Back to Journals » Cancer Management and Research » Volume 14
Factors Affecting the Risk of Brain Metastasis in Limited-Stage Small Cell Lung Cancer After Prophylactic Cranial Irradiation
Authors Chen MY, Ji Y, Hu X, Chen M
Received 17 November 2021
Accepted for publication 11 April 2022
Published 23 May 2022 Volume 2022:14 Pages 1807—1814
DOI https://doi.org/10.2147/CMAR.S347449
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Ahmet Emre Eşkazan
Meng-Yuan Chen, Yongling Ji, Xiao Hu, Ming Chen
Department of Radiation Oncology, Institute of Cancer and Basic Medicine of Chinese Academy of Sciences, Cancer Hospital of the University of Chinese Academy of Sciences, Zhejiang Cancer Hospital, Hangzhou, 310022, People’s Republic of China
Correspondence: Ming Chen, Department of Radiation Oncology, Institute of Cancer and Basic Medicine of Chinese Academy of Sciences, Cancer Hospital of the University of Chinese Academy of Sciences, Zhejiang Cancer Hospital, Hangzhou, No. 1, East Banshan Road, Banshan District, Hangzhou, 310022, People’s Republic of China, Email [email protected]
Background: Prophylactic cranial irradiation (PCI) can reduce the risk of brain metastases (BM) and improve overall survival (OS) in patients with limited-stage small cell lung cancer (LS-SCLC) after partial or complete response to primary therapy. However, some SCLC patients still develop BM after PCI. This study aimed to evaluate the risk factors of BM in patients with LS-SCLC after PCI and identify characteristics of patients who may not benefit from PCI.
Methods and Materials: We identified 550 patients with LS-SCLC who received chemoradiotherapy at Zhejiang Cancer Hospital between 2002 and 2017. All patients received PCI. Kaplan–Meier analyses and Cox regression analyses were used to identify factors affecting OS and brain metastasis-free survival (BMFS).
Results: For this patient population, the median survival time was 27.9 months, and the 5-year OS rate was 31%. The median survival time was 24.9 months (95% CI: 22.6– 27.2 months), and 30.2 months (95% CI: 24.2– 36.3 months) in patients with or without BM (P = 0.000). The overall BM rate was 15.6% (86/550). The frequency of BM in patients with pathologic stages I, II, and III were 9.3% (4/43), 13.4% (7/52), and 16.5% (75/455). The patients with tumors ≥ 5 cm had an increased risk of BM (HR: 1.781, 95% CI: 1.044– 3.039, P = 0.034) but not death (HR: 1.126, 95% CI: 0.925– 1.663, P = 0.182). The median survival time among patients < 60 years was significantly longer than patients ≥ 60 years (34.9 months vs 24.6 months, P = 0.001); however, the difference in the BM risk between the two groups was not statistically significant.
Conclusion: PCI remains the standard of care for LS-SCLC patients who achieve complete or partial response after completion of chemoradiotherapy. However, patients with tumors ≥ 5 cm may have a higher risk of developing BM after PCI.
Keywords: small cell lung cancer, brain metastases, chemo-radiotherapy, prognosis prophylactic cranial irradiation
Introduction
Small cell lung cancer (SCLC) is a neuroendocrine tumor, which is well known for its early development of widespread metastases and rapid doubling time, and accounts for 13–19% of all lung cancers.1,2 Brain is a common site of metastasis in patients with SCLC, and recently, the proportion of patients with brain metastases (BM) is increasing. Due to increased control of locoregional disease and distant metastases, BM are one of the main factors responsible for serious impairment of quality of life, and shortened survival. Prophylactic cranial irradiation (PCI) has been proposed in SCLC to suppress the risk of BM and improve survival, and eventually quality of life. PCI can reduce BM and improve overall survival (OS) in patients with limited-stage SCLC (LS-SCLC) after complete response to primary therapy.3 However, some patients still suffer from BM after PCI with unknown risk factors. Our study aimed to assess the factors affecting the risk of BM in patients with LS-SCLC after PCI and identify characteristics of patients who may not benefit from PCI.
Methods and Materials
Patient Selection and Data Collection
We identified 550 patients with LS-SCLC who had received definitive chemoradiotherapy at Zhejiang Cancer Hospital from 2002 through 2017. The information of patient’s diagnoses, demographics, treatment, and treatment response was extracted from medical records. Primary tumor size was measured on diagnostic images at the time of initial treatment, as the largest dimension of the primary parenchymal tumor. TNM staging was defined according to the current American Joint Committee on Cancer (AJCC) criteria, 7th edition. The patients’ characteristics are shown in Table 1.
 |
Table 1 Characteristics of Patients (n = 550) |
Treatment Characteristics
All patients had received definitive chemoradiotherapy and PCI. 40% of patients received concurrent chemotherapy with thoracic radiation. Radiotherapy typically consisted of 45 Gy in 30 fractions delivered twice daily or 54–70 Gy in 27–30 fractions delivered once daily. Patients who received surgery as part of treatment were excluded from this analysis. Chemotherapy consisted of 4–6 cycles of etoposide and cisplatin (EP) or etoposide and carboplatin (EC). The chemotherapy cycles for concurrent chemotherapy and induction chemotherapy were 2–3 and 1–3 cycles, respectively. PCI was administered to patients who achieved complete or partial remission of tumor. All patients received brain MRI/CT examination to exclude BM before PCI. Initiated 4–6 weeks after completion of primary chemoradiotherapy, patients received PCI of a total dose of 25 Gy over 2 weeks.
Statistical Analysis
Statistical analyses were carried out with SPSS 22.0 software. OS was calculated from the time of first treatment to the date of death or censored at the date of last follow-up. BMFS was calculated from the time of first treatment to the date of brain metastasis. The variables considered were age (<60 years or ≥60 years), sex (male or female), pathologic stage (I, II or III), Primary Tumor Size (<5 cm or ≥5 cm), brain metastases (yes or no), response to chemotherapy (ChT) (complete response (CR) or partial response (PR)), XRT fractionation (once daily or twice daily). Kaplan–Meier method was applied to estimate survival rates. Cox proportional hazards regression analyses were used to identify factors potentially associated with OS and BMFS. Log rank test was used to compare the survival curves, and P <0.05 was considered to indicate statistically significant differences.
Results
Patient Characteristics
A total of 550 LS-SCLC patients who received chemoradiotherapy and PCI were included in this analysis. The median age of all patients was 56 years (range 22–80 years), and 332 (60.4%) were ≥60 years old when treatment was started. At the time of treatment initiation, 257 (46.7%) had primary intrathoracic disease that was ≥5 cm in diameter. Patient characteristics are summarized in Table 1.
Survival
For the whole population, the median survival time was 27.9 months, the 5-year OS rate was 31%. Univariate analysis revealed that brain metastases, pathology stage, age, and XRT fractionation were significantly correlated with survival rate (Table 2). In a comparison of patients with BM and those without BM, the 5-year survival rate were 8.9% and 36.1%, the median survival was 24.9 months (95% CI: 22.6–27.2 months) in the brain metastasis group, and 30.2 months (95% CI: 24.2–36.3 months) in the non-brain metastases group, respectively, (P = 0.000; Figure 1). The 5-year survival rates for patients with pathology stage I, II, and III were 68.7%, 48.9%, and 24.7% (P = 0.000), respectively. Among patients <60 years, the median survival time were significantly higher than patients ≥60 years (34.9 months vs 24.6 months, P = 0.001; Figure 2). Twice daily XRT fractionation offered a better 5-year OS in contrast to once daily (34.8% vs 21.6%, P = 0.013).
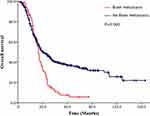 |
Figure 1 Comparison of overall survival (OS) of patients with limited-stage small cell lung cancer (LS-SCLC) between brain metastases group and no-brain metastases group. |
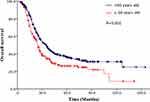 |
Figure 2 Comparison of overall survival (OS) of patients with limited-stage small cell lung cancer (LS-SCLC) between <60 years group and ≥60 years group. |
15.6% (86/550) of the entire patient population had evidence of metastases to brain. The frequency of BM in patients with pathologic stages I, II, and III were 9.3% (4/43), 13.4% (7/52), and 16.5% (75/455), P = 0.043. Univariate analysis revealed that primary tumor size ≥5 cm was associated with poor 5 year BMFS (71.6% vs 81.3%, P = 0.022; Figure 3).
 |
Figure 3 Comparison of brain metastasis-free survival (BMFS) of patients with limited-stage small cell lung cancer (LS-SCLC) between tumor size ≥5 cm group and <5 cm group. |
On multivariate analyses (Table 3), pathologic stages (HR: 1.733, 95% CI: 1.064–2.823, P = 0.027) were independent risk factors for both BMFS and OS. Tumor larger than 5 cm was an independent risk factor for BM (HR: 1.781, 95% CI: 1.044–3.039, P = 0.034), but not death (HR: 1.126, 95% CI: 0.925–1.663, P = 0.182).
Discussion
Lung cancer is the main cause of mortality from cancer worldwide.4,5 SCLC is a neuroendocrine tumor which is well known for its rapid doubling time and potential for widespread metastases.6,7 In two prior meta-analyses, PCI was associated with both reduced risk of BM and improved OS in patients with CR after definitive chemoradiotherapy. Overall, the effectiveness and outcomes of PCI with regard to BMFS and OS for patients in our analysis were similar to previous studies.3,8,9 The results of our study showed that risk of developing BM was significantly increased when the primary tumor was large (≥5 cm) at diagnosis. This outcome is consistent with prior research reporting correlation between higher pathologic tumor stage, which depends on locoregional spread and tumor size, and increased risk of developing BM. The rate of BM was 6.25% among patients with TNM pathologic stage I disease, 28.2% of stage II disease, and 29.1% of stage III disease.10 Other studies have reported similar findings, with <10% of pathologic stage I tumors with subsequent BM compared with 13.4% of pathologic stage II tumors, and 16.5% of pathologic stage III tumors.11–15
In those studies, tumor size could be measured directly after resection, in contrast to our study, which did not include patients with resected tumors; however, tumor size was measured on diagnostic CT scans. Tumor size at the time of treatment initiation was not associated with poor OS in our study, however, our findings, along with prior research, suggest that large tumor size may indicate a more aggressive phenotype with increased risk of metastases, especially to the brain metastases. Univariate analysis revealed that primary tumor size ≥5 cm was associated with poor 5-year BMFS in our study, pathologic stages (71.6% vs 81.3%, P = 0.022) were independent risk factors for both BMFS and OS, and that is why TNM staging is more widely used to help guide clinical decisions.16
The treatment of elderly patients can often be challenging, because they typically present with additional medical issues, which can complicate therapy. In our study, the median age of all patients was 56 years, and 60.4% were ≥60 years old when treatment was initiated. The median survival time among patients <60 years were significantly longer than patients ≥60 years (34.9 months vs 24.6 months, P = 0.001). Another study further emphasized that PCI did not confer a benefit in both OS and BMFS among patients ≥70 years old with large (≥5 cm) primary tumors, and age ≥70 years was an independent risk factor for increased overall mortality in their analysis. Besides, KPS score <80 also predicted poor outcome.17 This is not surprising, because older patients often have co-morbid conditions or poor performance status. In addition, elderly patients are also more susceptible to PCI-induced neurotoxicity than younger patients; indeed, increasing age was the most important predictor of chronic neurotoxicity (P = 0.005).18,19 However, the difference of the BM risk was not statistically significant with age in our study. Thoracic twice-daily radiotherapy is one of the standards of care for SCLC; a study showed that patients with SCLC who received thoracic twice-daily radiotherapy appeared to have a higher risk of BM rate than those who received once-daily (26.0% vs 16.9%; HR, 1.55, 95% CI: 1.06–2.26, P = 0.03),20 but our study had a different result, as the difference in the BM risk was not statistically significant with the two groups in the outcome.
The role of PCI in reducing the risk of developing BM has been extensively studied in patients with limited-stage SCLC that responds completely to definitive chemoradiotherapy, and PCI remains the standard therapy after complete response to chemoradiotherapy for limited-stage SCLC.3 Nevertheless, 15.6% of patients still had brain metastases after PCI in our study. Can all patients benefit from PCI after definitive chemoradiotherapy for LS-SCLC?
Conclusion
In conclusion, the results of our retrospective study of a large number of patients with limited-stage SCLC treated at a single institution suggest that patients with large tumors may not benefit from PCI, even after a complete response to definitive chemoradiotherapy. Further work to identify characteristics of patients with LS-SCLC who may not benefit from PCI is warranted. However, it is difficult to judge the curative effect and prompt the prognosis early by traditional imaging techniques such as CT and MRI. Therefore, to explore molecular markers which can give early prediction of brain metastasis and evaluation of efficacy of PCI is the direction of future research.
Acknowledgments
The study was approved by the Institutional Review Board and Ethics Committee of Zhejiang Cancer Hospital. This study was conducted in accordance with the Declaration of Helsinki. Written informed consent for the collection of medical information was obtained from all patients. All procedures performed in the study were in accordance with the ethical standards of the institutional research committee. This work was supported by the fund of National Natural Science Foundation of China (No. 81402540, 81672972). The abstract of this paper was presented at the WCLC 2019 Conference named ‘Factors affecting the risk of brain metastasis in limited-stage small cell lung cancer after prophylactic cranial irradiation’ as a poster presentation with interim findings. (https://wclc2019.iaslc.org/wp-content/uploads/2019/08/WCLC2019-Abstract-Book_web-friendly.pdf).
Funding
Zhejiang Province Medical and Health Science and Technology 2022KY618.
Disclosure
The authors disclose no conflicts of interest in this work.
References
1. Hirsch FR, Matthews MJ, Aisner S, et al. Histopathologic classification of small cell lung cancer changing concepts and terminology. Cancer. 1988;62:973–977.
2. Herbst RS, Heymach JV, Lippman SM. Lung cancer. N Engl J Med. 2008;359:1367–1380. doi:10.1056/NEJMra0802714
3. Aupérin A, Arriagada R, Pignon JP, et al. Prophylactic cranial irradiation for patients with small cell lung cancer in complete remission. N Engl J Med. 1999;341(7):
4. Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi:10.3322/caac.20107
5. Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–2917. doi:10.1002/ijc.25516
6. Govindan R, Page N, Morgensztern D, et al. Changing epidemiology of small-cell lung cancer in the United States over the last 30 years: analysis of the surveillance, epidemiologic, and end results database. Clin Oncol. 2006;24:4539–4544. doi:10.1200/JCO.2005.04.4859
7. Amini A, Byers LA, Welsh JW, Komaki RU. Progress in the management of limited-stage small cell lung cancer. Cancer. 2014;120:790–798. doi:10.1002/cncr.28505
8. Meert AP, Paesmans M, Berghmans T, et al. Prophylactic cranial irradiation in small cell lung cancer: a systematic review of the literature with meta-analysis. BMC Cancer. 2001;1:5. doi:10.1186/1471-2407-1-5
9. Yin X, Yan D, Qiu M, Huang L, Yan SX. Prophylactic cranial irradiation in small cell lung cancer: a systematic review and meta-analysis. BMC Cancer. 2019;19:95. doi:10.1186/s12885-018-5251-3
10. Gong L, Wang QI, Zhao L, Yuan ZY, Li RJ, Wang P. Factors affecting the risk of brain metastasis in small cell lung cancer with surgery: is prophylactic cranial irradiation necessary for stage I-III disease? Int J Radiat Oncol Biol Phys. 2013;85:196–200. doi:10.1016/j.ijrobp.2012.03.038
11. Tsuchiya R, Suzuki K, Ichinose Y, et al. Phase II trial of postoperative adjuvant cisplatin and etoposide in patients with completely resected stage I-IIIa small cell lung cancer: the Japan Clinical Oncology Lung Cancer Study Group Trial (JCOG9101). J Thorac Cardiovasc Surg. 2005;129:977–983. doi:10.1016/j.jtcvs.2004.05.030
12. Nakamura H, Kato Y, Kato H. Outcome of surgery for small cell lung cancer – response to induction chemotherapy predicts survival. Thorac Cardiovasc Surg. 2004;52:206–210. doi:10.1055/s-2004-821075
13. Ogawa S, Horio Y, Yatabe Y, et al. Patterns of recurrence and outcome in patients with surgically resected small cell lung cancer. Int J Clin Oncol. 2012;17:218–224. doi:10.1007/s10147-011-0277-4
14. Zhu H, Bi Y, Han A, et al. Risk factors for brain metastases in completely resected small cell lung cancer: a retrospective study to identify patients most likely to benefit from prophylactic cranial irradiation. Radiat Oncol. 2014;9:216. doi:10.1186/1748-717X-9-216
15. Meng-yuan C, Xiao H, Yong B, et al. Comparison of long term results between matched chemoradiotherapy and surgery for limited stage small cell lung cancer. Cancer Manag Res. 2019;11:9049–9055. doi:10.2147/CMAR.S222882
16. Mirsadraee S, Oswal D, Alizadeh Y, Caulo A, van Beek E
17. Farooqi AS, Emma B, Xiong W, James DC, Ritsuko K, Komaki R. Prophylactic cranial irradiation after definitive chemoradiotherapy for limited-stage small cell lung cancer: do all patients benefit? Radiother Oncol. 2017;122(2):307–312. doi:10.1016/j.radonc.2016.11.012
18. Le Pechoux C, Laplanche A, Faivre-Finn C, et al. Clinical neurological outcome and quality of life among patients with limited small-cell cancer treated with two different doses of prophylactic cranial irradiation in the intergroup Phase III trial (PCI99–01, EORTC 22003–08004, RTOG 0212 and IFCT 99–01). Ann Oncol. 2011;22:1154–1163. doi:10.1093/annonc/mdq576
19. Wolfson AH, Bae K, Komaki R, et al. Primary analysis of a phase II randomized trial Radiation Therapy Oncology Group (RTOG) 0212: impact of different total doses and schedules of prophylactic cranial irradiation on chronic neurotoxicity and quality of life for patients with limited-disease small-cell lung cancer. Int J Radiat Oncol Biol Phys. 2011;81:77–84. doi:10.1016/j.ijrobp.2010.05.013
20. Zeng H, Li R, Hu C, et al. Association of twice-daily radiotherapy with subsequent brain metastases in adults with small cell lung cancer. JAMA Netw Open. 2019;2(5):e190103. doi:10.1001/jamanetworkopen.2019.0103
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


