Back to Journals » International Journal of General Medicine » Volume 15
Factors and Outcomes Associated with Failed Noninvasive Positive Pressure Ventilation in Patients with Acute Respiratory Failure
Authors Liang YR, Lan CC, Su WL, Yang MC, Chen SY, Wu YK
Received 24 February 2022
Accepted for publication 23 August 2022
Published 12 September 2022 Volume 2022:15 Pages 7189—7199
DOI https://doi.org/10.2147/IJGM.S363892
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Ya-Ru Liang,1,2,* Chou-Chin Lan,1,3,* Wen-Lin Su,1,3 Mei-Chen Yang,1,3 Sin-Yi Chen,1 Yao-Kuang Wu1,3
1Division of Pulmonary Medicine, Department of Internal Medicine, Taipei Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, New Taipei City, Taiwan; 2Graduate Institute of Clinical Medical Sciences, College of Medicine, Chang Gung University, TaoYuan City, Taiwan; 3School of Medicine, Tzu-Chi University, Hualien, Taiwan
*These authors contributed equally to this work
Correspondence: Yao-Kuang Wu, Division of Pulmonary Medicine, Department of Internal Medicine, Taipei Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, No. 289, Jianguo Road, Xindian Dist, New Taipei City, Taiwan, Tel +886-2-66289779 ext 5709, Fax +886-2-66289009, Email [email protected]
Background: The decision guild for non-invasive positive pressure ventilation (NPPV) application in acute respiratory failure (ARF) patients still needs to work out.
Methods: Adult patients with acute hypoxemic or hypercapnic respiratory failure were recruited and treated with NPPV or primary invasive mechanical ventilation (IMV). Patients’ characteristic and clinical outcomes were recorded. Logistic regression models were used to estimate the adjusted odds ratio (aOR) and 95% confidence intervals for baseline characteristics and clinical outcomes. Subgroup analyses by reason behind successful NPPV were conducted to ascertain if any difference could influence the outcome.
Results: A total of 4525 ARF patients were recruited in our facility between year 2015 and 2017. After exclusion, 844 IMV patients, 66 patients with failed NPPV, and 74 patients with successful NPPV were enrolled. Statistical analysis showed APACHE II score (aOR = 0.93), time between admission and start NPPV (aOR = 0.92), and P/F ratio (aOR = 1.04) were associated with successful NPPV. When comparing with IMV patients, failed NPPV patients displayed a significantly lower APACHE II score, higher Glasgow Coma Scale, longer length of stay in hospital, longer duration of invasive ventilation, RCW/Home ventilator, and some comorbidities.
Conclusion: APACHE II score, time between admission and start NPPV, and PaO2 can be predictors for successful NPPV. The decision of NPPV application is critical as ARF patients with failed NPPV have various worse outcomes than patients receiving primary IMV.
Keywords: acute respiratory failure, hospital stay, invasive mechanical ventilation, non-invasive positive pressure ventilation
Introduction
Non-invasive ventilation (NIA) has been used in the treatment of acute respiratory failure (ARF), congestive heart failure (CHF), cardiogenic pulmonary edema (CPE), and immunosuppressed patients with pulmonary infiltrates.1 NIV not only reduces the need for endotracheal intubation and complications like airway trauma and pneumonia, but also reduces the factors like length of stay in the intensive care unit, the length of hospital stay, and mortality in selected patients.2
Noninvasive positive pressure ventilation (NPPV) has become increasingly important to manage selected cases of ARF in recent years.3,4 In NPPV, oxygen is delivered to a spontaneously breathing patient with a tight-fitting mask which covers nose or both nose and mouth. These portable and compact equipments are less expensive and easier operable. NPPV is useful as an intermediary between invasive ventilation and nasal facemask support to augment blood oxygenation. Some studies and meta-analyses have been performed in order to establish the efficacy of NPPV in patients and as an alternative to intubation in patients with ARF.5–7 The addition of NPPV to standard care procedure is associated with a marked reduction in intubation rate, complications, length of hospital stay and even mortality.8–10 But application of NPPV on ARF patients does not guarantee the result is always positive.
NPPV failure is defined as the need for invasive mechanical ventilation (IMV) after a trial of NPPV. In some patients, NPPV application is clearly insufficient as the patients do not obtain adequate ventilation. Other patients initially benefit from NPPV (for hours to few days) will then deteriorate and require IMV. NPPV failure is associated with various risk factors, including age, severity of illness scores, the presence of acute respiratory distress syndrome (ARDS) or community acquired pneumonia, acidosis (pH <7.25), persistent tachypnea, persistent hypercapnia, and poor neurologic scores.3,11–13 The failure rates of NPPV can range from 5% to 60% in different studies depending on the etiology and severity of ARF.11,12 Despite these uncertain outcomes, NPPV is still regularly used in different situations.3
Several studies indicated that patients failing NPPV have worse outcomes than patients with successful NPPV treatment.14–16 Other studies suggested that patients who failed NPPV and subsequently require endotracheal intubation experience significantly higher mortality and longer hospitalization than patients primarily intubated.17–19 These indicate that although NPPV do accelerate the progress of recovery, some patients who failed NPPV treatment do not take any benefits from it. This brings up an important decision. How do the physicians decide whether the patient is going to be treated with NPPV or IMV when the ARF patient is received? Is there any hint or indicator which can help for their decision? By comparing and contrasting potential differences in clinical variables and outcomes in ARF patients, we can find out the indicators which point out possible patients who can benefit from NPPV treatment and who should take IMV directly for better outcomes. The conclusions can then be applied clinically to achieve better therapeutic results.
Methods
Study Design and Participants
This retrospective observational study collected data from the records of patients admitted to Taipei Tzu Chi Hospital with acute hypoxemic (PaO2 of less than 8.0 kPa) or hypercapnic (PaCO2 of more than 6.0 kPa) respiratory failure and treated with NPPV between January 1, 2015 to December 31, 2017. Diagnostic criteria for respiratory failure were set as four conditions: (1) hypoxemia [partial pressure of oxygen (PaO2) <8.0 kPa]; (2) signs of inadequate respiratory muscle strength including accessory muscle or paradoxical respiration; (3) pH ≤7.35 and/or partial pressure of carbon dioxide (PaCO2) ≥6.0 kPa with dyspnea; (4) signs of increased respiratory work with respiratory rate of >30 breaths/min or hypoventilation with <12 breaths/minute. Patients with the following seven situations were excluded in this study. (1) aged <18 years; (2) NPPV was used in the home care setting; (3) had degenerative neuromuscular disease or obstructive sleep apnea syndrome; (4) made no-intubation decision; (5) when NPPV was used during the weaning phase after extubation; (6) follow-up data were incomplete due to transfer to another hospital; (7) ventilation is needed after surgery, cardiac arrest, seizures, or intoxication. If multiple admissions occurred during the study period, only the first eligible admission was evaluated; (8) patients who have missing value.
Ethical Considerations
This study complies with the requirement of the Declaration of Helsinki. The study protocol was approved by the Institutional Review Board of Tzu Chi Hospital. The need for informed consent and registration was waived because of the retrospective nature of the study. Patients’ data from routine care were deidentified by coding.
Data Collection and Baseline Measurements
Data of the following variables were collected from the hospital’s Patient Data Management System for all patients: age, gender, body mass index (BMI), Acute Physiology and Chronic Health Evaluation-II score (APACHE-II), Glasgow Coma Score (GCS), hospital unit where the respirator initiated (ICU or ward), days of NPPV application, and time between admission and start of ventilation. Besides, data of hemodynamic variables (respiratory rate, heart rate, blood pressure, and body temperature), ventilatory variables such as inspiratory positive airway pressure (IPAP) and expiratory positive airway pressure (EPAP), driving pressure and arterial blood gas values (pH, bicarbonate [HCO3−]), partial pressure of oxygen (PaO2), partial pressure of carbon dioxide (PaCO2), saturation of oxygen (SaO2), and ratio of arterial oxygen tension to fraction of inspired oxygen (P/F ratio) before starting of ventilation were collected. The primary diagnosis was recorded and categorized as exacerbation chronic obstruction pulmonary disease (COPD), pneumonia, cardiogenic pulmonary edema and other. Exacerbation COPD was defined as an acute worsening of respiratory symptoms in patients with COPD, which is associated with a variable degree of physiological deterioration. Pneumonia was diagnosed according to the definitions of Centers for Disease Control and Prevention.20 Cardiogenic pulmonary edema was defined as dyspnea of sudden onset, typical findings of fluid overload on chest X-ray, and widespread rales without a history. Other comorbidities including neuromuscular disease, chronic lung disease, ischemic heart disease, cancer, chronic renal disease, hypertension, diabetes mellitus, liver disease, and autoimmune disease requiring corticosteroid therapy or advanced cancer under anticancer chemotherapy were also documented.
Outcome Parameters
The primary study purpose was to identify clinical variables associated with NPPV failure. NPPV failure was defined as the need for intubation despite NPPV support. The NPPV failure might due to refractory hypoxemia, hypoventilation, worsening of clinical features such as respiratory distress (tachypnea, tachycardia, increased work of breathing) hypotension, worsening of the level of consciousness, laboratorial evidence of worsening or persistent respiratory distress while on NPPV (abnormality in PaO2, PaCO2, pH, and serum lactate level), or failure to tolerate the device. The secondary outcome parameters were in-hospital mortality, duration of hospital stay, duration of IMV either primary or after failed NPPV, admission to subacute respiratory care center and disposition after discharge.
Statistical Analysis
Baseline characteristics were compared between groups by using Chi-squared tests, independent t-tests, and Wilcoxon rank sum test to detect any differences in the categorical and continuous demographic variables, respectively. Data were expressed as number (percentage) for categorical variables and mean±SD for continuous variables with normal distribution or presented as median (25th-75th percentile) for continuous variables without normal distribution. Logistic regression models were used to estimate the odds ratio (OR) and 95% confidence intervals (CIs) for clinical outcomes in different characteristics comparisons. To develop a model predicting the successful NPPV, we used stepwise selection to enter variables with P value <0.20 into the model and retain variables with P value <0.05. Furthermore, ensemble modeling was employed to establish new model predicting the successful NPPV. The ensemble model integrated three machine learning algorithms to further improve predictive accuracy, including SVM, C5.0 and XGBoost. Stratified analysis for cause of respiratory failure was conducted to ascertain if differences among special subpopulations influence outcome. The interaction between each stratification factor and neutrophil/lymphocyte ratio was tested, with a P value <0.05 indicating significant interaction. A two-sided P value of <0.05 was regarded as statistically significant. Data management and statistical analysis were conducted by SAS software version 9.4 (SAS Institute, Inc.) and R ver. 4.0.4 (caretlist, caretensemble, and caretstack packages).
Results
A total of 4525 ARF patients were recruited in this study. After exclusion, 844 patients treated with IMV and 140 patients under NPPV treatment were enrolled. For patients with NPPV, 66 patients failed initial NPPV treatment and needed to conduct IMV, and the other 74 patients had successful NPPV results (Figure 1). The baseline characteristics of NPPV failure and NPPV success group are shown in Table 1. Patients in the NPPV success group had significantly lower APACHE II score, heart rate, and time between admission and start NPPV. Patients at intensive care unit were all failure for NPPV. Patients in NPPV failure group displayed a significantly longer time between admission and start NPPV, and lower arterial blood gas, including, partial pressure of oxygen (PaO2), saturation of oxygen (SaO2), and ratio of arterial oxygen tension to fraction of inspired oxygen (P/F ratio).
 |
Table 1 Baseline Characteristics of Patients (NPPV Failure Group vs NPPV Success Group) |
 |
Figure 1 Flowchart of study population. |
The comparing results of the univariable logistic regression show that APACHE II score, heart rate, and time between admission and start NPPV were significantly negative associated with successful NPPV (Table 2). On the contrary, PaO2, SaO2, and P/F ratio were positively associated with successful NPPV. Based on the result of stepwise selection, the clinical variables retained in the final multivariable logistic regression model were APACHE II score (adjusted OR, 0.93; 95% CI, 0.87–0.98; p = 0.014), PaO2 (adjusted OR, 1.04; 95% CI, 1.01–1.06; p = 0.003), and time between admission and start NPPV (adjusted OR, 0.92; 95% CI, 0.86–0.99; p = 0.024). The ROC curve of multivariate analysis model showed AUC (95% CI) = 0.775 (0.699–0.851), Youden’s index = 0.621, cutoff point = 0.482 (Figure 2).
 |
Table 2 Crude and Adjusted Odds Ratios for Successful NPPV in Different Clinical Characteristics Comparisons |
 |
Figure 2 Receiver operating characteristic (ROC) curve analysis for multivariate analysis for successful NPPV. (AUC (95% CI) = 0.738 (0.671–0.806), Youden’s index = 0.366, cutoff point = 0.450). |
Figure 3 shows the ROC curve from machine-learning models. The best performance was predicted by the ensemble model with 0.967 of AUC (95% CI = 0.921–1.000). Followed by the results predicted by C5.0 model with 0.938 of AUC (95% CI = 0.869–1.000). The ROC curve of XGBoost model and SVM model showed AUC (95% CI) = 0.857 (0.724–0.984) and 0.854 (0.724–0.984), respectively. Compared with the traditional model, the machine-learning models had better performance.
When we ranked the importance of all tested variables, it appeared that the PaO2 was the most important variable in the prediction of postoperative complications (Figure 4). This was followed by initial ventilation venue, and systolic blood pressure. However, P/F ratio and vasopressors in first 24 h of admission did not contribute to the prediction of the successful NPPV.
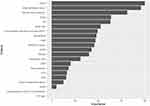 |
Figure 4 Variable-importance ranking in the gradient-boosting machine. |
The baseline characteristics of patients failing NPPV and patients with IMV are shown in Supplementary Table 1. Patients failing NPPV displayed a significantly lower APACHE II score and frequency of ICU admission for initial ventilation. Patients with IMV were more likely to have lower GSC and frequency of several comorbidities, including neuromuscular disease, chronic lung disease, ischemic heart disease, cancer, chronic renal disease, hypertension, diabetes mellitus, and liver disease. In addition, the cause of respiratory failure was significantly different between two groups. In patients who failed NPPV, respiratory failure has higher chance of being caused by COPD, pneumonia, and cardiogenic pulmonary edema.
The results of the multivariable logistic regression are shown in Supplementary Table 2. Patients with IMV were associated with significantly reduced risk of length of stay in hospital of ≥28 days (adjusted OR, 0.18; 95% CI, 0.09–0.37; p < 0.001), duration of invasive ventilation for ≥7 days (7-<14 days: adjusted OR, 0.37; 95% CI, 0.19–0.75; p = 0.009; 14-<21 days: adjusted OR, 0.41; 95% CI, 0.18–0.94; p = 0.036; ≥21 days: adjusted OR, 0.43; 95% CI, 0.23–0.81; p = 0.009), and RCW/Home ventilator (adjusted OR, 0.25; 95% CI, 0.11–0.54; p < 0.001).
Furthermore, the stratified analysis was conducted for NPPV failure and IMV patients. There appeared to be no significant difference in risk between IMV and failing NPPV patients in length of stay in hospital, duration of invasive ventilation and RCW/Home ventilator across several distinct subgroups (Supplementary Table 3). Stratified Analyses for Outcomes between IMV and NPPV failure patients were also conducted and shown in Supplementary Figure 1.
Discussion
In this retrospective study, lower APACHE II score, higher PaO2, and shorter time between admission and start NPPV were all associated with successful NPPV treatment by stepwise selection and multivariable logistic regression. On the contrary, initial ventilation venue (ICU) and higher heart rate were associated with NPPV failure. The AUC predicted by Ensemble model based on selected variants was 0.967. Besides, patients who failed NPPV and were forced to apply IMV had significant higher risk of various outcomes including various comorbidity, longer length of stay in hospital, longer duration of IMV, and higher RCW/home ventilator.
Our results indicated that when ARF patients were received, if the APACHE II score was low, PaO2 was high enough, and NPPV was applied soon, patients had high possibility to be treated with NPPV successfully. We also tried to find the threshold of each factor which can be used to decide whether NPPV or IMV should be used clinically. Unfortunately, univariate analysis for each factor did not show good response. The ROC curve of univariate analysis of APACHE II score and PaO2 showed AUC at 0.6504 and 0.7110, respectively (data not shown). This indicated that all three factors should be considered together to make final decision.
Several studies have focused on the use of NPPV for ARF.21,22 A meta-analysis supported that NPPV treatment improves survival in most acute settings when applied to treat or prevent ARF.23 Important advantages of NPPV include increased patient comforts, maintenance of airway defenses, ability to eat and speak, and avoiding the complications of endotracheal intubation such as nosocomial pneumonia, injury to airways, aspiration, post intubation laryngeal, and tracheal stenosis.24 The disadvantages of NPPV include slow improvement of blood gases, the need for conscious, cooperative patient and decreased ability to clear bronchial secretion.25 NPPV should be instituted if the respiratory rate is more than 30/min and pH is less than 7.35. Successful treatment with NPPV is associated with an increase in arterial pH and decrease in PaCO2 at two hours of treatment. If the variables do not improve, intubation should be considered.20
A proportion of patients will fail with NPPV, requiring intubation and invasive ventilation. It is important that personnel and the facility for intubation be rapidly available if needed. One meta-analysis does not support the association between using NPPV and in-hospital mortality rate or the length of the ICU and hospital stay in patients with ARF.7 Other studies suggested that patients who fail NPPV and subsequently require endotracheal intubation experience significantly higher mortality and longer hospitalization than patients primarily intubated.19,26 In this study, we indicated that NPPV failure, compared with IMV, is independently associated with worse outcomes among patients admitted to the hospital for ARF. Patients with failed NPPV had significantly higher APACHE-II scores, a higher percentage of pneumonia and cardiogenic pulmonary edema than successful ones due to their severity of illness. The results of a previous multi-center study suggested that patients with older age, higher severity scores, ARDS, or pneumonia have a higher risk of NPPV failure and patients who did not show improvement after the first hour of noninvasive treatment were also at greater risk of failed NPPV.22
This study was the first to select the control group from primary intubation under same patient characteristics. In the subgroup analysis, we found that NPPV failure did not seem to result in worse outcomes compared to the primary intubation in the COPD and pneumonia subgroups. On the contrary, in the cardiogenic pulmonary edema subgroup, the NPPV failure patients had longer length of invasive ventilation, lower survival rate and discharge to home. Schnell et al recently reported NPPV failure was an independent risk factor for mortality.3 Most notably, Schnell et al found a trend toward increased mortality in immunocompetent patients with respiratory failure, especially in hypoxemic respiratory failure, which has a high rate of intubation and a higher mortality when intubation is delayed by a trial of NPPV.3,27 In the propensity-matched cohort, NPPV therapy was associated with a 29% relative reduction of in-hospital mortality compared with IMV.17
Acute exacerbation of chronic obstructive pulmonary disease (AECOPD) is a leading cause of poor quality of life and mortality in developing countries. NPPV remains the first-line intervention in hospitalized patients with ARF due to AECOPD. However, NPPV may fail in some patients.28 As remarked in recent European Respiratory Society/American Thoracic Society guidelines, strong evidence supports the use of NPPV in patients who develop acute hypercapnic respiratory failure (pH ≤7.35, PaCO2 >45 mm Hg) due to AECOPD.29 In this study, 100% ARF patient received the NPPV at general ward had a positive result. But for ARF patients admitted to ICU, the rate of NPPV failure is 65.15%. This ratio was higher than other study which may relate to different severity of ARF.30
A successful outcome is highly dependent on accurate ARF patient selection, and the severity of hypercapnia and/or acidosis after initiation of NPPV is a major predictor of NPPV failure.31 Stefan et al found that mortality rates in patients with COPD exacerbation who failed NPPV were substantially higher compared with patients who were primarily intubated (22.5% vs 16.1%).32 In this study, the NPPV failure did not seem to result in worse outcomes compared to the primary intubation in the COPD subgroup. The explanations might be the smaller sample size, differences in severity, and circumstance including PH, PaO2 and PaCO2 level in this study.
Early predictors of NPPV failure are relevant to select the appropriate patients in daily practice. Logistic regression models of our study identified the APACHE-II score and PaO2 at admission as factors independently associated with NPPV failure. These factors could be of predictive value in the selection process of patients eligible for NPPV. In numerous studies, a higher Simplified Acute Physiology Score II (SAPS II) score was related to NPPV failure, as well as APACHE-II and SOFA scores.12,17,19,33 SAPS II of more than 34 was a predictor of failure.13 The population had a mean APACHE II of 18, compared to patients observed by Murad et al where APACHE II was 23 and our study was 24.34 Wang et al conducted a similar study and reported that serum albumin levels and duration of NPPV treatment were independent risk factors for the efficacy of NPPV treatment in respiratory failure.35 These results could be combined after a large-scale survey to make a final decision guild for physicians.
There are several limitations in this study. The present study is one of few that focused on outcomes in NPPV failure compared with immediate invasive ventilation.36 There is little reference can be used for comparison. The baseline variables of the groups of patients with NPPV and primary intubation are not fully comparable, although we addressed the imbalances by adjusting for significant baseline differences with respect to outcomes. The small study population precludes subgroup analyses and extensive multivariate analysis due to the limited number of events. Moreover, our study was conducted in a single center experienced with the practice of NPPV, which may limit the generalizability of findings.
Conclusions
An initial trial of NPPV should be considered carefully in ARF treatment. Patients with lower APACHE II score, higher PaO2, and shorter time between admission and start NPPV had higher possibility of positive results after NPPV treatment. On the other hand, other patients receiving NPPV faced higher risk of having failed NPPV, forced to apply IMV, and various comorbidities than patients receiving IMV directly. A larger multi-center prospective trial is warranted to confirm the findings of the present study and find out the threshold for each factor for clinical application.
Acknowledgments
Ya-Ru Liang and Chou-Chin Lan are considered co-first authors.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Disclosure
The authors have no relevant financial or non-financial interests to disclose.
References
1. Agarwal R, Aggarwal AN, Gupta D, Jindal SK. Non-invasive ventilation in acute cardiogenic pulmonary oedema. Postgrad Med J. 2005;81(960):637–643. doi:10.1136/pgmj.2004.031229
2. Brochard L. Mechanical ventilation: invasive versus noninvasive. Eur Respir J Suppl. 2003;22:4731s–37s.
3. Schnell D, Timsit JF, Darmon M, et al. Noninvasive mechanical ventilation in acute respiratory failure: trends in use and outcomes. Intensive Care Med. 2014;40(4):582–591. doi:10.1007/s00134-014-3222-y
4. Nava S, Hill N. Non-invasive ventilation in acute respiratory failure. Lancet. 2009;374(9685):250–259. doi:10.1016/S0140-6736(09)60496-7
5. David-Joao PG, Guedes MH, Rea-Neto A, Chaiben VBO, Baena CP. Noninvasive ventilation in acute hypoxemic respiratory failure: a systematic review and meta-analysis. J Crit Care. 2019;49:4984–4991.
6. Xu XP, Zhang XC, Hu SL, et al. Noninvasive ventilation in acute hypoxemic nonhypercapnic respiratory failure: a systematic review and meta-analysis. Crit Care Med. 2017;45(7):e727–e733. doi:10.1097/CCM.0000000000002361
7. Liu YJ, Zhao J, Tang H. Non-invasive ventilation in acute respiratory failure: a meta-analysis. Clin Med. 2016;16(6):514–523. doi:10.7861/clinmedicine.16-6-514
8. Comellini V, Pacilli AMG, Nava S. Benefits of non-invasive ventilation in acute hypercapnic respiratory failure. Respirology. 2019;24(4):308–317. doi:10.1111/resp.13469
9. Osadnik CR, Tee VS, Carson-Chahhoud KV, Picot J, Wedzicha JA, Smith BJ. Non-invasive ventilation for the management of acute hypercapnic respiratory failure due to exacerbation of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2017;7:CD004104.
10. Vital FM, Ladeira MT, Atallah AN. Non-invasive positive pressure ventilation (CPAP or bilevel NPPV) for cardiogenic pulmonary oedema. Cochrane Database Syst Rev. 2013;Cd005351. doi:10.1002/14651858.CD005351.pub3
11. Scala R, Pisani L. Noninvasive ventilation in acute respiratory failure: which recipe for success? Eur Respir Rev. 2018;27(149):180029. doi:10.1183/16000617.0029-2018
12. Ozyilmaz E, Ugurlu AO, Nava S. Timing of noninvasive ventilation failure: causes, risk factors, and potential remedies. BMC Pulm Med. 2014;14:1–0.
13. Antonelli M, Conti G, Esquinas A, et al. A multiple-center survey on the use in clinical practice of noninvasive ventilation as a first-line intervention for acute respiratory distress syndrome. Crit Care Med. 2007;35(1):18–25. doi:10.1097/01.CCM.0000251821.44259.F3
14. Permall DL, Pasha AB, Chen XQ. Current insights in non-invasive ventilation for the treatment of neonatal respiratory disease. Ital J Pediatr. 2019;45(1):105. doi:10.1186/s13052-019-0707-x
15. Roberts A. Understanding the principles of non-invasive positive pressure ventilation. Nurs Stand. 2021;36(8):61–66. doi:10.7748/ns.2021.e11750
16. Grieco DL, Menga LS, Eleuteri D, Antonelli M. Patient self-inflicted lung injury: implications for acute hypoxemic respiratory failure and ARDS patients on non-invasive support. Minerva Anestesiol. 2019;85(9):1014–1023. doi:10.23736/S0375-9393.19.13418-9
17. Stefan MS, Priya A, Pekow PS, et al. The comparative effectiveness of noninvasive and invasive ventilation in patients with pneumonia. J Crit Care. 2018;43:190–196.
18. Meeder AM, Tjan DH, van Zanten AR. Noninvasive and invasive positive pressure ventilation for acute respiratory failure in critically ill patients: a comparative cohort study. J Thorac Dis. 2016;8(5):813–825. doi:10.21037/jtd.2016.03.21
19. Mosier JM, Sakles JC, Whitmore SP, et al. Failed noninvasive positive-pressure ventilation is associated with an increased risk of intubation-related complications. Ann Intensive Care. 2015;54:1–9.
20. Hilbert G, Boyer A, Vargas F. Optimizing both noninvasive ventilation and antimicrobial approach in hematological patients with acute respiratory failure. Rev Clin Esp. 2014;214(7):385–386. doi:10.1016/j.rce.2014.05.026
21. Segovia B, Velasco D, Jaureguizar Oriol A, Diaz Lobato S. Combination therapy in patients with acute respiratory failure: high-flow nasal cannula and non-invasive mechanical ventilation. Arch Bronconeumol. 2019;55(3):166–167. doi:10.1016/j.arbres.2018.06.002
22. Nicolini A, Stieglitz S, Bou-Khalil P, Esquinas A. Cost-utility of non-invasive mechanical ventilation: analysis and implications in acute respiratory failure. A brief narrative review. Respir Investig. 2018;56(3):207–213. doi:10.1016/j.resinv.2017.12.011
23. Cabrini L, Landoni G, Oriani A, et al. Noninvasive ventilation and survival in acute care settings: a comprehensive systematic review and meta analysis of randomized controlled trials. Crit Care Med. 2015;43(4):880–888. doi:10.1097/CCM.0000000000000819
24. Kaya A, Ciledag A, Cayli I, Onen ZP, Sen E, Gulbay B. Associated factors with non-invasive mechanical ventilation failure in acute hypercapnic respiratory failure. Tuberk Toraks. 2010;58(2):128–134.
25. Fortis S, Lusczek ER, Weinert CR, Beilman GJ. Metabolomics in COPD acute respiratory failure requiring noninvasive positive pressure ventilation. Can Respir J. 2017;2017:9480346.
26. Chandra D, Stamm JA, Taylor B, et al. Outcomes of noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease in the United States, 1998–2008. Am J Respir Crit Care Med. 2012;185(2):152–159. doi:10.1164/rccm.201106-1094OC
27. Thille AW, Contou D, Fragnoli C, Cordoba-Izquierdo A, Boissier F, Brun-Buisson C. Non-invasive ventilation for acute hypoxemic respiratory failure: intubation rate and risk factors. Crit Care. 2013;17(6):R269. doi:10.1186/cc13103
28. Ansari SF, Memon M, Brohi N, Tahir A. Noninvasive positive pressure ventilation in patients with acute respiratory failure secondary to acute exacerbation of chronic obstructive pulmonary disease. Cureus. 2019;11(10):e5820. doi:10.7759/cureus.5820
29. Rochwerg B, Brochard L, Elliott MW, et al. Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J. 2017;50(2):1602426. doi:10.1183/13993003.02426-2016
30. Abroug F, Ouanes-Besbes L, Hammouda Z, et al. Noninvasive ventilation with helium-oxygen mixture in hypercapnic COPD exacerbation: aggregate meta-analysis of randomized controlled trials. Ann Intensive Care. 2017;7(1):59. doi:10.1186/s13613-017-0273-6
31. Phua J, Kong K, Lee KH, Shen L, Lim TK. Noninvasive ventilation in hypercapnic acute respiratory failure due to chronic obstructive pulmonary disease vs. other conditions: effectiveness and predictors of failure. Intensive Care Med. 2005;31(4):533–539. doi:10.1007/s00134-005-2582-8
32. Stefan MS, Nathanson BH, Higgins TL, et al. Comparative effectiveness of noninvasive and invasive ventilation in critically ill patients with acute exacerbation of chronic obstructive pulmonary disease. Crit Care Med. 2015;43(7):1386–1394. doi:10.1097/CCM.0000000000000945
33. Pacilli AM, Valentini I, Carbonara P, Marchetti A, Nava S. Determinants of noninvasive ventilation outcomes during an episode of acute hypercapnic respiratory failure in chronic obstructive pulmonary disease: the effects of comorbidities and causes of respiratory failure. Biomed Res Int. 2014;2014:976783.
34. Murad A, Li PZ, Dial S, Shahin J. The role of noninvasive positive pressure ventilation in community-acquired pneumonia. J Crit Care. 2015;30(1):49–54. doi:10.1016/j.jcrc.2014.09.021
35. Wang J, Bian S, Tang X, Ye S, Meng S, Lei W. Influencing factors of noninvasive positive pressure ventilation in the treatment of respiratory failure: a 10-year study in one single center. Eur J Med Res. 2021;26(1):136. doi:10.1186/s40001-021-00615-6
36. Zhu F, Liu ZL, Long X, et al. Effect of noninvasive positive pressure ventilation on weaning success in patients receiving invasive mechanical ventilation: a meta-analysis. Chin Med J. 2013;126(7):1337–1343.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

