Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 14
Factors Associated with Condom Use Among Out-of-School Young People on Anti-Retroviral Therapy in Central Uganda
Authors Kavuma D , Ndibazza J, Kirwana VB , Mukasa Kafeero H , Katongole SP , Baluku JB
Received 19 January 2022
Accepted for publication 2 April 2022
Published 26 April 2022 Volume 2022:14 Pages 217—230
DOI https://doi.org/10.2147/HIV.S357535
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Prof. Dr. Olubunmi Akindele Ogunrin
David Kavuma,1,2 Juliet Ndibazza,1 Venantius Bbaale Kirwana,3 Hussein Mukasa Kafeero,1 Simon Peter Katongole,1 Joseph Baruch Baluku2
1Faculty of Health Sciences, Uganda Martyrs University-Nkozi, Kampala, Uganda; 2Directorate of Medical Services, Mildmay Uganda, Kampala, Uganda; 3Monitoring, Evaluation and Learning, Sexual Reproductive Health and Rights Alliance, Kampala, Uganda
Correspondence: David Kavuma, Tel +2560772839416, Email [email protected]
Introduction: Evidence is lacking about condom use among out-of-school young people (OS-YP) on anti-retroviral therapy (ART). This study aimed to understand the factors associated with consistent condom use among OS-YP aged 15– 24 years old on ART in Central Uganda.
Methods: This was a quantitative descriptive cross-sectional study conducted among 357 OS-YP on ART from seven districts of Central Uganda. Interviewer-administered questionnaire was used to collect data on consistent condom use in the past 12 months from OS-YP, aged 15– 24 years, who did not intend to have children in that period. Consistent condom use by participants was considered to be the routine (always) use of condoms during sexual intercourse in the past 12 months. Frequencies and percentages were used for univariate analysis, while Pearson’s Chi-square was used to determine bivariate association and logistic regression analysis for multivariable association with consistent condom use, at 95% confidence level.
Results: Of the 357 sexually active OS-YP on ART, 73% were females. The age range of study participants was between 15 and 24 years old (with a mean ± standard deviation of 20± 3 years) where 55% were aged 20 to 24 years, while their sexual partners were aged ≥ 25 years, and 49% of respondents did not use condoms. Primary school education level, being employed, rural residence, and receiving ART from health facilities with a perceived adequate number of health workers were strongly associated with consistent condom use with the adjusted odds ratio (AOR) of 0.2 (95% CI 0.07– 0.69) level of education; 2.12 (95% CI 1.06– 4.26) employment status; 2.46 (95% CI 1.19– 5.10) residence and 6.08 (95% CI 1.05– 35.22) perceived level of staffing at the health facility, respectively.
Conclusion: Efforts to increase consistent condom use should focus on recruiting more providers in health facilities to intensify condom use sensitization among sexually active young people on ART in the context of HIV epidemic control.
Keywords: out-of-school young people, antiretroviral therapy, consistent condom use
Background
Correct and consistent condom use is one of the key behavioural HIV prevention interventions that not only limits spread of sexually transmitted infections (STIs), including HIV, but also prevents unwanted pregnancy particularly among the sexually active persons.1 UNAIDS notes that both male and female condoms, if correctly and consistently used, may be up to 95% effective.2 Since female condoms are more expensive and less accessible than male condoms, male condoms are the most widely and frequently used in prevention of unwanted pregnancy and sexually transmitted infections, including HIV.3,4 However, despite the fact that condoms are part of the comprehensive HIV prevention interventions, the spread of HIV remains high in most sub-Saharan African countries.5
Globally, out of the 38 million people who live with HIV, about 67% were accessing antiretroviral therapy (ART) by the end of 2019.6 The majority of those on ART are in sub-Saharan Africa, where over 10.3 million are accessing ART.7 In Uganda, of the 1.4 million people living with HIV (PLWH), 1.2 million are on ART.8 The 2017 UNFPA Technical Report on Sexual and Reproductive Health Rights (SRHR) and HIV in Uganda indicated that 360 young people aged 15–24 years are believed to contract HIV per week.9 Therefore, this age group contributes significantly to the HIV burden in Uganda. This could be attributed to high-risk sexual behaviour among young people living with HIV in Uganda.8 In addition, with the increasing HIV drug resistance (HIVDR) in Uganda, which is partly caused by poor patient adherence to antiretroviral therapy,10,11 young people on ART cannot be made an exception. This suggests that some Ugandan young people on ART may not be using condoms consistently hence greatly contributing to the HIV burden.
Out-of-school young people (OS-YP) are more likely to be sexually active than their counterparts at school. This is because schools tend to structure and limit the students’ time to engage in sex, create an environment which discourages sexual-risk-taking, and schools can increase a belief in the future by encouraging young people to plan for higher education thereby motivating them to avoid risky sexual behaviours.12,13 Notwithstanding, available evidence notes that OS-YP are more likely to report early sexual debut, and low sexually transmitted diseases and HIV risk perception with low condom use.14,15 These and other structural factors such as alcohol and substance abuse coupled with inadequate parental monitoring, among others, could easily lure them into risky sexual behaviours.12 Conversely, being in school is associated with 52% lower odds of HIV infection in Uganda.16
The sexual practices of OS-YP living with HIV on ART are largely unknown in Uganda. A meta-analysis of 14 studies from sub-Saharan Africa showed that people with HIV on ART had lower odds for having multiple sexual partners and unprotected sex.17 Further, a study from rural Southwestern Uganda suggests that young people with HIV are more likely to engage in risky sexual behavior if they are ART naïve.18 It is unclear whether high consistent condom use would be observed among OS-YP on ART in Uganda. Studies done in Europe,19 Thailand20 and Nigeria21 show an increase in inconsistent condom use among patients on antiretroviral therapy. An increase in inconsistent condom use among people on ART not only poses a risk to those on ART by making them susceptible to HIV superinfection (infection of an HIV positive individual with another strain of the virus) and drug-resistance, but also can be a public health threat which could lead to the spread of ART resistant strains to their partners and the general public.19,22,23
Uganda’s Consolidated Guidelines for HIV prevention, care and treatment indicate that the prevalence of sexually transmitted infections (STIs) among people on ART and those not on ART is equally high.24 It is against this background that health workers delivering HIV services to young people on ART are encouraged to provide adolescent-friendly risk-reduction HIV prevention interventions (such as encouraging consistent condom use among sexually active young people) to prevent HIV re-infection, teenage pregnancy and other STIs.24 Whereas there are some studies carried out on condom use in young people in Uganda, there is almost no literature on consistent condom use not only among the general category of sexually active young people on ART but also out-of-school young people on ART. Therefore, this study intended to investigate the factors associated with consistent condom use among 15–24 year old OS-YP on ART in Central Uganda. This would contribute to the existing knowledge on HIV management in young people in Uganda and inform the effective consistent condom use promotion interventions in sexually active young people on ART.
Methodology
Study Setting and Population
The study was conducted among 357 sexually active OS-YP aged 15–24 years, who had been on ART for over 12 months and did not intend to have babies in that period. They were recruited from seven districts of Central Uganda (Kassanda, Kyotera, Luwero, Mityana, Mubende, Mukono, and Wakiso) between May and July 2019. The 2019 Uganda Population HIV Impact Assessment (UPHIA) noted that the Central region of Uganda, which includes 13 districts (Butambala, Gomba, Mpigi, Bukomansimbi, Kalangala, Kalungu, Lwengo, Lyantonde, Masaka, Rakai, Kyotera, Sembabule, and Wakiso) had the highest prevalence (8%) of HIV compared with the other nine regions of Uganda.8 In addition, Uganda’s Ministry of Health indicated that Central region 1 is among the three regions (Kampala, Central 1, and Southwestern regions) that together have over 50% of the total number of young people on ART in Uganda. Central Region 1 was therefore selected for this study since it has a considerable number of young people on ART who can easily be accessed.
Study Design, Study Duration and Sampling Method
This was a quantitative descriptive cross-sectional study conducted among sexually active OS-YP on ART. The data were collected between May and July 2019. The Central region was purposefully selected since the 2019 UPHIA report indicated that this region had the highest number of young people (aged 15−24 years) on ART compared with other regions of Uganda. The study utilized a multi-level sampling procedure to select the seven districts that were included in the study, the 21 health facilities, and the 357 study participants. At all levels, simple random sampling was done using random number generators through Microsoft Excel. Fifty-one (51) participants were drawn from every district that participated in the study, with each participating health facility contributing 17 respondents to the study sample. There was no major difference in terms of HIV services provided in the participating districts. The selection criteria of study participants were based on: OS-YP (aged 15−24 years) that turned up for ART services on the day of data collection and had been on ART for 12 months and above; with no intentions of having a baby in that period and provided informed consent, were enrolled in the study (Figure 1).
 |
Figure 1 Selection Criteria. |
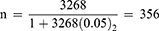
The sample size was determined using Israel’s (1992) formula. According to the Baseline Assessment of Access to HIV Testing, Care and Treatment among Adolescents in Uganda,25 the estimated number of young people receiving ART in Central Region 1 was 3268. After establishing the population size, the researchers established the Margin of Error or Confidence Interval which is 0.05. A sample size of 356 was calculated using the Israel formula:26
Where n = Sample Size
N = Size of the Target Population (which is 3268)
e = Margin Error/Level of Precision (which is 0.05)
So, the sample size is 356 respondents.
Data Collection
Data were collected using a structured questionnaire administered by the researchers and research assistants who spoke both English and a local language (Luganda).
The questionnaire was initially prepared in English and translated into the local language (Luganda) to obtain the required information from the respondents and was translated back to English to check for any inconsistencies or distortions.
The researchers pre-tested the data collection tool on a sample of 20 respondents (out-of-school young people receiving care at Mildmay Uganda, a peri-urban tertiary HIV care facility). After pre-testing, ambiguous items or questions were omitted.
The first section of the questionnaire included details about the person collecting data and health facility details. The second section contained 11 questions about socio-demographic characteristics of the respondent, while the third section contained 13 Likert scale questions and nine short-answer questions about the knowledge, skills, and attitudes of respondents on ART. The fourth section, that explored the factors influencing consistent condom use among study respondents, had 19 Likert scale questions with 14 short-answer questions. The last section, that explored the consistent condom use of study respondents, had six short-answer questions. In addition, in various sections of the questionnaire, there were closed questions that required ‘Yes’ or ‘No’ responses; while other questions required the respondents to choose from the given alternatives. There were also open questions that required short answers from the respondent. Such responses complemented the responses from closed questions. The questions were carefully constructed to capture relevant information concerning study objectives.
Study Measurements
The independent variables included: Age (15–19 years; 20–24 years); Sex (Male or Female); Religion (Adventist, Anglican, Pentecostal, Catholic, Muslim, Other); Marital status (Married/cohabiting, Single), Age of sex partner (15–19 years, 20–24 years, 25–29 years, >30 years), Source of HIV infection (from the mother, from partner, Other), Highest level of Education (No Education, Primary, Secondary); Staying with (Parents, Relative(s), Partner, Alone); Employment status (Not employed, Employed); Residence (Urban or Rural); Period on ART (1–4 years, 5–9 years, >10 years); Number of sexual partners (None, One, More than one); Type of partner (Casual, not casual), Knowledge on condom use [questions 14–18]; Attitude towards condom use (Negative, Positive [questions 19–24]); Perceived nature of service delivery (Poor, Good [questions 40–54]); Perceived level/number of staffing at health facility (Insufficient, Sufficient [questions 34–39]); Perceived level of health worker knowledge on sex education (Low, High [questions 55–59]). Perceived social support (Supportive, Not supportive [questions 60–67]). The dependent variable (Condom use) was binary whereby 0 = No; while 1 = Yes. The study variables, their categories and description are shown in Table 1.
 |
Table 1 Study Variables |
Data Management and Analysis
The completed questionnaires were checked for consistency and completeness on the day of data collection and errors were corrected in the field. The collected data were then sorted, coded, and entered into STATA version 14 which was used to summarise and analyze data. Descriptive statistics were produced for univariate analysis in the form of frequencies and mean standard deviations (SD). Cross-tabulation with a Chi-square statistic test was used to establish association between variables and condom use at last sexual intercourse in the past 12 months. Nine variables (highest level of education attained, residence, marital status, period on ART, source of HIV infection, age of sexual partners, perceived level of staffing at health facility, perceived level of health worker knowledge on sex education and perceived level of support from community social network) were significant at bivariate analysis and were included at multivariable analysis. Variables significant at bivariate analysis (highest level of education, employment status, residence and perceived level of staffing at health facility) were included in multivariable logistic regression after a multicollinearity check (Figure 2). Employment status was also included in the multivariable analysis because p = 0.08, was close to 0.05. Multivariable logistic regression was used to establish the association of various factors to consistent condom use among OS-YPs on ART. Statistical significance was set at p <0.05.
 |
Figure 2 Multicollinearity Check. |
Results
A total of 364 respondents were approached, seven did not consent while 357 consented to participate in the study. The response rate was 98%. Among the reasons they gave for not participating included: some said they did not have time for the questionnaire; others considered participating in the study would be intruding in their privacy while others wanted to be paid to participate in the study. However, the enumerators at the health facilities ensured that they reached out to the required number of participants. The data collection tool had 75 questions and it took an average of 50–70 minutes to complete it. On average, 1–5 questionnaires were filed per day. Since one day is scheduled for ART services for young people at most health facilities, data collection took about four weeks per health facility.
Socio-Demographic Characteristics of Study Respondents
Table 2 describes the characteristics of study participants. Of the 357 participants, 73% (n = 261) were females. The age range of study participants was between 15 and 24 years old (with a mean of 20±3 years) where 55% (n = 196) were aged 20–24 years. In addition, the age of sexual partners of sexually active OS-YP (as reported by participants) ranged from 15–52 years (with an average mean of 26±5 years). A total of 167 participants (47%) had completed senior secondary education school level and 154 (43%) had completed primary school education level, while 10% (n = 36) never went to school. Table 3 describes condom use among OS-YP on ART where 49% (n = 175) said they did not use condoms in the past 12 months.
 |
Table 2 Socio-Demographic Characteristics of Study Participants |
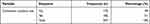 |
Table 3 Consistent Condom Use Among Out-of-School Young People on ART |
Factors Associated with Consistent Condom Use
Table 4 describes the bivariate analysis of the factors that were significantly associated with consistent condom use among study participants. The factors that were significantly associated with consistent condom use among study participants included: highest education level, residence, marital status, the period a participant had stayed on ART, the perceived source of HIV infection, age of sexual partner(s), health worker factors, health education factors as well as the community support factors, such as peer support. After adjusting for confounding variables, in multivariable logistic regression analysis (Table 5), level of education, employment status, residence, and health worker factors were significantly associated with consistent condom use among the OS-YP on ART. Participants with primary school education level had 21% lower odds of safer sex compared with those with no education (Odds = 0.21 [aOR: 0.07–0.69], p = 0.010). Participants who were employed were significantly (Odds = 2.12 [aOR: 1.06–4.26], p = 0.034) more likely to use condoms consistently than the unemployed. In addition, participants in rural areas were significantly (Odds = 2.46 [aOR: 1.19–5.10], p = 0.016) more likely to consistently use condoms than their counterparts in urban settings, whereas participants who believed enough health workers were providing reproductive health services to them, were six times (Odds = 6.08 [aOR: 1.05–35.22], p = 0.044) more likely to consistently use condoms than those who said they had insufficient health workers.
 |
Table 4 Association Between Consistent Condom Use and Various Factors (Bivariate Analysis) |
 |
Table 5 Multivariable Logistic Regression Model for Factors Associated with Condom Use Among Out-of-School Young People on ART in Central Uganda |
Discussion
Despite the fact that ART has proved to be an effective biomedical HIV prevention strategy, the WHO also recognises that if health workers integrate consistent and correct condom use in the HIV prevention intervention services, this would help reduce HIV transmission.5,27 Available literature indicates that condom use is the keystone of HIV prevention especially among the sexually active populations, in most countries.1 So, promotion of condom use through awareness campaigns and provision of free condoms are critical in behavioral change and HIV risk reductions.1,28,29 Contrariwise, inconsistent condom use by people living with HIV and/or on ART worsens HIV infection by increasing new HIV dug-resistant strains. This study established key findings on the factors associated with condom use among OS-YP on ART in Central Uganda.
This study found that a significant number of study participants (49%: n = 175) did not consistently use condoms. Despite the critical desire for people living with HIV to engage in safer sexual practices, particularly, correct and consistent condom use, the proportion of OS-YP on ART that consistently use condoms was not significant enough to contribute to the ending of HIV by the year 2030 (Table 3). The study findings indicated that fear of being dropped by a sexual partner, non-disclosure of HIV serostatus to the partner, and poverty (desire to access the basic needs especially among females) were the common reasons for inconsistent use of condoms. Other participants did not see the need for condom use since their partners were also HIV positive. The findings of this study are consistent with those from Ethiopian studies30,31 where many young people engaged in unsafe sexual activities. In a study by Mosisa et al., 32.9% of the 337 participants did not use condoms.30 A study by Molla and Gelagay found that 38% of 513 study participants (aged 18–29 years) on ART did not use condoms because they had not disclosed their HIV status to their sexual partners and others had fellow HIV positive partners.30 Similarly, an Indian study32 found that 24% of the 200 sexually active respondents engaged in unsafe sexual activity, just like in a Rwandan study33 where 63% of the 384 sexually active study participants (aged 15–49 years) did not use condoms; a study in Vietnam34 found that 60.9% of those on ART (n = 1133) inconsistently used condoms; a Malawian study35 found that 76% of study participants engaged in inconsistent condom use and another study in Botswana36 found that 79% of 979 study participants engaged in unsafe sexual activities. Consumption of alcohol was identified as one of the reasons for inconsistent condom use.
In a study carried out in South Africa, among 253 young people on ART, aged 18–25, 63% had not used condoms in the previous sexual encounter due to fear of abandonment from sexual partners, stigma and discrimination, and partner violence. In Malawian37 and Rwandan studies38 among young people on ART, low condom use was reported. This shows that, much as there are some OS-YP on ART that did not consistently use condoms, there were as well others who were consistently using condoms. Therefore, health workers need to strengthen the peer-led approach in HIV prevention and care services39 for young people to contribute to the achievement of ART goals.
Unlike the previous studies40,41 that have reported participants who have attained higher education level were more likely to use condoms consistently compared with lower educational status participants, this study did not find a significant association between the highest level of education attained and and consistent condom use. Study findings have shown that participants who completed or attained primary education engaged more in inconsistent condom use, unlike their counterparts who did not go to school. Such finding is consistent with a study carried out in Ethiopia where 75% (n = 19,148) respondents had engaged in unsafe sexual activity in the past 12 months and those with higher educational attainment had higher likelihood of engaging in unsafe sex (OR = 3.1; 95% CI: 2.33–3.99) compared with their less-educated counterparts.42 Probably, this disparity might be due to the difference in study setting, sample size, and the methods used. However, it shows that those running HIV programs should use the same level of effort in their SRH services to young people on ART irrespective of education level.
Consistent with studies carried out in Zambia,43 Kenya and Malawi,44,45 the findings of this study indicate that living in urban areas was associated with higher odds of inconsistent condom use compared with rural settings. This is consistent with the UNAIDS report which noted that 42% of young people aged 15–24 years residing in urban areas engage in unsafe sexual intercourse compared with 30% in rural areas. Unmet needs relating to housing, food, and health care were cited as having a positive association with unsafe sexual activities among urban young people. This has implications for social-economic interventions to address the unique needs of young people on ART, especially those in urban centers.
Further still, findings of this study showed a significant association between unemployment and inconsistent condom use among sexually active young people on ART compared with those who were employed. Inability to access basic needs (poverty) was identified as a major factor that influenced most unemployed OS-YP on ART into inconsistent condom use. With unemployment, a person can hardly access the basic needs45,46 and this would lead the person to engage in transactional sex46 to access basic needs such as food, clothing, money for rent, among others. In circumstances of transactional sex, consistent condom use is less likely and this would easily fuel the spread of HIV,47 especially where the male is infected and is not willing to use a condom. So, the public health experts, especially those in HIV programming and policymaking, should pay special attention to interventions to fight poverty, especially among sexually active young people, since it is entwined with inconsistent condom use among OS-YP on ART.
Findings of this study further indicate that respondents who received ART services from health facilities that were perceived to have inadequate number of health workers were six times more likely to engage in inconsistent condom use compared with their counterparts who received services from health facilities with adequate health workers. The WHO emphasizes that health workers are the most essential element in the health system building blocks.48,49 Relatedly, studies demonstrate a significant relationship between the numbers of health workers and health-care outcomes.50,51 The WHO notes that ART is highly labor-intensive, thus requires a more skilled health workforce to address the diverse health-care needs of PLWH in a holistic way;52 it is the same case with promotion of condom use that requires discussing correct and consistent use, benefits of condom use, dispelling the myths around condoms, demonstrating negotiation skills for condom use and provision of free condoms. So, policymakers need to recruit the minimum number of health workers at each facility to strengthen the provision of youth-friendly services that in the context of HIV epidemic control if we are to eliminate HIV by the year 2030.
Study Limitations
This study’s methods had some limitations. The study did not include partners of respondents and this provided a one-sided response on consistent condom use among study participants. Secondly, this being a cross-sectional quantitative study, some qualitative data that complemented the quantitative data would have been missed. More details on “how”, or “why” relating to consistent condom use among out-of-school young people on ART could have been missed. Thirdly, there could have been selection bias emanating from the convenience sampling technique utilized during data collection and this reduced the generalisability of our results. Fourthly, our study methods relied on participants’ ability to recall their consistent condom use and other elements of their activity; such responses were subject to social desirability bias and, because of the retrospective nature of some measures, responses are also subject to recall bias. Because we used a cross-sectional study design, we could not draw causal conclusions. Fifthly, the consideration of correct condom use, a major component of condom use, was not studied. The phenomenon is complex to measure and to objectively self-report, thus its elimination from the study. Lastly, the study did not consider use of other contraceptives apart from condom use. Despite these limitations, the findings of this study provide evidence to inform advocacy, policy, and program design and research in the context of HIV prevention and care among young people on ART.
Conclusion
Our study highlights that, generally, there was a high prevalence of inconsistent condom use among out-of-school sexually active young people on ART in Central Uganda. This poses a big public health threat since it could contribute to an increase in the spread of HIV. Results suggest the need to recruit adequate number of health providers so as to strengthen the promotion of consistent condom use among sexually active people on ART.
Abbreviations
ART, antiretroviral therapy; HIV, human immunodeficiency virus; HIVDR, HIV drug resistance; OS-YP, out of school young people; PLWH, people living with HIV; SRHR, Sexual and Reproductive Health Rights.
Data Sharing Statement
The corresponding author will share the data set in this study upon reasonable request.
Ethics Approval and Consent to Participate
The study was conducted following the internationally acceptable ethics of scientific research. To confirm that all methods were carried out in accordance with relevant guidelines and regulations, the study and all documents involved, were approved by Mildmay Uganda Research Ethics Committee (REF 0303-2019), an accredited Ethics research body by the Uganda National Council of Science and Technology. All experiments and handling of data were conducted in accordance with the Declaration of Helsinki. After obtaining ethical clearance, further study approval was provided by the Uganda National Council of Science and Technology (UNCST), District Health officers of the targeted districts, and Hospital administrators and managers before engaging the potential study respondents. Written informed consent, which was both in English and Luganda languages, was obtained from all respondents. Participants aged 14–17 years were considered to be mature minors and provided informed consent independent of parents. Uganda’s National Guidelines for Research involving Humans as Research participants53 recommend that participants aged 14–17 years can be considered mature minors if they have a sexually transmitted infection. Further, the guidelines recommend that mature minors can provide independent consent if there is justification for not involving parents. The study focused on sexual practices of the OS-YPs with HIV infection. Therefore, it was justified not to involve parents to preserve the confidentiality of the sexual practices and HIV status of the participants.
Acknowledgments
We would like to extend our gratitude to the OS-YP on ART who participated in this study. We are deeply indebted to study participants, research assistants, Mildmay Uganda Internal Review Board, District Health Officers in the districts where this study was conducted and health workers in health facilities where data were collected.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition, of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare no conflicts of interest.
References
1. Lépine A, Treibich C, Ndour CT, Gueye K, Vickerman P. HIV infection risk and condom use among sex workers in Senegal: evidence from the list experiment method. Health Policy Plan. 2020;35(4):408–415. doi:10.1093/heapol/czz155
2. UNAIDS. Joint United Nations Programme on HIV/AIDS. Condoms: The Prevention of HIV, Other Sexually Transmitted Infections and Unintended Pregnancies. UNAIDS; 2016:1–48.
3. Galvão LW, Oliveira LC, Díaz J, et al. Effectiveness of female and male condoms in preventing exposure to semen during vaginal intercourse: a randomized trial. Contraception. 2005;71(2):130–136. doi:10.1016/j.contraception.2004.08.008
4. Nelson AL. Male Condoms. Contraception. Springer; 2011:114–122.
5. Ayele WM, Tegegne TB, Damtie Y, Chanie MG, Mekonen AM, Ekwunife OI. Prevalence of consistent condom use and associated factors among serodiscordant couples in Ethiopia, 2020: a mixed-method study. Biomed Res Int. 2021;2021:1–10. doi:10.1155/2021/9923012
6. UNAIDS. On the to End AIDS. UNAIDS; 2016.
7. Duesberg P. AIDS data. Science. 1995;268(5209):350–351. doi:10.1126/science.268.5209.350.b
8. Ministry of Health Uganda. Uganda Population - Based Hiv I Mpact a Ssessment. 2019:0–252.
9. World Health Organization. Technical brief. 2017.
10. Asio J, Watera C, Namuwenge N, et al. Population-based monitoring of HIV drug resistance early warning indicators in Uganda: a nationally representative survey following revised WHO recommendations. PLoS One. 2020;15(4):1–15. doi:10.1371/journal.pone.0230451
11. World Health Organization. HIV drug resistance report 2019. World Health Organization; 2019:68. Available from: http://www.who.int/hiv/pub/drugresistance/hivdr-report-2019.
12. Kirby D, Kirby D. The impact of schools and school programs upon adolescent sexual behavior The impact of schools and school programs upon adolescent sexual behavior. 2010:4499.
13. Mbalinda SN, Kiwanuka N, Eriksson LE, Wanyenze RK, Kaye DK. Correlates of ever had sex among perinatally HIV-infected adolescents in Uganda. Reprod Health. 2015;12:1–10.
14. Tarkang EE, Pencille LB, Dadah E, Nzegge MM, Komesuor J. Youths in urban Cameroon. J AIDS Clin Res. 2018;8688:1–12.
15. Nobelius AA, Kalina B, Pool R, et al. Delaying sexual debut amongst out-of-school youth in rural southwest Uganda Linked references are available on JSTOR for this article: Uganda. Culture Health Sexual. 2010;12(6):663–676.
16. Mee P, Fearon E, Hassan S, et al. The association between being currently in school and HIV prevalence among young women in nine eastern and Southern African countries. 2018:1–12.
17. Berhan A, Berhan Y. Is the sexual behaviour of HIV patients on antiretroviral therapy safe or risky in Sub-Saharan Africa? Meta-analysis and meta-regression. 2012:1–9.
18. Society for Adolescent Health and Medicine. Research poster presentations. J Adolesc Health. 2019;64(2):S97.
19. Cambiano V, O’Connor J, Phillips AN, et al. Antiretroviral therapy for prevention of HIV transmission: implications for Europe. Eurosurveillance. 2013;18(48). doi:10.2807/1560-7917.ES2013.18.48.20647
20. Thanawuth N, Rojpibulstit M. Sexual risk behaviors among HIV-patients receiving antiretroviral therapy in Southern Thailand: roles of antiretroviral adherence and serostatus disclosure. AIDS Care. 2016;28(5):612–619. doi:10.1080/09540121.2015.1120856
21. Ebuenyi ID, Ogoina D, Harry TC. Predictors of unprotected sexual intercourse among HIV-infected patients receiving antiretroviral drugs in the Niger Delta Region of Nigeria. AIDS Care. 2018;30(3):296–299. doi:10.1080/09540121.2017.1368443
22. Redd AD, Quinn TC, Tobian AAR. Frequency and implications of HIV superinfection. Lancet Infect Dis. 2013;13(7):622–628. doi:10.1016/S1473-3099(13)70066-5
23. Sakthivel V, Krishnasamy V, Mehalingam V. Level of medication adherence and its associated factors among patients receiving antiretroviral therapy at a tertiary care hospital in South India. J Caring Sci. 2020;9(2):93–97. doi:10.34172/JCS.2020.014
24. GAC. National HIV and AIDS strategic plan. 2016:1–8.
25. King CA, O’mara RM, Hayward CN, Cunningham RM. Adolescent assessment report. 2009:1–16.
26. Polonia G. Analysis of sample size in consumer surveys. 2013.
27. Enegela JE. Rates of condom use among HIV positive patients on ART in Nasarawa Eggon North Central Nigeria. Biomed J Sci Tech Res. 2019;18(5):0–6.
28. Ministry of Health. Consolidated guidelines for prevention and treatment of HIV and AIDS in Uganda; 2020. Available from: http://library.health.go.ug/publications/hivaids/consolidated-guidelines-prevention-and-treatment-hiv-uganda.
29. Ministry of Health. Consolidated guidelines for prevention. 2018;2:2016–2019.
30. Molla AA, Gelagay AA. Risky sexual practice and associated factors among HIV positive adults attending anti-retroviral treatment clinic at Gondar University Referral Hospital, Northwest Ethiopia. PLoS One. 2017;12(3):1–12. doi:10.1371/journal.pone.0174267
31. Mosisa G, Woldemichael K, Ayalew F. Risky sexual behavior and associated factors among antiretroviral therapy attendees in nekemte referral hospital, Western Ethiopia: a cross-sectional study. HIV/AIDS Res Palliat Care. 2018;10:125–131. doi:10.2147/HIV.S159670
32. Shukla M, Agarwal M, Singh JV, Tripathi AK, Srivastava AK, Singh VK. High-risk sexual behavior among people living with HIV/AIDS attending tertiary care hospitals in district of Northern India. Indian J Sex Transm Dis. 2016;37(1):46–51. doi:10.4103/0253-7184.176212
33. Determining risk perception regarding unprotected sex among people living with HIV presenting to Butare University Teaching Hospital, Huye District, Rwanda Fundi Ngongo Emmanuel. MPH/0190/2012 A Thesis Submitted in Partial Fulfillment of the Requirem. 2016.
34. Minh T, Vu T, Boggiano VL, Tran BX, Nguyen LH. Sexual risk behaviors of patients with HIV/AIDS over the course of antiretroviral treatment in Northern Vietnam. 2018.
35. Zgambo M, Kalembo FW, Mbakaya BC. Risky behaviours and their correlates among adolescents living with HIV in sub-Saharan Africa: a systematic review. Reprod Health. 2018;15(1):1–12. doi:10.1186/s12978-018-0614-4
36. Wirth K, Kadima E, Pretorius-holme M. Self-reported risky sexual practices among adolescents and young adults in Botswana. South Afri J HIV Med. 2019;20:1–8.
37. Haddad LB, Tang JH, Krashin J, et al. Factors associated with condom use among men and women living with HIV in Lilongwe, Malawi: a cross-sectional study. BMJ Sex Reprod Health. 2018;44(1):42–53.
38. Van Nuil JI, Mutwa P, Asiimwe-Kateera B, et al. “Let’s talk about sex”: a qualitative study of Rwandan adolescents’ views on sex and HIV. PLoS One. 2014;9(8):6–11. doi:10.1371/journal.pone.0102933
39. Tapera T, Willis N, Madzeke K, et al. Effects of a peer-led intervention on HIV care continuum outcomes among contacts of children, adolescents, and young adults living with HIV in Zimbabwe. Glob Health Sci Pract. 2019;7:575–584. doi:10.9745/GHSP-D-19-00210
40. Kefale B, Kefale Y. Knowledge, attitude, practice and determinants of condom use among people living with HIV/AIDS in Gondar University Hospital, North West Ethiopia. J Phys Pharm Adv. 2013;3(10):247–260.
41. Shewamene Z, Legesse B, Tsega B, Bhagavathula AS, Endale A. Consistent condom use in HIV/AIDS patients receiving antiretroviral therapy in northwestern Ethiopia: implication to reduce transmission and multiple infections. HIV/AIDS Res Palliat Care. 2015;7:119–124. doi:10.2147/HIV.S79122
42. Berhan Y, Berhan A. A meta-analysis of risky sexual behaviour among male youth in developing countries. AIDS Res Treat. 2015;2015. doi:10.1155/2015/580961
43. Nakazwe C, Michelo C, Sandøy IF, Fylkesnes K. Contrasting HIV prevalence trends among young women and men in Zambia in the past 12 years: data from demographic and health surveys 2002–2014. BMC Infect Dis. 2019;19(1):1–9. doi:10.1186/s12879-019-4059-3
44. Kamndaya M, Vearey J, Thomas L, Kabiru CW, Kazembe LN. The role of material deprivation and consumerism in the decisions to engage in transactional sex among young people in the urban slums of Blantyre, Malawi. Glob Public Health. 2016;11(3):295–308. doi:10.1080/17441692.2015.1014393
45. Muiya BM. The nature, challenges and consequences of urban youth unemployment: a case of Nairobi City, Kenya. Univ J Educ Res. 2014;2(7):495–503.
46. Hammar A, Janlert U. Unemployment and sexual risk-taking among adolescents Author (s): Anne Hammarström and Urban Janlert Source. Scand J Soc Med. 1997;25(4):266–270. doi:10.1177/140349489702500409
47. Austin KF, Berndt V, Berndt V. Trading sex for security: unemployment and the unequal HIV burden among young women in developing nations. Int Sociol. 2017;32:343–368. doi:10.1177/0268580917693172
48. World Health Organization. Global Strategy on Human Resources for Health: Workforce 2030. World Health Organization; 2016:64.
49. Mutale W, Bond V, Mwanamwenge MT, et al. Systems thinking in practice: the current status of the six WHO building blocks for health system strengthening in three BHOMA intervention districts of Zambia: a baseline qualitative study. BMC Health Serv Res. 2013;13(1):1–9. doi:10.1186/1472-6963-13-291
50. Nguyen MP, Mirzoev T, Le TM. Contribution of health workforce to health outcomes: empirical evidence from Vietnam. Hum Resour Health. 2016;14(1):1–11. doi:10.1186/s12960-016-0165-0
51. Hewitt C, Lankshear A, Kazanjian A, Maynard A, Sheldon T, Smith K. Health service workforce and health outcomes. 2005:1–148.
52. World Health Organization. Scaling Up HIV/AIDS Care: Service Delivery & Human Resources Perspectives. World Health Organization; 2004:1–100.
53. Uganda National Council for Science and Technology (UNCST). National guidelines for research involving humans as research participants. Kampala Uganda. 2014.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.