Back to Journals » Hepatic Medicine: Evidence and Research » Volume 15
Factors Associated with in-Hospital Mortality in Malagasy Patients with Acute Decompensation of Liver Cirrhosis: A Retrospective Cohort
Authors Razafindrazoto CI , Randriamifidy NH , Ralaizanaka BM , Andrianoelison JT, Ravelomanantsoa HT, Rakotomaharo M , Hasina Laingonirina DH , Maherison S, Rakotomalala JA, Rasolonjatovo AS, Rakotozafindrabe ALR , Rabenjanahary TH , Razafimahefa SH, Ramanampamonjy RM
Received 29 December 2022
Accepted for publication 10 March 2023
Published 12 March 2023 Volume 2023:15 Pages 21—26
DOI https://doi.org/10.2147/HMER.S401628
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Gerry Lake-Bakaar
Chantelli Iamblaudiot Razafindrazoto,1 Nitah Harivony Randriamifidy,1 Behoavy Mahafaly Ralaizanaka,2 Jean Tsitamita Andrianoelison,1 Haga Tsilavo Ravelomanantsoa,1 Mialitiana Rakotomaharo,1 Domoina Harivonjy Hasina Laingonirina,1 Sonny Maherison,1 Jolivet Auguste Rakotomalala,3 Anjaramalala Sitraka Rasolonjatovo,1 Andry Lalaina Rinà Rakotozafindrabe,1 Tovo Harimanana Rabenjanahary,1 Soloniaina Hélio Razafimahefa,2 Rado Manitrala Ramanampamonjy1
1Gastroenterology Unit, University Hospital Joseph Raseta Befelatanana, Antananarivo, Madagascar; 2Hepato-Gastroenterology Unit, University Hospital Andrainjato, Fianarantsoa, Madagascar; 3Hepato-Gastroenterology Unit, University Hospital Mahavoky Atsimo, Mahajanga, Madagascar
Correspondence: Chantelli Iamblaudiot Razafindrazoto, Gastroenterology Unit, University Hospital Joseph Raseta Befelatanana, Antananarivo, Madagascar, Email [email protected]
Background: Cirrhosis is a pathology responsible for a significant hospital morbidity and mortality. The objective of this study was to determine the factors associated with hospital mortality in a sample of Malagasy cirrhotics.
Patients and Methods: This was a retrospective cohort study from January 2018 to August 2020 conducted in the Hepato-Gastroenterology Unity, University Hospital Joseph Raseta Befelatanana, Antananarivo, Madagascar.
Results: One hundred and eight patients were included. The mean age was 51.13± 13.50 years with a sex ratio of 2.37. The etiology of cirrhosis was dominated by alcohol (44.44%), hepatitis B virus (24.07%) and hepatitis C virus (13.89%). Twenty-eight patients (25.93%) had died. Factors associated with in-hospital mortality were hepatic encephalopathy (OR: 14.16; 95% CI: 5.08– 39.4; p: 0.000), renal failure (OR: 8.55; 95% CI: 2.03– 39.9; p: 0.0034), gastrointestinal bleeding (OR: 3.25; 95% CI: 1.32– 7.92; p: 0.0099), hyponatraemia < 130mmol/L (OR: 3.34; 95% CI: 1.04– 10.6; p=0.046), Child-Pugh C classification (OR: 0.19; 95% CI: 0.12– 0.21; p: 0.000), and MELD-Na score > 32 (OR: 27.5; 95% CI: 4.32– 174.8; p: 0.004).
Conclusion: The in-hospital mortality rate during acute decompensation of cirrhosis remains high in Madagascar. Hepatic encephalopathy, renal failure, GI bleeding and hyponatraemia are the main clinico-biological factors affecting in-hospital mortality. Early intervention on these modifiable factors is an important step to improve hospital outcomes. The natraemia, MELD score and MELD-Na score should be used in routine practice in Madagascar to identify patients with acute decompensation of cirrhosis at high risk of death.
Keywords: risk factors, in-hospital mortality, liver cirrhosis, Madagascar
Background
Decompensated cirrhosis is a terminal liver disease, the evolution of which is characterized by the occurrence of frequent and potentially serious life-threatening complications.1,2 It is a global public health problem, especially in sub-Saharan Africa due to the high mortality rate and the inaccessibility of treatment.1–3 Cirrhosis accounts for approximately 2 million deaths per year worldwide.1,4 In Madagascar, it represents the first digestive pathology encountered in hospitalization with 33.54%2 and has a high mortality rate estimated at 26.5%.3 Patients with decompensated cirrhosis have a very high risk of mortality, due to multiple complications.1–6 Although liver transplantation significantly improves the survival of patients with decompensated cirrhosis, it is not widely used due to limited liver resources, high costs and immunological reactions to transplantation.6 This procedure remains unavailable in Madagascar to this day. Thus, in a low-income country like Madagascar, the existence of readily available clinical and paraclinical parameters to assess the risk of in-hospital mortality may help the clinician to identify vulnerable patients. The objective of this study was to determine the factors associated with hospital mortality in a sample of Malagasy cirrhotics.
Patients and Methods
Study Design and Participants
This was a retrospective cohort study from January 2018 to August 2020 conducted in the Hepato-Gastroenterology Unity, University Hospital Joseph Raseta Befelatanana. Patients hospitalized during the study period with decompensated cirrhosis were included in the study. Patients with incomplete records (absence of sodium level and/or parameters needed to calculate Model for End stage Liver Disease (MELD) score and MELD-sodium (MELD-Na) score like INR, creatinine, total bilirubin) and with hepatocellular carcinoma had been excluded. The clinico-biological characteristics at admission (gender, ascites, hepatic encephalopathy, gastrointestinal (GI) bleeding, spontaneous bacterial peritonitis, renal failure at admission, hyponatraemia, death) and the prognostic scores at admission (Child-Pugh, MELD and MELD-Na scores) were collected.
Methodology and Definitions
The diagnosis of cirrhosis was based on an unequivocal clinical and biochemical profile, a highly suggestive endoscopic examination, or typical imaging findings in agreement with current guidelines. The diagnosis of hepatic encephalopathy was primarily clinical, with the presence of disorientation, confusion, inappropriate behavior, agitation, drowsiness, stupor, frank coma, and asterixis. Spontaneous bacterial peritonitis was diagnosed based on an ascitic fluid polymorphonuclear count of > 250 cells/mm3 and the absence of data suggesting secondary peritonitis. The alcoholic etiology of the cirrhosis was retained on the basis of an alcoholic consumption of more than 20 g/day in women and 40 g/day in men for at least 10 years, and without any other etiologies found. The viral and autoimmune origin was retained in view of the positivity of viral markers (HBs Antigen and anti-HCV antibody) and anti-tissue autoantibodies. Non-alcoholic steatohepatitis was evoked in case of metabolic syndrome in a non-alcoholic patient, without other causes found.
All patients with acutely decompensated liver cirrhosis received standard medical treatment based on international consensus. Patients with ascites underwent ascitic puncture and ascitic fluid analysis. Patients with gastrointestinal hemorrhage were supportively cared according to a standardized protocol. Ligation and beta-blocker combination was performed for esophageal varices. Patients with hepatic encephalopathy received lactulose therapy. Empirical antibiotic administration was based on local guidelines. None of the patients underwent transjugular intrahepatic portosystemic shunt (TIPSS). None of the patients underwent liver transplantation.
The Child-Pugh score was calculated using the MDcalc® application available at https://www.mdcalc.com/calc/340/child-pugh-score-cirrhosis-mortality.
The MELD score was calculated using the MDcalc® application available at https://www.mdcalc.com/calc/2693/meld-score-original-pre-2016-model-end-stage-liver-disease. The MELD-Na score was calculated using the MDcalc® application available at https://www.mdcalc.com/meldna-meld-na-score-liver-cirrhosis#evidence.
Statistical Analysis
Statistical analysis was performed using Epi-Info® 7.2.4.0 software. Continuous variables were expressed as mean ± standard deviation. Categorical variables were expressed as proportion (%). A multivariate study was performed using logistic regression to identify associations between variables (Gender, ascites, hepatic encephalopathy, gastrointestinal bleeding, spontaneous bacterial peritonitis, renal failure, natraemia, Child-Pugh, MELD score, MELD-Na score) and death. A value of p<0.05 was considered significant.
Results
Clinico-Biological Characteristics and Outcome of the Patients
The mean age of the patients was 51.13±13.50 years with extremes from 16 to 81 years. Seventy-six patients (70.4%) were male, with a sex ratio of 2.37. The etiology of cirrhosis was dominated by alcohol (44.44%), hepatitis B virus (24.07%) and hepatitis C virus (13.89%). Ascites (97.2%), gastrointestinal (GI) bleeding (33.3%) and hepatic encephalopathy (29.6%) were the 3 main modes of decompensation. Ten patients (9.3%) had renal failure on admission. Sixty patients (55.56%) had a Child-Pugh C score. The mean natraemia was 131.8 mmol/L with extremes ranging from 94 to 148 mmol/L. The mean MELD and MELD-Na scores were 19.7 (range 7–54) and 22.9 (range 7–44), respectively. Twenty-eight patients died during hospitalization, giving an in-hospital mortality rate of 25.9%. The causes of death were hepatic encephalopathy (53.6%), GI bleeding (35.7%), bacterial infections (7.1%) and hepatorenal syndrome (3.6%). The clinical and biological characteristics and outcome of the patients are reported in Table 1.
 |
Table 1 Clinical and Biological Characteristics of Study Population |
Factors Associated with in-Hospital Mortality
Factors associated with in-hospital mortality were hepatic encephalopathy (OR: 14.16; 95% CI: 5.08–39.4; p: 0.000), renal failure (OR: 8.55; 95% CI: 2.03–39.9; p: 0.0034), GI bleeding (OR: 3.25; 95% CI: 1.32–7.92; p: 0.0099), hyponatraemia <130mmol/L (OR: 3.34; 95% CI: 1.04–10.6; p=0.046), Child-Pugh C classification (OR: 0.19; 95% CI: 0.12–0.21; p: 0.000), and MELD-Na score >32 (OR: 27.5; 95% CI: 4.32–174.8; p: 0.004). The factors associated with in-hospital mortality are reported in Table 2.
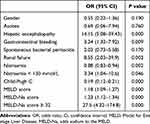 |
Table 2 Factors Associated with in-Hospital Mortality |
Discussion
The aim of this study was to investigate factors associated with mortality in patients with acute decompensation of cirrhosis. Several parameters were evaluated, whether clinical, such as the presence of hepatic encephalopathy and GI bleeding, or biological, such as the existence of renal dysfunction and/or hyponatraemia, or the MELD and MELD-Na scores usually used in pre-transplantation.
In this study, the in-hospital mortality rate was 25.9%. This rate was similar to that found in a previous study in 2010 performed in the same unit.3 In contrast, the overall in-hospital mortality rate in America was 8% in 2017.7 This clear difference can be explained by the difficulty of managing cirrhosis in Madagascar due to the absence of certain drugs (albumin, vasoactive drugs.), the inadequacy of the technical platform (few endoscopic centers) And different severity of illness at the time of admission. As for the causes of death, they remained the same between our study and that of 20103 with respectively hepatic encephalopathy in 53.6% vs 51.6% and GI bleeding in 35.7% vs 25.8%.
In our study, ascites did not appear to be a factor associated with in-hospital mortality (OR: 0.69; CI95%: 0.06 to 7.94, p=0.76). In fact, its appearance constitutes a turning point in the evolution of cirrhosis in the short and medium term. Approximately 60% of cirrhotic patients will develop ascites within 10 years, which is a poor prognostic factor since the survival rate is 40% at 1 year.8
Our results showed that hepatic encephalopathy (EH) was not only the first cause of mortality, but also appeared to be a risk factor for death during hospitalization (OR: 14.15; 95% CI: 5.08 to 39.43, p=0.000). In a Ghanaian study, including 167 cirrhotic patients, 53 patients had presented a HE of which 40 (75.5%) died during hospitalization. They had objectified a strong association between HE and death (p≤0.001).9
GI bleeding represented the second complication in this present study (33.3%). In addition, it was strongly associated with the risk of death (OR: 3.24; CI95%:1.32 to 7.92, p=0.0099). This prevalence of GI bleeding was lower in an Argentinean study (10%) and was not associated with risk of in-hospital mortality (p=0.055).8 This difference is due to the difficulty of performing emergency endoscopic variceal ligation in Madagascar.
Renal dysfunction was strongly associated with the risk of death during hospitalization (OR: 8.55; 95% CI: 2.034 to 39.9, p=0.0034). In a Brazilian study, 51 patients (26%) out of 198 cirrhotic patients with renal failure died, with hospital mortality being higher in those with increased creatinine (p<0.000001).10 These results were confirmed by another publication (OR=2; CI95%: 0.5–3.47, p=0.04) with an area under the curve of 92% (CI95% 87.6–95.8).8
Hyponatraemia was very frequent in our patients (61.11%). Indeed, 38 patients (35.2%) with sodium level<130mmol/L and 28 (25.0%) between 130–135mmol/L. A hyponatraemia <130mmol/L was strongly associated with the risk of death (OR=3.34; CI95%: 1.04 to 10.6, p=0.04). This relatively high prevalence of hyponatraemia was found in an American (87%)11 and Tunisian (31.4%) study.12 In the Tunisian study,12 hyponatraemia was significantly associated with severe Child-Pugh C cirrhosis (OR=7.84; CI95%: 2.47 to 24.9, p<0.001) with an overall 1-year survival estimated at 22.5%. However, in an American study,11 patients with severe hyponatraemia had more hepatic encephalopathy (28%; p<0.05) and hospital mortality related to hyponatraemia was higher but not significant (16% vs 10%; p=0.25). Several studies reported that the presence of hyponatraemia can be the harbinger of several complications such as hepatic encephalopathy, hepatorenal syndrome and therefore the risk of death related to hyponatraemia before transplantation is very high.13,14
Our outcomes showed that the MELD score was associated with a risk of in-hospital mortality (OR=1.18; CI95%: 1.09 to 1.27, p=0.000). Usually the MELD score is used by several countries for graft allocation of liver transplants.15 It was originally developed to predict 3-month mortality in patients who received TIPS.15 All studies on MELD were mainly aimed at demonstrating the possibility of using it as a predictive factor of 3-month or 1-year mortality in comparison with other scores (Child-Pugh, MELD-Na.).16,17
The MELD-Na score especially when it was ≥32 was strongly associated with the death of our patients (OR: 27.5; CI95%: 4.32–174.8; p=0.0004). This score had incorporated sodium level, which is an independent risk factor for mortality in cirrhosis, into the MELD score.18 The MELD-Na score had taken the place of the MELD score for liver transplant allocation in the United States.19 A study done in Hong Kong, including patients with chronic hepatitis B, reported a strong correlation between MELD-Na score and in-hospital mortality, especially when the MELD-Na score > 30 with a mortality of 64% (p<0.0001).20 The MELD-Na score is mainly used to assess the risk of death of patients at 3 months with c-statistic at 0.83 (p<0.0001, CI 95% 0.77–0.89).16
Conclusion
In-hospital mortality in patients with cirrhosis remains high in Madagascar. This study had highlighted the poor prognostic factors that should be compulsorily searched for on admission of patients with cirrhosis, such as the presence of hepatic encephalopathy, GI bleeding, renal failure, hyponatraemia <130mmol/L and a MELD-Na score ≥32. These patients will need to be closely monitored. In addition, improved management of its complications is necessary if the in-hospital mortality rate of cirrhosis is to be improved.
Data Sharing Statement
Data supporting the conclusions of this study are available from the corresponding author on reasonable request.
Ethical Considerations
This study was ethically and scientifically approved by ethic committee of University Hospital Joseph Raseta Befelatanana, with a waiver for informed consent as all patients were de-identified. All study procedures were conducted in accordance with the Declaration of Helsinki. All authors had access to the study data and reviewed and approved the final manuscript before submission.
Acknowledgments
The authors would like to thank the members of the Gastroenterology Unit of the Joseph Raseta Befelatanana University Hospital, Antananarivo, Madagascar.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflicts of interest in relation to this work.
References
1. Razafindrazoto CI, Rabenjanahary TH, Ralaizanaka BM, et al. Aspects épidémio-clinique, étiologique et évolutive des cirrhoses hépatiques à Fianarantsoa, Madagascar. Med Afr Noire. 2021;68(2):112–118.
2. Razafimahefa SH, Rabenjanahary TH, Razanaparany OM, Rakotozafindrabe R, Rakotoarivelo RA, Ramanampamonjy RM. Digestive diseases in a medical ward in Madagascar: a retrospective study. J Afr Hepatol Gastroenterol. 2012;6:116–127. doi:10.1007/s12157-012-0378-3
3. Razafimahefa SH, Rabenjanahary TH, Rakotoarivelo RA, Ramilitiana B, Ramanampamonjy RM, Rajaona HR. Causes of death in a sample of cirrhotic patients from Madagascar. Med Trop. 2010;70:163–165.
4. Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–2128. doi:10.1016/S0140-6736(12)61728-0
5. Asrani SK, Devarbhavi H, Eaton J, Kamath PS. Burden of liver diseases in the world. J Hepatol. 2019;70:151–171. doi:10.1016/j.jhep.2018.09.014
6. Cárdenas A, Ginès P. Management of patients with cirrhosis awaiting liver transplantation. Gut. 2011;60:412–421. doi:10.1136/gut.2009.179937
7. Mathur AK, Chakrabarti AK, Mellinger JL, et al. Hospital resource intensity and cirrhosis mortality in United States. World J Gastroenterol. 2017;23(10):1857–1865. doi:10.3748/wjg.v23.i10.1857
8. Vicco MH, Rodeles L, Ferini F, Long AK, Musacchio HM. In hospital mortality risk factors in patients with ascites due to cirrhosis. Rev Assoc Med Bras. 2015;61(1):35–39. doi:10.1590/1806-9282.61.01.035
9. Duah A, Agyei-Nkansah A, Osei-Poku F, Duah F, Ampofo-Boobi D, Peprah B. The prevalence, predictors, and In-hospital mortality of hepatic encephalopathy in patients with liver cirrhosis admitted at St. Dominic hospital in Akwatia, Ghana. Can J Gastroenterol Hepatol. 2020;2020:8816522. doi:10.1155/2020/8816522
10. De Carvalho GC, De Andrade Regis C, Kalil JR, et al. Causes of renal failure in patients with decompensated cirrhosis and its impact in hospital mortality. Ann Hepatol. 2012;11(1):90–95. doi:10.1016/S1665-2681(19)31491-7
11. Sigal SH, Amin A, Chiodo JA, Sanyal A. Management strategies and outcomes for hyponatremia in cirrhosis in the hyponatremia registry. Can J Gastroenterol Hepatol. 2018;2018:1579508. doi:10.1155/2018/1579508
12. Ennaifer R, Cheikh M, Romdhane H, et al. Hyponatremia in cirrhosis: risk factors and prognostic value. Tunis Med. 2016;94(5):401–405.
13. Jang C, Jung YK. Hyponatremia in Liver cirrhosis. Korean J Gastroenterol. 2018;72(2):74–78. doi:10.4166/kjg.2018.72.2.74
14. John S, Thuluvath PJ. Hyponatremia in cirrhosis: pathophysiology and management. World J Gastroenterol. 2015;21(11):3197–3205. doi:10.3748/wjg.v21.i11.3197
15. Wiesner R, Edwards E, Freeman R, et al. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology. 2003;124:91–96. doi:10.1053/gast.2003.50016
16. Acharya G, Kaushik RM, Gupta R, Kaushik R. Child-Turcotte-Pugh Score, MELD Score and MELD-Na score as predictors of short-term mortality among patients with End-stage liver disease in Northern India. Inflamm Intest Dis. 2020;5:1–10. doi:10.1159/000503921
17. Peng Y, Qi X, Guo X. Child-Pugh versus MELD score for the assessment of prognosis in liver cirrhosis: a systematic review and meta-analysis of observational studies. Medicine. 2016;95(8):e2877. doi:10.1097/MD.0000000000002877
18. Kim WR, Biggins SW, Kremers WK, et al. Hyponatremia and mortality among patients on the liver-transplant waiting list. N Engl J Med. 2008;359(10):1018–1026. doi:10.1056/NEJMoa0801209
19. Nagai S, Chau LC, Schilke RE, et al. Effects of allocating livers for transplantation based on model for end-stage liver disease-sodium scores on patient outcomes. Gastroenterology. 2018;155:1451–1462. doi:10.1053/j.gastro.2018.07.025
20. Wong VWS, Chim AML, Wong GLH, Sung JJY, Chan HLY. Performance of the new MELD-Na score in predicting 3-month and 1-year mortality in Chinese patients with chronic hepatitis B. Liver Transpl. 2007;13(9):1228–1235. doi:10.1002/lt.21222
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
