Back to Journals » Patient Preference and Adherence » Volume 12
Fatigue of systemic lupus erythematosus in China: contributors and effects on the quality of life
Authors Du X, Zhao Q, Zhuang Y, Chen H, Shen B
Received 13 April 2018
Accepted for publication 21 June 2018
Published 6 September 2018 Volume 2018:12 Pages 1729—1735
DOI https://doi.org/10.2147/PPA.S170984
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Naifeng Liu
Xian Du,1,2,* Qian Zhao,2,* Yuan Zhuang,2,* Haoyang Chen,1 Biyu Shen1,2
1Department of Nursing, The Second Affiliated Hospital of Nantong University, Nantong, China; 2School of Nursing, Nantong University, Nantong, China
*These authors contributed equally to this work
Objective: Fatigue is a very common symptom of systemic lupus erythematosus (SLE), which significantly impairs patients’ quality of life. The purpose of this study is to evaluate contributors of fatigue and effects of fatigue on the quality of life in Chinese SLE patients.
Methods: A survey of 119 SLE patients using the Fatigue Severity Scale (FSS) to assess the severity of fatigue was carried out. SLE patients completed the Systemic Lupus Erythematosus Disease Activity Index, the Hospital Anxiety and Depression Scale, the Short Form 36 health survey and the Pittsburgh Sleep Quality Index. Meanwhile, 105 healthy individuals completed FSS, the Hospital Anxiety and Depression Scale and Short Form 36 health survey. We used chi-squared analysis, independent samples t-tests and logistic regression models to analyze data.
Results: Our results found that the FSS score of patients with SLE was higher than that of healthy controls. The disease duration, anxiety, depression, subjective sleep quality and sleep disorders significantly correlated with fatigue in SLE patients. Moreover, logistic regression models showed depression and sleep disorders as predictors of fatigue. In SLE patients, fatigued patients had lower quality of life than those who were non-fatigued.
Conclusion: This is the first time to explore contributors of fatigue and the influence of fatigue on SLE patients’ quality of life in China. Our study showed that depression and sleep disorders were predictors of fatigue, and fatigue seriously damaged SLE patients’ quality of life. The results indicate that it is necessary to conduct holistic assessment and effective intervention, such as systemic psychiatric screening, psychological care and practical sleep guidance, to relieve symptoms of fatigue and finally improve their quality of life in SLE patients.
Keywords: systemic lupus erythematosus, fatigue, quality of life, depression, sleep disorders
Background
Systemic lupus erythematosus (SLE) is a chronic, progressive and recurrent autoimmune disease, which may cause inflammation activity and damage in any of the organs, often resulting in decreased physical, emotional and social abilities, and depression, pain, fatigue and so on.1,2 Moreover, fatigue, as a common symptom, affects more than 90% of SLE patients.3,4 Previous studies reported that fatigue had a negative impact on work performance, family responsibility and social activities,4,5 which can seriously affect the quality of life in SLE patients.6,7 Therefore, it is very important to identify factors leading to fatigue and improve their quality of life in SLE patients.
Due to the complexity of study on SLE fatigue mechanism and the lack of a unified conclusion, we explore the factors related to SLE fatigue through cross-sectional studies. Studies indicate that fatigue in SLE is associated with anxiety, depression, pain and body mass index (BMI).8,9 The correlation between fatigue scoring and depression is higher in the SLE population than other medical conditions such as Lyme disease or multiple sclerosis.10,11 Jump et al12 find the importance of pain in predicting fatigue levels in SLE patients. Data from a multiethnic SLE cohort study show that 28% of the patients are obese, with a BMI of 30 kg/m2 and above, and that this is associated with more severe fatigue.11 Physical inactivity, lack of social support and sleep disorders are also associated with fatigue in SLE patients.13,14 But the cause of fatigue is still unclear. For example, the association between fatigue and disease activity in SLE is still controversial.15
Although patients with SLE suffer from severe fatigue, only few studies related to fatigue of SLE patients have been conducted in China. The purpose of our study is 1) to explore contributing factors of fatigue in SLE patients and 2) to evaluate the impact of fatigue on the quality of life in Chinese SLE patients.
Methods
Participants
Patients were recruited from the Second Affiliated Hospital of Nantong University between November 2016 and November 2017. A total of 125 SLE patients from outpatients or inpatients of the rheumatology department and 110 healthy individuals based on patients’ gender and age from those attending for an annual examination were invited to participate in a cross-sectional study, and 119 (95.2% of the patients) and 105 (95.5% of the healthy individuals) of them were eventually included in the present research, as six SLE patients and five healthy individuals were reluctant to spend time filling out questionnaires. All patients fulfilled the 1997 American College of Rheumatology revised criteria for the classification of SLE.16 Patients were excluded on the basis of the following: 1) they had comorbidities (for instance, malignancy, cardiopathy, respiratory or endocrine diseases) that could affect fatigue and 2) they did not complete questionnaires. Healthy subjects were excluded if they had a history of or if they are currently diagnosed with other systemic or neurological diseases. This research was approved by the Ethics Committee of the Second Affiliated Hospital of Nantong University, and the written informed consents were acquired from all participants based on the Declaration of Helsinki.
Demographic and clinical characteristics
Demographic and clinical data included gender, age (years), BMI, marital status, education level (years), employment status, income/person/year, personal health insurance, tobacco and alcohol usage and exercise. The disease duration (years) and use of hormones were obtained by viewing medical records combined with SLE patients’ self-report. At the same time, we used the Systemic Lupus Erythematosus Disease Activity Index (SLEDAI) to measure disease activity when collecting questionnaires.16
Measures of clinical variables
Fatigue Severity Scale (FSS): The FSS questionnaire was used to assess the severity of fatigue. The FSS contained nine items formulated as statements on the fatigue experience itself (item 3), what caused fatigue (item 2) and how fatigue affected daily life (seven items). People were instructed to assign a score between 1 (completely disagree) and 7 (completely agree) to each of 9 FSS items. The average of scores of the nine items was the overall score, and higher scores demonstrated more severe fatigue. The FSS has been proved to have reliability, high sensitivity and internal consistency in fatigue assessment.17 We used a cutoff score ≥4 to define fatigue cases based on data in the literature demonstrating that the FSS score ≥4 reliably differentiated subjects with fatigue from the controls.17–19
The Hospital Anxiety and Depression Scale (HADS): We used the HADS to assess psychological status. The seven-item subscales were used to assess anxiety and depression scores ranging from 0 to 21, and the higher the score, the more serious the mood disorder.20
The Pittsburgh Sleep Quality Index (PSQI): We used the PSQI to assess sleep quality. It had 19 questions including seven aspects (subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disorders, use of hypnotics and daytime dysfunction), and each part’s score from 0 (score of no difficulty) to 3 (score of severe difficulty) was summed to get a total score from 0 to 21.21
The Short Form 36 health survey (SF-36): We used the SF-36 to assess quality of life. It evaluated eight aspects (physical functioning (PF), role limitations due to physical problems (RP), bodily pain (BP), general health perception (GH), energy/vitality (VT), social function (SF), role limitations due to emotional problems (RE), and mental health (MH)), and the score range was 0–100, with the higher score demonstrating the better health status. The score of Z-transformed and normalized domain was divided into the Physical Components Summary (PCS) score and the Mental Components Summary (MCS) score.22
Data collection
These written questionnaires were finished by patients with the physician present or by the physician enquiring patients linked questions (an interview-led questionnaire) in the clinical surrounding. After finishing data collection, the results were calculated by nurses. Two research assistants double-checked original data and then added the results to a computer database.
Statistical analysis
Descriptive analyses were performed as number (percentage) or mean (±SD) according to type and distribution of measured variables. The differences on the basis of categorical variables and continuous variables that were investigated in SLE patients who were divided into non-fatigued patients and fatigued patients were measured with the chi-squared analyses and t-tests, respectively, as well as the differences between the SLE patients and healthy individuals. All variables significantly related to fatigue by univariate tests were included into logistic regression models with the dichotomous fatigue assessed by the FSS as the dependent variable. We used independent sample t-test based on continuous variables to assess groups (non-fatigued patients or fatigued patients) differences on the quality of life. We considered that it had statistical significance when P<0.05 (two-sided), and we used SPSS (version 20.0) to analyze the data.
Results
Patient characteristics
Table 1 showed baseline participant characteristics in this analysis. SLE patients’ mean (SD) age was 36.16 (11.80) years and 96.6% were female. Of them, 37.8% SLE patients used hormones more than 7.5 mg/d. The mean (SD) of disease duration and SLEDAI were 6.58 (5.51) years and 4.32 (3.36), respectively. There was no significant difference in gender, age, BMI, marital status, education, employment status, yearly income, personal health insurance, smoking use, alcohol use and exercise between the SLE patients and the controls (P>0.05).
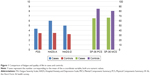
Comparison of fatigue and quality of life
From Figure 1, SLE patients scored higher than healthy controls on FSS, HADS-A and HADS-D and scored lower on SF-36 PCS and SF-36 MCS, which demonstrated that SLE patients obviously had more serious fatigue, higher levels of anxiety, depression and worse quality of life compared with the healthy controls.
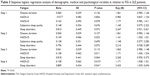
Differences between non-fatigued patients and fatigued patients in SLE
As indicated in Table 2, a great number of demographic, clinical and psychological factors were checked for possible differences between non-fatigued patients and fatigued patients in SLE. Fatigued patients tended to have longer disease duration (P=0.041), higher degree of anxiety (P=0.006), higher degree of depression (P=0.001), worse subjective sleep quality (P=0.038) and severer sleep disorders (P=0.003) compared with non-fatigued patients. However, there was no significant difference in the degree of disease activity (P=0.882).
Determinants of fatigue in SLE patients
Logistic regression analysis was used to explore predictors of fatigue, as presented in Table 3. We examined that HADS-D (β=0.158, P<0.05) and sleep disorders (β=0.889, P<0.05) were the predictors of fatigue.
Effects of fatigue on quality of life in SLE patients
Comparison of non-fatigued patients and fatigued patients in terms of quality of life was exhibited in Table 4. Fatigued patients in SLE had significantly lower quality of life in all domains of the SF-36 scale (P<0.05).
Discussion
Fatigue problems are common. Overman et al23 reported that one out of every two patients with a rheumatic disease was severely fatigued. In SLE patients, fatigue has been found to have an impact on multiple aspects of SLE patients’ life, such as work and activities of daily living, emotions, cognition, social and family activities.24 In the present study, depression and sleep disorders were independent predictors of fatigue in SLE patients. What’s more, fatigued patients had impaired quality of life than non-fatigued patients.
Previous studies found that the degree of disease activity was associated with fatigue.12,13 However, Wang et al25 concluded that fatigue in SLE patients did not correlate with disease activity using scales of SLEDAI and FSS. A recent study in Turkey showed that disease activity was not related to fatigue.15 Our study has indicated that fatigue was not associated with disease activity, but it was related to the disease duration. The possible explanation may be that the proportion of SLE patients with damage increased significantly with disease duration,26 which may affect SLE patients’ fatigue and the quality of life.
An increasing number of studies have indicated that depression was consistently associated with fatigue in SLE patients.27,28 It has been reported that the prevalence of depression in SLE patients was two times higher than that in the general population.29 In our previous study, the incidence of depression in SLE patients was up to 32.9%.30 Depression had a huge impact on SLE patients, including suicide ideation,31 increased incidence of cardiovascular disease,32 and a decline in quality of life.33 In the present study, we also found that fatigued patients had significantly higher levels of HADS-A and HADS-D scores compared with non-fatigued patients. Interestingly, logistic regression analysis indicated that depression played an important role in fatigue, which was consistent with previous studies.15,34 The data suggested the need for systemic psychiatric screening and management and the importance of helping SLE patients to develop cognitive, behavioral and emotional strategies, which can relieve fatigue and improve quality of life.4,35
Previous research found that sleep disorders were also related to fatigue in SLE patients.36 Our study has also shown fatigued patients tended to have severer sleep disorders compared to non-fatigued patients. Importantly, logistic regression analysis indicated that sleep disorders had significant impacts on fatigue. In chronic inflammatory diseases including SLE, sleep disorders were thought to worsen the disease symptoms including fatigue and lower the patients’ quality of life.37 This suggests that it is necessary to take measures to improve sleep quality, such as sleep management including sleep education and cognitive-behavioral interventions, so as to alleviate fatigue.38
SLE, as a chronic disease, led to patients’ physical and mental impacts and decreased their quality of life.39 Our study also showed SLE patients had worse quality of life than healthy controls. Studies indicated that fatigue can affect the quality of life of patients in SLE.40 In the present study, we found that fatigued patients in SLE had significantly lower quality of life compared with non-fatigued patients. Therefore, it is very important to intervene in fatigue and improve their quality of life in SLE patients.
To our knowledge, this study is the first to examine the related factors of fatigue and the impact of fatigue on the quality of life in Chinese SLE patients. However, we still had several shortcomings. First, because all SLE patients participated in our survey were from a single clinic of rheumatology and sample sizes were relatively small, it should be cautious to generalize findings to other population. Second, we cannot check causal relationships between variables due to cross-sectional design. Further research with expanded sample sizes, targeted fatigue measures and prospective researches on SLE patients’ fatigue should be implemented, which is more conducive to alleviating fatigue and improving the quality of life.
Conclusion
In short, this study is the first known assessment of the contributors of fatigue and the effects of fatigue on quality of life in Chinese patients with SLE. Our study has found that severity of fatigue in SLE patients was higher than in healthy individuals, and fatigue may significantly damage patients’ quality of life. Depression and sleep disorders play important roles in fatigue of SLE patients. The results suggest that overall assessment and targeted management (eg, systemic psychiatric screening and sleep intervention) of SLE patients are needed to relieve symptoms of fatigue and finally improve their quality of life.
Acknowledgments
We want to thank Zhifeng Gu, Lin Li and other members of the team for their assistance with this study. The study was supported by the Humanistic Nursing Care Foundation of China (grant number RW2016AM14), the Jiangsu Provincial Commission of Health and Family Planning Foundation (grant number Z201622), the Jiangsu Province “333 high level talent training project” Foundation (grant number BRA2016198) and the Jiangsu Province Youth Medical Talent Foundation (grant number QNRC2016409).
Author contributions
All authors contributed toward study design, data analysis, drafting and critically revising the paper, and agreed to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Thong B, Olsen NJ. Systemic lupus erythematosus diagnosis and management. Rheumatology. 2017;56(Suppl 1):i3–i13. | ||
Jolly M, Pickard AS, Mikolaitis RA, et al. Body image in patients with systemic lupus erythematosus. Int J Behav Med. 2012;19(2):157–164. | ||
Cleanthous S, Tyagi M, Isenberg DA, Newman SP. What do we know about self-reported fatigue in systemic lupus erythematosus? Lupus. 2012;21(5):465–476. | ||
O’Riordan R, Doran M, Connolly D. Fatigue and activity management education for individuals with systemic lupus erythematosus. Occup Ther Int. 2017;2017:1–11. | ||
Gallop K, Nixon A, Swinburn P, Sterling KL, Naegeli AN, Silk ME. Development of a conceptual model of health-related quality of life for systemic lupus erythematosus from the patient’s perspective. Lupus. 2012;21(9):934–943. | ||
Connolly D, O’Toole L, Redmond P, Smith SM. Managing fatigue in patients with chronic conditions in primary care. Fam Pract. 2013;30(2):123–124. | ||
Petri M, Kawata AK, Fernandes AW, et al. Impaired health status and the effect of pain and fatigue on functioning in clinical trial patients with systemic lupus erythematosus. J Rheumatol. 2013;40(11):1865–1874. | ||
Wiseman SJ, Bastin ME, Hamilton IF, et al. Fatigue and cognitive function in systemic lupus erythematosus: associations with white matter microstructural damage. A diffusion tensor MRI study and meta-analysis. Lupus. 2017;26(6):588–597. | ||
Özel F, Argon G. The effects of fatigue and pain on daily life activities in systemic lupus erythematosus. Agri. 2015;27(4):181–189. | ||
Krupp LB, Larocca NC, Luft BJ, Halpern JJ. Comparison of neurologic and psychologic findings in patients with Lyme disease and chronic fatigue syndrome. Neurology. 1989;39(Suppl 39):144. | ||
Chaiamnuay S, Bertoli AM, Fernández M, et al. The impact of increased body mass index on systemic lupus erythematosus: data from LUMINA, a multiethnic cohort (LUMINA XLVI). J Clin Rheumatol. 2007;13(3):128–133. | ||
Jump RL, Robinson ME, Armstrong AE, Barnes EV, Kilbourn KM, Richards HB. Fatigue in systemic lupus erythematosus: contributions of disease activity, pain, depression, and perceived social support. J Rheumatol. 2005;32(9):1699–1705. | ||
da Costa D, Dritsa M, Bernatsky S, et al. Dimensions of fatigue in systemic lupus erythematosus: relationship to disease status and behavioral and psychosocial factors. J Rheumatol. 2006;33(7):1282–1288. | ||
Mancuso CA, Perna M, Sargent AB, Salmon JE. Perceptions and measurements of physical activity in patients with systemic lupus erythematosus. Lupus. 2011;20(3):231–242. | ||
Yilmaz-Oner S, Ilhan B, Can M, et al. Fatigue in systemic lupus erythematosus: association with disease activity, quality of life and psychosocial factors. Z Rheumatol. 2017;76(10):913–919. | ||
Hochberg MC. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1997;40(9):1725. | ||
Krupp LB, Larocca NG, Muir-Nash J, Steinberg AD. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989;46(10):1121–1123. | ||
Flachenecker P, Kümpfel T, Kallmann B, et al. Fatigue in multiple sclerosis: a comparison of different rating scales and correlation to clinical parameters. Mult Scler. 2002;8(6):523–526. | ||
Ad Hoc Committee on Systemic Lupus Erythematosus Response Criteria for Fatigue. Measurement of fatigue in SLE: a systematic review. Arthrit Rheum. 2007;57:1348–1357. | ||
Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52(2):69–77. | ||
Liu XC, Tang MQ. Reliability and validity of the Pittsburgh sleep quality index. Chin J Psychiatry. 1996;29(02):103–107. | ||
Li L, Wang HM, Shen Y. Chinese SF-36 Health Survey: translation, cultural adaptation, validation, and normalisation. J Epidemiol Community Health. 2003;57(4):259–263. | ||
Overman CL, Kool MB, da Silva JA, Geenen R. The prevalence of severe fatigue in rheumatic diseases: an international study. Clin Rheumatol. 2016;35(2):409–415. | ||
Sterling K, Gallop K, Swinburn P, et al. Patient-reported fatigue and its impact on patients with systemic lupus erythematosus. Lupus. 2014;23(2):124–132. | ||
Wang B, Gladman DD, Urowitz MB. Fatigue in lupus is not correlated with disease activity. J Rheumatol. 1998;25(5):892–895. | ||
Zonana-Nacach A, Camargo-Coronel A, Yáñez P, et al. Measurement of damage in 210 Mexican patients with systemic lupus erythematosus: relationship with disease duration. Lupus. 1998;7(2):119–123. | ||
Xie X, Wu D, Chen H. Prevalence and risk factors of anxiety and depression in patients with systemic lupus erythematosus in Southwest China. Rheumatol Int. 2016;36(12):1705–1710. | ||
Skapinakis P, Lewis G, Mavreas V. Temporal relations between unexplained fatigue and depression: longitudinal data from an international study in primary care. Psychosom Med. 2004;66(3):330–335. | ||
Zhang L, Fu T, Yin R, Zhang Q, Shen B. Prevalence of depression and anxiety in systemic lupus erythematosus: a systematic review and meta-analysis. BMC Psychiatry. 2017;17(1):70. | ||
Shen B, Tan W, Feng G, et al. The correlations of disease activity, socioeconomic status, quality of life, and depression/anxiety in Chinese patients with systemic lupus erythematosus. Clin Dev Immunol. 2013;2013:270878. | ||
Mok CC, Chan KL, Cheung EF, Yip PS. Suicidal ideation in patients with systemic lupus erythematosus: incidence and risk factors. Rheumatology. 2014;53(4):714–721. | ||
Greco CM, Li T, Sattar A, et al. Association between depression and vascular disease in systemic lupus erythematosus. J Rheumatol. 2012;39(2):262–268. | ||
Mok CC, Chan KL, Ho LY, Ly H. Association of depressive/anxiety symptoms with quality of life and work ability in patients with systemic lupus erythematosus. Clin Exp Rheumatol. 2016;34(3):389–395. | ||
Pettersson S, Boström C, Eriksson K, Svenungsson E, Gunnarsson I, Henriksson EW. Lifestyle habits and fatigue among people with systemic lupus erythematosus and matched population controls. Lupus. 2015;24(9):955–965. | ||
Barlow J, Wright C, Sheasby J, Turner A, Hainsworth J. Self-management approaches for people with chronic conditions: a review. Patient Educ Couns. 2002;48(2):177–187. | ||
Moraleda V, Prados G, Martínez MP, Sánchez AI, Sabio JM, Miró E. Sleep quality, clinical and psychological manifestations in women with systemic lupus erythematosus. Int J Rheum Dis. 2017;20(10):1541–1550. | ||
Ranjbaran Z, Keefer L, Stepanski E, Farhadi A, Keshavarzian A. The relevance of sleep abnormalities to chronic inflammatory conditions. Inflamm Res. 2007;56(2):51–57. | ||
Inoue M, Shiozawa K, Yoshihara R, et al. Predictors of poor sleep quality in patients with systemic lupus erythematosus. Clin Rheumatol. 2017;36(5):1053–1062. | ||
Solati K, Mousavi M, Kheiri S, Hasanpour-Dehkordi A. The effectiveness of mindfulness-based cognitive therapy on psychological symptoms and quality of life in systemic lupus erythematosus patients: a randomized controlled trial. Oman Med J. 2017;32(5):378–385. | ||
Choi ST, Kang JI, Park IH, et al. Subscale analysis of quality of life in patients with systemic lupus erythematosus: association with depression, fatigue, disease activity and damage. Clin Exp Rheumatol. 2012;30(5):665–672. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.