Back to Journals » Journal of Pain Research » Volume 12
Factors associated with waiting times for persons with rheumatic conditions in multidisciplinary pain treatment facilities
Authors Deslauriers S, Roy JS, Bernatsky S , Feldman DE, Pinard AM, Desmeules F, Fitzcharles MA, Perreault K
Received 23 February 2019
Accepted for publication 29 May 2019
Published 30 July 2019 Volume 2019:12 Pages 2379—2390
DOI https://doi.org/10.2147/JPR.S206519
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Michael A Ueberall
Simon Deslauriers,1,2 Jean-Sébastien Roy,1,2 Sasha Bernatsky,3–5 Debbie E Feldman,6–8 Anne Marie Pinard,1,2,9 François Desmeules,6,10 Mary-Ann Fitzcharles,3,4 Kadija Perreault1,2
1Center for Interdisciplinary Research in Rehabilitation and Social Integration (CIRRIS), Québec, QC, Canada; 2Faculty of Medicine, Université Laval, Québec, QC, Canada; 3McGill University Health Centre (MUHC), Montréal, QC, Canada; 4Faculty of Medicine, McGill University, Montréal, QC, Canada; 5Research Institute of the McGill University Health Centre (RI-MUHC), Montréal, QC, Canada; 6Faculty of Medicine, Université de Montréal, Montréal, QC, Canada; 7Centre for Interdisciplinary Research in Rehabilitation of Greater Montreal (CRIR), Montréal, QC, Canada; 8Public Health Research Institute of Université de Montréal, Montréal, QC, Canada; 9Centre Hospitalier Universitaire (CHU) de Québec, Québec, QC, Canada; 10Maisonneuve-Rosemont Hospital (CRHMR) Research Center, Montréal, QC, Canada
Objectives: Access to multidisciplinary pain treatment facilities (MPTF) in Canada is limited by long waiting lists. However, little is known about the factors associated with access to MPTF specifically for persons with rheumatic conditions. This study aimed to 1) determine the waiting time for services in publicly funded MPTF for persons with rheumatic conditions in the province of Quebec, Canada, as well as 2) identify the factors associated with waiting time.
Methods: This study was conducted using the Quebec Pain Registry, a large database of patients who received pain management services in MPTF. Sociodemographic and clinical variables were assessed for potential associations with waiting time. Descriptive, bivariate analyses and multiple linear regression analyses were conducted.
Results: A total of 3,665 patients with rheumatic conditions were identified within the registry. Patients had a mean age of 55±14 years and the majority were women (65.7%). The average waiting time was 241.2±308.9 days (median=126), with 34.2% of the patients waiting longer than 6 months before having a first appointment. Results indicate that longer pain duration, lower household income, pain onset following a motor vehicle accident, having fibromyalgia, being on permanent disability or unemployed and being referred by a family physician (versus specialist) were significantly associated with longer waiting times.
Conclusions: Many patients with rheumatic conditions (especially fibromyalgia) face long delays before receiving services in Quebec’s MPTF. This study identified several factors associated with waiting time and emphasizes the need to improve access to pain management services.
Keywords: access, waiting time, rheumatic conditions, chronic pain, multidisciplinary pain treatment facilities
Introduction
Arthritis and other rheumatic conditions are an increasingly prevalent cause of disability worldwide and result in a substantial individual and societal burden.1,2 In North American and European countries, over 20% of the population has arthritis or another rheumatic condition.2,3 These conditions encompass a large variety of diseases and syndromes that are frequently characterized by pain and disability.4 Rheumatic conditions may be related to autoimmune disorders (eg, rheumatoid arthritis), be predominantly inflammatory (eg, gout), degenerative (eg, osteoarthritis) or be characterized by widespread body pain (eg, fibromyalgia).4
Pain is the main symptom reported by persons with rheumatic conditions,5 with a quarter reporting frequent and severe joint pain.6 Chronic pain, defined as a pain lasting three months or longer, is regarded as a distinct disorder in itself, in part because of the central pain mechanisms often involved in chronic pain.7 Multimodal pain management programs that include medical, physical and psychological interventions are often recommended for the treatment of chronic pain. In chronic pain conditions, they have been shown to reduce health care utilization and costs as well as opioid use.8,9 These programs have proven effective for patients with fibromyalgia and osteoarthritis by improving pain, fatigue, depressed mood, health-related quality of life, self-efficacy and physical fitness.10,11 These programs are often delivered in multidisciplinary pain treatment facilities (MPTF), where various health professionals provide coordinated and patient-centered treatments aimed at reducing pain and disability while empowering patients and improving their quality of life.
Unfortunately, barriers in access to chronic pain treatment in MPTF have been reported in multiple countries around the world.12–14 Results from a survey of MPTF conducted in 2006 in Canada, where the majority of MPTF are publicly funded, indicated waiting times for patients with any chronic pain condition extending over 6 months in 50% of the facilities.12 Long waiting times are recognized as the main barrier to MPTF referral by family physicians.15 In addition, long delays to access services in MPTF may affect a patient’s condition. A systematic review by Lynch et al concluded that a delay of six months or more before receiving chronic pain treatment was associated with a worsening of health-related quality of life and psychological symptoms for patients with various chronic pain conditions.16 Another study found a small deterioration in psychological symptoms during a waiting period of three months,17 as well as a high financial burden for patients on MPTF waiting lists.18 However, these studies on MPTF waiting lists did not focus specifically on patients with rheumatic conditions.
Considering the lack of research investigating access to services in MPTF specifically for patients with rheumatic conditions, along with the high prevalence and substantial burden associated with these conditions, this topic warrants attention. Moreover, identifying the characteristics of patients who wait longer before receiving multidisciplinary pain treatments may inform decisions on resource allocation and prioritization strategies. Accordingly, the objectives of this study were 1) to determine the waiting time to access services in publicly funded MPTF for persons with rheumatic conditions in the province of Quebec, Canada, as well as 2) to identify sociodemographic and clinical factors associated with waiting time.
Methods
Data source
This study was conducted using the data from the Quebec Pain Registry (QPR), a large research database of patients with chronic non-cancer pain who received services within five university-affiliated MPTF in Quebec, Canada’s second most populous province. The sociodemographic and clinical data were collected from 2008 to 2014 via a self-administered questionnaire, a structured interview with a research nurse and a physician assessment. Consecutive ambulatory patients aged 18 years and over were enrolled in the QPR database when they were scheduled for a first visit at one of the five participating MPTF. Patients were excluded if they were unable to understand written and spoken French or English or unable to participate due to severe physical or cognitive impairments. A more detailed description of the QPR, including data collection procedures, is available elsewhere.19
Study population and selection process
The National Arthritis Data Workgroup (NADW) case definition of rheumatic conditions was used.20 The NADW definition lists a set of arthritis diagnostic codes from the 9th edition of the International Classification of Diseases (ICD-9-CM)20 that the Centers for Disease Control and Prevention divided into ten distinct categories: rheumatoid arthritis; fibromyalgia, myalgia and myositis; osteoarthritis and allied disorders; spondylarthropathy; gout and other crystal arthropathies; diffuse connective tissue disease (eg, systemic lupus erythematosus); carpal tunnel syndrome; soft tissue disorders, excluding back; joint pain, effusion and other unspecified joint disorders; other specified rheumatic conditions (see Additional file 1 for the list of NADW ICD-9-CM diagnostic codes).21 This case definition is recommended for research at the health care system level.22
Patients with rheumatic conditions were identified within the QPR as those having either 1) received a diagnosis corresponding to a NADW rheumatic condition by the referring or MPTF's physician, 2) self-reported a comorbidity corresponding to a NADW rheumatic condition or 3) reported a pain onset caused by a NADW rheumatic condition (eg, pain onset due to ankylosing spondylitis). This combination of physician-diagnosed and self-reported rheumatic conditions aimed to include all patients with such conditions.
Variables
For objectives 1 and 2, waiting time was defined as the number of days between the receipt of the referral at the MPTF and the initial visit to the MPTF. To answer objective 2, various sociodemographic and clinical variables available in the QPR were assessed for their association with waiting time, based on the results of previous studies on access to care in different contexts as well as the Andersen’s behavioral model of health care utilization (Table 1).23 This well-accepted theoretical model conceptualizes individual and contextual determinants of health care utilization that help understand how and why individuals access health services.23 Thus, access to and utilization of services are explained by various predisposing characteristics, enabling resources and the need for health services.23
 |
Table 1 Potential factors associated with waiting time, based on the Andersen’s behavioral model of health care utilization |
Statistical analyses
Data were checked for deviations from normal distribution, and a log 10 transformation was computed for positively skewed variables to improve skewness and kurtosis. Controlling for the effects of the hospitals or clinics in which data are collected is critical to identify factors associated with waiting time. Thus, in order to control for the variability of waiting time between the five MPTF, the waiting time variable was standardized using z-scores. More specifically, a z-score was calculated for each patient from clinic A using the mean waiting time and standard deviation of clinic A; this procedure was repeated for patients of each clinic.
In order to explore the association between factors and waiting time, bivariate analyses were conducted with the transformed waiting time variable as the dependent variable. Because even negligible differences can reach statistical significance in large datasets, we considered the effect size in addition to the statistical significance as criteria for inclusion in the multiple regression analysis. Thus, variables significantly associated with waiting time (p<0.05) in bivariate analyses and with a minimum effect size of either Hedges’ g>0.2, eta-squared (η2)>0.01 or R-squared>0.02 (depending on the type of variable) were included in the multiple regression analysis. To account for potential changes in waiting time over the years, the association between waiting time and the date of the first visit to the MPTF was also tested in bivariate analyses. This potential control variable was included in the regression analysis if it met the previously mentioned criteria of statistical significance and effect size. A standard multiple linear regression was computed by entering all independent variables in the regression at once without any backward deletion of variables.24 In order to limit the number of dummy variables entered in the regression analysis, categories for certain ordinal variables (eg, household income) were merged based on recursive partitioning analyses that indicated optimal cutoffs. For nominal variables with multiple categories (eg, pain onset, principal source of income, employment status), ANOVA’s post-hoc analyses were used to select relevant categories (those with significant differences with other categories) to include as dummy variables in the regression. The pairwise deletion technique was used to handle missing data. Variance inflation factor scores were checked to avoid multicollinearity. Assumptions of normality, linearity and homoscedasticity of residuals were also verified.24 The bootstrapping resampling procedure (15,000 samples) was applied to test the regression model stability.24 All statistical analyses were computed using SPSS Statistics™ v25.0 (SPSS Inc., Chicago, IL, USA).
Results
Study sample
Among the 8,402 Quebec Pain Registry patients, 3,665 patients (43.6%) were identified as having a NADW rheumatic condition (self-reported and/or diagnosed by a physician) and were included in the study; 62.5% of them were included based on a physician diagnosis and the rest were included based on self-report. The participants’ sociodemographic characteristics are summarized in Table 2. Patients had a mean age of 55±14 years and the majority were women (65.7%), Caucasian (92.7%) and married or living in common law (55.7%). Twenty percent were on permanent disability and 45.2% had an annual household income of less than $35,000 CDN.
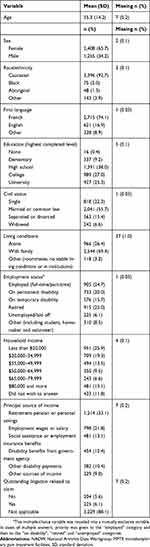 |
Table 2 Sociodemographic characteristics of patients with NADW rheumatic conditions in MPTF (n=3665) |
The clinical characteristics of patients are presented in Table 3. Patients had a mean pain duration of 7.4±9.0 years (mean±standard deviation) and a median of 4.0 years (interquartile range=2–10). A substantial proportion of patients self-reported a diagnosis of depression (45.4%) or anxiety (41.1%). Thirty-four percent of patients waited longer than 6 months before having a first appointment at an MPTF and 62.3% waited longer than 2 months. There were 435 patients with missing waiting time data; this group did not differ from the rest of the sample in terms of age, sex, diagnosis, pain duration and type of referring physicians (p>0.05).
 |
Table 3 Clinical characteristics of patients with NADW rheumatic conditions in MPTF (n=3665) |
For the overall sample of patients with NADW rheumatic conditions, the mean waiting time was 241.2±308.9 days (median=126; interquartile range=50–297) (Table 4). Patients with fibromyalgia (with or without other rheumatic conditions) represented 38.1% of the sample. The proportions of patients with rheumatoid arthritis only or osteoarthritis only were 1.3% and 21.0%, respectively.
 |
Table 4 Waiting time to access services in MPTF based on presentation of rheumatic conditions (NADW diagnostic categories) |
Determinants of waiting time
For bivariate and regression analyses, two positively skewed variables (waiting time and pain duration) were log transformed. As previously described, the log-transformed waiting time was then standardized based on the mean and standard deviation of each MPTF. Based on bivariate analysis, seven variables were retained for the regression analysis (Table 5). Of these seven variables entered in the standard multiple regression, six remained significantly positively associated with waiting time: longer pain duration, lower household income, pain onset following a motor vehicle accident, having fibromyalgia, being on permanent disability or unemployed and being referred by a family physician. The standard multiple regression resulted in a multiple R of 0.308 (F (8, 2797)=36.569; p<0.001) and an R2 of 0.095.
 |
Table 5 Factors associated with waiting time: results of the standard multiple regressiona |
Discussion
This study examined access to services in MPTF for persons with NADW rheumatic conditions and identified several significant sociodemographic and clinical factors associated with waiting time. A considerable proportion (44%) of patients receiving services in MPTF had a NADW rheumatic condition (self-reported or physician-diagnosed). Most of these patients had to wait a long period of time to access services in MPTF, with a third of them waiting over 6 months. This is consistent with the findings of another study conducted with patient data from the Quebec Pain Registry, which found a proportion of 35% of the patients waiting more than 6 months before their initial MPTF visit.19 That study included patients with all types of pain conditions, suggesting that the average waiting time for patients with rheumatic conditions may be relatively similar to that of other conditions. As waiting time data for patients with non-rheumatic condition was not available in our study, further comparison between patients with or without rheumatic conditions was not possible.
In our study, the median waiting time was just over 4 months, slightly shorter than the median waiting time of 6 months reported for Canadian MPTF (for any chronic pain condition) in 2006.12 However, the differences in populations, settings and methodology (Peng et al used a survey methodology) prevent direct comparison between the two studies.
Nevertheless, these delays considerably exceed the International Association for the Study of Pain’s benchmarks for chronic pain treatment, which recommend a 1-month delay for urgent or semi-urgent conditions and 2 months for routine conditions.25 Sixty-two percent of our sample did not meet this recommendation. As a result of waiting for chronic pain treatment, patients may experience a deterioration of their health-related quality of life and psychological well-being.16,17
Other studies from Canada, Europe and Australia report long waiting times for rheumatology care,26 for rehabilitation services for persons with rheumatic conditions27 and for pain management services for persons with chronic pain conditions.13,14 Many authors have suggested improving triage processes and increasing supply of services to meet the growing demand for pain services.14 Strategies targeting referral prioritization processes and addressing waiting list bottlenecks are warranted. Another potential avenue for improvement is to increase access to multidisciplinary teams able to manage chronic pain conditions within rheumatology departments or at the primary care level, which could be better suited for patients with rheumatic conditions who may not need highly specialized pain interventions.28 Supporting primary care physicians and rheumatologists by providing prompt recommendations and advice from chronic pain specialists is another strategy to consider.29 The use of technology and social media (eg, online support groups, pain management videos and blogs)30 as well as self-management interventions31 have also raised interest as innovative ways to reduce patients’ burden while waiting for MPTF.
The variables identified in the multiple regression analysis accounted for only 9.5% of the variance of the waiting time, reflecting the importance of other potential organizational factors that were not available in our study, such as prioritization processes and eligibility criteria. MPTF prioritization processes are reported to vary between facilities and include different prioritization criteria such as pain characteristics and psychological status.32 Eligibility criteria may also influence waiting times by limiting the number of referrals. For example, after recent changes in eligibility criteria in one of the included MPTF, patients with fibromyalgia are no longer eligible for treatment and are redirected for management in primary care. This practice, however, may not reflect the current situation in other pain clinics. Other organizational factors potentially associated with waiting time include the volume of referrals received and the volume of patients seen at the MPTF32 as well as the type of setting (university-affiliated versus district hospitals) in the case of orthopedic surgery.33 Had they been available, such data would likely have accounted for an additional percentage of the variance of the waiting time.
Nevertheless, the multiple regression analysis identified several factors associated with waiting time pertaining to the different categories of determinants described in the Andersen’s model.23 As opposed to other studies conducted on access and health care utilization with the Andersen’s model,34 no predisposing characteristic of patients with rheumatic conditions was associated with waiting time. However, several factors related to enabling resources were significantly associated with waiting time. Patients who were on permanent disability or unemployed waited longer than patients with other employment status (ie, employed, retired, temporary disability, other). This is consistent with the results of other studies on waiting time for specialty care or elective surgery33,35 and may be explained by an explicit or an implicit prioritization criterion being the potential for return to work. Another factor associated with waiting time was the type of referring physician, with patients referred to MPTF by a family physician waiting longer compared to those referred by medical specialists. This may reflect the need to improve the care pathway from primary care to specialized pain management services. The impact of physicians’ characteristics on health services access has also been noted by other researchers.36 For example, physicians’ gender, age and location have been associated with waiting time for specific medical specialties in Ontario.36
Household income was another enabling resource significantly associated with waiting time; lower income patients waited longer before their first visit to the MPTF. This finding is in line with that of other studies reporting barriers in access to various health services for persons of lower socio-economic status, even in publicly funded health systems.37,38 Underlying explanations of this finding may involve potential implicit biases in the prioritization of referrals regarding socio-economic status.39 This might also be partially explained by the association between lower rate of attendance and lower socio-economic status found in previous studies.40 Other studies, however, suggest income is not associated with waiting time.41,42 The differences in type of health services (eg, surgery, rehabilitation, medical specialist consultation), settings (eg, outpatient or inpatient hospital departments, primary care setting) and study methodologies make comparisons between studies difficult to interpret. Nonetheless, the possible inequity of access to services in MPTF based on income raises important ethical issues, especially if it has an impact on health outcomes.43 In a study by Harrington et al on access to medical specialists, persons with lower income were significantly more likely to report that their life had been affected by the waiting time compared to higher-income individuals.44 The World Health Organization advocates that equitable access to services is a key principle of universal health coverage.45
The need for health care is also considered to have an influence on access and health care utilization. Need factors associated with longer waiting time included presenting a fibromyalgia condition, having a longer duration of pain and having a pain onset following a motor vehicle accident. Qian et al46 also found a trend towards shorter rheumatology waiting times for patients with inflammatory arthritis such as rheumatoid arthritis compared to conditions such as fibromyalgia. Patients with fibromyalgia represent more than a third of our sample, similar to the proportion found in a previous study,47 in which 43% of the patients with rheumatic conditions referred to an MPTF in Quebec had a diagnosis of fibromyalgia. This large number of patients with fibromyalgia may illustrate the challenges in treating this condition in primary or secondary care, leading to frequent MPTF referrals. Regarding the duration of pain, other studies also reported longer waiting times to access health services for patients with more chronic musculoskeletal conditions.48,49 As for the pain onset following a motor vehicle accident, we did not find any literature to support this finding.
Limitations
This study has some limitations. First, our analyses were limited to the data available. As previously mentioned, it is possible that unavailable variables such as the pain characteristics at the time of referral, the volume of referrals in each MPTF or the prioritization processes could have been associated with waiting time. It would be interesting for future studies to conduct a complete assessment of the patients at the time of referral and also take into account organizational factors (volume of referrals, staff composition, etc.) pertaining to each MPTF. Second, the procedure we used to select patients with rheumatic conditions was not limited to the primary diagnosis and most likely included some patients with rheumatic conditions who were primarily referred for a non-rheumatic condition, which could have affected the waiting times for those patients. In the absence of consensus in the literature, we opted for a procedure that would favor a higher sensitivity (likely at the expense of specificity) by selecting patients based on any diagnoses, self-reported comorbidities and pain onsets that matched the NADW case definition. Despite its limitation, self-reported diagnosis is often used in health services research to identify patients from an administrative database.50 The NADW case definition was also retained for this study because it had the highest sensitivity compared to two other ICD-9-CM-based definitions of rheumatic conditions,50 which allowed to maximize case detection. Third, the number of missing data, especially for the waiting time variable, may have altered the analysis. However, no differences were found in the main sociodemographic and clinical variables between the group with missing waiting time data and the rest of the sample. Lastly, our study is subject to limitations inherent to most patient registry studies, including potential inaccuracy of self-reported data, coding errors or inconsistency in the data collection procedures.
Conclusion
Patients with NADW rheumatic conditions face long delays before accessing services in MPTF, during which their condition may deteriorate. Although a substantial amount of the variance in waiting time remains unexplained, this study identified various factors associated with waiting time. Some of the findings, notably that persons with lower household income waited longer before the initial visit, raise important issues. Longer waiting times for patients referred by a family physician suggest the need to improve the care pathway from primary care to specialized pain management services. In addition, improvement in the provision of services for patients with fibromyalgia seems necessary considering they represent a large proportion of patients referred to MPTF and that they wait a longer period of time before receiving services. Research on service provision and health care trajectory for patients with fibromyalgia from primary to tertiary care is warranted. Finally, the results of this study clearly indicate the magnitude of the challenge for persons with NADW rheumatic conditions to receive services in MPTF and emphasize the need for strategies to improve equitable and timely access to services, including better resource allocation, waiting list management and prioritization of referrals.
Ethics approval
Ethics approval for this study was obtained from the Institut de réadaptation en déficience physique de Québec (IRDPQ) Ethics Committee (#EMP-2015-449). Consent to participate was initially obtained upon enrollment in the Quebec Pain Registry and the current study did not require additional consent.
Acknowledgments
The research team sincerely thanks Jean Leblond for his guidance in conducting the statistical analyses as well as Éliane Morissette for her contribution to the study. SD received PhD salary awards from the Arthritis Society, the Ordre professionnel de la physiothérapie du Québec, the Fonds de recherche du Québec Santé (FRQS) and the Canadian MSK Rehab Research Network. This work was supported by the Canadian Initiative for Outcomes in Rheumatology Care (CIORA) grant from the Canadian Rheumatology Association.
Disclosure
Dr Anne Marie Pinard reports grants from Medisca, personal fees from Allergan and Paladin Labs, speaker fees from Purdue Pharma, Allergan and Paladins Labs outside the submitted work and has served as a member of the external advisory board to Purdue Pharma and Paladin Labs. The authors report no other conflicts of interest in this work.
References
1. 'Vos T, Allen C, Arora M, Barber RM, Bhutta ZA, Brown A, Carter A, Casey DC, Charlson FJ, Chen AZ, Coggeshall M. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015. a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1545–1602.
2. Barbour KE, Helmick CG, Boring M, Brady TJ. Vital signs: prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation - United States, 2013–2015. MMWR Morb Mortal Wkly Rep. 2017;66(9):246–253. doi:10.15585/mmwr.mm6609e1
3. Reis C, Viana Queiroz M. Prevalence of self-reported rheumatic diseases in a Portuguese population. Acta Reumatol Port. 2014;39(1):54–59.
4. van der Heijde D, Daikh DI, Betteridge N, et al. Common language description of the term rheumatic and musculoskeletal diseases (RMDs) for use in communication with the lay public, healthcare providers and other stakeholders endorsed by the European League Against Rheumatism (EULAR) and the American College of Rheumatology (ACR). Ann Rheum Dis. 2018;77(6):829–832. doi:10.1136/annrheumdis-2017-212565
5. Sarzi-Puttini P, Atzeni F, Clauw DJ, Perrot S. The impact of pain on systemic rheumatic diseases. Best Pract Res Clin Rheumatol. 2015;29(1):1–5. doi:10.1016/j.berh.2015.05.004
6. Barbour KE. Prevalence of severe joint pain among adults with doctor-diagnosed arthritis—United States, 2002–2014. MMWR Morb Mortal Wkly Rep. 2016;65(39):1052–1056.
7. Phillips K, Clauw DJ. Central pain mechanisms in the rheumatic diseases: future directions. Arthritis Rheum. 2013;65(2):291–302. doi:10.1002/art.37739
8. Hooten WM, Townsend CO, Sletten CD, Bruce BK, Rome JD. Treatment outcomes after multidisciplinary pain rehabilitation with analgesic medication withdrawal for patients with fibromyalgia. Pain Med. 2007;8(1):8–16. doi:10.1111/j.1526-4637.2007.00253.x
9. Sletten CD, Kurklinsky S, Chinburapa V, Ghazi S. Economic analysis of a comprehensive pain rehabilitation program: a collaboration between Florida Blue and Mayo Clinic Florida. Pain Med. 2015;16(5):898–904. doi:10.1111/pme.12679
10. Hauser W, Bernardy K, Arnold B, Offenbacher M, Schiltenwolf M. Efficacy of multicomponent treatment in fibromyalgia syndrome: a meta-analysis of randomized controlled clinical trials. Arthritis Rheum. 2009;61(2):216–224. doi:10.1002/art.24276
11. Finney A, Healey E, Jordan JL, Ryan S, Dziedzic KS. Multidisciplinary approaches to managing osteoarthritis in multiple joint sites: a systematic review. BMC Musculoskelet Disord. 2016;17:266. doi:10.1186/s12891-016-1134-4
12. Peng P, Choiniere M, Dion D, et al. Challenges in accessing multidisciplinary pain treatment facilities in Canada. Can J Anaesth. 2007;54(12):977–984. doi:10.1007/BF03016631
13. Hogg MN, Gibson S, Helou A, DeGabriele J, Farrell MJ. Waiting in pain: a systematic investigation into the provision of persistent pain services in Australia. Med J Aust. 2012;196(6):386–390.
14. Siddiqui Q, Rangaswamy G. Waiting times for access to a UK multidisciplinary chronic pain service: how do we comply with IASP recommendations? Pain News Br Pain Soc. 2013;11(4):239–241.
15. Lakha SF, Yegneswaran B, Furlan JC, Legnini V, Nicholson K, Mailis-Gagnon A. Referring patients with chronic noncancer pain to pain clinics: survey of Ontario family physicians. Can Fam Physician. 2011;57(3):e106–e112.
16. Lynch ME, Campbell F, Clark AJ, et al. A systematic review of the effect of waiting for treatment for chronic pain. Pain. 2008;136(1–2):97–116. doi:10.1016/j.pain.2007.06.018
17. Choiniere M, Dion D, Peng P, et al. The Canadian STOP-PAIN project - Part 1: who are the patients on the waitlists of multidisciplinary pain treatment facilities? Can J Anaesth. 2010;57(6):539–548. doi:10.1007/s12630-010-9305-5
18. Guerriere DN, Choiniere M, Dion D, et al. The Canadian STOP-PAIN project - Part 2: what is the cost of pain for patients on waitlists of multidisciplinary pain treatment facilities? Can J Anaesth. 2010;57(6):549–558. doi:10.1007/s12630-010-9306-4
19. Choiniere M, Ware MA, Page MG, et al. Development and implementation of a registry of patients attending multidisciplinary pain treatment clinics: the quebec pain registry. Pain Res Manage. 2017;2017:8123812. doi:10.1155/2017/8123812
20. Helmick CG, Lawrence RC, Pollard RA, Lloyd E, Heyse SP. Arthritis and other rheumatic conditions: who is affected now, who will be affected later? National Arthritis Data Workgroup. Arthritis Care Res. 1995;8(4):203–211.
21. Centers for Disease Control and Prevention. National Arthritis Data Workgroup ICD-9-CM diagnostic codes for arthritis and other rheumatic conditions; 2017. Available from: http://www.cdc.gov/arthritis/data_statistics/pdf/arthritis_codes_2004.pdf.
22. Helmick CG; United States Bone and Joint Initiative. Arthritis - definitions. Available from: http://www.boneandjointburden.org/2014-report/iva0/definitions.
23. Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10.
24. Tabachnick BG, Fidell LS. Using Multivariate Statistics.
25. International Association for the Study of Pain. Task force on wait-times. Summary and recommendations; 2017. Available from: http://www.iasp-pain.org/files/Content/NavigationMenu/EducationalResources/IASP_Wait_Times.pdf.
26. Widdifield J, Bernatsky S, Thorne JC, et al. Wait times to rheumatology care for patients with rheumatic diseases: a data linkage study of primary care electronic medical records and administrative data. CMAJ Open. 2016;4(2):E205–E212. doi:10.9778/cmajo.20150116
27. Delaurier A, Bernatsky S, Raymond MH, Feldman DE. Wait times for physical and occupational therapy in the public system for people with arthritis in quebec. Physiother Can Physiotherapie Canada. 2013;65(3):238–243. doi:10.3138/ptc.2011-62
28. Peterson K, Anderson J, Bourne D, Mackey K, Helfand M. Effectiveness of models used to deliver multimodal care for chronic musculoskeletal pain: a rapid evidence review. J Gen Intern Med. 2018;33(Suppl 1):71–81. doi:10.1007/s11606-018-4328-7
29. Liddy C, Smyth C, Poulin PA, Joschko J, Sheppard M, Keely E. Supporting better access to chronic pain specialists: the champlain BASE() eConsult service. J Am Board Fam Med. 2017;30(6):766–774. doi:10.3122/jabfm.2017.06.170170
30. Merolli M, Gray K, Martin-Sanchez F. Patient participation in chronic pain management through social media: a clinical study. Stud Health Technol Inform. 2016;225:577–581.
31. Lee C, Crawford C, Schoomaker E. Movement therapies for the self-management of chronic pain symptoms. Pain Med. 2014;15(Suppl 1):S40–S53. doi:10.1111/pme.12411
32. Pagé MG, Ziemianski D, Shir Y. Triage processes at multidisciplinary chronic pain clinics: an international review of current procedures. Can J Pain. 2017;1(1):94–105. doi:10.1080/24740527.2017.1331115
33. Lofvendahl S, Eckerlund I, Hansagi H, Malmqvist B, Resch S, Hanning M. Waiting for orthopaedic surgery: factors associated with waiting times and patients’ opinion. Int J Qual Health Care. 2005;17(2):133–140. doi:10.1093/intqhc/mzi012
34. Babitsch B, Gohl D, von Lengerke T. Re-revisiting Andersen’s behavioral model of health services use: a systematic review of studies from 1998–2011. Psychosoc Med. 2012;9:Doc11.
35. Clover KA, Dobbins TA, Smyth TJ, Sanson-Fisher RW. Factors associated with waiting time for surgery. Med J Aust. 1998;169(9):464–468.
36. Jaakkimainen L, Glazier R, Barnsley J, Salkeld E, Lu H, Tu K. Waiting to see the specialist: patient and provider characteristics of wait times from primary to specialty care. BMC Fam Pract. 2014;15:16. doi:10.1186/1471-2296-15-16
37. Laudicella M, Siciliani L, Cookson R. Waiting times and socioeconomic status: evidence from England. Soc Sci Med. 2012;74(9):1331–1341. doi:10.1016/j.socscimed.2011.12.049
38. Hajizadeh M. Does socioeconomic status affect lengthy wait time in Canada? Evidence from Canadian community health surveys. Eur J Health Econ. 2018;19(3):369–383. doi:10.1007/s10198-017-0889-3
39. Arpey NC, Gaglioti AH, Rosenbaum ME. How socioeconomic status affects patient perceptions of health care: a qualitative study. J Prim Care Community Health. 2017;8(3):169–175. doi:10.1177/2150131917697439
40. Ellis DA, McQueenie R, McConnachie A, Wilson P, Williamson AE. Demographic and practice factors predicting repeated non-attendance in primary care: a national retrospective cohort analysis. Lancet Public Health. 2017;2(12):e551–e559. doi:10.1016/S2468-2667(17)30217-7
41. Thind A, Stewart M, Manuel D, et al. What are wait times to see a specialist? an analysis of 26,942 referrals in southwestern Ontario. Healthc Policy. 2012;8(1):80–91.
42. Sanmartin C, Pierre F, Tremblay S. Waiting for care in Canada: findings from the health services access survey. Healthc Policy. 2006;2(2):43–51.
43. van Doorslaer E, Masseria C, Koolman X, Group OHER. Inequalities in access to medical care by income in developed countries. Cmaj. 2006;174(2):177–183. doi:10.1503/cmaj.050584
44. Harrington DW, Wilson K, Rosenberg MW. Waiting for a specialist consultation for a new condition in Ontario: impacts on patients’ lives. Healthc Policy. 2014;9(4):90–103.
45. World Health Organization. Making Fair Choices on the Path to Universal Health Coverage. Final Report of the WHO Consultative Group on Equity and Universal Health Coverage. Geneva: WHO; 2014.
46. Qian J, Ehrmann Feldman D, Bissonauth A, et al. A retrospective review of rheumatology referral wait times within a health centre in Quebec, Canada. Rheumatol Int. 2010;30(5):705–707. doi:10.1007/s00296-009-1297-5
47. Fitzcharles MA, Almahrezi A, Ware MA. Clinical profile of rheumatic disease patients referred to a multidisciplinary pain center. J Rheumatol. 2004;31(2):359–363.
48. Passalent LA, Landry MD, Cott CA. Exploring wait list prioritization and management strategies for publicly funded ambulatory rehabilitation services in ontario, canada: further evidence of barriers to access for people with chronic disease. Healthc Policy. 2010;5(4):e139–e156.
49. Quon JA, Levy AR, Sobolev B, et al. The effect of compensation status on waiting time for elective surgical lumbar discectomy. Spine. 2009;34(19):2052–2059. doi:10.1097/BRS.0b013e3181b2f233
50. Murphy LB, Cisternas MG, Greenlund KJ, Giles W, Hannan C, Helmick CG. Defining arthritis for public health surveillance: methods and estimates in four US population health surveys. Arthritis Care Res (Hoboken). 2017;69(3):356–367. doi:10.1002/acr.22943
Supplementary material
 |
Table S1 Categories of rheumatic conditions corresponding to the National Arthritis Data Workgroup (NADW) ICD-9-CM diagnostics codes |
Reference
1. Centers for Disease Control and Prevention. National Arthritis Data Workgroup ICD-9-CM diagnostic codes for arthritis and other rheumatic conditions. Atlanta, GA: CDC; 2004. Available from: http://www.cdc.gov/arthritis/data_statistics/pdf/arthritis_codes_2004.pdf. Accessed March 21, 2017.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
