Back to Journals » Clinical Interventions in Aging » Volume 9
Feasibility and efficacy of cognitive telerehabilitation in early Alzheimer’s disease: a pilot study
Authors Jelcic N, Agostini M, Meneghello F, Bussè C, Parise S, Galano A, Tonin P, Dam M, Cagnin A
Received 21 May 2014
Accepted for publication 16 July 2014
Published 24 September 2014 Volume 2014:9 Pages 1605—1611
DOI https://doi.org/10.2147/CIA.S68145
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Nela Jelcic,1 Michela Agostini,1 Francesca Meneghello,1 Cinzia Bussè,2 Sara Parise,2 Antonietta Galano,2 Paolo Tonin,1 Mauro Dam,1 Annachiara Cagnin1,2
1Foundation IRCCS San Camillo Hospital, Laboratory of Kinematics and Robotics and Laboratory of Psychology, Neurorehabilitation Department, Venice, Italy; 2Department of Neurosciences: Sciences NPSRR, University of Padova, Padova, Italy
Background: This pilot study compared the effects of lexical-semantic stimulation through telecommunication technology (LSS-tele) with in-person LSS (LSS-direct) and unstructured cognitive treatment (UCS) in patients with early Alzheimer’s disease.
Methods: Twenty-seven patients with Alzheimer’s disease in the very early stage (Mini-Mental State Examination [MMSE] >26/30) were divided into three groups: seven patients received LSS-tele treatment, ten received standard LSS-direct intervention, and ten participants underwent UCS as control condition. Intervention treatments consisted of two weekly sessions of LSS (through teleconference or face to face depending on group assignment) or UCS exercises administered to small groups throughout a 3-month period. The main outcome measures were changes of global cognitive performance, language abilities, and memory function. Secondary outcome measures were changes in attention, working memory, executive functions, and visual-spatial abilities tests.
Results: The mean MMSE score improved significantly in LSS-tele and LSS-direct treatments; LSS-tele improved language abilities, both phonemic and semantic, and stabilized delayed verbal episodic memory with respect to an improved performance after the LSS-direct intervention and to a memory decline observed in the control group. Improvement was not achieved in any neuropsychological test score after UCS.
Conclusion: Clinical application of telecommunication technology to cognitive rehabilitation of elderly patients with neurodegenerative cognitive impairment is feasible and may improve global cognitive performance. Technical aspects to ameliorate efficacy of delivery may further improve its impact on domain-specific cognitive abilities.
Keywords: cognitive rehabilitation, telecommunication, telemedicine
Introduction
In the last 10 years the role of telemedicine has been widely expanded. The use of information and communication technologies for the delivery of several health services, ie, telerehabilitation (TR), to patients living at their own homes from a remote provider has been encouraged by many national health systems worldwide.1 TR represents the opportunity to convey rehabilitative interventions at distance to subjects experiencing disabilities of multiple functions due to a wide variety of injuries. The added value of TR relies on the concrete possibility to supply effective rehabilitation care to subjects at home and avoiding the displacement of therapist or patient, which may be difficult in remote communities, in conditions characterized by limited access to health services or for patients with limited functional dependence.1,2
Recent reviews highlighted that poststroke patients early discharged at home and receiving specific rehabilitation treatments in the familiar environment experienced less mortality and dependence than those undergoing conventional care, and they obtained earlier reintegration and better quality of life.3–5 More recently, a few randomized studies demonstrated that motor rehabilitation treatments delivered via TR achieved similar results as standard rehabilitation care in poststroke patients.6–8 Meanwhile, high levels of satisfaction with all aspects of TR of brain injuries have been reported.9,10
Motor rehabilitation represents the major topic studied using TR. Nevertheless, other rehabilitation specialties are emerging, with promising results of efficacy, such as treatment of speech-language disorders and cognitive impairment.11 In the field of acquired speech and language disorders, some studies showed comparable results of remote assessment and treatment when compared with conventional face to face procedures.12 The main areas of assessment and treatment were articulation disturbances,13 aphasia,14 and lexical retrieval.15,16
The feasibility to perform cognitive assessments via telemedicine in elderly subjects with dementia has been recently investigated.17–19 However, to date very few studies have been performed aiming at assessing the feasibility and efficacy of cognitive TR in patients affected by neurodegenerative dementia such as Alzheimer’s disease (AD).11,20
AD is the most common neurodegenerative dementia in the elderly and represents the most significant social, health, and economic burden of the 21st century.21 In the World Alzheimer Report 2011, it was estimated that 36 million people worldwide are affected by dementia with numbers doubling every 20 years.21 Nonpharmacological interventions such as cognitive rehabilitation are emerging as a potential approach to improve or stabilize cognitive functions in AD patients, particularly considering the limited benefit obtained with antidementia drug treatments.22–24 However, the clinical impact of generalized cognitive stimulation and specific memory training are not conclusively proven,22–24 making the use of this approach not widely applied.
A comprehensive review of cognitive stimulation treatment studies in neurodegenerative dementia, with a thorough discussion of potential and pitfalls of this intervention, has been recently published.25 A previous study from our group showed that domain-specific cognitive stimulation targeting semantic abilities could significantly improve global cognition, naming, and also episodic verbal memory in early AD with respect to unstructured cognitive enrichment training, which did not improve any cognitive domain.26 The benefit on global cognition persisted 6 months after treatment discontinuation. These results suggested that rehabilitation targeting lexical-semantic verbal function improved the efficiency of the corresponding semantically-related domains and reshaped other connected memory-related cognitive networks.
Following the encouraging results obtained from the previous face to face semantic stimulation study,26 we designed an observer-blinded, controlled pilot study of the effects of this domain-specific cognitive training, delivered through telecommunication technology to patients with early AD, and compared it with the same cognitive training delivered face to face. Outcome measures were changes of neuropsychological test scores assessing global cognition, language abilities, verbal and nonverbal related memory domains, attention and executive functions, and visual-spatial abilities.
Materials and methods
Subjects
A total of 38 participants with mild memory decline, referred to the outpatient Memory Unit of the San Camillo Hospital in Venice (Italy), were screened from July to September 2012. The hospital is located on a small island (Lido of Venice), and the patients referred to this health service are residents of this island or the neighboring islands of Venice lagoon. The baseline evaluation was performed by a multidisciplinary team consisting of a neurologist, a neuropsychologist, a speech therapist, and a social worker. All subjects referred to the memory clinic were diagnosed as being affected by cognitive impairment due to prodromal or mild neurodegenerative diseases and were followed through periodic visits to the outpatient clinic.
The inclusion criteria were diagnosis of probable AD according to the National Institute of Neurological and Communicative Disorders and Stroke–AD and Related Disorders Association criteria;27 early stage of the disease, with a Clinical Dementia Rating score ranging from 0.5 to 1; and stable psychoactive medication in the previous 3 months. Participants were not on antidementia drug therapy (cholinesterase inhibitors or memantine) for the presence of prescription contraindications (ie, heart arrhythmia, previous episodes of syncope, severity of cognitive impairment above the threshold required from the Italian health regulatory system) or no guarantee of drug assumption compliance. The exclusion criteria were presence of brain lesions, ascertained with brain imaging studies; severe systemic diseases or depression; severe behavioral symptoms, evaluated with the Neuropsychiatric Inventory28 questionnaire; and serious lexical-semantic deficits that may interfere with the rehabilitation, assessed with the verbal naming test score ≥2 standard deviations below normal values.
After applying the exclusion criteria, 27 participants met the selection criteria and entered the study. After being informed of the treatment protocol and considering individual preferences, they were randomly assigned to three treatment groups: seven patients received lexical-semantic stimulation (LSS) with a teleconference technology (LSS-tele); ten were treated with a face to face direct administration of LSS (LSS-direct), and ten control subjects underwent unstructured cognitive stimulation (UCS). The unequal distribution among the three treatment groups was due to the preference of two patients, initially enrolled in the LSS-tele group, to not be involved with computer technology and who were shifted into the other two treatment arms.
The study followed the ethical principles for medical research involving human subjects required by the Declaration of Helsinki. The study was approved by the local ethics committee, and written informed consent was obtained from each patient.
Interventions
The methodology referring to the LSS treatment has been described in a previous study,26 where it was provided face to face. In brief, the LSS protocol contained lexical tasks aimed at enhancing semantic verbal processing. The exercises focused on the interpretation of written words, sentences, and stories and were divided into eight main parts: semantic categories, syntagmatic and paradigmatic relationship, level of semantic affinity between words, adequacy of adjectives to the context of the text, part–whole relationship, recognition of nonsense sentences, identification of semantic definition, and context of a short story. Group discussion about response choices was encouraged to stimulate verbal competencies. A description of the type of exercises for each part of the LSS protocol is provided in the study by Jelcic et al.26
In the LSS-tele treatment, the same LSS exercises were delivered through remote control based on telecommunication technology. In the LSS-tele protocol, the therapist (NJ) was based at San Camillo Hospital in the island of Lido (Venice) and was connected to a group of patients placed in two elderly day care centers in the city of Venice. One trained operator (CB or AG) was based in the patients’ room with the aim to guarantee the correct access to the technologies and to facilitate the interaction with the treatment therapist, when required.
The rehabilitation protocol was provided at distance by a customized system, based on two applications run on two personal computer workstations using Windows® 7 or XP operating systems. The teleconference and communication technology was based on Skype® control for Windows application programming interface provided by Skype®, allowing the use of a stable connection regardless of router configuration. Skype® uses a 256 bit Advanced Encryption Standard to encrypt communication between users. The encryption is inherent in the Skype protocol and is transparent to callers, and the server application was installed in patients’ workstations. The application displayed two different interfaces: one specifically designed for the therapist and one designed for the patient. The therapist’s interface allowed for control of all the experimental information. The patients’ side of the interface was designed with two windows: one showing the therapist by videoconference, the other displaying the target exercise. The integrated, high-quality videoconference software allowed the remote control to tilt and zoom a network camera placed on the patient side, allowing for the visual monitoring for safety and behavioral conditions during the rehabilitation session. The technology employed for videoconferencing was the same as that used in a recently published study from our research group assessing the effects of TR in aphasia.16
Participants of the LSS-direct group received the LSS intervention by the same face to face modality, in the presence of the therapist during the entire session, as previously described.26 Participants of the UCS group were engaged in face to face exercises consisting of creative work such as practicing manual skills, stimulating fantasy and creativeness, reading the newspaper with active participation and discussion, and improving verbal communication.
The intervention protocol consisted of two weekly sessions of LSS-tele, LSS-direct, or UCS exercises, lasting 1 hour each in the morning, over a period of 3 months. All the treatments were administered to small subgroups of 3–4 participants who were based in day care centers for the elderly. Nonspecific, cognitive reinforcement by caregivers was planned in between sessions when staying at home. The same therapist (NJ) performed the LSS-tele, LSS-direct, and UCS treatments.
Outcome measures
Extensive neuropsychological assessment addressing multiple cognitive domains was given to each subject at study entry and postintervention after 3 months of treatments. Baseline and posttreatment examinations were performed in the Memory Clinic at San Camillo Hospital in Venice.
All the assessments were carried out by an experienced neuropsychologist (SP), blinded to the treatment group to which each patient was allocated. Primary outcome measures were a) global cognitive performance, assessed with the Mini-Mental State Examination (MMSE);29 b) lexical-semantic abilities, assessed with the Verbal Naming Test30 and phonemic and semantic fluency;30 and c) semantically-related and unrelated immediate and delayed episodic verbal memory, assessed respectively with Brief Story Recall31 and Rey Auditory Verbal Learning (RAVL) tests.32
Secondary outcome measures were a) working memory, assessed with the Forward Digit Span Test;30 b) visual-spatial memory, assessed with the Rey–Osterrieth Complex Figure (ROCF) Delayed Recall Test;31 c) attention and executive functions, assessed with Digit Cancellation Test30 and Trail Making Test (A and B); d) visual-spatial abilities, evaluated with the ROCF Copy Test.31
At the end of 3 months, patients of the LSS-tele group completed an ad hoc questionnaire of satisfaction, which consisted of two items addressing subjective perception of treatment efficacy and feasibility: 1) general utility and appeal of exercises and 2) valuable enough to be advisable to others. Questions were rated on a 10 point Likert scale (1= strongly disagree; 10= strongly agree).
Statistical analysis
The Kolmogorov–Smirnov method was used to test for the normality of variables such as age expressed in years. For dichotomy variables (sex) the chi-square test was employed. The Kruskal–Wallis ANOVA was used to test for between-group differences in more than two groups. When it was significant, the Mann–Whitney U-test was employed for comparisons in two groups.
The Student’s t-test was used for normally distributed variables, while for ordinal variables the Wilcoxon test was used for paired data (within-group analysis). The significance level was set at P<0.05.
Results
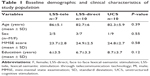
At entry into the study, the three groups were comparable for mean age, sex distribution, severity of cognitive decline, and education level (Table 1).
As illustrated in Table 2, the mean MMSE score significantly improved after both LSS-tele (P=0.03) and LSS-direct (P=0.01) treatments compared to baseline values. Moreover, looking at the individual values, each subject in these two groups showed an improvement of the MMSE score compared with the corresponding baseline value. Conversely, in the UCS group, the mean MMSE score slightly decreased compared to baseline.
Considering specific cognitive domains, language abilities were significantly improved after LSS-tele treatment (phonemic fluency: P=0.04; semantic fluency: P=0.03). For episodic memory, delayed verbal memory stabilized after LSS-tele and improved only after LSS-direct intervention, with respect to deterioration in the control group. Immediate episodic memory (story immediate recall) improved significantly only in the LSS-direct group (P=0.03).
As showed in Table 3, there was a significant change in working memory performance, ie, the Forward Digit Span mean score. The between-group comparison showed a stabilization of the working memory performance with respect to baseline values in the LSS-tele group, a small significant improvement after LSS-direct treatment, and a significant decline of the test mean score after UCS therapy. There were no differences between the groups in visual-spatial memory, as measured by means of ROCF Delayed Recall mean score. Attention abilities assessed with the Digit Cancellation Test improved significantly only in the LSS-tele group (P=0.01). No therapy-related significant modification of visual-spatial abilities (scored by means of ROCF Copy) was found.
Eighty-six percent (6/7) of the patients undergoing LSS-tele rated 10 for the satisfactory question item on general utility and appeal of exercises. One hundred percent of participants would advise the treatment to friends.
Discussion
This study compared the effects of LSS-tele, LSS-direct, and UCS interventions on specific cognitive abilities such as language, memory, attention, and visual-spatial abilities in three groups of subjects in the early stage of AD. At the end of 3 months of treatment, between-group comparisons showed that stimulation of lexical-semantic abilities through TR improved global cognitive performance and language abilities in the same manner as LSS delivered in-person, and stabilized delayed verbal episodic memory and working memory performances with respect to the control group, which showed severe memory deterioration.
However, several differences with respect to direct delivery of LSS were also detected. The most important difference refers to the memory domain. In fact, the performance in delayed memory stabilized but did not improve compared to the LSS-direct group. The lower effect on memory of LSS-tele intervention may be explained in several ways. Patients in the LSS-tele group were slightly older than patients of the LSS-direct group. This demographic characteristic may underscore a possible selection bias effect, for which older patients could have more brain and systemic comorbidities influencing the cognitive profile towards a mixed amnestic/dysexecutive profile. Patients with more impaired executive functions may have a more rapid decline of immediate memory and a poor response to the rehabilitation of delayed memory.33 Indeed, the elaboration of information and learning capacities of patients in the LSS-tele group could have compromised a successful storage of new information in the long-term episodic memory.
Another possible explanation considers that the use of telecommunication technologies could have influenced the profile of cognitive changes after rehabilitation; hearing and vision impairments, although subtle, may interfere with some aspects of telecommunication logistic such as the appreciation of good sound or visual quality or clarity. All these factors could be an important cause of distraction, especially for older people, who may have little or no experience or confidence in using technology involving computers. All these factors concurrently might have created a condition where LSS-tele patients were disadvantaged in the learning process, with direct consequences on the ability of storage and recall of learned material.
Notwithstanding these limitations, the stabilization of delayed memory performance, although with worse immediate memory, with respect to the trend of impairment in the control group should be underscored. In fact, UCS-treated participants showed impairments or no changes of the examined cognitive domains, confirming the slowly progressive deterioration typical of the clinical course of AD, even in 3 months.
This is the first pilot study investigating rehabilitation of amnestic cognitive impairment through telecommunication technology via teleconference. This methodology has been widely applied in the rehabilitation of speech disorders.11,12 Vestal et al34 demonstrated that assessment of language skills in mild AD patients can be accomplished via telemedicine, achieving results that are comparable with in-person assessment.
There is a limited number of studies which assessed an in-home videoconferencing system to determine the feasibility of delivering remote rehabilitation services to aged subjects.20,34 One study by Poon et al20 compared for the first time the effects of cognitive intervention through telemedicine with a face to face treatment in older patients with memory decline. Interestingly, the size effect of TR on global cognition was similar to that obtained from our study, MMSE score increase of 2–3 points and comparable to that of face to face intervention. However, in this first study, enrolled patients had memory complaints, without a better classification of the type of disease pathology causing such cognitive deficits; the methodology of cognitive intervention was not explained. A more recent study by Peel et al35 in 2011 found that cognitive impairment was one of the variables making delivery of TR challenging for aged individuals. The authors concluded that there are barriers to be overcome related to patient limitations (hearing and/or vision impairment, poor confidence in using computer-based technology), staff issues (specific training), and the logistics of the system (video and sound quality, location of equipment, need of initial training).35 Despite the logistic and experience limitations, Ramos-Ríos et al18 highlighted that use of telemedicine in the elderly population appeared to be well accepted by patients.
In conclusion, LSS through teleconference seems to be less efficient on memory abilities than face to face LSS treatment. However, compared to control UCS, domain-specific telecommunication rehabilitation improved general cognitive performance and denomination, while stabilizing delayed memory and working memory. Moreover, telecommunication technology delivery of cognitive rehabilitation was reported as a valuable and well-accepted methodology by the patients. Disseminating routine clinical use of TR services might offer a cost-effective approach for people affected by neurodegenerative diseases that otherwise could not be given more intensive face to face treatment and, therefore, may improve access to rehabilitation care.
Acknowledgment
We thank Prof Mario Ermani for assistance in statistical analysis.
Disclosure
The authors report no conflicts of interest in this work.
References
Brennan DM, Tindall L, Theodoros D, et al; American Telemedicine Association. A blueprint for telerehabilitation guidelines – October 2010. Telemed J E Health. 2011;17(8):662–665. | ||
Forducey PG, Ruwe WD, Dawson SJ, Scheideman-Miller C, McDonald NB, Hantla MR. Using telerehabilitation to promote TBI recovery and transfer of knowledge. Neuro Rehabilitation. 2003;18(2):103–111. | ||
Fearon P, Langhorne P; Early Supported Discharge Trialists. Services for reducing duration of hospital care for acute stroke patients. Cochrane Database Syst Rev. 2012;9:CD000443. | ||
Mas MA, Inzitari M. A critical review of Early Supported Discharge for stroke patients: from evidence to implementation into practice. Int J Stroke. Epub 2012 Dec 11. | ||
Langhorne P, Holmqvist LW; Early Supported Discharge Trialist. Early supported discharge after stroke. J Rehabil Med. 2007;39(2):103–108. | ||
Finkelstein J, Wood J, Cha E. Impact of physical telerehabilitation on functional outcomes in seniors with mobility limitations. Conf Proc IEEE Eng Med Biol Soc. 2012;2012:5827–5832. | ||
Cikajlo I, Rudolf M, Goljar N, Burger H, Matjačić Z. Telerehabilitation using virtual reality task can improve balance in patients with stroke. Disabil Rehabil. 2012;34(1):13–18. | ||
Piron L, Turolla A, Agostini M, et al. Exercises for paretic upper limb after stroke: a combined virtual-reality and telemedicine approach. J Rehabil Med. 2009;41(12):1016–1102. | ||
Yip MP, Chang AM, Chan J, MacKenzie AE. Development of the Telemedicine Satisfaction Questionnaire to evaluate patient satisfaction with telemedicine: a preliminary study. J Telemed Telecare. 2003;9(1):46–50. | ||
Piron L, Turolla A, Tonin P, Piccione F, Lain L, Dam M. Satisfaction with care in post-stroke patients undergoing a telerehabilitation programme at home. J Telemed Telecare. 2008;14(5):257–260. | ||
Caltagirone C, Zannino GD. Telecommunications technology in cognitive rehabilitation. Funct Neurol. 2008;23(4):195–199. | ||
Cherney LR, van Vuuren S. Telerehabilitation, virtual therapists, and acquired neurologic speech and language disorders. Semin Speech Lang. 2012;33(3):243–257. | ||
Constantinescu G, Theodoros D, Russell T, Ward E, Wilson S, Wootton R. Treating disordered speech and voice in Parkinson’s disease online: a randomized controlled non-inferiority trial. Int J Lang Commun Disord. 2011;46(1):1–16. | ||
Brennan DM, Georgeadis AC, Baron CR, Barker LM. The effect of videoconference-based telerehabilitation on story retelling performance by brain-injured subjects and its implications for remote speech-language therapy. Telemed J E Health. 2004;10(2):147–154. | ||
Dechene L, Tousignant M, Boissy P, et al. Simulated in-home teletreatment for anomia. Int J Telerehab. 2011;3(2):3–10. | ||
Agostini M, Garzon M, Benavides-Varela S, et al. Telerehabilitation in poststroke anomia. Biomed Res Int. 2014;2014:706909. | ||
Hildebrand R, Chow H, Williams C, Nelson M, Wass P. Feasibility of neuropsychological testing of older adults via videoconference: implications for assessing the capacity for independent living. J Telemed Telecare. 2004;10(3):130–134. | ||
Ramos-Ríos R, Mateos R, Lojo D, Conn DK, Patterson T. Telepsychogeriatrics: a new horizon in the care of mental health problems in the elderly. Int Psychogeriatr. 2012;24(11):1708–1724. | ||
Cullum CM, Weiner MF, Gehrmann HR, Hynan LS. Feasibility of telecognitive assessment in dementia. Assessment. 2006;13(4):385–390. | ||
Poon P, Hui E, Dai D, Kwok T, Woo J. Cognitive intervention for community-dwelling older persons with memory problems: telemedicine versus face-to-face treatment. Int J Geriatr Psychiatry. 2005;20(3):285–286. | ||
Alzheimer’s Disease International. World Alzheimer Report 2011: The benefits of early diagnosis and intervention [webpage on the Internet]. London: Alzheimer’s Disease International; 2011. Available from: www.alz.co.uk/worldreport2011. | ||
Olazarán J, Reisberg B, Clare L, et al. Nonpharmachological therapies in Alzheimer’s disease: a systematic review of efficacy. Dement Geriatr Cogn Disord. 2010;30(2):161–178. | ||
Stott J, Spector A. A review of the effectiveness of memory interventions in mild cognitive impairment (MCI). Int Psychogeriatr. 2011;23(4):526–538. | ||
Martin M, Clare L, Altgassen AM, Cameron MH, Zehnder F. Cognition-based interventions for healthy older people and people with mild cognitive impairment. Cochrane Database Syst Rev. 2011;1:CD006220. | ||
De Marco M, Shanks MF, Venneri A. Cognitive stimulation: the evidence base for its application in neurodegenerative disease. Curr Alzheimer Res. 2014;11(5):469–483. | ||
Jelcic N, Cagnin A, Meneghello F, Turolla A, Ermani M, Dam M. Effects of lexical-semantic treatment on memory in early Alzheimer disease: an observer-blinded randomized controlled trial. Neurorehabil Neural Repair. 2012;26(8):949–956. | ||
McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology. 1984;34(7):939–944. | ||
Cummings JL, Mega M, Gray K, Rosemberg-Thompson S, Carusi DA, Gornbein J. The Neuropsychiatric Inventory: comprehensive assessment of psychopathology in dimentia. Neurology.1994;44(12):2308–2314. | ||
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. | ||
Carlesimo GA, Caltagirone C, Gainotti G. The Mental Deterioration Battery: normative data, diagnostic reliability and qualitative analyses of cognitive impairment. The Group for the Standardization of the Mental Deterioration Battery. Eur Neurol. 1996;36(6):378–384. | ||
Novelli G, Papagno C, Capitani E, Laiacona N, Vallar G, Cappa SF. Tre tests clinici di memoria verbale a lungo termine. Taratura su soggetti normali [Three clinical tests for the assessment of verbal long-term memory function: norms from 320 normal subjects]. Arch Psicol Neurol Psichiatr. 1986;47(2):278–296. Italian [with English abstract]. | ||
Rey A. L’examen Clinique en Psychologie. Paris, France: Presses Universitaire de France; 1964. | ||
Schmidt C, Wolff M, Weitz M, Bartlau T, Korth C, Zerr I. Rapidly progressive Alzheimer disease. Arch Neurol. 2011;68(9):1124–1130. | ||
Vestal L, Smith-Olinde L, Hicks G, Hutton T, Hart J. Efficacy of language assessment in Alzheimer’s disease: comparing in-person examination and telemedicine. Clin Interv Aging. 2006;1(4):467–471. | ||
Peel NM, Russell TG, Gray LC. Feasibility of using an in-home video conferencing system in geriatric rehabilitation. J Rehabil Med. 2011;43(4):364–366. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.