Back to Journals » Patient Preference and Adherence » Volume 15
Factors Associated with Anticoagulation Adherence in Chinese Patients with Non-Valvular Atrial Fibrillation
Authors Song T , Xin X, Cui P , Zong M , Li X
Received 13 October 2020
Accepted for publication 25 December 2020
Published 1 March 2021 Volume 2021:15 Pages 493—500
DOI https://doi.org/10.2147/PPA.S285020
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Naifeng Liu
Ting Song,1,* Xiao Xin,2,* Peirong Cui,1 Mingcan Zong,1 Xianhua Li3
1School of Nursing, Shanghai Jiaotong University, Shanghai, People’s Republic of China; 2Department of Oncology, Ruijin Hospital, Shanghai Jiaotong University School of Medicine, Shanghai, People’s Republic of China; 3Department of Outpatient Office, Ruijin Hospital, Shanghai Jiaotong University School of Medicine, Shanghai, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xianhua Li
Department of Outpatient Office, Ruijin Hospital, Shanghai Jiaotong University School of Medicine, Shanghai, People’s Republic of China
Tel +86 18917762081
Email [email protected]
Purpose: Inadequate medication adherence among patients with non-valvular atrial fibrillation (NVAF) will directly affect the efficacy and safety of anticoagulation therapy, leading to a considerable increase in the risk of ischemic stroke and death. In this study, we aim to investigate medication adherence and identify the influencing factors, including social-demographic, disease-related information and self-efficacy.
Patients and Methods: We recruited 170 patients with NVAF from a tertiary hospital atrial fibrillation outpatient clinics and cardiology ward from June 2020 to September 2020. Patients who had been taking oral anticoagulation medication for at least 3 months were included. And Morisky medication adherence scale (MGL) was used to assess the adherence to anticoagulants, which scores < 4 were considered as low adherence.
Results: Fifty (29.4%) NVAF patients had a MGL score< 4. Monthly income, types of comorbidities, number of drugs, and self-efficacy were determinants of anticoagulation adherence. Binomial logistic regression showed that patients had been prescribed more durgs (OR: 3.51, p=0.002), had high monthly income (OR: 7.87, p=0.001), without other diseases (OR: 8.00, p=0.005), and with higher self-efficacy (OR: 1.42, p=0.001) showed high adherence.
Conclusion: Number of drugs, types of comorbidities, monthly income, and self-efficacy were associated with the adherence of non-vitamin K antagonist oral anticoagulants (NOACs).
Keywords: atrial fibrillation, medication adherence, anticoagulation, non-vitamin K antagonist oral anticoagulants, determinants
Introduction
Atrial fibrillation(AF) includes non-valvular atrial fibrillation (NVAF) and valvular atrial fibrillation (VAF). There is an incidence rate of 77 per 10,000 people among Chinese people over 35 years old. AF significantly increases the risk of stroke by about five times. Appropriate oral anticoagulant (OAC) therapy can positively prevent the stroke.1–3 OAC treatment can prevent most ischemic stroke in AF patients and can extend their survival time.4,5 Currently, vitamin K antagonist (VKA) and non-vitamin K antagonist oral anticoagulants (NOACs) are the primary drugs used in the treatment for NVAF. NOACs is an appropriate alternative to prevent ischemic stroke.6 The 2016 European Society of Cardiology (ESC) Atrial Fibrillation Management Guidelines have expressed a preference for NOACs over VKA in stroke prevention for AF patients.7 World Health Organization (WHO) defines adherence as the extent of taking medications as prescribed by heath care professionals. However, patients with NVAF usually had low adherence, leading to a significantly increased risk of stroke.8,9 Moreover, some studies have found that the factors such as gender, age, educational level, and economic status can affect anticoagulation adherence of NVAF patients,9–11 while other factors, such as clinical factors and self-efficacy can also affect medication adherence.12
Self-efficacy is an individual’s subjective judgement on whether he or she can complete a specific task or achieve a set goal in a particular situation.13 Many studies have shown that the level of self-efficacy affects patients’ medication adherence. Research by Fang et al showed that the self-efficacy level of AF patients affects their adherence to anticoagulation, the higher self-efficacy, the better anticoagulation adherence.12
Through reviewing previous publications, we found that studies on anticoagulation adherence in NVAF patients few focused on self-efficacy, which is an essential factor influencing adherence in other populations. Therefore, we designed a cross-sectional study to investigate medication adherence and explore its independent predictors among patients with NVAF in China.
Study Design
This study was a cross-sectional study conducted in NVAF outpatient clinics and cardiology ward at the RuiJing hospital Shanghai Jiao Tong University School of Medicine, China. Inclusion criteria were as follows: (a) aged more than 18 years, (b) diagnosed with NVAF, (c) had been taking oral anticoagulation medication for at least 3 months, (d) currently taking NOACs for NVAF treatment. Patients diagnosed with cognitive impairment, valvular atrial fibrillation, and hard to understand the content of questionnaires were excluded. All included patients were given informed consent and signed an informed consent form.The patients were asked to fill out three questionnaires, included social-demographic information, self-efficacy scale and Morisky adherence scale. Futhermore, disease-related information were collected from medical records.
Measurements
The social-demographic and disease-related information contains 17 variables, including age, gender, marital status, education level, monthly income (less than 367€, 367–612€, above 612€), residence (town and country), employment status (employed and unemployed) and insurance type (urban employee/resident basic medical insurance, new rural cooperative medical insurance), atrial fibrillation type, EHRA symptom classification, duration of NVAF, duration of medication, radiofrequency ablation surgery in the past, adverse events, number of drugs, types of complications, and CHA2DS2-VASc score. Self-efficacy in the medical therapywere evaluated by the Self-Efficacy for Appropriate Medication Use Scale,14 compiled by Risser et al.15 This scale includes one dimension, 13 items. Each item used a 3-point Likert scale and ranging from 1 - 3, which 1 is not confident, 2 is relatively confident, and 3 is very confident. Higher scores indicate a higher level of self-efficacy in medication adherence. The total score ranged from 13 to 39 points. We used Morisky medication adherence scale (MGL) to evaluate medication adherence. For four items, if the patient's choice is “yes,” it is counted as 0 point, and the option is “no” counted as 1 point, the highest point is 4 points.Based on the scores, we divided the patient’s adherence into two levels: below 4 points were defined as low adherence, and 4 were high adherence.16 A total of 170 patients were included. The detailed flow chart is shown in Figure 1.
 |
Figure 1 Sample selection flowchart. |
Ethics Approval
This study was conducted in accordance with the Declaration of Helsinki and approved by the Clinical Trial Ethics Committee of the RuiJing Hospital Shanghai Jiao Tong University School of Medicine. (No.2019227). The attributes, benefits, uses and disadvantageous effects of the study were explained to all participants and informed consent was also obtained. Patients have the right to refuse to fill in questions that he/she does not want to answer. In order to protect the privacy of patients, we use numbers to code these questionnaires.
Statistical Analysis
We used IBM SPSS20.0 for data entry and analysis. Mean, standard deviation (SD), frequency and percentage were used for descriptive statistics. For the two group comparisons(low adherence vs high adherence), we used the chi-square test for categorical variables, and the Student's t-tests or Wilcoxon rank sum test for continuous data. Multivariate analysis was performed by binomial logistic regression, which P<0.05 was considered statistically significant.
Results
Medication Adherence According to Morisky Medication Adherence Scale (MGL)
Adherence to anticoagulation therapy, according to the MGL, 50 (29.4%) patients were defined as low adherers, 120 (70.6%) were defined as high adherers.Main reason for poor adherence was forgeting to take the medicine (21.20%), followed by stoping taking the medicine when they feel better (9.40%). The third reason was they stop taking the medicine when they feel worse (7.60%), and finally, sometimes they were careless to taking the medicine (7.10%), which are shown in Table 1.
 |
Table 1 Anticoagulation Adherence According to Morisky Medication Adherence Scale (MGL) |
Sociodemographic and Clinical Disease Characteristics of Chinese NVAF Patient
The sociodemographic and clinical characteristics of the participants are shown in Table 2. Among the 170 participants, 99 (58.2%) were male, 71 (41.8%) were female, and 158 (92.9%) lived in the town. 89 were taking three or more drugs. 71 (41.8%) had undergone radiofrequency catheter ablation (RFCA), and 91 (53.5%) had more than one complication. 129 (75.9%) were diagnosed with paroxysmal atrial fibrillation, 41 (24.1%) were persistent atrial fibrillation. 138 (81.2%) had the CHA2DS2-VaSc score more than 2. Monthly income, number of drugs and types of complications were significantly difference between two groups while others were not, which are shown in Table 3.
 |
Table 2 Sociodemographic and Clinical Characteristics of Patients (n=170) |
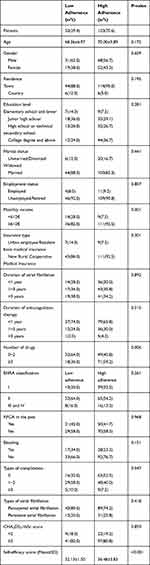 |
Table 3 Characteristics of the Patients According to Anticoagulation Adherence |
Results of Logistic Regression
Logistic regression showed that high adherence was associated with higher self-efficacy (OR=1.42; 95% CI=1.15–1.74, p=0.001). As shown in Table 4, patients who take three or more drugs were more adherent to anticoagulation therapy than those less than three (OR=3.51; 95% CI=1.57–8.01 p=0.002). And patients whose monthly income is more than 612€ showed better adherence than patients with a monthly payment less than 612€ (OR=7.87, 95% CI=2.68–23.11 p=0.001). The adherence of patients without other diseases is better than patients with more than 3 diseases (OR=8.00, 95% CI= [1.90–33.71]). Still, there is no difference of adherence between patients with one or two diseases and those with more than three diseases.
 |
Table 4 Logistic Regression: Factors Influencing NOACs Adherence |
Discussion
In our study, patients’ medication adherence was evaluated by MGL and we found that almost 30% of Chinese NVAF patients had low adherence, which was similar to the adherence rate in other countries (21.1% to 26.2%).17,18 Adherence was suboptimal in this study population. Compared with the results of other Chinese study, there were also specific differences,19 resulted from the different evaluation tools and the included populations. We found that the poor adherence of NVAF patients, in a large extent, is due to forgeting to take medication. E-health is an emerging field in the intersection of medical informatics, public health and business, referring to health services and information delivered or enhanced through the Internet and related technologies.20 Approaches such as e-health, including remote medication adherence monitoring system, short message service, medication reminder application (APP), were proven to be effortable at improving patient adherence.21,22 Therefore, we can try to make use of these reminder techniques to help patients improve adherence. Surprisingly, we found that the rate of non-adherence of NOACs was lower than the warfarin.23 One possible explanation was that the NOACs could make the blood concentration stable, do not require frequent blood tests, was much more convenient. Therefore, for physicians, if NVAF patients had low adherence to warfarin, they can consider prescribing NOACs for the patient according to their condition. For patients’ factors, previous studies had shown that being younger age, male, employed predicted of low adherence in NVAF patients.24,25 But our investigation found no correlation between age, gender, employment and adherence. One possible explanation was the sample size is small or the economic and cultural background differences between China and other countries. Besides, in our study, the educational level did not seem to affect adherence. And there was no relationship between marital status, residence, or insurance type, but monthly income, which was found to be related to adherence, and patients who had a higher monthly income showed better adherence. One possible explanation was the high price of NOACs. People with higher monthly payments can afford the cost of the drug and are more inclined to insist on taking the medication. And clinicians should help patients get more social support, such as the help of social charity organizations, to reduce their financial burden. Also, the remarkable discovery was patients with higher self-efficacy scores show better adherence, which had been reported in NVAF patients.26 Self-efficacy reflects one’s confidence in accomplishing things; thus, high self-efficacy of patients has the confidence to take medicine on time, under the condition of uncertainty and difficulty to insist on taking medicine. A previous study showed that the effectiveness of the self-efficacy enhancement program could effectively improve medication adherence in patients with acute myocardial infarction.27 Therefore, physicians can design relevant interventions to improve the self-efficacy of patients and further improve the adherence of patients with oral anticoagulants. For treatment-related factors, our study found that the adherence of patients taking more than 3 drugs is higher than that of less than 3, which is consistent with Bennish’s research.28 This may be explained by that patients taking more than one medication may remember that they need to take anticoagulants while taking other drugs . Clinicians and nurses should increase the frequency of assessing patients' adherence, as the guidelines recommended that adherence be evaluated on each visit.7 In our study, we also found that patients who had more diseases combined had low adherence, which may be related to the poor physical condition. Choosing the variable of self-efficacy is an advantage of this study. In contrast, previous studies have mostly considered the influence of demographic-related factors and disease-related factors on adherence. Furthermore, our study focused on NOACs adherence in NVAF patients in Shanghai, the southeast coastal city of China, which can reflect the adherence status of economically developed regions to a certain extent. This study also had certain limitations. This study only included patients from one tertiary hospital, which resulted in limited sample representation. There may be a selection bias in the research results. The research is a cross-sectional survey, it is difficult to obtain the causal relationship between variables. Therefore, the results of this research need to be further confirmed by future multi-center, longitudinal study and large-sample studies, or we could use the instrumental variables to prove the causality relationship in medication adherence.29,30 In summary, the adherence level of NOACs in patients with NVAF in Shanghai is suboptimal. Monthly income, number of drugs, types of complications, and self-efficacy are associated with adherence.
Highlights
- Poor oral anticoagulants in patients with non-valvular atrial fibrillation increase the risk of stroke and bleeding.
- Adherence was suboptimal in patients with NVAF; the proportion of non-adherent patients is about 30%.
- Monthly income, number of drugs, type of comorbidities, and self-efficacy are associated with NOACs adherence.
Abbreviations
NVAF, non-valvular atrial fibrillation; NOACs, non-vitamin K oral anticoagulants; RFCA, radiofrequency catheter ablation.
Acknowledgments
The author would like to thank Wu LQ, Jin Qi, Kang Lei, members of the graduate tutor group, and all patients involved. Ting Song and Xiao Xin are co-first authors for this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study received funding from the Scientific Research Project of Shanghai Jiaotong University (funding number: hlgy1904kygg).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Li Y, Wu YF, Chen KP, et al. Prevalence of atrial fibrillation in china and its risk factors. Biomed Environ Sci. 2013;26(9):709–716. doi:10.3967/0895-3988.2013.09.001
2. Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22(8):983–988. doi:10.1161/01.str.22.8.983
3. Giugliano RP, Ruff CT, Braunwald E, et al. Edoxaban versus Warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369(22):2093. doi:10.1056/NEJMoa1310907
4. Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383(9921):955–962. doi:10.1016/S0140-6736(13)62343-0
5. Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med. 2007;146(12):857. doi:10.7326/0003-4819-146-12-200706190-00007
6. Olesen JB, Sorensen R, Hansen ML, et al. Non-vitamin K antagonist oral anticoagulation agents in anticoagulant naive atrial fibrillation patients: danish nationwide descriptive data 2011-2013. Europace. 2015;17(2):187–193. doi:10.1093/europace/euu225
7. Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37(38):2893–2962. doi:10.1093/eurheartj/ehw210
8. Deshpande CG, Kogut S, Laforge R, et al. Impact of medication adherence on risk of ischemic stroke, major bleeding and deep vein thrombosis in atrial fibrillation patients using novel oral anticoagulants. Curr Med Res Opin. 2018;34(7):1285–1292. doi:10.1080/03007995.2018.1428543
9. Borne RT, O’Donnell C, Turakhia MP, et al. Adherence and outcomes to direct oral anticoagulants among patients with atrial fibrillation: findings from the veterans health administration. BMC Cardiovasc Disord. 2017;17(1):236. doi:10.1186/s12872-017-0671-6
10. Laliberté F, Nelson WW, Lefebvre P, et al. Impact of daily dosing frequency on adherence to chronic medications among nonvalvular atrial fibrillation patients. Adv Ther. 2012;29(8):675–690. doi:10.1007/s12325-012-0040-x
11. Emren SV, Senoz O, Bilgin M, et al. Drug adherence in patients with nonvalvular atrial fibrillation taking non-Vitamin K antagonist oral anticoagulants in Turkey: NOAC-TR.. Clin Appl Thrombosis/Hemostasis. 2018;24(3):525–531. doi:10.1177/1076029617693940
12. Fang SJ, Linzheng SG. Study on the relationship between warfarin anticoagulation compliance and self-efficacy in patients with non-valvular atrial fibrillation . Chin J Pract Nurs. 2010;(35):1–4. doi:10.3760/cma.j.issn.1672-7088.2010.12.040
13. Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. doi:10.1037//0033-295x.84.2.191
14. Dong XF, Liu YJ, Wang AX, et al. Psychometric properties of the Chinese version of the Self-Efficacy for Appropriate Medication Use Scale in patients with stroke. Patient Prefer Adherence. 2016;10:321–327. doi:10.3870/hlxzz.2015.11.047
15. Risser J, Jacobson TA, Kripalani S. Development and psychometric evaluation of the Self-Efficacy for Appropriate Medication Use Scale (SEAMS) in low-literacy patients with chronic disease. J Nurs Meas. 2007;15(3):203–219. doi:10.1891/106137407783095757
16. Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67–74. doi:10.1097/00005650-198601000-00007
17. Miyazaki M, Nakashima A, Nakamura Y, et al. Association between medication adherence and illness perceptions in atrial fibrillation patients treated with direct oral anticoagulants: an observational cross-sectional pilot study. PLoS One. 2018;13(9):e204814. doi:10.1371/journal.pone.0204814
18. Rossi AP, Facchinetti R, Ferrari E, et al. Predictors of self-reported adherence to direct oral anticoagulation in a population of elderly men and women with non-valvular atrial fibrillation. J Thromb Thrombolysis. 2018;46(2):139–144. doi:10.1007/s11239-018-1679-1
19. Qiao J, Bai YY, Ma JL, et al. Compliance of new oral anticoagulants in elderly patients with non-valvular atrial fibrillation: an analysis on influence factors. Chin J Evid Bases Cardiovasc Med. 2020;12(5):540–542. doi:10.3969/j.issn.1674-4055.2020.05.09
20. Eysenbach G. What is e-health? . J Med Internet Res. 2001;3(2):e20. doi:10.2196/jmir.3.2.e20
21. Desteghe L, Vijgen J, Koopman P, et al. Telemonitoring-based feedback improves adherence to non-vitamin K antagonist oral anticoagulants intake in patients with atrial fibrillation. Eur Heart J. 2018;39(16):1394–1403. doi:10.1093/eurheartj/ehx762
22. Guo Y, Chen Y, Lane DA, et al. Mobile health technology for atrial fibrillation management integrating decision support, education, and patient involvement: mAF App Trial. Am J Med. 2017;30(12):1388–1396. doi:10.1016/j.amjmed.2017.07.003
23. Zhao S, Zhao H, Wang X, et al. Factors influencing medication knowledge and beliefs on warfarin adherence among patients with atrial fibrillation in China[J. 2017;11:213–220. doi:10.2147/PPA.S120962
24. Suzuki T, Shiga T, Omori H, et al. Adherence to medication and characteristics of Japanese patients with non-valvular atrial fibrillation. J Cardiol. 2017;70(3):238–243. doi:10.1016/j.jjcc.2016.11.009
25. Gorst-Rasmussen A, Skjoth F, Larsen TB, et al. Dabigatran adherence in atrial fibrillation patients during the first year after diagnosis: a nationwide cohort study. J Thromb Haemost. 2015;13(4):495–504. doi:10.1111/jth.12845
26. Chen P, Wang T, Hsieh M, et al. Anticoagulation adherence and its associated factors in patients with atrial fibrillation: a cross-sectional study. BMJ Open. 2019;9(9):e29974. doi:10.1136/bmjopen-2019-029974
27. Polsook R, Aungsuroch Y, Thongvichean T. The effect of self-efficacy enhancement program on medication adherence among post-acute myocardial infarction. Appl Nurs Res. 2016;32:67–72. doi:10.1016/j.apnr.2016.05.002
28. Manzoor BS, Lee TA, Sharp LK, et al. Real-world adherence and persistence with direct oral anticoagulants in adults with atrial fibrillation. Pharmacotherapy. 2017;37(10):1221–30. doi:10.1002/phar.1989
29. Jiang Y, Ni W. Health care utilization and treatment persistence associated with oral paliperidone and lurasidone in schizophrenia treatment. J Manage Care Spec Pharm. 2015;21(9):780–792. doi:10.18553/jmcp.2015.21.9.780
30. Jiang Y, Weiyi N. Estimating the impact of adherence to and persistence with atypical antipsychotic therapy on health care costs and risk of hospitalization. Pharmacotherapy. 2015;35(9):813–822. doi:10.1002/phar.1634
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
