Back to Journals » Patient Preference and Adherence » Volume 13
Factors influencing completion of treatment among pulmonary tuberculosis patients
Authors Fang XH, Dan YL, Liu J, Jun L, Zhang ZP, Kan XH, Ma DC, Wu GC
Received 12 December 2018
Accepted for publication 12 March 2019
Published 10 April 2019 Volume 2019:13 Pages 491—496
DOI https://doi.org/10.2147/PPA.S198007
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Xue-Hui Fang,1,* Yi-Lin Dan,2,* Jie Liu,1 Lei Jun,1 Zhi-Ping Zhang,3 Xiao-Hong Kan,1 Dong-Chun Ma,1 Guo-Cui Wu4
1Department of Science and Education, Anhui Provincial TB Institute, Hefei, Anhui, People’s Republic of China; 2Department of Epidemiology and Biostatistics, School of Public Health, Anhui Medical University, Hefei, Anhui, People’s Republic of China; 3Department of Tuberculosis Prevention, Anqing Center for Disease Control and Prevention, Anqing, Anhui, People’s Republic of China; 4School of Nursing, Anhui Medical University, Hefei, Anhui, People’s Republic of China
*These authors contributed equally to this work
Objective: This study aimed to understand the influencing factors of treatment completion among pulmonary tuberculosis (PTB) patients in Anhui province, eastern People’s Republic of China, in order to provide scientific evidence for improving the follow-up rate and treatment completion rate.
Methods: A total of 262 PTB patients in six counties (districts) of Anhui province were investigated by questionnaire, and data about treatment interruption were collected.
Results: The main causes of treatment interruption were forgetting to take medicine (24.5%), drug side effects (23.3%), and symptomatic improvement (19.5%). The education background, patient type, cause of interruption, and tracking method were factors influencing completion of treatment (all P<0.05). The education level was positively associated with the treatment completion rate. New smear-positive patients had a significantly higher completion rate than others. The patients interrupted by drug side effects had the highest risk of interruption. In terms of the tracking method, the completion rate of patients tracked by the rural medical staff was significantly lower.
Conclusions: The management of PTB patients by medication supervision should be strengthened, especially for those with low education level and who had drug side effects, in order to improve their treatment completion rate.
Keywords: pulmonary tuberculosis, treatment completion, influencing factors
Background
Tuberculosis (TB) is a chronic disease transmitted by the respiratory tract caused by Mycobacterium tuberculosis,1 which may infect almost all body tissues and organs, but pulmonary tuberculosis (PTB) is the most common.2 PTB continues to be a very serious disease in People's Republic of China.3–5 With the progress of medical standards and the continual updating of the anti-TB drug, PTB is curable under the principles of early, combined, regular, moderate, and complete medication. However, PTB patients’ treatment compliance directly affects the treatment effect, and treatment interruption can lead to increased risk of drug resistance in these patients.6–9 PTB control work is difficult. A previous study has shown that the risk of drug resistance in PTB patients with treatment interruption was 13 times higher than that in patients without treatment interruption, and the drug resistance rate was significantly higher than that of patients without interruption.10 In developing countries, PTB patients with drug side effects, poverty, and low level of education were not highly compliant in the treatment, and patients were prone to treatment interruption.11–13 In this study, we explored the main causes of treatment interruption and influencing factors of treatment completion among PTB patients in Anhui province, eastern People's Republic of China, so as to provide a scientific basis for reducing the treatment interruption rate among TB patients and improving the patient tracking rate and the treatment completion rate.
Patients and methods
Patients
Anhui province is divided into three regions (Jiangnan, Jianghuai, and Huaibei), and two counties (districts) were randomly selected from each region. Using a stratified cluster sampling method, 283 PTB patients who had an interruption (stop taking the drug for one week or more) in treatment between March 1, 2014 and November 30, 2014 were selected from six counties (districts); 262 valid questionnaires were retrieved (Figure 1).
 | Figure 1 Patient recruitment flow chart. |
Methods
A self-designed questionnaire included general information (such as the social, demographic, and economic characteristics of PTB patients), patients’ treatment interruption, tracking methods, and treatment outcomes. Before the investigation, relevant experts were invited to conduct special training on the investigation among the investigators, focusing on the questionnaire survey techniques and quality control during the survey. A pilot area was selected to conduct the pre-surveys, and then the content of the questionnaire was revised according to the pre-survey results.
The study procedure was approved by the ethics committee of Anhui Provincial TB Institute. Written informed consent was provided by the participants, and the study was conducted in accordance with the Declaration of Helsinki.
Statistical analysis
Data were input and validation was performed with the double entry method using EpiData software version 3.1. SPSS version 23.0 was used for data analysis. Continuous variables were presented as mean±SD. The difference in categorical data among different groups was compared by χ2-test, and multiple logistic regression analyses were used to access the association between the completion rate and influencing factors. P≤0.05 was considered to be statistically significant.
Results
Demographic characteristics of patients, causes of interruption, and follow-up situation
All of the selected 283 PTB patients were investigated for socioeconomic and demographic characteristics, interruption of treatment, follow-up, and treatment outcome. A total of 262 valid questionnaires were retrieved, so the effective rate of the questionnaire was 92.6%. Among the 262 patients surveyed, there were 197 males (75.2%) and 65 females (24.8%) with a mean age of 51.42±19.93 years. The majority of patients had only a primary education level or below (47.3%). The main causes of interruption were drug side effects (23.3%) and forgetting to take medicine (24.5%) (Table 1).
 | Table 1 The demographic characteristics of patients, causes of interruption, and follow-up situation |
Influencing factors of the treatment completion rate
In the univariate analysis, education background, marital status, patient type, cause of interruption, and tracking methods were influencing factors of the treatment completion rate (all P<0.05). For example, the completion rate of patients with higher education level was higher than that of patients with lower education level. The completion rate of divorced or widowed patients was the lowest (54.55%). The completion rate of new smear-positive patients (86.83%) was significantly higher than that of other patients. In terms of the cause of interruption, the completion rate of patients who were interrupted due to forgetting to take medicine was the highest (93.85%), while patients who were interrupted by drug side effects had the lowest completion rate (54.10%). With regard to tracking personnel, the completion rate was significantly lower in patients who were followed by rural medical staff than that in patients followed by urban medical staff (Table 2).
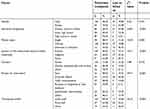 | Table 2 Factors related to the treatment completion rate of patients |
In multivariate analysis, four variables (education background, patient type, reason for interruption, and tracking method) appeared in the last step of the forward stepwise logistic regression model. Patients with an education background of junior high school had 3.28 times higher risk of non-completion than patients with an education background of high school or above, and patients with an education background of primary school or below had 4.7 times higher risk of non-completion than patients with an education background of high school or above. Smear-negative TB patients had 3.95 times higher risk than smear-positive TB patients. Regarding the reason for interruption, patients interrupted by drug side effects had the highest risk of non-completion. In terms of tracking personnel, patients who were tracked by urban medical staff had the lowest risk of non-completion (Table 3).
 | Table 3 Factors related to the treatment completion rate of patients by logistic regression analysis |
Discussion
As a chronic infectious disease, treatment of PTB usually requires a long period, generally at least half a year. In the treatment process, affected by many factors, patients are prone to treatment interruption. Thus, it affects the therapeutic effect forTB patients, and can even lead to the occurrence of drug resistance.14,15 There are many causes of treatment interruption among PTB patients. The causes of interruptions are different in patients from different regions, vocations, and education background.
Our study suggests that education background, patient type, cause of interruption, and tracking method were factors affecting the treatment completion rate. The lower the education level, the lower the rate of completion. The possible reason is that patients with lower educational level may lack related knowledge about TB and awareness of the importance of regular treatment, thus they are less likely to complete treatment.16 Previous studies found that the main influencing factor of treatment completion was a lack of knowledge about the disease, and better-educated patients were at lower risk of non-completion.11,16–18 In terms of patient type, smear-positive TB patients had a higher completion rate than smear-negative TB patients. It may be that the greater the perceived disease severity, the higher the treatment completion rate, which is similar to the results of a previous study.19 Our study found that the main causes of the treatment interruption were forgetting to take medicine, drug side effects, symptomatic improvement, poverty, traffic inconvenience, etc, which is consistent with several previous studies. Wei et al15 reported that the first three causes of treatment interruption in PTB patients were drug side effects, forgetting to take medicine because of busyness, and symptomatic improvement. Actual disease severity may affect the adherence to treatment, and patients were prone to interruption after feeling better.19 Long et al20reported the relationship between treatment cost and adherence, and higher cost leads to higher likelihood of non-adherence. In addition, our study found that patients interrupted due to drug side effects had the highest risk of non-completion. Regarding the tracking personnel, the completion rate of patients tracked by rural medical staff is significantly lower than for patients who were followed by urban medical staff. In accord with previous studies,21–24 the higher the level of tracking personnel, the higher the treatment completion rate. Obviously, medical staff not only spread knowledge about TB, but also make patients aware of the importance of regular treatment. We think that urban medical staff have a higher level of health education than rural medical staff, and patients tracked by urban staff also thought they got more attention, thus they had more confidence to be cured.
The study has some limitations. Firstly, the information of reason for interruption was based on self-report by patients, thus recall bias was inevitable. Secondly, we only investigated six counties (districts) in Anhui province, and the sample size was small, which may restrict the generalizability of our results.
Conclusion
Education background, patient type, reason for interruption, and tracking method are influencing factors of the treatment completion rate. In the future, the treatment management of TB patients should be strengthened, especially for patients with low educational level and drug side effects. Then, further reducing the medical burden of patients with financial difficulties in families, encouraging patients to cohabit with relatives, family members playing the role of supervision, standardizing diagnosis and treatment, and strengthening medication supervision could significantly improve the treatment compliance of TB patients, and further achieve the purpose of reducing drug resistance and improving the cure rate.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Berry MPR, Graham CM, McNab FW, et al. An interferon-inducible neutrophil-driven blood transcriptional signature in human tuberculosis. Nature. 2010;466(7309):973–977. doi:10.1038/nature09247
2. Lyon SM, Rossman MD. Pulmonary tuberculosis. Microbiol Spectr. 2017;5:1. doi:10.1128/microbiolspec.TNMI7-0032-2016
3. Zhang, Y., Wang Xl, Feng T, Fang Cz. Analysis of spatial-temporal distribution and influencing factors of pulmonary tuberculosis in China, during 2008–2015. Epidemiol Infect. 2018;10:1–9.
4. Li T, Zhang H, Shewade HD, Soe KT, Wang L, Du X. Patient and health system delays before registration among migrant patients with tuberculosis who were transferred out in China. BMC Health Serv Res. 2018;18(1):786. doi:10.1186/s12913-018-3583-y
5. Davies FL, Niward K, Hu Y, et al. Plasma concentrations of second-line antituberculosis drugs in relation to minimum inhibitory concentrations in multidrug-resistant tuberculosis patients in China: a study protocol of a prospective observational cohort study. BMJ Open. 2018;8(9):e023899. doi:10.1136/bmjopen-2018-023899
6. Kadhiravan T. Adherence and acquired drug-resistance in tuberculosis: wisdom stood on its head. Indian J Chest Dis Allied Sci. 2013;55(1):9–10.
7. Kidenya BR, Mshana SE, Gerwing-Adima L, Kidola J, Kasang C. Drug adherence and efficacy of smear microscopy in the diagnosis of pulmonary tuberculosis after 2 months of medication in North-western Tanzania. Int J Infect Dis. 2017;63:43–47. doi:10.1016/j.ijid.2017.07.025
8. Cadosch D, Guerrero P, Briscoe J, Page KM. The role of adherence and retreatment in De Novo emergence of MDR-TB. PLoS Comput Biol. 2016;12(3):e1004749. doi:10.1371/journal.pcbi.1005154
9. Seung KJ, Keshavjee S, Rich ML, Tuberculosis M-R. Extensively drug-resistant tuberculosis. Cold Spring Harb Perspect Med. 2015;5(9):a017863. doi:10.1101/cshperspect.a017863
10. Hirpa S, Medhin G, Girma B, et al. Determinants of multidrug-resistant tuberculosis in patients who underwent first-line treatment in Addis Ababa: a case control study. BMC Public Health. 2013;13:782. doi:10.1186/1471-2458-13-782
11. DiStefano MJ, Schmidt H. mHealth for tuberculosis treatment adherence: a framework to guide ethical planning, implementation, and evaluation. Glob Health Sci Pract. 2016;4(2):211–221. doi:10.9745/GHSP-D-16-00018
12. Gebremariam MK, Bjune GA, Frich JC. Barriers and facilitators of adherence to TB treatment in patients on concomitant TB and HIV treatment: a qualitative study. BMC Public Health. 2010;10:651. doi:10.1186/1471-2458-10-651
13. Kebede A, Wabe NT. Medication adherence and its determinants among patients on concomitant tuberculosis and antiretroviral therapy in South west ethiopia. N Am J Med Sci. 2012;4(2):67–71. doi:10.4103/1947-2714.93376
14. Metcalfe JZ, O’Donnell MR, Bangsberg DR. Moving beyond directly observed therapy for tuberculosis. PLoS Med. 2015;12(9):e1001877. doi:10.1371/journal.pmed.1001809
15. Wei X-L, Yin J, Zou G-Y, et al. Treatment interruption and directly observed treatment of multidrug-resistant tuberculosis patients in China. Int J Tuberc Lung Dis. 2015;19(4):413–419. doi:10.5588/ijtld.14.0485
16. Choowong J, Tillgren P, Söderbäck M. Thai people living with tuberculosis and how they adhere to treatment: a grounded theory study. Nurs Health Sci. 2017;19(4):436–443. doi:10.1111/nhs.12362
17. Yin J, Wang X, Zhou L, Wei X. The relationship between social support, treatment interruption and treatment outcome in patients with multidrug-resistant tuberculosis in China: a mixed-methods study. Trop Med Int Health. 2018;23(6):668–677. doi:10.1111/tmi.13066
18. Shargie EB, Lindtjorn B. Determinants of treatment adherence among smear-positive pulmonary tuberculosis patients in Southern Ethiopia. PLoS Med. 2007;4(2):e37. doi:10.1371/journal.pmed.0040037
19. DiMatteo MR, Haskard KB, Williams SL. Health beliefs, disease severity, and patient adherence: a meta-analysis. Med Care. 2007;45(6):521–528. doi:10.1097/MLR.0b013e318032937e
20. Long Q, Smith H, Zhang T, Tang S, Garner P. Patient medical costs for tuberculosis treatment and impact on adherence in China: a systematic review. BMC Public Health. 2011;11:393. doi:10.1186/1471-2458-11-393
21. Wares DF, Singh S, Acharya AK, Dangi R. Non-adherence to tuberculosis treatment in the eastern Tarai of Nepal. Int J Tuberc Lung Dis. 2003;7(4):327–335.
22. Jaiswal A, Singh V, Ogden JA, et al. Adherence to tuberculosis treatment: lessons from the urban setting of Delhi, India. Trop Med Int Health. 2003;8(7):625–633.
23. Sun Q, Meng Q, Yip W, Yin X, Li H. DOT in rural China: experience from a case study in Shandong Province, China. Int J Tuberc Lung Dis. 2008;12(6):625–630.
24. Hu D, Liu X, Chen J, et al. Direct observation and adherence to tuberculosis treatment in Chongqing, China: a descriptive study. Health Policy Plan. 2008;23(1):43–55. doi:10.1093/heapol/czm038
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
