Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 15
Factors Associated with Retention in HIV Care Among HIV-Positive Adolescents in Public Antiretroviral Therapy Clinics in Ibanda District, Rural South Western Uganda
Authors Nimwesiga C, Taremwa IM , Nakanjako D , Nasuuna E
Received 15 December 2022
Accepted for publication 26 February 2023
Published 4 March 2023 Volume 2023:15 Pages 71—81
DOI https://doi.org/10.2147/HIV.S401611
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Olubunmi Akindele Ogunrin
Christine Nimwesiga,1– 3 Ivan Mugisha Taremwa,3 Damalie Nakanjako,4 Esther Nasuuna2
1Uganda Nurses and Midwives Council, Ministry of Health, Kampala, Uganda; 2Infectious Diseases Institute, Kampala, Uganda; 3Institute of Allied Health Sciences, Clarke International University, Kampala, Uganda; 4College of Health Sciences, Makerere University, Kampala, Uganda
Correspondence: Christine Nimwesiga, Uganda Nurses and Midwives Council, Ministry of Health, P.O Box 4046, Kampala, Uganda, Email [email protected]
Background: Retention in antiretroviral therapy (ART) care is a key indicator of Human Immunodeficiency Virus (HIV) treatment success as it improves adherence, critical for better treatment outcomes and prevention of drug resistance. HIV treatment among adolescents living with HIV (ALHIV) is characterized by loss to follow-up, poor ART adherence, and eventual death. This study assessed retention in ART care and the associated factors among ALHIV in Ibanda district, rural South Western Uganda.
Methods: This was a retrospective cohort study using clinical data from ALHIV enrolled from 2019 to 2020 in eight health facilities in Ibanda district. Data from the Electronic Medical Record (EMR) system was extracted to assess the associated factors and participants’ status two years after enrollment. Data were analyzed using EPIdata version 3.1 in which Univariate and multivariate cox proportional hazard regression analyses were determined. A hazard ratio (HR) at a 95% confidence interval was obtained, and a P-value < 0.05 was considered statistically significant.
Results: Eighty-four ALHIV comprising 86.9% (N = 73) females were enrolled. The majority 63.1% (N = 53) resided in semi/peri-urban, and 44.0% (N = 37) stayed less than 5 km from the facility. Only 35.7% (N = 30) were active on ART, while 17 (20.2%) and 36 (42.9%) were lost to follow-up and transfer-outs, respectively. Factors associated with low retention were: ALHIV that moved 5– 10Km (HR = 5.371; 95% CI: 1.227– 23.5050, p = 0.026), used differential service delivery model was Facility-Based Group (FBG) (HR = 12.419; 95% CI: 4.034– 38.236, p < 0.001) and those enrolled on the Young Adolescent Program Support (YAPs) (HR = 4.868; 95CI:1.851– 12.803; p = 0.001). Retention reduced with increasing ART duration, ALHIV on (TDF/3TC/EFV) (p < 0.001), lived more than 10Km (p = 0.043) and did not benefit from any intervention (p < 0.001).
Conclusion: Results showed low retention in care and the urgent need to strengthen individual case management strategies for ALHIV, thus interventions focusing on peer support are desired.
Keywords: adolescents living with HIV, retention in ART care, Uganda
Background
Human Immunodeficiency Virus (HIV) is a global public health threat affecting 37.6 million people (30.2 million to 45 million) by 2020.1 Africa has a disproportionately high burden reported at 25.7 million people living with HIV.2 Uganda bears the largest burden in the East African region with a prevalence of 5.8% (range 5.4–6.2%) in 2019 among the national adults (15–49 years). The southwestern part of Uganda has a higher burden at 10.4%.3,4 Its high burden has been attributed to high-risk sexual practices, gender, economic causes, and prenatal transmission.2
Adolescents (10–19 years) make up a growing proportion of people living with HIV around the world, and the outcomes of HIV infection are worse than those of all other age groups.5 This is due to the early initiation of sexual activity, as well as a proclivity for peer pressure and a lack of problem-solving skills.6,7 Adolescents who were prenatally HIV-infected may face additional health and developmental challenges.8 The introduction of combination antiretroviral therapy (ART) has resulted in increased survival and quality of life among HIV-infected people all over the world.9 This has been made possible by the current public HIV/AIDS program, which focuses on the prevention of mother-to-child transmission (PMTCT) and treatment scale-up.10
Deaths due to AIDS have reduced after ART became widely available in Uganda.3,11 Furthermore, persistent global efforts to ensure free and widespread access to ART have been supported by the World Health Organization’s innovative modeling, which includes standard treatment combinations, regionalized facility care from higher health centers to lower health facilities, and regular laboratory monitoring.2 This pragmatic approach has increased by 84% of HIV-confirmed cases being started on ART as soon as possible (range 78–92%).9
Despite these notable achievements, inadequate retention in HIV care and adherence to ART treatment requirements are significant limitations that may jeopardize the gains that have already been made.12 Retention in ART care is a priority of HIV prevention, care, treatment, and support programs for the adolescent population, and adherence to ART is still routine for HIV care.2 Good retention is considered for best practice required to achieve (not less than 95%) HIV suppression.2,9 Poor HIV retention and ART adherence jeopardize global achievements and pose a significant challenge across multiple HIV programs. According to a study conducted by the AIDS Support Organization (TASO) in Uganda, only 65% of adolescents remained in care at the end of the fifth year, and the attrition rate increased with increasing time lapse.10
Although the causes of poor retention and ART adherence vary, they are all related to a lack of basic and essential human needs, as well as negative attitudes toward HIV-infected clients.2 Furthermore, barriers related to socioeconomic status and stigma of HIV-infected clients, as well as determinants related to the health facility, such as the availability of drug stocks, the quality of care provided, and clientele waiting time, were identified.4–7,9,10 More, factors related to the medicines have been described, such as the number of pills administered, the reported adverse effects of the drugs, and the dosage used.2,11,12 Efforts to stop the spread of HIV are increasing, necessitating a variety of measures to improve HIV diagnosis and management. The joint United Nations Programme on HIV/AIDS’ 95-95-95 approach envisions 95% of HIV-positive people being diagnosed, 95% of those being enrolled in antiretroviral therapy (ART), and 95% of those on ART achieving virological suppression by 2030.1 As Uganda works towards the 95-95-95 strategy, it is critical to investigate the level of retention in HIV care as well as the specific local associated factors. There is an urgent need to design, implement, and integrate interventions that are effective at retaining ALHIV in treatment and care by responding to their specific risks and needs. This study set out to determine the two-year retention in HIV care and to characterize predictors of attrition among ALHIV aged 10–19 years receiving ART in Ibanda district, rural South Western Uganda.
Materials and Methods
Operation Definition
In this study, we defined retention in ART care as the proportion of the infected patients who are remaining alive and are still receiving health care at study facilities after they were initiated on therapy.2,9 Patients were classified as not being on ART at the time they stopped treatment, as being lost to follow-up (LTFU), or as having died at the study facility
Study Design
A retrospective cohort study involving secondary analysis of routinely collected clinical data of adolescents aged 10–19 years. Data were collected from January 2019 to December 2020.
Study Setting
The study was carried out at eight health facilities in Ibanda district that offer ART services. They are located in both urban and peri-urban South Western Uganda and comprised a hospital (1), health centre-IV (2), and health center III (5). Ibanda district borders the districts of Mbarara to the south, Kiruhura to the East, Buhweju to the West, and Kamwenge to the North. The district has a total population of 277,300 people. The HIV/AIDS prevalence stands at 6.0%, and 8 health facilities offer ART care. The study area is a rural setting with households earning livelihood through subsistence farming.
Study Population, Selection Criteria, and Data Collection
The study recruited ALHIV aged 10 to 19 years with a confirmed HIV-positive status that was enrolled in HIV care in 2019 and followed up for retention at two years.
Study Variables
The outcome variable was the current status in HIV care of each selected participant and was determined based on the information in the ART register or patient follow-up card. It was categorized as died (of any cause), lost, dropped, stopped or retained in care. The participant was defined as “lost” if one missed his or her next clinic or pharmacy refill appointment for at least 1 month and at most 3 consecutive months. A participant was considered as “dropped” if one missed his or her planned clinic or pharmacy refill appointment for more than 3 consecutive months. A participant known to be alive and retained in care, but temporarily discontinued taking ART due to medical or personal reasons was defined as “stopped”. A participant was defined as “retained in care” if they were alive and known to be still receiving medical care at the time of the study, including those considered as “stopped”. Attrition was defined as the number of participants documented as died, lost or dropped. Both patients who were lost or dropped were considered as lost to follow up (LTFU).
The independent variables were the socio-demographic variables at enrolment in HIV care including age, sex, marital status, religion, educational level, and HIV-status disclosure. In addition, dates of HIV diagnosis, enrolment in HIV care and ART initiation, type of antiretroviral treatment regimen, and evidence of tuberculosis at or after start ART were considered. Also, WHO clinical stage, functional status, CD4 cell count, and hemoglobin level were collected from the intake form or follow-up card. The following variables were included in the analysis: time since the start of ART at study entry (“date of the last known clinic or pharmacy refill visit” minus “date of ART initiation”), and time since HIV diagnosis at start ART (“date of ART initiation” minus “date of HIV diagnosis”).
Data Extraction, Management, and Analysis
A data extraction tool was used to collect data from Electronic Medical Records (EMR).
The primary outcome of interest was the enrollment status which could be lost to follow-up (LTFU), active in HIV care, transfers out, and death which was estimated using available data in the medical records. All documented LTFU patients were considered to be “not-retained in care” and these estimates were used in the analyses to identify predictors of attrition. Deaths previously known to the ART clinic during routine follow-up care were gathered from medical records. Data were analyzed using EPIdata version 3.1 (EPIdata Association, Odense, Denmark, 2008). Cox proportional hazards regression was performed to identify the variables that predicted post-ART attrition. The Hazard Ratio (HR) in the Cox regression model estimates the relative likelihood of attrition at consecutive points in time after ART initiation. Univariate and multivariate Cox regression models were used to identify predictor variables with a p-value and variables that significantly (P-value <0.05) predicted attrition were kept in the final model. The analysis estimated the probability of retention in ART care among adolescents. Adjustments for the potential confounding and interaction effects were made, and the final model was checked for the goodness-of-fit using the Hosmer-Lemeshow test.
Results
The study enrolled 84 ALHIV. The majority 80 (95.2%) were aged 15–19 years (p = 0.614), female 73 (86.9%) (P = 0.739) and single 70 (83.3%). More than half 53 (63.1%) of the respondents were located in semi/peri-urban areas as compared to the 31 (36.9%) found in rural areas (p = 0.48). More, 29 (34.5%) of the respondents stayed less than 5km away from the health facilities unlike 37 (44.0%) and 18 (21.4%) that stayed 5–10Km and more than 10Km away from the facility (p = 0.043), as shown in Table 1.
 |
Table 1 Demographic Characteristics of Participants |
The assessment of retention showed that 30 (35.7%) were active on ART, 1 (1.2%) died, 17 (20.2%) were lost to follow up and 36 (42.9%) were transferred out, as shown in Figure 1.
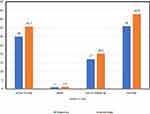 |
Figure 1 Assessment of retention in HIV care (N = 84). Shows the status of respondents’ source secondary data from the health facility. |
Factors Associated with Retention in HIV Care
Factors associated with retention in care found that 66.7% of the respondents whose ART clinic day was once a month were retained in care as compared to the 33.3% retention among those 2–3 days (p = 0.807). Majority who were in WHO stage I were retained in care (N = 82) (p = 0.535) and 93.3% among those whose regimen initiation was TDF/3TC/EFV (p = 0.024). On the other hand, 66.7% of the respondents on TDF/3TC/DTG had retention in HIV care as compared to the 30.0% among those on TDF/3TC/EFV (p < 0.001). More so, 96.7% of the respondents that had treatment supporters had retention in HIV care unlike those who did not have treatment supporters (p = 0.088). Furthermore, retention in HIV care was found at 90.0% among respondents without any medical condition, and 100% among those that tested negative for TB (p > 0.05). The differential service delivery model had a significant association with retention in HIV care (p < 0.001). Finally, 70.0% of the respondents that had psychosocial support had retention to HIV care (p = 0.107) and 100% retention was observed among those that disclosed their HIV status to either a family member or a friend (p = 0.292) and the availability of current interventions had a significant association with retention in HIV care (p < 0.001), as given in Table 2.
 |
Table 2 Client-Related Factors Associated with Retention in HIV Care N=84 |
Multivariable Cox proportion Hazard regression showed that respondents that move 5–10 km had a higher hazard/risk of retention in HIV care as compared to those that move less than 5km (HR = 5.371; 95% CI:1.227–23.5050, p = 0.026). In addition, respondents whose differential service delivery mode was FBG were 12 times retained in HIV care unlike those who were using First Track Drug Refill (FTDR) (HR = 12.419; 95% CI: 4.034–38.236, p < 0.001). More so, respondents whose intervention was Young Adolescent program support (YAPs) had four times the higher hazard of retention in HIV care unlike their counterparts in ARIEL clubs (HR=4.868; 95CI:1.851–12.803; p = 0.001), as given in Table 3.
 |
Table 3 Multivariate Analysis of Factors Associated with Retention in HIV Care Model Summary of Attrition (N = 84) |
The odds of being retained in HIV reduced with an increase in months spent on ART. For example, there was 100% retention in HIV care at the start of the study and on the other hand, some patients were censored at zero months. However, 93.9% retention was registered in the second month, 84.95% at less than five months, 77.18% at ten months, 60.78% at twenty months, and 51.28% at twenty-four months while only 32.82% of the respondents were HIV care retention after twenty-four months as shown in Figure 2.
 |
Figure 2 Retention in HIV care at varied time points in months. Shows the cumulative probability of retention in HIV care for two years. |
Discussion
Retention in care among ALHIV was 51.28% at twenty-four months and 32.82% after forty-eight months. At both intervals, the observed retention in this study is higher than the 29.3% HIV-positive adolescent retention rate at Katooke Health Center in Midwestern Uganda.13 The difference may be ascribed to the variance in the study area. The observed ART retention is however lower than the 69% reported among adolescents attending the eleven TASO clinics in rural Uganda who were initiated on ART care between January 2006 and December 2011.14 The difference is attributable to the study setting in TASO Uganda where intensive resources are geared toward HIV testing, counseling, treatment, and support services.14 This suggests that although resources for supporting ART retention may not always be available, the programs provide valuable lessons for improving access to treatment services for HIV-positive adolescents.14
The retention in ART care was directly affected by other factors including respondents being in rural areas, and distance from the health facility. Long-distance from the clinic of more than 10Km, and unavailable or expensive means of transport to the ART facility which hinders transport means as explored by other studies,6–8,13 are critical determinants of retention in care. As this study was conducted in a rural setting, these factors were prevalent and were compounded by poor terrain and unreliable means of transport.15,16
Client-related factors associated with retention in ART care were more evident among those who attended a single ART clinic day, respondents with clinical WHO stage I and having a treatment supporter. These factors are consistent with previous reports. For example, a single ART day dedicated to adolescents reduced stigma and ensured positive responses as elucidated in earlier studies.17,18 This suggests that ALHIV may present with age-specific requirements that may be addressed through a dedicated clinic day approach.6,18 Similarly, early initiation of ART as seen in WHO stages I and II improved ART adherence and reduced adverse treatment events. This drives retention in their HIV treatment programs.18,19 This factor is critical in light of the better immunological response and subsequently good virological suppression during these infection stages.14 Also, this may circumvent the HIV infection progresses to a more life-threatening AIDS disease.2,5,12 As previously indicated, the risk of adolescent non-retention in care was significantly greater among those in WHO clinical stages 3 and 4 than among those in stages 1 and 2 at month 24.14
ALHIV that had psychosocial support were retained in HIV care. Treatment supporters offer psychosocial and peer support, a phenomenon that improves ART retention.20,21 If extrapolated, this can divulge into strong bonding networks and encourage each other to ensure treatment continuity models.19
Besides, retention in HIV care was found at 90% among respondents without any medical condition, 100% among those that tested negative for TB, and without disease comorbidities (p > 0.05). The absence of other medical conditions or comorbidities improves the quality of life and ART retention.22,23 Additionally, 100% retention was observed among those that disclosed their HIV status (p = 0.292). As previously explored, disclosure of ALHIV has strong empirical support.24,25 Also, the availability of current interventions had a significant association with retention in HIV care (p < 0.001). This finding is consistent with earlier reports.26–28
The differentiated service delivery (DSD) model had a significant association with retention in HIV care (p < 0.001). The positive impact of the DSD has been explored.23 The DSD aim at taking care close to clients to improve access while also decongesting health facilities.29 This approach ensures that adolescents are apprehensive of the idea of bringing care closer to their doorsteps mainly because of the fear of stigmatization and the resultant discrimination. This could likely improve the overall outcome of ALHIV as found in earlier studies.26,30 This may reflect the indirect challenges faced in seeking care at the facility.
Respondents that moved 5–10 Km had a higher hazard/risk of retention in HIV care as compared to those that move less than 5km (HR = 5.371; 95% CI:1.227–23.5050, p = 0.026). Transportation costs and geographical distance to routine HIV clinic is a factor that is more prevalent in rural compared to urban areas and is compounded by poor terrain and a lack of transportation infrastructure.15,16 As found by this study, ALHIV who lived within a radius of 5–10Km showed a statistical association with retention in care. This finding asserts previous reports,13,16 and this affirms that a short distance costs less and is manageable to access the health facility.
More so, respondents whose intervention was YAPs had four times the higher hazard of retention in HIV care unlike their counterparts in ARIEL clubs (HR = 4.868; 95CI:1.851–12.803; p = 0.001). The Young Adolescent Program Support (YAPS) which started in 2019 is attempting to empower adolescents and young people to contribute to the reduction of HIV-related morbidity and mortality by increasing the HIV status disclosure, improving ART treatment coverage, increasing viral load suppression, and strengthening psychosocial care.5,31 Thus, YAPs present high-quality social support and age-appropriate information to ALHIV towards achieving improved health outcomes.32
The likelihood of being retained in HIV care reduces with an increase in months spent on ART. For example, there was 100% retention in HIV care at the start of the study; however, 93.9% retention was registered in the second month, 89.9% in the fourth month, 78.8% at six months, 61.3% at eight months, 43.8% at ten months while only 21.9% of the respondents were in HIV care retention at twelve months. Also, this trend corroborates well with the overall level of retention of adolescents in TASO ART programs which was reported at 96% at 6 months, 90% at 12 months, 83% at 24 months, 76% at 36 months, and 71% at 48 months.14 There is growing evidence that ALHIV (15–24 years) had 59% higher attrition than adults (25–54 years) one year after initiating ART underscoring the need to develop and test interventions to improve retention that specifically target adolescents.33 Consistent with a recent systematic review of 154 adult HIV patient cohorts in low- and middle-income countries, on average, 83% of patients were retained in HIV treatment services after 12 months on ART, but only 60% were retained after 60 months on ART.34 As countries begin to implement the WHO-recommended “Test and Treat” strategy, all individuals who test HIV positive will immediately initiate ART, substantially increasing the number of ART. The challenges of retaining patients in care will likely only amplify as the number of people living with HIV on ART increases, in the absence of effective interventions.2,3,29
Strength of the Study
The strength of this study is premised on the fact that there has been a research gap among ALHIV as no research has ever explored the determinants of ART retention among ALHIV in the study area. Also, all the ART sites are offering services to ALHIV and are located in urban, peri-urban, and rural areas which makes results generalizable.
Limitations of the Study
The results of this study ought to be interpreted in light of the following: We relied on past medical records as this was a retrospective study, and we had no control over missing data due to poor documentation. Thus, the study’s findings could have been influenced by the amount of missing data and files. Further, the type of data recorded in patients’ records is limited, preventing us from exploring deeper into certain patterns in the data, such as the unexpected variations in adolescent retention levels by year of ART initiation. Because we used a retrospective cohort study design, we had to rely on the accuracy of the health-care workers’ record-keeping. Also, we were unable to control the exposures and outcomes of interest. Also, the study was unable to assess the relationship between retention and key factors such as immunological/virologic status (CD4 count and HIV viral load measures) and the socioeconomic characteristics of ALHIV enrolled. Even so, no interviews with health-care providers, ALHIV, or caregivers were conducted to corroborate the information provided. To this, a qualitative study is critical to explore the phenomenological responses obtained from this study.
Conclusions
In this study, we found that ART retention was low, and was dependent on numerous factors. To improve retention, there is an urgent need to strengthen individual case management strategies for ALHIV, treatment, and support programs such as community drug distribution points. Also, there is a need to set up transition units to cater to those transiting from pediatric care to adolescence and assess if this could improve the retention of adolescents in HIV care and treatment programs. Another study to describe adolescent retention in care after longer periods of ART may also be helpful.
Abbreviations
ART, Antiretroviral therapy; ALHIV, Adolescents living with HIV; HIV, Human Immune deficiency virus; YAPS, Young Adolescent Program Support.
Data Sharing Statement
All relevant data are within the paper. The data abstraction tool is included as a Supplementary Material.
Ethics Approval and Consent to Participate
Ethical approval was obtained from the Infectious Diseases Institute (IDI) Research and Ethics Committee. Administrative permission was obtained from the District Health Officer, Ibanda district. Also, a waiver of consent was obtained and anonymity of data was ensured at all stages of data collection and analysis. The study complied with the Declaration of Helsinki.
Acknowledgments
We are grateful to the study participants and health-care providers at these health facilities in Ibanda district. We acknowledge the financial support from the Afya Bora fellowship to the first author.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The first author was supported by the Afya Bora fellowship grant. The funders had no role in the study design, data collection, analysis, or decision to publish.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. UNAIDS. Global HIV & AIDS statistics — fact sheet; 2020. Available from: https://www.unaids.org/en/resources/fact-sheet.
2. World Health Organization. HIV/AIDS; 2021. Available from: https://www.afro.who.int/health-topics/hivaids.
3. Elflein J. HIV/AIDS worldwide - statistics & facts; 2021. Available from: https://www.statista.com/topics/773/hiv-aids-worldwide/#dossierKeyfigures.
4. Phillips K. Review of the AVERT, a global information and education on HIV and AIDS resource. J Consum Health Internet. 2019;23(3):290–298. doi:10.1080/15398285.2019.1648162
5. Widman L, Choukas-Bradley S, Helms SW, Prinstein MJ. Adolescent susceptibility to peer influence in sexual situations. J Adolesc Health. 2016;58(3):323–329. doi:10.1016/j.jadohealth.2015.10.253
6. Kassahun EA, Gelagay AA, Muche AA, Dessie AA, Kassie BA. Factors associated with early sexual initiation among preparatory and high school youths in Woldia town, northeast Ethiopia: a cross-sectional study. BMC Public Health. 2019;19(1):1–8. doi:10.1186/s12889-019-6682-8
7. Okoboi S, Ssali L, Yansaneh AI, et al. Factors associated with long‐term antiretroviral therapy attrition among adolescents in rural Uganda: a retrospective study. J Int AIDS Soc. 2016;19:20841. doi:10.7448/IAS.19.5.20841
8. Mahy M, Marsh K, Sabin K, Wanyeki I, Daher J, Ghys PD. HIV estimates through 2018: data for decision-making. AIDS. 2019;33(Suppl 3):S203. doi:10.1097/QAD.0000000000002321
9. Nabukeera-Barungi N, Elyanu P, Asire B, et al. Adherence to antiretroviral therapy and retention in care for adolescents living with HIV from 10 districts in Uganda. BMC Infect Dis. 2015;15(1):1–10. doi:10.1186/s12879-015-1265-5
10. Larson E, Bendavid E, Tuoane-Nkhasi M, et al. Population-level associations between antiretroviral therapy scale-up and all-cause mortality in South Africa. Int J STD AIDS. 2014;25(9):636–642. doi:10.1177/0956462413515639
11. Kiragga AN, Mubiru F, Kambugu AD, Kamya MR, Castelnuovo B. A decade of antiretroviral therapy in Uganda: what are the emerging causes of death? BMC Infect Dis. 2019;19(1):1–6. doi:10.1186/s12879-019-3724-x
12. Mesic A, Halim N, MacLeod W, Haker C, Mwansa M, Biemba G. Facilitators and barriers to adherence to antiretroviral therapy and retention in care among adolescents living with HIV/AIDS in Zambia: a mixed methods study. AIDS Behav. 2019;23(9):2618–2628. doi:10.1007/s10461-019-02533-5
13. Izudi J, Mugenyi J, Mugabekazi M, et al. Retention of HIV-positive adolescents in care: a quality improvement intervention in mid-western Uganda. BioMed Res Int. 2018;2018. doi:10.1155/2018/1524016
14. Atuyambe LM, Ssegujja E, Ssali S, et al. HIV/AIDS status disclosure increases support, behavioral change and, HIV prevention in the long term: a case for an Urban Clinic, Kampala, Uganda. BMC Health Serv Res. 2014;14(1):1–11. doi:10.1186/1472-6963-14-276
15. Janssen S, Wieten RW, Stolp S, et al. Factors associated with retention to care in an HIV clinic in Gabon, Central Africa. PLoS One. 2015;10(10):e0140746. doi:10.1371/journal.pone.0140746
16. Pellowski JA. Barriers to care for rural people living with HIV: a review of domestic research and health care models. J Assoc Nurses AIDS Care. 2013;24(5):422–437. doi:10.1016/j.jana.2012.08.007
17. Geng EH, Nash D, Kambugu A, Zhang Y, Braitstein P. Retention in care among HIV-infected patients in resource-limited settings: emerging insights and new directions. Curr HIV/AIDS Rep. 2010;7(4):234–244. doi:10.1007/s11904-010-0061-5
18. Harries AD, Zachariah R, Lawn SD, Rosen S. Strategies to improve patient retention on antiretroviral therapy in Sub‐Saharan Africa. Trop Med Int Health. 2010;15:70–75. doi:10.1111/j.1365-3156.2010.02506.x
19. Chawla A, Wang C, Patton C, et al. A review of long-term toxicity of antiretroviral treatment regimens and implications for an aging population. Infect Dis Ther. 2018;7(2):183–195. doi:10.1007/s40121-018-0201-6
20. Assefa M, Abegaz WE, Shewamare A, Medhin G, Belay M. Prevalence and correlates of anemia among HIV infected patients on highly active anti-retroviral therapy at Zewditu Memorial Hospital, Ethiopia. BMC Hematol. 2015;15(1):1–8. doi:10.1186/s12878-015-0024-6
21. Penn AW, Azman H, Horvath H, et al. Supportive interventions to improve retention on ART in people with HIV in low-and middle-income countries: a systematic review. PLoS One. 2018;13(12):e0208814. doi:10.1371/journal.pone.0208814
22. Tong PD, Atuhairwe C, Taremwa IM. Differential self-reported determinants to antiretroviral therapy adherence: findings from caregivers of children under five years living with human immunodeficiency virus infection attending Al-Sabah Hospital, South Sudan. HIV/AIDS. 2020;12:175.
23. Wadunde I, Tuhebwe D, Ediau M, Okure G, Mpimbaza A, Wanyenze RK. Factors associated with adherence to antiretroviral therapy among HIV infected children in Kabale district, Uganda: a cross sectional study. BMC Res Notes. 2018;11(1):1–6. doi:10.1186/s13104-018-3575-3
24. Jobanputra K, Parker LA, Azih C, et al. Factors associated with virological failure and suppression after enhanced adherence counseling, in children, adolescents, and adults on antiretroviral therapy for HIV in Swaziland. PLoS One. 2015;10(2):e0116144. doi:10.1371/journal.pone.0116144
25. Nyogea D, Mtenga S, Henning L, et al. Determinants of antiretroviral adherence among HIV positive children and teenagers in rural Tanzania: a mixed methods study. BMC Infect Dis. 2015;15(1):1–13. doi:10.1186/s12879-015-0753-y
26. Mutwa PR, Van Nuil JI, Asiimwe-Kateera B, et al. Living situation affects adherence to combination antiretroviral therapy in HIV-infected adolescents in Rwanda: a qualitative study. PLoS One. 2013;8(4):e60073. doi:10.1371/journal.pone.0060073
27. Rudy BJ, Murphy DA, Harris DR, Muenz L, Ellen J. Prevalence and interactions of patient-related risks for nonadherence to antiretroviral therapy among perinatally infected youth in the United States. AIDS Patient Care STDS. 2010;24(2):97–104. doi:10.1089/apc.2009.0198
28. Seifu W, Ali W, Meresa B. Predictors of loss to follow up among adult clients attending antiretroviral treatment at Karamara general hospital, Jigjiga town, Eastern Ethiopia, 2015: a retrospective cohort study. BMC Infect Dis. 2018;18(1):1–8. doi:10.1186/s12879-018-3188-4
29. Ministry of Health Uganda. Epidemiological bulletin. Epidemiol Bull. 2019;4:1.
30. Oku AO, Oku OO, Monjok E, Owoaje ET. Prevalence and determinants of adherence to highly active anti-retroviral therapy amongst people living with HIV/AIDS in a rural setting in South-South Nigeria. Afr J Reprod Health. 2014;18(1):133–144.
31. Slogrove AL, Sohn AH. The global epidemiology of adolescents living with HIV: time for more granular data to improve adolescent health outcomes. Curr Opin HIV AIDS. 2018;13(3):170. doi:10.1097/COH.0000000000000449
32. Xu L, Munir K, Kanabkaew C, Le Coeur S. Factors influencing antiretroviral treatment suboptimal adherence among perinatally HIV-infected adolescents in Thailand. PLoS One. 2017;12(2):e0172392. doi:10.1371/journal.pone.0172392
33. Mutumba M, Ssewamala F, Namirembe R, et al. A multilevel integrated intervention to reduce the impact of HIV stigma on HIV treatment outcomes among adolescents living with HIV in Uganda: protocol for a randomized controlled trial. JMIR Res Protoc. 2022;11(10):e40101. doi:10.2196/40101
34. Fox MP, Rosen S. Retention of adult patients on antiretroviral therapy in low-and middle-income countries: systematic review and meta-analysis 2008–2013. J Acquir Immune Defic Syndr. 2015;69(1):98–108. doi:10.1097/QAI.0000000000000553
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
