Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 14
Factors Associated with Low Uptake of Medical Male Circumcision Among Adolescent Boys in Tanzania: A Multinomial Logistic Regression Modeling
Authors Bendera A , Nakamura K , Seino K, Al-Sobaihi S
Received 24 August 2022
Accepted for publication 1 December 2022
Published 19 December 2022 Volume 2022:14 Pages 565—575
DOI https://doi.org/10.2147/HIV.S387380
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Olubunmi Akindele Ogunrin
Anderson Bendera, Keiko Nakamura, Kaoruko Seino, Saber Al-Sobaihi
Department of Global Health Entrepreneurship, Division of Public Health, Tokyo Medical and Dental University, Tokyo, Japan
Correspondence: Keiko Nakamura, Department of Global Health Entrepreneurship, Division of Public Health, Tokyo Medical and Dental University, Tokyo, Japan, Tel +81 3-5803-4048, Fax +81-3-5803-4034, Email [email protected]
Background: Human immunodeficiency virus (HIV) remains the leading cause of years of life lost among adolescent boys in eastern and southern Africa. Medical male circumcision (MMC) is a cost-effective one-time intervention that can reduce the risk of heterosexual HIV acquisition in men by approximately 60%. Despite its importance in HIV prevention, the uptake of MMC remains suboptimal among adolescent boys. This study aimed to identify factors associated with low MMC uptake among adolescent boys in Tanzania.
Methods: This study was a secondary analysis of the 2016– 17 Tanzania HIV Impact Survey. Descriptive statistics were used to summarize the participants’ characteristics. Unadjusted and adjusted multinomial logistic regression models were fitted to identify factors associated with low MMC uptake among adolescent boys.
Results: A total of 2605 older adolescents (15– 19 years) and 1296 young adolescents (10– 14 years) were analyzed. The MMC uptake rates among older and young adolescents were 56.5% and 45.1%, respectively. Lower MMC uptake was found among respondents in rural areas (adjusted relative risk ratio [aRRR] = 0.40, 95% CI: 0.28– 0.57), in the traditionally non-circumcising zone (aRRR = 0.30, 95% CI: 0.23– 0.41), participants with no formal education (aRRR = 0.32, 95% CI: 0.23– 0.41), and those living in lower wealth quintile households (aRRR = 0.20, 95% CI: 0.11– 0.36). Respondents who were not covered by health insurance (aRRR = 0.67, 95% CI: 0.48– 0.94) and those who had no comprehensive HIV knowledge (aRRR = 0.55, 95% CI: 0.44– 0.70) were also found to have lower uptake of MMC.
Conclusion: To achieve and maintain high MMC coverage, MMC interventions for HIV prevention should focus on uncircumcised adolescent boys who are rural residents, of lower socioeconomic status, and residing in traditionally non-circumcising communities. Furthermore, dissemination of HIV knowledge and increasing health insurance coverage may encourage more adolescent boys to undergo MMC.
Keywords: adolescent boys, HIV prevention, medical male circumcision, Tanzania
Introduction
HIV remains the leading source of years of life lost among adolescent boys and men of reproductive age in Eastern and Southern Africa (ESA).1 Robust evidence has indicated that medical male circumcision (MMC) is a cost-effective biomedical intervention that can reduce the risk of heterosexual HIV acquisition in men by approximately 60%.2–5 MMC services are provided as a part of a package of HIV prevention interventions consisting of sexual risk reduction counseling, provision of condoms and condom use education, management of sexually transmitted infections, HIV testing, and linkage to care and treatment if found positive.6,7 The 18.6 million MMCs performed in the ESA through 2017 were estimated to have averted 230,000 new HIV infections.8
The goals of the joint strategic action framework to accelerate the scale-up of voluntary MMC for HIV prevention in ESA were to achieve 80% MMC coverage among men aged 15–49 years in the priority countries and to establish sustainable national programs that provide MMC services to young infants and adolescent boys.9 The new World Health Organization (WHO) and the Joint United Nations Programme on HIV and AIDS (UNAIDS) strategic framework for voluntary MMC aims to increase MMC coverage to 90% among males aged 10–29 years in priority countries.1
In Tanzania, MMC services for HIV prevention were introduced in 2009 and focused on regions with low male circumcision coverage and relatively high HIV prevalence, particularly in the western regions.10,11 The services were rolled out in three phases: scale-up, catch-up, and sustainability. The scale-up phase involved establishment of MMC centers and outreach services; the catch-up phase involved demand creation, maintenance, and expansion of MMC centers; and the sustainability phase involved maintenance of high MMC service coverage by reaching uncircumcised adults and focusing on young adolescents.10,12 By 2016, Tanzania had achieved an average male circumcision coverage of 80.3% among men aged 15–49 years, an increase from 66.8% in 2008.13,14 The MMC uptake among adolescent boys aged 15–19 years was 52.8%.13 To sustain the established HIV prevention benefits and high MMC coverage, MMC services focus on reaching uncircumcised adolescent boys.6,15
Scaling up and maintaining high MMC coverage among adolescent boys have been shown to be attainable and cost effective.16 Evidence shows that MMC among older adolescents (15–19 years) and men aged 20–29 years has more immediate benefits on HIV acquisition risk reduction, whereas MMC among young adolescents (10–14 years) is primarily an investment for the near future.1 Older adolescents (15–19 years) and young adults (20–24 years) are in fact more likely to engage in risky sexual behaviors than older adults. Therefore efforts to prevent HIV acquisition among older adolescents and young adults are essential for long-term epidemic control.17
MMC uptake is often deterred by the fear of pain, stigma, shame, high transport costs, fear of delayed wound healing, limited access to MMC services, attendance by female health providers, the time needed away from work, cultural values of traditional male circumcision (TMC), and the need to abstain from sex for six weeks after circumcision.18–20 The demographic and health surveys conducted in Lesotho and Malawi reported a lower MMC uptake among rural residents compared to their urban counterparts.21,22 Moreover, a study done in Rwanda found that, education, marital status, and religion affiliation were significantly associated with low MMC uptake among adult men.23 Traditionally, Tanzania has high male circumcision coverage; however, MMC uptake remains low among adolescent boys.13,24 The objective of this study was to identify factors associated with low MMC uptake among adolescent boys in Tanzania by using multinomial logistic regression modeling. Identification of the factors associated with low MMC uptake among adolescent boys is crucial for resource prioritization, considering the shortage of the healthcare workforce and limited resources in low-income countries.
Methods
Study Design
This study was a secondary analysis of the 2016–17 Tanzania HIV Impact Survey (THIS) datasets. The 2016–17 THIS was a two-stage stratified cluster sample-design survey. Census enumeration areas (clusters) were selected in the first stage using the probability proportional to size (PPS) method. Households were randomly selected in the second stage using the PPS method, and the sample was stratified into 31 regions. All people who slept in the selected households the night before the survey, who consented to participate in the survey were considered eligible. The overall household response rates in urban and rural settings were 94.5% and 94.8% respectively. Interview response rates among males aged 10–14 years and 15–24 years were 91.6% and 88.5% respectively.17
Study Settings
In Tanzania, approximately 70% of the general population resides in rural settings.25 By 2017 Tanzania was home to about 12 million adolescents aged 10–19 years. During the same period, the prevalence of HIV among men aged 15 years and above was 3.4%.17 Tanzania has two broad male circumcision zones: eastern zone and western zone. The eastern zone is largely comprised of traditionally circumcising communities and the western zone is largely comprised of traditionally non-circumcising communities.11
Study Participants
The current study included adolescent boys aged 10–19 years who participated in the survey regardless of their HIV status. They are from all 31 regions of Tanzania including both urban and rural settings of Tanzania. They are from both traditionally circumcising/ non-circumcising communities. A total of 7683 adolescent boys aged 10–19 years were interviewed. A total of 3782 adolescent boys were excluded from the current analysis due to missing data in the variables of interest.
Study Variables
The outcome variable was “male circumcision”, which was categorized as “uncircumcised”, “MMC”, or “TMC”. The independent variables included age, residence, male circumcision zone, household wealth index, formal education, health insurance, work-for-pay, sexual activity, disability, and HIV knowledge.
Data
Data for older adolescents (15–19 years) were obtained from the adult interview dataset, and data for young adolescents (10–14 years) were obtained from the child interview dataset. Male circumcision status was self-reported. Wealth index was constructed using categorical variables indicating ownership of household assets, construction materials, and durable goods. The variables were analyzed using principal component analysis (PCA). The first component was ranked into wealth quintiles and used as a summary indicator for wealth.26 HIV knowledge was assessed using a set of five questions on HIV infection. Respondents who correctly answered all five questions regarding HIV were considered to have comprehensive knowledge of HIV. Respondents who responded incorrectly to any of the five questions were considered not to have comprehensive HIV knowledge.27–29 Two questions were regarding the prevention of sexual transmission of HIV and three were regarding common misconceptions about contracting HIV. The two questions regarding the prevention of sexual transmission of HIV assessed whether respondents had knowledge about the possibility of reducing the risk of contracting HIV by always using condoms during sex and whether they knew about the possibility of reducing the risk of getting HIV by having sex with only one uninfected partner who has no other partners. The three questions regarding misconceptions were as follows: Can a healthy-looking person have HIV? Can a person get HIV from mosquito bites? Can a person get HIV by sharing food with a person who has HIV?
Definitions
MMC was defined as circumcision performed by a medical professional.6 TMC was defined as circumcision done by a traditional circumcizer.30 Disability was defined as having albinism or having difficulties or limitations in any of the following core domains: vision, hearing, walking, memory, self-care, or communication.31
Data Analysis
Data from older and young adolescents were independently analyzed. Data were summarized using the mean and standard deviation (SD) or frequency and percentage, where appropriate. Multinomial logistic regression (MLR) uses maximum likelihood estimation to predict categorical membership,32 allowing the identification of factors associated with MMC uptake among adolescent boys. Unadjusted and adjusted multinomial logistic regression models (MLRMs) were fitted to identify the factors associated with low MMC uptake. The first step was fitting simple bivariate multinomial models between each of the independent variables and the outcome variable. In the second step, all independent variables were included to one model at once and the adjusted MLRMs were applied by adjusting the influence of all independent variables. Multinomial logistic regression involves selection of a baseline category for the outcome variable, and the estimated coefficients are relative to the baseline category.32,33 The category “uncircumcised” was selected as the baseline category and was compared against the “MMC” and “TMC” categories. Statistical significance was set at a p-value < 0.05.
Results
Main Participant Characteristics
The distribution of older and young adolescents by circumcision status is summarized in Tables 1 and 2 respectively. A total of 2605 older adolescents (mean age, 16.9 years) and 1296 young adolescents (mean age, 11.9 years) were analyzed. The majority of participants (71.1% of older adolescents and 74.2% of young adolescents) were rural residents. Over half of the older adolescents (56.5%) were medically circumcised and about a quarter (26.1%) were uncircumcised. Less than half of the young adolescents (45.1%) were medically circumcised and 40.0% were uncircumcised. Moreover, only one-third (31.2%) of the older adolescents had comprehensive knowledge of HIV (Tables 1 and 2).
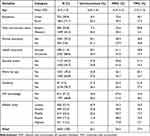 |
Table 1 Characteristics of Older Adolescents (15–19 Years) in Tanzania, n = 2605 |
 |
Table 2 Characteristics of Young Adolescents (10–14 Years) in Tanzania, n = 1296 |
Multinomial Logistic Regression Model Diagnostics
The adjusted MLRMs for older and young adolescents showed a statistically significant decrease in unexplained variance from the baseline models (p < 0.001). Pearson and Deviance chi-squared tests tested whether the predicted values from the model differed significantly from the observed values.32 Both Pearson and Deviance chi-square values for the two models were not significantly different from the observed values (p > 0.05), indicating a good fit. For MLR, the measure of the strength of the relationship between variables is the effect size and can be measured by the pseudo R-square.32 The pseudo R-square for the adjusted MLRMs for older adolescents was 0.33 (Cox & Snell) and 0.38 (Nagelkerke), and for young adolescents, it was 0.28 (Cox & Snell) and 0.32 (Nagelkerke), representing decent effect sizes.
Factors Associated with MMC Uptake
Factors associated with low uptake of MMC among older and young adolescents are presented in Tables 3 and 4 respectively. Age was a significant factor associated with uptake of MMC among young adolescents, p < 0.001. Each additional year of age increased the likelihood of young adolescents being medically circumcised versus uncircumcised by 29% (Table 4).
 |
Table 3 Results of the Multinomial Logistic Regression Model for Predicting MMC Uptake Among Older Adolescents in Tanzania |
 |
Table 4 Results of the Multinomial Logistic Regression Model for Predicting MMC Uptake Among Young Adolescents in Tanzania |
Rural older adolescents were 0.40 times less likely to be medically circumcised versus being uncircumcised compared to urban older adolescents, p < 0.001 (Table 3). Similarly, rural young adolescents were 0.44 times less likely to be medically circumcised versus being uncircumcised compared to urban young adolescents (Table 4).
Older adolescents residing in the western zone were 0.30 times less likely to be medically circumcised versus being uncircumcised compared to older adolescents residing in the eastern zone, p < 0.001 (Table 3). Also, young adolescents residing in the western zone were 0.45 times less likely to be medically circumcised versus being uncircumcised compared to young adolescents residing in the eastern zone, p < 0.001 (Table 4).
Older adolescents with no formal education were 0.32 times less likely to be medically circumcised versus being uncircumcised compared to those with formal education, p < 0.001 (Table 3). Similarly, young adolescents with no formal education were 0.61 times less likely to be medically circumcised versus being uncircumcised compared to those with formal education p < 0.05 (Table 4).
Older adolescents who were uninsured were 0.67 times less likely to be medically circumcised versus being uncircumcised compared to those who were insured, p < 0.05 (Table 3). Unlike older adolescents, health insurance was not significantly associated with MMC uptake among young adolescents, p > 0.05 (Table 4).
Older adolescents in the lowest wealth quintile were 0.20 times less likely to be medically circumcised versus being uncircumcised compared to older adolescents in the highest wealth quintile (Table 3). Also, young adolescents in the lowest wealth quintile were 0.18 times less likely to be medically circumcised versus being uncircumcised compared to young adolescents in the highest wealth quintile (Table 4).
Older adolescents with no comprehensive HIV knowledge were 0.55 times less likely to be medically circumcised versus being uncircumcised compared to older adolescents with comprehensive HIV knowledge, p < 0.001. Both, sexual activeness, and work-for-pay were not significantly associated with MMC uptake among older adolescents, p > 0.05. However, they were significant factors associated with TMC, p < 0.05 (Table 3).
Factors Associated with TMC Uptake
Factors associated with TMC uptake among older and young adolescents are presented in Tables 3 and 4 respectively. Adolescents residing in the traditionally non-circumcising zone, in rural settings, and those living in the lowest wealth quintile households were less likely to be traditionally circumcised versus being uncircumcised compared to their counterparts (Tables 3 and 4). Older adolescents who were uninsured, had no formal education, and had no comprehensive HIV knowledge were also less likely to be traditionally circumcised versus being uncircumcised compared to their counterparts. Moreover, older adolescents who were not working for pay and those who were not sexually active were less likely to be traditionally circumcised versus uncircumcised than their counterparts (Table 3).
Discussion
The overall MMC uptake among the older and young adolescents was 56.5% and 45.1%, respectively. Lower uptake of MMC was found among adolescent boys residing in rural areas, those with no formal education, those in traditionally non-circumcising communities, and those from households of lower wealth quintiles. Older adolescents who were uninsured and those with no comprehensive HIV knowledge were also more likely to have a lower MMC uptake. Moreover, younger adolescent boys were less likely to be medically circumcised.
Adolescent boys residing in rural areas were found to have a lower MMC uptake than those residing in urban areas. Demographic and health surveys conducted in Tanzania, Lesotho, and Malawi found similar findings among men aged 15–49 years.13,21,34 The observed male circumcision gap between urban and rural adolescent boys could partly be attributed to the low demand for MMC and limited healthcare services in rural areas.11,35 Targeting uncircumcised adolescent boys in rural areas goes hand-in-hand with MMC demand creation and outreach or mobile service delivery.6,11 Our findings underscore the need to continue targeting uncircumcised adolescent boys in rural areas.
This study found that adolescent boys with no formal education were less likely to be medically circumcised. Education is intrinsically linked to healthy behaviors.36,37 However, the association between education and MMC uptake has not been consistent across studies. Some studies found no link between formal education and uptake of MMC,38 and some studies found that men with formal education were less likely to be medically circumcised compared to uneducated men.23 The results of this study are in line with the findings of a study in northern Uganda,39 and reaffirm the paradigm that education is a powerful determinant of healthy behaviors.
Adolescent boys residing in the western zone (a traditionally non-circumcising zone) were less likely to be circumcised either medically or traditionally. In many traditionally circumcising communities, TMC rivals MMC.40 In these communities, men who are medically circumcised are often stigmatized and ridiculed.41 However, in Tanzania a situation analysis reported adequate acceptability of MMC in both traditionally circumcising and non-circumcising communities.42 The findings in this study (better uptake of MMC in traditionally circumcising communities) are in accordance with a study conducted in a traditionally circumcising community in Tanzania, which indicated a shift in preference from TMC to MMC.43
Adolescent boys residing in households in the lower wealth quintiles were less likely to be medically circumcised. MMC services are often provided at no direct cost to clients. The government and funding agencies often incur costs related to the surgical procedure. However, indirect costs, such as travel costs from homes to MMC centers, often deter men from accessing MMC services.44,45 To reach low-income clients in rural settings, the government of Tanzania introduced outreach services to healthcare facilities and mobile service delivery for hard-to-reach populations.11
This study found that older uninsured adolescents were more likely to have lower MMC uptake. Tanzania has two main health insurance schemes: the improved Community Health Fund (iCHF), a voluntary scheme mainly targeting the informal sector, and the National Health Insurance Fund (NHIF), a compulsory scheme for the formal sector.46 The two health insurance schemes are designed to cover medical and surgical expenses incurred by the insured. Despite MMC services being provided free of charge to clients, health insurance covers healthcare expenses related to surgical complications. Therefore, being insured may attract adolescent boys to circumcision. This theory may also explain why insured older adolescents were also more likely to be traditionally circumcised versus uncircumcised.
The current study found that older adolescents with no comprehensive HIV knowledge were more likely to have a low MMC uptake. Similar findings were reported among men aged 15–59 years.47 However, this association has not been consistent across studies. Some studies found no statistically significant association between knowledge and MMC uptake.23 In the context of adolescents, appropriate health-related knowledge is necessary, but not sufficient by itself to improve adolescents’ health behavior.48 We also found that only one-third of older adolescents had comprehensive HIV knowledge. Our findings emphasize the need to improve HIV knowledge among adolescent boys as part of efforts to improve MMC uptake.
Age was an important factor associated with MMC uptake among young adolescents. Younger adolescent boys were less likely to be medically circumcised. Current MMC services focus on uncircumcised young adolescents.15 Evidence shows that prepubertal male circumcision is more effective in preventing HIV than circumcision performed after adolescence.49 However, the decision to circumcise younger adolescents should be taken with care. The decision should be based on considerations of safety, consent, feasibility, and the local context. Circumcision for young adolescents with immature genitalia should be postponed until they become physically mature.6
Barriers and facilitators of MMC uptake are broad. They range from religion, culture, peer influence, and perception towards MMC, to fear of the unknown.50 Some studies have also shown that family members and female partners have influence on men’s decision making regarding male circumcision.45,50 Generally, the barriers and facilitators of MMC can be at individual/interpersonal level, community level, and/or health provider level.50
Most studies aiming to explore the factors associated with MMC uptake focused on adults23,38 and older adolescents were often assessed concurrently with adults.18,47,51,52 Prioritization of adolescent boys is likely to yield MMC targets quicker and cost-effectively than focusing on older, harder-to-reach men.53 The current study focused entirely on understanding and identifying the factors associated with low uptake of MMC among adolescent boys.
Nonetheless, this study had several limitations. First, we analyzed data from a cross-sectional survey; therefore, causal relationships could not be established. Second, the circumcision status was self-reported; therefore, the study was subject to reporting bias. Third, the datasets were not weighted; therefore, some areas may have been over- or under-sampled. However, the use of proper sampling techniques, an adequate sample size, and thorough analyses have ensured robust findings.
Conclusion
The government of Tanzania has adopted MMC as an essential component of a comprehensive HIV prevention package. To achieve and maintain high MMC coverage, focused MMC interventions for HIV prevention should focus on uncircumcised adolescent boys, who were found to be largely younger, rural residents, of lower socioeconomic status, and in traditionally non-circumcising communities. Moreover, dissemination of HIV-related knowledge and increasing health insurance coverage may attract more adolescent boys to circumcision.
Abbreviations
HIV, human immunodeficiency virus; MMC, medical male circumcision; MLRM, multinomial logistic regression model; RRR, relative risk ratio; THIS, Tanzania HIV impact survey; TMC, traditional male circumcision; WHO, World Health Organization; UNAIDS, Joint United Nations Programme on HIV and AIDS.
Data Sharing Statement
Datasets used in this study are available upon request from the PHIA website: https://phia-data.icap.columbia.edu/datasets?country_id=10.
Ethics Approval and Informed Consent
The 2016–17 THIS was approved by the National Institute for Medical Research (NIMR) and the Zanzibar Medical Research and Ethics Committee (ZAMREC). Adolescent boys aged 10-17 years provided informed verbal assent and those aged 18-19 years provided informed verbal consent.17 Permission to use the datasets for the current analyses was obtained from the Population-based HIV Impact Assessment (PHIA) website https://phia-data.icap.columbia.edu/ Participants’ confidentiality and privacy were secured. All methods applied in this study were in accordance with the standards and regulations of the Declaration of Helsinki.54
Acknowledgments
Authors are thankful to the PHIA project for allowing us to access and use the 2016-17 THIS datasets. We extend our gratitude the US President’s Emergency Plan for AIDS Relief (PEPFER) through the US Centers for Disease Control and Prevention (CDC) for funding the PHIA project.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organization. A framework for voluntary medical male circumcision: effective HIV prevention and a gateway to improved adolescent boys’\& men’s health in Eastern and Southern Africa by 2021: World Health Organization; 2016.
2. Bailey RC, Moses S, Parker CB, et al. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet. 2007;369(9562):643–656. doi:10.1016/S0140-6736(07)60312-2
3. Auvert B, Taljaard D, Lagarde E, Sobngwi-Tambekou J, Sitta R, Puren A. Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 trial. PLoS Med. 2005;2(11):1112–1122. doi:10.1371/journal.pmed.0020298
4. Gray RH, Kigozi G, Serwadda D, et al. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet. 2007;369(9562):657–666. doi:10.1016/S0140-6736(07)60313-4
5. Galarraga O, Shah P, Wilson-Barthes M, Ayuku D, Braitstein P. Cost and cost-effectiveness of voluntary medical male circumcision in street-connected youth: findings from an education-based pilot intervention in Eldoret, Kenya. AIDS Res Ther. 2018;15(1):1–7. doi:10.1186/s12981-018-0207-x
6. World Health Organization. Preventing HIV Through Safe Voluntary Medical Male Circumcision for Adolescent Boys and Men in Generalized HIV Epidemics: Recommendations and Key Considerations: Guidelines. World Health Organization; 2020.
7. World Health Organization. Remarkable progress in the scale up of voluntary medical male circumcision as an HIV prevention intervention in 15 ESA countries; 2019. Available from: https://www.who.int/publications/i/item/voluntary-medical-male-circumcision-progress-brief–2019.
8. World Health Organization. WHO Progress Brief: voluntary medical male circumcision for HIV prevention, July 2018 [Internet]; 2018. Available from: https://reliefweb.int/report/world/who-progress-brief-voluntary-medical-male-circumcision-hiv-prevention-july–2018.
9. PEPFAR. Joint Strategic Action Framework to Accelerate the Scale-Up of Voluntary Medical Male Circumcision for HIV Prevention in Eastern and Southern Africa. WHO, UNAIDS, PEPFAR; 2011.
10. National AIDS Control Programme (NACP). National Guidelines for Voluntary Male Medical Circumcision (VMMC) and Early Infant Male Circumcision (EIMC) [Internet]; 2016. Available from: http://www.nacp.go.tz/download/national-guidelines-for-voluntary-male-medical-circumcision-vmmc-and-early-infant-male-circumcision-eimc/.
11. National AIDS Control Programme (NACP). National Strategy to Scale up Male Circumcision for HIV Prevention: “Enhancing Men’s Role in HIV Prevention”2010–2015 [Internet]; 2010. Available from: https://www.nacp.go.tz/site/download/nationalscallingmc2010.pdf.
12. Strengthening High Impact Interventions for an AIDS-free Generation (AIDSFree) Project. VMMC Sustainability Summit Meeting Report. Arlington, VA: Dar es Salaam; 2017.
13. Ministry of Health Community Development Gender Elderly and Children [Tanzania] Ministry of Health [Zanzibar], ICF, National Bureau of Statistics. Tanzania Demorgraphic and Health Survey Indicator Survey (TDHS-MIS) 2015-2016. Dar es Salaam, Tanzania, Rockville, Maryland, USA: MoHCDGEC, MoH, NBS, OCGS, ICF; 2016:1–630.
14. Tanzania Commission for AIDS (TACAIDS). Tanzania HIV/AIDS and Malaria Indicator Survey 2007-08. Dar es Salaam, Tanzania: TACAIDS/Tanzania, ZAC/Tanzania, NBS/Tanzania, OCGS/Tanzania, and Macro International; 2008.
15. Njeuhmeli E, Gorgens M, Gold E, et al. Scaling up and sustaining voluntary medical male circumcision. maintaining HIV prevention benefits. Glob Heal Sci Pract. 2016;4(Supplement 1):S9––S17.
16. Dent J, Gaspar N, Njeuhmeli E, Kripke K. Age targeting and scale-up of voluntary medical male circumcision in Mozambique. PLoS One. 2019;14(2):1–14. doi:10.1371/journal.pone.0211958
17. Tanzania Commission for AIDS (TACAIDS) Zanzibar AIDS Commission (ZAC). Tanzania HIV Impact Survey (THIS) 2016–2017: Final Report. Dar Es Salaam, Tanzania; 2017.
18. Chiringa IO, Ramathuba DU, Mashau NS. Factors contributing to the low uptake of medical male circumcision in Mutare Rural District, Zimbabwe. African J Prim Heal Care Fam Med. 2016;8(2):1–6.
19. Masese RJ, Chimango JL. Overcoming barriers to uptake of voluntary medical male circumcision in a traditionally circumcising community in Machinga District, Malawi. World J AIDS. 2017;7(1):40. doi:10.4236/wja.2017.71005
20. George G, Strauss M, Chirawu P, et al. Barriers and facilitators to the uptake of voluntary medical male circumcision (VMMC) among adolescent boys in KwaZulu--Natal, South Africa. African J AIDS Res. 2014;13(2):179–187. doi:10.2989/16085906.2014.943253
21. Ministry of Health [Lesotho] and ICF International. Lesotho Demographic and Health Survey 2014 [Internet]. Maseru, Lesotho: ministry of Health/Lesotho and ICF International; 2016. Available from: http://dhsprogram.com/pubs/pdf/FR309/FR309.pdf.
22. Population-based HIV Impact Assessment (PHIA). Available from: https://phia.icap.columbia.edu/.
23. Nzamwita P, Biracyaza E. Factors Associated with Low Uptake of Voluntary Medical Male Circumcision as HIV-Prevention Strategy among Men Aged 18--49 Years from Nyanza District, Rwanda. HIV/AIDS. 2021;13:377.
24. Tanzania Commission for AIDS (TACAIDS), Zanzibar AIDS Commission (ZAC) NB of, Statistics (NBS), Office of the Chief Government Statistician (OCGS) and II 2013. Tanzania HIV/AIDS and Malaria Indicator Survey 2011–12. Dar es Salaam, Tanzania: TACAIDS/Tanzania, ZAC/Tanzania, NBS/Tanzania, OCGS/Tanzania, and ICF International; 2013.
25. Tanzania NBS. Population and housing census: population distribution by administrative areas: Ministry of Finance, Dar es Salaam; 2012.
26. Population-based HIV Impact Assessment (PHIA) Data Use Manual. 2021.
27. UNAIDS. Securing the future today: synthesis of strategic information on HIV and young people. Geneva: UNAIDS; 2011; Available from: https://www.unaids.org/sites/default/files/media_asset/20110727_JC2112_Synthesis_report_en_0.pdf.
28. Aniley AB, Ayele TA, Zeleke EG, Kassa AA. Factors associated with late Human Immunodeficiency Virus (HIV) diagnosis among peoples living with it, Northwest Ethiopia: hospital based unmatched case-control study. BMC Public Health. 2016;16(1):1–8. doi:10.1186/s12889-016-3727-0
29. Chan BT, Tsai AC. HIV knowledge trends during an era of rapid antiretroviral therapy scale-up: an analysis of 33 sub-Saharan African countries. J Int AIDS Soc. 2018;21(7):e25169. doi:10.1002/jia2.25169
30. World Health Organization. Traditional Male Circumcision Among Young People: A Public Health Perspective in the Context of HIV Prevention; 2009.
31. Garcia Mora ME, Schwartz Orellana S, Freire G. Disability Inclusion in Latin America and the Caribbean. 2021.
32. Field A. Discovering Statistics Using IBM SPSS Statistics. sage; 2013.
33. Kwak C, Clayton-Matthews A. Multinomial logistic regression. Nurs Res. 2002;51(6):404–410. doi:10.1097/00006199-200211000-00009
34. National Statistical Office (NSO) [Malawi] and ICF. Malawi Demographic and Health Survey 2015–16 [Internet]. Zomba, Malawi: National Statistical Office and ICF; 2017. Available from: http://dhsprogram.com/pubs/pdf/FR319/FR319.pdf.
35. Tanzania Service Provision Assessment Survey 2014–2015 [Internet]. Dar es Salaam, Tanzania: ministry of Health and Social Welfare (MoHSW) [Tanzania Mainland], Ministry of Health (MoH) [Zanzibar], National Bureau of Statistics (NBS), Office of the Chief Government Statistician (OCGS), and ICF International; 2015. Available from: http://dhsprogram.com/pubs/pdf/SPA22/SPA22.pdf.
36. Raghupathi V, Raghupathi W. The influence of education on health: an empirical assessment of OECD countries for the period 1995--2015. Arch Public Heal. 2020;78(1):1–18.
37. Cowell AJ. The relationship between education and health behavior: some empirical evidence. Health Econ. 2006;15(2):125–146. doi:10.1002/hec.1019
38. Rupfutse M, Tshuma C, Tshimanga M, Gombe N, Bangure D, Wellington M. Factors associated with uptake of voluntary medical male circumcision, Mazowe District, Zimbabwe, 2014. Pan Afr Med J. 2014;1:19.
39. Nanteza BM, Serwadda D, Kankaka EN, Mongo GB, Gray R, Makumbi FE. Knowledge on voluntary medical male circumcision in a low uptake setting in northern Uganda. BMC Public Health. 2018;18(1):1–7. doi:10.1186/s12889-018-6158-2
40. Masese R, Mwalabu G, Petrucka P, Mapulanga P. Key challenges to voluntary medical male circumcision uptake in traditionally circumcising settings of Machinga district in Malawi. BMC Public Health. 2021;21(1):1–11. doi:10.1186/s12889-021-11979-z
41. Sabet Sarvestani A, Bufumbo L, Geiger JD, Sienko KH. Traditional male circumcision in Uganda: a qualitative focus group discussion analysis. Pan Afr Med J. 2012;1:548. doi:10.1371/journal.pone.0045316
42. Wambura M, Mwanga J, Mosha J, Mshana G, Mosha F, Changalucha J. Situation analysis for male circumcision in Tanzania: final report. Mwanza Natl Inst Med Res. 2009;1:86.
43. Wambura M, Mwanga JR, Mosha JF, Mshana G, Mosha F, Changalucha J. Acceptability of medical male circumcision in the traditionally circumcising communities in Northern Tanzania. BMC Public Health. 2011;11(1):1–8. doi:10.1186/1471-2458-11-373
44. Muhamadi L, Ibrahim M, Wabwire-Mangen F, Peterson S, Reynolds SJ. Perceived medical benefit, peer/partner influence and safety and cost to access the service: client motivators for voluntary seeking of medical male circumcision in Iganga district eastern Uganda, a qualitative study. Pan Afr Med J. 2013;15(1). doi:10.11604/pamj.2013.15.117.2540
45. Carrasco MA, Wilkinson J, Kasdan B, Fleming P. Systematic review of barriers and facilitators to voluntary medical male circumcision in priority countries and programmatic implications for service uptake. Glob Public Health. 2019;14(1):91–111. doi:10.1080/17441692.2018.1465108
46. Ministry of Health Community Development Gender Elderly and Children [Tanzania]. Tanzania Health Sector Strategic Plan (HSSP V) 2021-2026; 2021:2026.
47. Edossa ZK, Kumsa AT, Gebre MN. Male circumcision uptake and its predictors among sexually active men aged 15--59 years living in the highest HIV prevalence region of Ethiopia: evidence from 2016 Ethiopia demographic and health survey. BMC Public Health. 2020;20(1):1–8. doi:10.1186/s12889-020-09918-5
48. Nagy-Pénzes G, Vincze F, Sándor J, B\’\iró É. Does better health-related knowledge predict favorable health behavior in adolescents? Int J Environ Res Public Health. 2020;17(5):1680. doi:10.3390/ijerph17051680
49. Kelly R, Kiwanuka N, Wawer MJ, et al. Age of male circumcision and risk of prevalent HIV infection in rural Uganda. Aids. 1999;13(3):399–405. doi:10.1097/00002030-199902250-00013
50. Nanteza BM, Makumbi FE, Gray RH, Serwadda D, Yeh PT, Kennedy CE. Enhancers and barriers to uptake of male circumcision services in Northern Uganda: a qualitative study. AIDS Care. 2020;32(8):1061–1068. doi:10.1080/09540121.2019.1698703
51. Tapera R, Kebofe T, Tumoyagae T, January J. Factors associated with uptake of voluntary medical male circumcision among University of Botswana undergraduate male students. Int J Heal Promot Educ. 2017;55(5–6):333–342. doi:10.1080/14635240.2017.1394796
52. Hatzold K, Mavhu W, Jasi P, et al. Barriers and motivators to voluntary medical male circumcision uptake among different age groups of men in Zimbabwe: results from a mixed methods study. PLoS One. 2014;9(5):e85051. doi:10.1371/journal.pone.0085051
53. Lane C, Bailey RC, Luo C, Parks N. Adolescent male circumcision for HIV prevention in high priority countries: Opportunities for improvement. Clin Infect Dis. 2018;66(suppl_3):S161––S165
54. World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–2194. doi:10.1001/jama.2013.281053
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
