doi.org/10.2147/PPA.S178444
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Long Hoang Nguyen,1 Bach Xuan Tran,2–4 Cuong Duy Do,5 Chi Linh Hoang,6 Thao Phuong Nguyen,2 Trang Thi Dang,2 Giang Thu Vu,7 Tung Thanh Tran,7 Carl A Latkin,3 Cyrus S Ho,8 Roger CM Ho9
1Department of Public Health Sciences, Karolinska Institutet, Stockholm, Sweden; 2Institute for Preventive Medicine and Public Health, Hanoi Medical University, Hanoi, Vietnam; 3Department of Health, Behavior, and Society, Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD, USA; 4Vietnam Young Physician Association, Hanoi, Vietnam; 5Department of Infectious Diseases, Bach Mai Hospital, Hanoi, Vietnam; 6Center of Excellence in Behavioral Medicine, Nguyen Tat Thanh University, Ho Chi Minh city, Vietnam; 7Institute for Global Health Innovations, Duy Tan University, Da Nang, Vietnam; 8Department of Psychological Medicine, National University Hospital, Singapore, Singapore; 9Department of Psychological Medicine, Yong Loo Lin School of Medicine, National University of Singapore, Singapore
Background: The escalation of dengue fever (DF) cases in recent years and the occurrence of a large-scale DF outbreak in 2017 underline the importance of dengue vaccines in Vietnam. Given the potential benefits of the dengue vaccines and the need for copayment by the private sector, this study aims to evaluate the willingness to pay (WTP) for the dengue vaccines in patients with DF in Northern Vietnam.
Methods: A cross-sectional study was conducted on 330 in-and-out patients with DF admitted to the Bach Mai Hospital. We used the contingent valuation method to evaluate the WTP for dengue vaccines. Socioeconomic and clinical characteristics were also investigated. Multivariate interval and logistic regression models were used to estimate the average amount of WTP and identify the factors associated with the WTP.
Results: Around 77.3% patients were willing to pay an average amount of US$ 67.4 (95% CI=57.4–77.4) for the vaccine. People of higher ages, those having health insurance, those traveling in the past 15 days or suffering from anxiety/depression were less likely to be willing to pay for the dengue vaccine. However, people having a longer duration of DF or having problems with mobility were positively associated with WTP for the dengue vaccine. Patients educated to more than high school levels (Coeff.=31.31; 95% CI=3.26–59.35), those in the richest quintile (Coeff.=62.76; 95% CI=25.40; 100.13), or those having a longer duration of the disease (Coeff.=6.18; 95% CI=0.72–11.63) were willing to pay a higher amount.
Conclusion: This study highlights a relatively high rate and amount of WTP for the dengue vaccine among patients with DF. Psychological counseling services as well as educational campaigns should be undertaken to improve the WTP for the vaccine. Moreover, government subsidies should be given to increase the coverage of the vaccine in the future, especially for the poor.
Keywords: dengue, vaccine, willingness to pay, contingent valuation, Vietnam
Introduction
Dengue fever (DF) is one of the most common vector-borne infections causing great social and economic burdens globally.1 Annually, more than 390 million cases are infected, and 4 billion people live in epidemic and endemic regions, particularly in tropical and subtropical countries.2,3 The South-East Asia region has the highest incidence rate with more than 34.3 cases per 1,000 residents yearly,1 and this rate continues to increase significantly over time due to climate change, urbanization and development of trade and travel across nations.4 In addition, more than US$ 8.9 billion is spent every year on DF-related mortality and morbidity in the world.5 Currently, no effective treatment for this infectious disease is available.6,7 Efforts to control this illness primarily concentrate on personal and environmental strategies such as using bed-net, insecticides or cleaning water storage containers.1,5 However, these interventions are less effective in controlling and managing this infection.1 Therefore, the development of dengue vaccines is an advanced strategy to alleviate dengue-related burden.8,9
In recent years, diverse dengue vaccines have been developed and tested in clinical trials.8 However, one obstacle in developing an effective vaccine is that it should prevent transmission from all 4 serotypes of dengue virus.10 Therefore, to date, only tetravalent chimeric vaccine (CYD-TDV) has been approved for the prevention of dengue infection among people aged 9 years or older in Mexico (in 2015), and then in some South-East Asian and Latin America countries.7,11 This vaccine underwent two Phase III trials in more than 35,000 children aged 2–16 years. The results indicated that the efficacy of the vaccine against serotypes 3 and 4 was superior to serotypes 1 and 2, and the efficacy was relied dependent on age at immunization and history of DF.12 The manufacturer (Sanofi Pasteur) suggested three doses every six months to achieve optimal preventive effect.11 Five other dengue vaccines are being developed, of which two candidates (produced by NIH/Butantan and Takeda) are in Phase III trials.12 With such difficulties faced in developing the vaccines it will take a long time to include a new dengue vaccine in a national immunization program at an affordable price.13,14
Vietnam is among the tropical countries with the highest burden of dengue. The DF endemic, characterized by annual seasonal peaks and outbreaks, occurred every 4–10 years (1983, 1987, 1998, 2009 and 2017).15 In the 1998 outbreak, ~240,000 cases were reported with 377 deaths; and in the 2009–2010 epidemic, more than 230,000 cases were infected (142 deaths).15,16 In 1999, a National Dengue Control Program was established to implement DF control activities, primarily focusing on controlling the vector–human transmission.17 However, despite significant efforts, in 2017, Vietnam again suffered a large-scale outbreak from July to December with more than 184,000 people infected (32 fatal cases).18,19 Climate change was supposed to greatly contribute to the occurrence of the outbreaks since they coincided with the increased activity of El Nino and La Nina phenomenon.15 Thus, the dengue vaccine has been proposed as a favorable approach and is being prioritized in the national DF control strategies.20,21 Coudeville and Garnett in their mathematical models indicated that if the vaccine had 30-year protection, the coverage would be about 70%, and if the growth rate of the population were stable, the incidence rate of DF in Vietnam would decrease to 57%.22 To date, only the efficacy of the CYD-TDV vaccine was tested in Vietnam and it showed preliminary benefits in reducing dengue-related hospitalizations as well as having highly protective effects.23,24 These results show a potential application of dengue vaccine in Vietnam although this vaccine should be evaluated more for social and economic impact.25
Nonetheless, to implement a new vaccine successfully, the Vietnam Government should consider public acceptance as public distrust of immunizations has been increasing in recent years.26 Moreover, the availability of financial resources for distributing the new vaccine on a large-scale is also a great challenge. Lee et al estimated that to achieve an optimal coverage 1 million to 2.6 million doses would be required for routine vaccination of 9 year-old children in the first year of implementation and an additional 8–18 million doses for people aged 10–17 years for a one-off catch-up campaign.27 Thus, it is not feasible for the government to provide this vast amount of vaccine thus necessitating the need of copayment by the private sector. Studies in other countries such as Thailand, Colombia, Philippines and Brazil found that a high percentage of people were willing to pay for the vaccine, with the average amount ranging from US$ 20 to US$ 69.8.6,7,28,29 In Vietnam, there has been only one study in Nha Trang, investigating the willingness to pay (WTP) for the vaccine, which revealed that people were willing to pay US$ 26.1 for a three-dose regime.6 More evidence about public acceptance and WTP are essential to evaluate the feasibility of the implementation of the vaccine, particularly among patients with DF. These patients may have an antibody-dependent enhancement after infection with dengue virus; however, they are expected to have a better perception of prevention of dengue transmission,30 that makes them potential consumers of the dengue vaccine, not only for themselves but also for their families. Therefore, this study aims to understand the WTP for the dengue vaccine, in patients with DF in the 2017 DF outbreak in Hanoi, Vietnam.
Methods
Study design
A hospital-based survey was performed at the Department of Infectious Diseases, Bach Mai hospital in Hanoi, Vietnam from July to November 2017. During the dengue outbreak, there were around 50–70 patients with DF hospitalized every day at the department.31 Patients were invited to the study if they: 1) used any services (inpatient or outpatient) at the department; 2) had DF symptoms; 3) had confirmed positive results for dengue virus (via NS1 Ag/IgM/IgG rapid test); 4) did not have any severe cognitive impairment and thus unable to respond to the questionnaire and 5) agreed to enroll in the survey and gave their written informed consent. Expecting that 50% of patients would be willing to pay for the dengue vaccine, level of CI=95%, and margin of error=0.11 (relative precision), we computed that a minimum of 318 patients were required for the study. We added 5% of total sample size to compensate for people who did not complete the questionnaire. A total number of 334 patients were enrolled in the survey using the convenience sampling technique, and the data of 330 patients were used for data analysis (98.8%).
Contingent valuation (CV) method
We applied the CV method to evaluate the WTP for dengue vaccination in patients with DF. This method allowed us to measure the WTP as well as the amount of WTP for a hypothetical product, ie, three doses of dengue vaccine, in customers. First, we presented all necessary information about: 1) the dengue epidemic in Vietnam; 2) the characteristics of the disease; 3) the available interventions and treatments for the disease and 4) the potential benefits of dengue vaccine (efficacy of vaccines and protective effect if scaling up the vaccine to a wider community). Awareness of the product was vital for patients to accurately estimate their WTP for the product.32,33
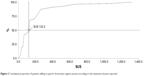
Then, we asked a series of questions, the so-called double-bounded dichotomous choice questions, followed by open-ended questions to assess the WTP. Patients were asked several “Yes/No” questions about their WTP for a certain amount. For instance, the first question would be “Suppose that the dengue vaccine costs US$ 66.1 for three doses for one person, would you be willing to pay for this product?” Then, if they said “Yes,” the next price would be double, and halved if they said “No.” Finally, a final question about the maximum amount of WTP that they were willing to pay for the dengue vaccine was asked. The bidding process is detailed in Figure 1.
  | Figure 1 The Bidding process (Unit: US$). |
Data collection
A structured questionnaire was administered via face-to-face interviews. Each interview lasted 15 minutes. This questionnaire was piloted in a small sample to test its validity and reliability. It was revised to correct for any misunderstood texts and questions. The data collection team included well-trained medical students at the Hanoi Medical University.
This questionnaire consisted of four parts: 1) sociodemographic characteristics (age, gender, occupation, education, marital status, income and health insurance status); 2) epidemiology characteristics (duration of infection, level of severity, types of service, whether neighborhood/relatives suffered DF, comorbidities, travel history and mosquito density at home); 3) health status; 4) awareness of and attitude toward the dengue vaccine and 5) CV questions for the dengue vaccine. Health status was measured using EuroQol-5 dimensions-5 levels tools, which evaluated patients’ health in five domains: mobility, self-care, usual activities, pain/discomfort and anxiety/depression with five levels of response from no problem to extreme problem.37
Statistical analysis
Statistical significance was identified if the P-value was less than 0.05. Characteristics of respondents were described and compared regarding the WTP for dengue vaccine using Chi-squared and Mann–Whitney tests. The mean amount of WTP was estimated using interval regression. Multivariate logistic and interval regressions were used to identify potential predictors of WTP and the amount of WTP for dengue vaccine. These models were combined with stepwise backward strategies to construct reduced models (excluding variables if their P-value of log likelihood test was higher than 0.2).
Ethical consideration
The study protocol was approved by the Institution Review Board of Hanoi Medical University.
Result
Table 1 shows that among 330 patients, the mean age was 31.6 (SD=12.7) years. The majority of respondents were male (52.1%), living in urban areas (77.9%), having more than high school education (51.5%) and married (52.8%), having health insurance (64.6%) followed by freelancers (25.8%). There were 77.3% willing to pay for the vaccine. Only difference in occupation was found significant between patients who were willing and not willing to pay (P<0.05).
  | Table 1 Sociodemographic characteristics of participants |
Table 2 presents the WTP for the dengue vaccine according to the epidemiological characteristics of patients. The average duration of DF was 5.5 days (SD=4.3). Most of the respondents had symptomatic DF (68.5%) and used the outpatient service (55.3%). There were 43.1% and 19.0% patients having neighborhoods and relatives with DF, respectively. More than one-third (34.2%) of patients had comorbidities. Only 14.3% and 6.8% of our sample traveled or had relatives traveling to other locales in the past 15 days, correspondingly. No differences were found between willingness and not willingness to pay for the dengue vaccine for the epidemiological characteristics.
  | Table 2 Epidemiological characteristics |
About 85.0% patients wanted to vaccinate their family members. Only 19.8% knew of any dengue vaccines and 92.8% perceived the necessity of dengue vaccine. The percentage of people willing to pay for the dengue vaccine decreased with the levels of necessity (P<0.01) (Table 3).
  | Table 3 Awareness and Attitude toward dengue vaccine |
Figure 2 reveals that 77.3% of patients were willing to pay US$ 67.4 (95% CI=57.4–77.4) for the three-dose regime of the vaccine or US$ 22.5 per dose. People who were males, having less than a high school education, singles, unemployed and living in rural areas were willing to pay less than others.
Figure 3 reveals that among 77.3% patients willing to pay for the vaccine, 42.5% of patients reported that their maximum amount of WTP equaled or was less than US$ 66.1/three doses – equal to the starting bid. The median of the maximum amount of WTP was US$ 132.2/three doses or US$ 44.1 per dose, which means that among those being willing to pay, 50% of patients were willing to pay for this amount or less.
  | Figure 3 Cumulative proportion of patients willing to pay for three-dose regime vaccine according to the maximum amount reported. |
Table 4 shows that people with higher age (OR=0.94; 95% CI=0.89; 0.99), having health insurance (OR=0.34; 95% CI=0.12; 0.95), who had travelled in the past 15 days (OR=0.14; 95% CI=0.03–0.70) or suffering from anxiety/depression (OR=0.13; 95% CI=0.03–0.55) were less likely to be willing to pay for dengue vaccine. Meanwhile, having higher a duration of the disease or having problems with mobility were positively associated with the WTP for dengue vaccine. In terms of the amount of WTP, patients having high school education (Coeff.=31.31; 95% CI=3.26–59.35), being in the richest quintile (Coeff.=62.76; 95% CI=25.40; 100.13) or having a higher duration of the disease (Coeff.=6.18; 95% CI=0.72–11.63), were willing to pay higher compared to the reference group. Meanwhile, suffering problems in usual activities was negatively associated with the amount of WTP (Coeff.= −31.18; 95% CI= −61.09; −1.28).
  | Table 4 Several factors are associated with willingness to pay for dengue vaccination services |
Discussion
This study offered insights into the WTP for the dengue vaccine among patients with DF in the outbreak in Vietnam. In this study, we found a high acceptance rate as well as high amount of WTP for the vaccine, implying the feasibility of the implementation of the dengue vaccine in Vietnam. Our regression models also found some potential factors associated with WTP in terms of socioeconomic and epidemiological characteristics, which might contribute to some implications to improve the WTP of people for the dengue vaccine.
Our findings indicated that a relatively high fraction of our sample were willing to pay for the dengue vaccine (77.3%). This was similar to recent community-based studies in Aceh, Indonesia (77.3%)38 and Philippines (75%);29 and lower than that of previous studies in Bandung, Indonesia (94.6%)13 and Colombia (88.6%).35 Notably, most of these studies used hypothetical scenarios to evaluate the WTP for dengue vaccine. The differences could be explained by several reasons. First, we conducted this study in clinical settings while all of previous studies were performed in community settings. Second, in Vietnam, to date, no type of dengue vaccine is available; therefore, when there were no official reports about the efficacy of this vaccine from Vietnam authorities, our patients might not believe in the hypothetical dengue vaccine in the CV scenario. Thus, the WTP for this vaccine would be different if the actual dengue vaccine were available in the market. In addition, all of them were patients with DF, resulting in the opinion that they would have antibody-dependent enhancement, or in other words, they did not need to be vaccinated to prevent this disease. Finally, since the public confidence on vaccination has been decreased due to several adverse events in previous years, we observed that our patients expressed their fears about vaccination, leading to their unwillingness to pay for the vaccine. Notably, although more than 90% of patients perceived the necessity of the vaccine, 15.0% of patients refused to vaccinate their family’ members even if the vaccine was assumed to be provided free of cost. This result was significantly higher than that in Brazil, Indonesia, Thailand and Colombia,7,34 necessitating the need for educational campaigns to promote dengue vaccination in the future.
Among people being willing to pay for the vaccine, the mean amount of WTP was US$ 67.4 for a three-dose regime or US$ 22.5 per dose. This amount was in the cost interval that was revealed in prior community surveys such as in Nha Trang, Vietnam (US$ 26.1 for three doses), Thailand (US$ 69.8), Colombia (US$ 20–22.6),6,28 and Brazil (US$ 33.6 for three doses)7 and was consistent to the finding in Philippines (US$ 27.1–32.3 per dose).29 We supposed that people were willing to pay this high amount because our study was conducted during the outbreak of dengue. Our finding was much higher than that in two community-based studies in Indonesia (US$ 1.94 per dose13 or US$ 4 for a dengue vaccine).39 It should be noted that the study in Indonesia was conducted to investigate the WTP for pediatric dengue vaccines, which the Indonesian Government would want to use in the national immunization program.21 Therefore, the price used for the WTP approach in the Indonesian study equaled the production cost (~ US$ 0.2 per dose if the quantity of doses produced were 60 million per year).40 However, literatures have highlighted that a significant effort would be required to bring the cost of a new vaccine to an affordable level for developing countries (more than 20 years in the case of hepatitis B).13,14
In this study, we found associations of age, education and income with WTP and amount of WTP, which were similar to previous studies.6,13,28,38 As more than 50% of our patients were willing to pay less than US$ 132.2 for a three-dose scheme, and wealthier patients were willing to pay more for the dengue vaccine, it suggests an establishment of a private market for the dengue vaccine in the near future, as well as a threshold where sales would be robust.28 Nonetheless, a high price of the dengue vaccine would be a great barrier to increasing coverage as social insurance schemes in Vietnam do not cover vaccination services. Clearly, government subsidies or financial aid as well as efforts to include the dengue vaccine into the national Expanded Programme on Immunization should be considered, particularly for the poor people, who have a higher likelihood of being affected by DF.41
Mobility impairment and higher duration of DF were found to be associated with the WTP. These findings were consistent with the previous literature since people having illnesses were more likely to accept and be willing to pay for preventive services against this diseases.38,42–44 Meanwhile, those suffering anxiety/depression had a lower likelihood of being willing to pay for the vaccine. These patients were more likely to develop pessimism and thus, had a negative viewpoint of the preventive measures and were less likely to be willing to pay for the vaccine.45 Notably, we did not find any relationships between awareness of and attitude toward the dengue vaccine and the WTP for the vaccine. Previous studies in Indonesia, Philippines and Vietnam indicated significant associations between the knowledge of preventive methods against dengue with WTP.6,29,38 The difference might be probably because of the homogeneous nature of our sample. Moreover, people who had traveled to other locales in the past 15 days were less likely to be willing to pay for the dengue vaccine. Literature indicated that travel was a critical factor in transmitting the dengue virus from endemic to non-endemic settings.46,47 This result suggested an emerging problem among travelers, requiring educational campaigns to improve their awareness about the usefulness of the vaccine in preventing dengue infection not only for them but also for their community.
The findings of this study would be used to propose several implications. First, appropriate counseling services should be provided to patients with DF helping them increase their psychological health, thus increasing their likelihood of willingness to pay. Second, educational campaigns should be implemented carried out to improve people’s awareness and attitude toward the dengue vaccine, particularly among travelers, resulting in acceptance and WTP of the community for the vaccine. Third, the findings of this study could be used by policy makers in economic evaluations to have appropriate resource allocation strategies for the introduction of the dengue vaccine. In addition, the understanding of the contextual factors is important in designing vaccination programs as well as marketing strategies in the future. Moreover, this study will give the authorities and vaccine manufactures knowledge of people’s perception of dengue vaccines in a dengue outbreak.
Several limitations should be acknowledged. First, our scenarios did not mention any specific vaccines. However, because this study aimed at exploring the demand of people for vaccines, this is an appropriate approach since no dengue vaccine is officially available in Vietnam.28 Second, a social desirability bias possibly occurred when patients tended to respond to favorable options. Third, a cross-sectional design used in the study limited the possibility of drawing causal relations between WTP and its determinants. Finally, a convenience sampling approach was used in this study, decreasing the generalizability of our results.
Conclusion
In conclusion, this study emphasized a relatively high rate and amount of WTP for the dengue vaccine among patients with DF. Psychological counseling services as well as educational campaigns should be implemented to improve the WTP for the vaccine. Moreover, government subsidies should be given to increase the coverage of the vaccine in future, especially for the poor.
Disclosure
The authors report no conflicts of interest in this work.
References
Stanaway JD, Shepard DS, Undurraga EA, et al. The global burden of dengue: an analysis from the Global Burden of Disease Study 2013. Lancet Infect Dis. 2016;16(6):712–723. | ||
Bhatt S, Gething PW, Brady OJ, et al. The global distribution and burden of dengue. Nature. 2013;496(7446):504–507. | ||
Singhi S, Kissoon N, Bansal A. Dengue and dengue hemorrhagic fever: management issues in an intensive care unit. J Pediatr. 2007;83(Suppl 2):S22–S35. | ||
Ooi EE, Gubler DJ. Dengue in Southeast Asia: epidemiological characteristics and strategic challenges in disease prevention. Cad Saude Publica. 2009;25(Suppl 1):S115–S124. | ||
Shepard DS, Undurraga EA, Halasa YA, Stanaway JD. The global economic burden of dengue: a systematic analysis. Lancet Infect Dis. 2016;16(8):935–941. | ||
Lee JS, Mogasale V, Lim JK, et al. A multi-country study of the household willingness-to-pay for dengue vaccines: household surveys in Vietnam, Thailand, and Colombia. PLoS Negl Trop Dis. 2015;9(6):e0003810. | ||
Godói IP, Santos AS, Reis EA, et al. Consumer Willingness to Pay for Dengue Vaccine (CYD-TDV, Dengvaxia®) in Brazil; Implications for Future Pricing Considerations. Front Pharmacol. 2017;8:41. | ||
Webster DP, Farrar J, Rowland-Jones S. Progress towards a dengue vaccine. Lancet Infect Dis. 2009;9(11):678–687. | ||
Durbin AP, Whitehead SS. Next-generation dengue vaccines: novel strategies currently under development. Viruses. 2011;3(10):1800–1814. | ||
Schwartz LM, Halloran ME, Durbin AP, Longini IM. The dengue vaccine pipeline: Implications for the future of dengue control. Vaccine. 2015;33(29):3293–3298. | ||
Dengue vaccine: WHO position paper – July 2016. Wkly Epidemiol Rec. 2016;91(30):349–364. | ||
WHO. Immunization, Vaccines and Biologicals – Dengue vaccine research; 2017. Available from: http://www.who.int/immunization/research/development/dengue_vaccines/en/. Accessed July 23, 2018. | ||
Hadisoemarto PF, Castro MC. Public acceptance and willingness-to-pay for a future dengue vaccine: a community-based survey in Bandung, Indonesia. PLoS Negl Trop Dis. 2013;7(9):e2427. | ||
Frost LJ, Reich MR. Hepatitis B vaccine: access to vaccine. In: Frost LJ, Reich MR, editors. Access: How Do Good Health Technologies Get to Poor People in Poor Countries? Cambridge: Harvard Center for Population and Development Studies; 2008:67–90. | ||
Minh An DT, Rocklöv J. Epidemiology of dengue fever in Hanoi from 2002 to 2010 and its meteorological determinants. Glob Health Action. 2014;7(1):23074. | ||
Arima Y, Matsui T. Epidemiologic update of dengue in the Western Pacific Region, 2010. Western Pac Surveill Response J. 2011;2(2):e1–e8. | ||
Lee HS, Nguyen-Viet H, Nam VS, et al. Seasonal patterns of dengue fever and associated climate factors in 4 provinces in Vietnam from 1994 to 2013. BMC Infect Dis. 2017;17(1):218. | ||
Minh An DT, Rocklöv J. Epidemiology of dengue fever in Hanoi from 2002 to 2010 and its meteorological determinants. Glob Health Action. 2014;7:23074. | ||
World Health Organization Western Pacific Region. Dengue Situation Update Number 533: Update on the Dengue situation in the Western Pacific Region. Manila: World Health Organization Western Pacific Region; 2018. | ||
Prime Minister. Decision No. 122/QD-TTg approving the national strategy to protech, care, and improve public health during 2011–2020, and the orientation towards 2030. Hanoi: 2013. Available from: http://www.chinhphu.vn/portal/page/portal/chinhphu/hethongvanban?class_id=2&mode=detail&document_id=165437. Accessed May 7, 2018. | ||
Deroeck D, Deen J, Clemens JD. Policymakers’ views on dengue fever/dengue haemorrhagic fever and the need for dengue vaccines in four southeast Asian countries. Vaccine. 2003;22(1):121–129. | ||
Coudeville L, Garnett GP. Transmission Dynamics of the Four Dengue Serotypes in Southern Vietnam and the Potential Impact of Vaccination. PLoS One. 2012;7(12):e51244. | ||
Arredondo-García JL, Hadinegoro SR, Reynales H, et al. Four-year safety follow-up of the tetravalent dengue vaccine efficacy randomized controlled trials in Asia and Latin America. Clin Microbiol Infect. 2018;24(7):755–763. | ||
Capeding MR, Tran NH, Hadinegoro SR, et al. Clinical efficacy and safety of a novel tetravalent dengue vaccine in healthy children in Asia: a phase 3, randomised, observer-masked, placebo-controlled trial. Lancet. 2014;384(9951):1358–1365. | ||
Lee JS, Lourenço J, Gupta S, Farlow A. A multi-country study of dengue vaccination strategies with Dengvaxia and a future vaccine candidate in three dengue-endemic countries: Vietnam, Thailand, and Colombia. Vaccine. 2018;36(17):2346–2355. | ||
Li X, Wiesen E, Diorditsa S, et al. Impact of Adverse Events Following Immunization in Viet Nam in 2013 on chronic hepatitis B infection. Vaccine. 2016;34(6):869–873. | ||
Lee JS, Lim JK, Dang DA, Nguyen THA, Farlow A. Dengue vaccine supplies under endemic and epidemic conditions in three dengue-endemic countries: Colombia, Thailand, and Vietnam. Vaccine. 2017;35(50):6957–6966. | ||
Bracho-Churio YT, Martínez-Vega RA, Rodriguez-Morales AJ, Díaz-Quijano RG, Luna-González ML, Diaz-Quijano FA. Determinants of felt demand for dengue vaccines in the North Caribbean region of Colombia. Ann Clin Microbiol Antimicrob. 2017;16(1):38. | ||
Palanca-Tan R. The demand for a dengue vaccine: a contingent valuation survey in Metro Manila. Vaccine. 2008;26(7):914–923. | ||
Wong LP, AbuBakar S, Chinna K. Community knowledge, health beliefs, practices and experiences related to dengue fever and its association with IgG seropositivity. PLoS Negl. Trop. Dis. 20148(5):e2789. | ||
MoH Portal. Medical News Point. Available from: http://www.moh.gov.vn/news/Pages/TinHoatDongV2.aspx?ItemId=2397. Accessed January 1, 2018. | ||
Nguyen LH, Tran BX, Nguyen NP, Phan HT, Bui TT, Latkin CA. Mobilization for HIV voluntary counseling and testing services in Vietnam: clients’ risk behaviors, attitudes and willingness to pay. AIDS Behav. 2015. | ||
Tran BX, Nguyen NK, Nguyen LP, Nguyen CT, Nong VM, Nguyen LH. Preference and willingness to pay for traditional medicine services in rural ethnic minority community in Vietnam. BMC Complement Altern Med. 2016;16(1):48. | ||
Lee JS, Mogasale V, Lim JK, et al. A multi-country study of the household willingness-to-pay for dengue vaccines: household surveys in Vietnam, Thailand, and Colombia. PLoS Negl Trop Dis. 2015;9(6):e0003810. | ||
Bracho-Churio YT, Martínez-Vega RA, Rodriguez-Morales AJ, Díaz-Quijano RG, Luna-González ML, Diaz-Quijano FA. Determinants of felt demand for dengue vaccines in the North Caribbean region of Colombia. Ann Clin Microbiol Antimicrob. 2017;16(1):38. | ||
Fajar JK, Harapan H. Socioeconomic and attitudinal variables associated with acceptance and willingness to pay towards dengue vaccine: a systematic review. Arch Clin Infect Dis. 2017;12(3):e13914. | ||
EuroQol Group. EQ-5D-5L User Guide. Basic information on how to use the EQ-5D-5L instrument; 2011. Available from: https://euroqol.org/wp-content/uploads/2016/09/EQ-5D-5L_UserGuide_2015.pdf. Accessed September 1, 2013. | ||
Harapan H, Anwar S, Setiawan AM, Sasmono RT, Aceh Dengue Study. Dengue vaccine acceptance and associated factors in Indonesia: a community-based cross-sectional survey in Aceh. Vaccine. 2016;34(32):3670–3675. | ||
Harapan H, Anwar S, Bustamam A, et al. Willingness to pay for a dengue vaccine and its associated determinants in Indonesia: a community-based, cross-sectional survey in Aceh. Acta Trop. 2017;166:249–256. | ||
Mahoney RT, Francis DP, Frazatti-Gallina NM, et al. Cost of production of live attenuated dengue vaccines: a case study of the Instituto Butantan, Sao Paulo, Brazil. Vaccine. 2012;30(32):4892–4896. | ||
Mulligan K, Dixon J, Sinn CL, Elliott SJ. Is dengue a disease of poverty? A systematic review. Pathog Glob Health. 2015;109(1):10–18. | ||
Kesztyüs D, Lauer R, Schreiber AC, Kesztyüs T, Kilian R, Steinacker JM. Parents’ willingness to pay for the prevention of childhood overweight and obesity. Health Econ Rev. 2014;4(1):20. | ||
Yasunaga H, Ide H, Imamura T, Ohe K. Willingness to pay for health care services in common cold, retinal detachment, and myocardiac infarction: an internet survey in Japan. BMC Health Serv Res. 2006;6:12. | ||
Hammitt JK, Graham JD. Willingness to pay for health protection: inadequate sensitivity to probability? J Risk Uncertain. 1999;18(1):33–62. | ||
Nguyen QL, Nguyen LH, Tran BX, et al. Co-financing for viral load monitoring during the course of antiretroviral therapy among patients with HIV/AIDS in Vietnam: a contingent valuation survey. PLoS One. 2017;12(2):e0172050. | ||
Wilder-Smith A. Dengue infections in travellers. Paediatr Int Child Health. 2012;32 Suppl 1(s1):28–32. | ||
Verma S, Kanga A, Singh D, et al. Emergence of travel: associated dengue fever in a non-endemic, hilly state. Adv Biomed Res. 2014;3:239. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

