Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 13
Factors influencing treatment escalation from long-acting muscarinic antagonist monotherapy to triple therapy in patients with COPD: a retrospective THIN-database analysis
Authors Hurst JR , Dilleen M, Morris K, Hills S, Emir B, Jones R
Received 10 October 2017
Accepted for publication 16 January 2018
Published 5 March 2018 Volume 2018:13 Pages 781—792
DOI https://doi.org/10.2147/COPD.S153655
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
John R Hurst,1 Maria Dilleen,2 Kevin Morris,3 Siân Hills,3 Birol Emir,4 Rupert Jones5
1UCL Respiratory, University College London, London, UK; 2Statistics, Global Product Development, Pfizer, Tadworth, UK; 3Medical Affairs, Pfizer, Tadworth, UK; 4Biostatistics, Global Product Development, Pfizer, New York, NY, USA; 5Clinical Trials & Health Research, Institute of Translational and Stratified Medicine, Plymouth University Peninsula Schools of Medicine and Dentistry, Plymouth, UK
Purpose: Inappropriate use of an inhaled corticosteroid (ICS) for COPD has clinical and economic disadvantages. This retrospective analysis of The UK Health Improvement Network (THIN) database identified factors influencing treatment escalation (step-up) from a long-acting muscarinic antagonist (LAMA) to triple therapy (LAMA + long-acting β-agonist-ICS). Secondary objectives included time to step up from first LAMA prescription, Global Initiative for Chronic Obstructive Lung Disease (GOLD) grouping (2011/2013, 2017), and Medical Research Council (MRC) grade prior to treatment escalation.
Materials and methods: Data were included from 14,866 people ≥35 years old with a COPD diagnosis (June 1, 2010–May 10, 2015) and initiated on LAMA monotherapy. The most commonly used LAMA at baseline was tiotropium (92%).
Results: Multivariate analysis (10,492 patients) revealed that COPD exacerbations, lower forced expiratory volume in 1 second (FEV1), “asthma”, MRC grade, proactive and reactive COPD primary care, elective secondary-care contact, cough, and number of short-acting bronchodilator prescriptions were positively associated with treatment escalation (P<0.05). Being older, a current/ex-smoker, or having increased sputum symptom codes were negatively associated with treatment escalation (P<0.05). Median MRC score was 2 at baseline and 3 prior to treatment escalation. Using the last MRC reading and exacerbation history in the year prior to escalation, GOLD 2017 groupings were A 27.4%, B 37.3%, C 15.3%, and D 20%. In patients with available FEV1 measures, exacerbations, and MRC code (n=1,064), GOLD 2011/2013 groupings were A 20.4%, B 19.2%, C 24.8%, and D 35.6%.
Conclusion: While the presence of COPD exacerbations seems to be the main driver for treatment escalation, according to the 2017 GOLD strategy many patients appear to be overtreated, as they would not be recommended for treatment escalation. Reviewing patients’ treatment in the light of the new GOLD strategy has the potential to reduce inappropriate use of triple therapy.
Keywords: inhaled corticosteroid, treatment step-up, GOLD 2017 grouping, patient overtreatment
Plain-language summary
In patients with COPD initiated on long-acting muscarinic antagonist monotherapy, this study identified that COPD exacerbations, lower forced expiratory volume in 1 second, “asthma”, and health-care contact were associated with escalation to triple therapy (long-acting muscarinic antagonist + long-acting β-agonist + inhaled corticosteroid [ICS]). When treatment practices were analyzed according to the 2017 Global Initiative for Chronic Obstructive Lung Disease strategy, many patients appeared to be overtreated, particularly with respect to prescription of triple therapy comprising ICSs. Understanding factors associated with the escalation of treatment to include ICSs may improve treatment practices in patients with COPD and bring them in line with the 2017 Global Initiative for Chronic Obstructive Lung Disease strategy, and moreover reduce the inappropriate, expensive, and potentially harmful overprescribing of ICSs for COPD.
Introduction
COPD is a complex respiratory disorder characterized by persistent airflow limitation that is usually progressive in nature and a major cause of morbidity and mortality.1–3 The World Health Organization estimates that approximately 3 million people died of COPD worldwide in 2015 (5% of all deaths), and predicts that due to higher smoking prevalence and aging populations in many countries, the prevalence of COPD is likely to increase in the future.4
The updated 2017 Global Initiative for Chronic Obstructive Lung Disease (GOLD) strategy categorizes patients into four grades of airflow obstruction (1–4), based on percentage of predicted forced expiratory volume in 1 second (FEV1), and into four risk groups (A–D), based on symptoms and exacerbation history.2,3 The previous 2011 GOLD strategy (which was slightly adapted in 2013) used the degree of airflow obstruction to contribute to A–D grouping, such that those individuals with FEV1 <50% were considered in groups C and D.1 In 2013, GOLD made a minor update and treated patients with one hospitalized exacerbation the same as patients with two or more nonhospitalized exacerbations.1
Long-term treatment with an inhaled corticosteroid (ICS) in combination with a long-acting β-agonist (LABA) is recommended therapy for certain patients in GOLD 2011/2013 groups C and D, but now there are preferred pathways that recommend optimal bronchodilation using a long-acting muscarinic antagonist (LAMA) or LAMA + LABA before the addition of ICS therapy (as triple therapy) in patients whose symptoms are not adequately controlled.3 In some patients, such as those with a history and/or findings suggestive of an asthma–COPD overlap, LABA–ICS therapy may be the first choice, but other options should also be considered.3 Despite these treatment pathways indicating appropriate prescription of ICSs, real-world data suggest that ICSs may be prescribed inappropriately in some patients. For example, in a study of more than 24,000 electronic patient records and patient-completed questionnaires from a large UK primary-care database, ~50% of patients in both the overall cohort (n=24,957) and the cohort with moderate airflow limitation (n=13,557) were receiving ICSs, either in combination with a LABA (26.7% for both cohorts) or in combination with a LABA and a LAMA (23.2% and 19.9%, respectively).5 These findings revealed that an ICS in combination with LABA or LABA + LAMA was the most frequently used treatment in patients in GOLD group A or B, and that ICSs had been prescribed in 49% of patients with moderate airflow obstruction and no exacerbations in the previous year.5 In light of this, the authors concluded that ICSs were prescribed irrespective of the severity of airflow limitation, asthma diagnosis, and exacerbation history,5 which is not in accordance with the 2017 GOLD strategy.3 Studies of ICS withdrawal, even in COPD patients with a history of exacerbations, have shown strategies can be safely undertaken that enable patients to change to a more appropriate therapy according to up-to-date guidances.6,7
The potentially inappropriate use of ICSs in patients with COPD has economic and clinical implications,8–12 being associated with an increased risk of adverse events, including pneumonia, osteoporosis, diabetes, and cataracts.8 The increased risk of pneumonia, for example, is particularly well documented.9–12 The economic impact of COPD and its treatment costs are considerable. For example, the UK National Institute for Health and Care Excellence (NICE) estimated that COPD costs the National Health Service (NHS) over £268 million in prescriptions alone (based on 2011 data).13 Furthermore, the net ingredient cost of preparations containing ICSs for respiratory disease (asthma and COPD) in England alone has been estimated to be in excess of £700 million, based on 2014 data.13 If ICSs are inappropriately prescribed to certain patients, it is one more factor adding to the already high economic and social burden associated with COPD.
Guidelines from expert panels, such as GOLD, are developed and routinely updated to aid most appropriate treatment practices, supported by clinical observations. Therefore, understanding the pathway and predictors for treatment escalation in COPD may help identify patients for whom alternative treatment strategies or treatment escalation without ICSs may be more appropriate. This study was conducted to determine the factors influencing treatment escalation (step-up) to a LAMA + LABA–ICS fixed-dose combination (FDC) inhaler (triple therapy) in patients with COPD who had been initiated on LAMA monotherapy, and included assessment of patients and their treatment using both the GOLD 2011/2013 and the more up-to-date GOLD 2017 classification criteria.1,3 The primary objective was to identify factors significantly associated with time to step-up from LAMA monotherapy to LAMA + LABA–ICS (triple therapy). Secondary objectives included assessing time to step-up from first LAMA prescription, GOLD category according to 2017 criteria, and change in breathlessness (Medical Research Council [MRC]) score prior to treatment escalation.
Materials and methods
Study design
This was a retrospective analysis of anonymized electronic medical records (EMRs) in The UK Health Improvement Network (THIN) database, a primary-care EMR-data resource with 3 million active patients and 385 active GP practices. Patients were representative of the UK population by age, sex, medical conditions, and death rates adjusted for demographics and social deprivation. The EMRs were consistently updated and could be followed over time. The GPs contributing data to THIN provided health services under the terms of the UK’s NHS.14
The THIN data-collection scheme is approved by the UK South-East Multicentre Research Ethics Committee (SRC). Approval for this study was gained from the IMS Health Independent Scientific Board (SRC reference 16THIN, approval March 29, 2016). The study was conducted in accordance with legal and regulatory requirements and followed research practices described in the Guidelines for Good Pharmacoepidemiology Practices issued by the International Society for Pharmacoepidemiology, International Society for Pharmacoeconomics and Outcomes Research guidance, and Pharmaceutical Research and Manufacturers Association guidelines.
Study periods
The study period included data until May 10, 2016, and was the time from the index event (date of first LAMA prescription) until the time that the patient received LAMA + LABA–ICS (triple therapy, defined as any LABA–ICS FDC prescription after initiation of LAMA monotherapy; patients must have also received a LAMA within 2 months of treatment escalation). Patients were included if they had a COPD diagnosis between June 1, 2010 and May 10, 2015, allowing for at least 1 year of follow-up.
Participants
Data were extracted for patients who had a diagnosis of COPD (excluding an asthma diagnosis) who were ≥35 years old and who had received LAMA monotherapy only (aclidinium, glycopyrronium, tiotropium, or umeclidinium) as initial COPD treatment prior to treatment escalation. Data from patients who started therapy comprising a LAMA in combination with any other COPD maintenance therapy (LABA, ICS, or LABA–ICS FDC) or who had a history of LAMA, LABA, LABA–LAMA FDC, ICS, or LABA–ICS use in the 2-month (60-day) preindex period were excluded. Use of reliever medications, mucolytics, and xanthines was accepted.
Statistical analysis
As the study was a retrospective noninterventional database analysis of anonymized patient records, a formal sample size was not calculated. A feasibility calculation was carried out to assess the potential size of the population to be studied. SAS version 9.4 (SAS Institute, Cary, NC, USA) was used for all analyses. No missing data imputations and no multiplicity adjustments were performed.
Patient characteristics and comorbidities recorded at any time are summarized descriptively (Table S1). Time to treatment escalation (step-up) was assessed using univariate and multivariable Cox regression incorporating time-varying covariates.15 The univariate analysis included 14,866 patients, and any missing data due to missing covariates were censored for that observation. For the multivariate Cox regression, to ensure inclusion of patients who had FEV1 and MRC recorded, the final data set was reduced to 10,492. Statistically significant time-varying covariates were included in the final model using a stepwise model-selection procedure. Factors significantly associated with treatment escalation (P<0.05) were retained in the model.
In the prespecified analysis plan, the following initial terms were included in the multivariate analysis selection: age, sex, FEV1, physician-coded asthma, chronic kidney disease, mental health disorders, depression, anxiety, osteoporosis, rheumatoid arthritis, lung cancer, obesity, epilepsy, diabetes, pneumonia, MRC grade, smoking status, cough symptoms (number of consultations with code for cough), sputum symptoms (number of consultations with code for sputum), short-acting bronchodilator use, proactive COPD primary care (defined as COPD monitoring [including by doctor or nurse], shared-care disease monitoring, COPD 3-, 6-, or 12-month review follow-up, COPD health education, COPD-medication optimization, issue of COPD rescue pack or advance supply of steroid medication or antibiotic medication [or deferred antibiotic therapy], COPD leaflet given, has COPD care plan or care pathway, COPD clinical management plan, on COPD supportive care pathway, seen in COPD clinic), reactive COPD primary care (defined as nighttime or out-of-hours visit, follow-up or acute visit, home-, hotel-, or nursing/residential home visit, twilight visit by the practice, their cooperative, deputizing service, or local roster service, reactive or cooperative surgery consultation, minor-injury service, medicine management or telephone consultation related to COPD), elective secondary-care contact (defined as COPD secondary-care consultation or respiratory hospital referral), COPD exacerbations (composite end point defined as COPD emergency admission or acute exacerbation of COPD, lower respiratory tract infection, oral corticosteroids (OCS) and antibiotic prescription on same day, according to the definition used previously),16 and cardiovascular risk (composite end point defined as combined comorbidity for cardiovascular risk). Cough symptoms, sputum symptoms, proactive and reactive COPD primary care, and elective secondary-care contact were based on Read code data only.
A stepwise procedure was followed, which is useful where there is a large number of potential explanatory variables and no underlying theory for the order on which to base the model selection. The order of importance of variables automatically selected in the stepwise process was: COPD exacerbations (composite), FEV1, “asthma”, proactive COPD primary care, use of short-acting bronchodilators, reactive COPD primary care, MRC grade, smoking status, cough symptoms, elective secondary-care contact, sputum symptoms, and age. Terms were retained in the model if P<0.05.
GOLD grouping was analyzed according to GOLD 2011/2013 criteria for patients with any FEV1, MRC available during the last 360 days of the study period (and exacerbations/hospitalizations as previously described),1 and GOLD 2017 classification criteria for patients with any MRC available during the last 360 days of the study period (and exacerbations/hospitalizations as previously described).3
Results
Patient baseline characteristics
In total, data from 14,866 patients were included in this analysis (Figure 1): 6,482 of 14,866 (43.6%) received treatment escalation, and 8,384 of 14,866 (56.4%) remained on LAMA monotherapy. Overall, 1,875 of 14,866 patients (12.6%) were lost to follow-up due to death. Patient baseline characteristics are given in Table 1. The mean age of the overall population was 68 years, and 54% were male. In the treatment-escalation group, the mean age was 68 years and 55% were male. The most commonly used LAMA at baseline was tiotropium (92%). Of patients who received treatment escalation, the majority were prescribed fluticasone propionate 500 μg–salmeterol 50 μg (as Seretide 500 Accuhaler; 29%), followed by salmeterol 25 μg–fluticasone 250 μg (as Seretide 250 Evohaler, 16%). The Seretide 250 Evohaler inhaler device does not have a license for the treatment of COPD.
Comorbidities
The most prevalent comorbidities were hypertension (44%), chronic heart disease (20%), anxiety (20%), and diabetes (15%) (Table 2). Comparison of comorbidities in the population studied here with those in the general population of England17 suggests that the prevalence of heart failure (6.7% vs 0.7%, respectively) and osteoporosis (7.9% vs 0.1%, respectively) is greater in this COPD population, as might be expected.
  | Table 2 Comorbidities recorded at any time during the study period |
Time to treatment escalation
In total, 44% of the cohort received treatment escalation (Figure 2). Of these patients, 85% did so within 2 years of initiating LAMA monotherapy. The median time to treatment escalation from the first LAMA prescription was 155 days (interquartile range 422–464 days). In the treatment-escalation group, 33% of patients who had an FEV1 recording had FEV1 <50% and 67% had FEV1 ≥50% prior to treatment escalation.
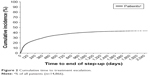  | Figure 2 Cumulative time to treatment escalation. |
Factors associated with treatment escalation
Univariate analysis
Factors associated with treatment escalation are reported in Table 3, of which COPD exacerbation was associated with the highest HR (2.68). Other factors positively associated (P<0.05) with treatment escalation included (in decreasing order of HR) MRC grade, “asthma”, elective secondary-care contact, proactive COPD primary care, pneumonia, cough symptoms, reactive COPD primary care, mental health disorders, depression, sputum symptoms, anxiety, number of short-acting bronchodilator prescriptions, and number of steroid prescriptions. Statistically significant factors that were negatively associated with treatment escalation were older age, higher FEV1, and current or ex-smoker status (Table 3). A small number of COPD patients in this study were recorded as never having smoked. However, the risk of treatment escalation for the two larger, more clinically relevant patient groups of current smokers and ex-smokers was similar (Table 3).
  | Table 3 Univariate Cox regression analysis with significant (P<0.05) unadjusted predictors of treatment escalation |
Multivariate analysis
The multivariate analysis included 10,492 patients, 4,591 of whom received treatment escalation. Observations confirmed that COPD exacerbations remained the factor most closely associated with treatment escalation (Table 4). Other factors, in decreasing order of HR, were “asthma”, MRC grade, proactive COPD primary care, reactive COPD primary care, elective secondary-care contact, cough symptoms, and number of short-acting bronchodilator prescriptions (all P<0.05). Age at index date, higher FEV1, sputum symptoms, and being a current or ex-smoker were negatively associated with treatment escalation (Table 4).
  | Table 4 Multivariate analysis outcomes: predictors of treatment escalation |
GOLD grade and group classification of patients prior to treatment escalation
The GOLD 2011/2013 group was determined in a subgroup of 1,064 patients with FEV1 exacerbations and MRC score available during the last 12 months of the study period who received treatment escalation (Table 5): 60% were classified as being in group C or D compared with 40% in A or B. The GOLD 2017 group was determined in a subgroup of 5,090 patients who had received treatment escalation and had an MRC score during the last 12 months of the study period (Table 5). In total, 35% of patients were classified as being in GOLD group C or D compared with 65% in group A or B. Similarly, GOLD 2017 grade was determined in a subgroup of 1,703 patients who had received treatment escalation and had an FEV1 score during the last 12 months of the study period (Table 5). In total, 67% of patients were classified as being grade 1 or 2 compared with 33% grade 3 or 4.
Assessment of treatment escalation per MRC group
Median MRC scores in the treatment-escalation group were 2 (interquartile range 2–3) at baseline (n=3,823) and 3 (interquartile range 2–3) during the study period (n=5,611, Figure 3), suggesting that patients became more breathless prior to treatment escalation.
Discussion
This retrospective analysis of the UK THIN database was conducted to determine the factors influencing treatment escalation to a LAMA + LABA–ICS (triple therapy) in patients with COPD who were initiated on LAMA monotherapy. To assess prescribing practices at the time of the study, we analyzed patients categorized by the then-current GOLD 2011/2013 groupings. In addition, as GOLD updated their guidance in 2017, we also analyzed patients according to the GOLD 2017 strategy. The multivariate analysis demonstrated that COPD exacerbations were the most significant factor (ie, had the highest HR) associated with treatment escalation, but physician-coded asthma, MRC grade, proactive COPD primary care, reactive COPD primary care, elective secondary-care contact, cough symptoms, and number of short-acting bronchodilator prescriptions were also clinically and statistically significantly associated with treatment escalation in these patients. The majority of patients had their treatment escalated within 2 years. As treatment escalation (or step-down) is likely to be initiated during a point of contact with a primary-care provider, it would be expected that patients with treatment-defined exacerbations and other consultations are more likely to receive treatment escalation. Indeed, similar findings have been reported by others.18,19 Both lower age and greater use of short-acting bronchodilators were statistically significant predictors of treatment escalation in both our univariate and multivariate analyses. Although the HRs were relatively small, it is of note that they represent the impact of one unit of the covariate. For age, the unit is 1 year, and for short-acting bronchodilator use, the unit is one extra prescription over the follow-up period. Age was negatively associated with treatment escalation; therefore, if age increased by 1 year, the hazard is multiplied by 0.994. Given the poor recording of FEV1 in this patient cohort, short-acting bronchodilator use could be an important marker to consider in the identification of patients who are more likely to require treatment optimization.
Our study focused on treatment escalation in patients receiving LAMA monotherapy only, and in the majority of cases we found that treatment escalation occurred within 2 years of treatment initiation. A smaller retrospective cohort study of 3,268 patients from the US Truven MarketScan commercial database likewise demonstrated dynamic changes to COPD prescriptions within 2 years of treatment initiation with a LABA.18 More specifically, within 24 months of follow-up, 16% of patients received treatment escalation, the majority of whom had added therapy (84%) progressed to triple therapy.18 This escalation may be a result of poor control of symptoms,18 in line with the present study, which suggests that treatment escalation is a direct result of COPD exacerbations or other symptoms that lead patients to contact their primary-care provider.20
A secondary objective of this study was to analyze how GOLD strategies guide treatment practices. Although UK treatment practices may be guided by NICE,13 guidelines from COPD-specific organizations, such as GOLD, are routinely updated to provide care paradigms reflective of recent clinical evidence.3 We analyzed treatment patterns according to GOLD grouping prior to treatment escalation by applying the GOLD 2017 strategy document, in addition to the GOLD 2011/2013 strategies that were contemporary to the study window. When data were analyzed using the 2011/2013 GOLD strategy, 60% of the 1,064 patients who received treatment escalation were classified as group C or D. When data were grouped according to the GOLD 2017 strategy, only 35% of the 5,090 patients who received treatment escalation were classified as group C or D. Although a larger sample was available for the 2017 analysis, this observation indicates that fewer patients are recommended for ICS treatment than under the GOLD 2011/2013 strategy, providing that they do not have comorbid asthma. Our findings reflect the impact of previous iterations of GOLD strategies or other national guidance, such as NICE in the UK, but may also be a result of an increase over time in the proportion of patients who are receiving triple therapy.21 According to the GOLD 2011/2013 strategy, which was in place during the study window, patients in group D (35.6% of the population) would have been recommended LABA–ICS therapy.1 In fact, at the time of the study, use of triple therapy was common practice, and NICE 2011 guidelines recommended that some patients with advanced COPD may require maintenance with OCS when these cannot be withdrawn following an exacerbation,13 and many UK GPs would follow this practice above all other strategies. It was not until after the period covered in this study, with publication of such studies as WISDOM and FLAME,7,22 that many doctors became aware that dual bronchodilation with LABA and LAMA is preferable to the use of ICS-containing regimens as first-line therapy for the majority of patients with COPD, particularly if the aim of treatment is to reduce the frequency of exacerbations.21,23 Published in 2014, the WISDOM study demonstrated that exacerbating patients with severe COPD run in on triple therapy (according to GOLD 2011/2013) were not at higher risk of severe exacerbations following withdrawal of ICSs compared with patients who continued on triple therapy.7 The GOLD 2017 strategy now recommends that alternative treatment strategies should be considered before the use of ICSs, including pulmonary rehabilitation, smoking cessation, and the addition of LABA without ICSs. The present observations suggest that if the GOLD 2017 strategy recommendations were adopted by clinicians, there would be a reduction in overprescription of ICSs. Future studies may highlight changes in treatment practice with the uptake and application of the GOLD 2017 strategy and other updates in national treatment guidance since the study was sampled.
This retrospective analysis has several strengths, but also some limitations. The THIN database is a very large data set that is representative of the UK population.24 Data are collected in a noninterventional way, thus reflecting “real-life” clinical practice. Information is continually updated, permitting investigation of the effects of new interventions/treatments. A literature search of the terms “THIN” and “validation” revealed that the THIN database has been validated for the Read codes for some but not all of the covariates used in this study.16,25–29 It is important to note that the GOLD guidelines were updated while the manuscript was in progress. Although GOLD guidance, such as GOLD 2011/2013, may have been contemporary to treatment practices during the study period, we additionally assessed patients according to GOLD 2017 grouping, in order to demonstrate how physicians may need to adapt their treatment practices in light of new evidence. As discussed, it is likely that physicians were treating according to older GOLD strategy or other guidance contemporary to the study window, such as NICE 2011, and this is a possible explanation for the high proportion of patients in the treatment-escalation group. Although only a minority of the study population had FEV1 measurements recorded in the database (17.7%, 2,635 of 14,866), FEV1 measurements were not required for COPD diagnosis. Furthermore, GOLD 2017 guidelines do not use FEV1 for determining categories (and hence treatment), which is a welcome change in policy, as FEV1 has been reported to be a poor predictor of exacerbation risk.30
Other limitations of this study include noncompliance to medication prescriptions, which results in inaccurate assumptions of drug-related exposure; validation gaps, and the fact that some covariates, even though validated (eg, COPD exacerbations and emergency admissions), may be poorly reported. A Hospital Episode Statistics-linked subset of the THIN database could have been employed for secondary-care COPD exacerbations, but it would have significantly reduced the number of eligible patients. However, comorbidities were chosen using Read codes used in the Quality and Outcomes Framework where relevant, which are well recorded. As with any database study, the quality of spirometry is not always assured. Finally, whether the current observations on treatment escalation can be generalized to the wider, non-UK COPD population is unknown and would require further study.
Conclusion
Overall, 44% of COPD patients in UK primary care received treatment escalation from LAMA monotherapy to triple therapy (LAMA + ICS–LABA). While the presence of COPD exacerbations appears to be the main driver for treatment escalation in this cohort, according to the 2017 GOLD strategy, 65% of the cohort who had their treatment escalated were classified as GOLD group A or B and would thus not now be recommended for treatment escalation. Reviewing patients’ treatment in light of updated GOLD strategy has the potential to reduce inappropriate prescription of triple therapy. If treatment escalation is needed in these patients, the GOLD strategy suggests the use of alternative strategies without ICSs.3 Given the gaps identified in EMR data recording, education on appropriate assessment and recording of data is required to guide rational treatment decisions and review.
Acknowledgments
This study was sponsored by Pfizer. The authors would like to thank Ewa Śleszyńska-Dopiera of Quanticate Ltd for her programming support. Medical writing support was provided by Helen Jones and Karen Burrows of Engage Scientific Solutions and was funded by Pfizer.
Disclosure
JRH reports personal fees for advisory boards and educational activities and support to attend meetings from pharmaceutical companies that make medicines to treat COPD. MD, SH, and BE are employees of Pfizer and have company stock/shares. KM was an employee of Pfizer at the time of study conduct. RJ reports no conflicts of interest in relation to this study, but reports personal fees from AstraZeneca, Boehringer Ingelheim, Chiesi, Cipla, GSK, Novartis, and Pfizer. The authors report no other conflicts of interest in this work.
References
Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of COPD. Bethesda (MD): GOLD; 2013. | ||
Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global Strategy for the Diagnosis, Management and Prevention of Chronic Obstructive Lung Disease 2017 report: GOLD Executive summary. Respirology. 2017;22(3):575–601. | ||
Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of COPD. Bethesda (MD): GOLD; 2017. | ||
World Health Organization. The top 10 causes of death. 2017. Available from: http://www.who.int/mediacentre/factsheets/fs310/en. Accessed April 12, 2017. | ||
Price D, West D, Brusselle G, et al. Management of COPD in the UK primary-care setting: an analysis of real-life prescribing patterns. Int J Chron Obstruct Pulmon Dis. 2014;9:889–904. | ||
Kaplan AG. Applying the wisdom of stepping down inhaled corticosteroids in patients with COPD: a proposed algorithm for clinical practice. Int J Chron Obstruct Pulmon Dis. 2015;10:2535–2548. | ||
Magnussen H, Disse B, Rodriguez-Roisin R, et al. Withdrawal of inhaled glucocorticoids and exacerbations of COPD. N Engl J Med. 2014;371(14):1285–1294. | ||
Price D, Yawn B, Brusselle G, Rossi A. Risk-to-benefit ratio of inhaled corticosteroids in patients with COPD. Prim Care Respir J. 2013;22(1):92–100. | ||
Calverley PM, Anderson JA, Celli B, et al. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med. 2007;356(8):775–789. | ||
Suissa S. Number needed to treat in COPD: exacerbations versus pneumonias. Thorax. 2013;68(6):540–543. | ||
Larsson K, Janson C, Lisspers K, et al. Combination of budesonide/formoterol more effective than fluticasone/salmeterol in preventing exacerbations in chronic obstructive pulmonary disease: the PATHOS study. J Intern Med. 2013;273(6):584–594. | ||
Yawn BP, Li Y, Tian H, Zhang J, Arcona S, Kahler KH. Inhaled corticosteroid use in patients with chronic obstructive pulmonary disease and the risk of pneumonia: a retrospective claims data analysis. Int J Chron Obstruct Pulmon Dis. 2013;8:295–304. | ||
National Institute for Health and Care Excellence. Chronic Obstructive Pulmonary Disease in Over 16s: Diagnosis and Management. London: NICE; 2011. | ||
IQVIA. Available from: https://www.visionhealth.co.uk/portfolio-items/the-health-improvement-network-thin/?portfolioCats=52. Accessed February 5, 2018. | ||
Cox DR. Regression models and life-tables. J R Stat Soc Series B Stat Methodol. 1972;34(2):187–220. | ||
Rothnie KJ, Müllerová H, Hurst JR, et al. Validation of the recording of acute exacerbations of COPD in UK primary care electronic healthcare records. PLoS One. 2016;11(3):e0151357. | ||
NHS England. QOF database. 2015. Available from: https://www.gpcontract.co.uk/browse/ENG/15. Accessed October 7, 2016. | ||
Wurst KE, St Laurent S, Müllerová H, Davis KJ. Characteristics of patients with COPD newly prescribed a long-acting bronchodilator: a retrospective cohort study. Int J Chron Obstruct Pulmon Dis. 2014;9:1021–1031. | ||
Kerkhof M, Freeman D, Jones R, Chisholm A, Price DB. Predicting frequent COPD exacerbations using primary care data. Int J Chron Obstruct Pulmon Dis. 2015;10:2439–2450. | ||
Hurst JR, Vestbo J, Anzueto A, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med. 2010;363(12):1128–1138. | ||
Brusselle G, Price D, Gruffydd-Jones K, et al. The inevitable drift to triple therapy in COPD: an analysis of prescribing pathways in the UK. Int J Chron Obstruct Pulmon Dis. 2015;10:2207–2217. | ||
Wedzicha JA, Banerji D, Chapman KR, et al. Indacaterol-glycopyrronium versus salmeterol-fluticasone for COPD. N Engl J Med. 2016;374(23):2222–2234. | ||
Halpin DM, Quint JK. The WISDOM of inhaled corticosteroids in COPD. Thorax. 2014;69(12):1071–1072. | ||
University College London. THIN database. 2015. Available from: https://www.ucl.ac.uk/pcph/research-groups-themes/thin-pub/database. Accessed April 12, 2017. | ||
Langley TE, Szatkowski LC, Wythe S, Lewis SA. Can primary care data be used to monitor regional smoking prevalence? An analysis of the Health Improvement Network primary care data. BMC Public Health. 2011;11:773. | ||
Iyen-Omofoman B, Hubbard RB, Smith CJ, et al. The distribution of lung cancer across sectors of society in the United Kingdom: a study using national primary care data. BMC Public Health. 2011;11:857. | ||
Meropol SB, Metlay JP. Accuracy of pneumonia hospital admissions in a primary care electronic medical record database. Pharmacoepidemiol Drug Saf. 2012;21(6):659–665. | ||
Quint JK, Müllerová H, DiSantostefano RL, et al. Validation of chronic obstructive pulmonary disease recording in the Clinical Practice Research Datalink (CPRD-GOLD). BMJ Open. 2014;4(7):e005540. | ||
Peng M, Chen G, Kaplan GG, et al. Methods of defining hypertension in electronic medical records: validation against national survey data. J Public Health (Oxf). 2016;38(3):e392–e399. | ||
Jones RC, Price D, Chavannes NH, et al. Multi-component assessment of chronic obstructive pulmonary disease: an evaluation of the ADO and DOSE indices and the global obstructive lung disease categories in international primary care data sets. NPJ Prim Care Respir Med. 2016;26:16010. |
Supplementary material
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.





