Back to Journals » Patient Preference and Adherence » Volume 17
Factors Affecting Patient Adherence to Inhalation Therapy: An Application of SEIPS Model 2.0
Authors Ma J , Sun X, Wang X, Liu B, Shi K
Received 31 October 2022
Accepted for publication 18 February 2023
Published 3 March 2023 Volume 2023:17 Pages 531—545
DOI https://doi.org/10.2147/PPA.S395327
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Johnny Chen
Jing Ma,1 Xu Sun,1,2 Xinwei Wang,1,2 Bingjian Liu,1,2 Kaiqi Shi3
1Faculty of Science and Engineering, University of Nottingham, Ningbo, People’s Republic of China; 2Nottingham Ningbo China Beacons of Excellence Research and Innovation Institute, Ningbo, People’s Republic of China; 3Suzhou Inhal Pharma Co., Ltd., Suzhou, People’s Republic of China
Correspondence: Xu Sun, Department of Mechanical, Materials and Manufacturing, Faculty of Science and Engineering, University of Nottingham, Ningbo, People’s Republic of China, Tel/Fax +8657488186443, Email [email protected]
Purpose: This study aims to explore factors that affect patient adherence to inhalation therapy by applying a patient-centered approach.
Patients and Methods: We conducted a qualitative study to identify the factors that influence adherent behaviors among asthma/COPD patients. 35 semi-structured interviews with patients, and 15 semi-structured interviews with healthcare providers (HCPs) who manage asthma/COPD patients were conducted. The SEIPS 2.0 model was applied as a conceptual framework for guiding the interview content and analysis of the interview data.
Results: Based on the findings of this study, a conceptual framework of patient adherence in asthma/COPD during inhalation therapy was constructed including five themes: person, task, tool, physical environment, and culture and society. Person-related factors include patient ability and emotional experience. Task-related factors refer to task type and frequency and flexibility. Tool-related factors are the type of inhalers and usability of inhalers. Physical environment-related factors include home environment and COVID-19 situation. Culture and social related factors consist of two aspects: cultural beliefs and social stigma.
Conclusion: The findings of the study identified 10 influential factors that impact on patient adherence to inhalation therapy. A SEIPS-based conceptual model was constructed based on the responses of patients and HCPs to explore the experiences of patients engaging in inhalation therapy and interacting with inhalation devices. In particular, new insight about factors of emotional experience, physical environment and traditional cultural beliefs were found crucial for patients with Asthma/COPD to conduct patients’ adherent behaviors.
Keywords: adherence, inhalation therapy, human factors and ergonomics, asthma, chronic obstructive pulmonary disease, drug-device combination products
Introduction
Chronic respiratory diseases such as asthma and Chronic Obstructive Pulmonary Disease (COPD) are perceived as serious public health problems in the overall population.1 Inhalation therapy is the foundation stone for such chronic respiratory disease treatment. This application allows drug delivery directly into the airways, thus resulting in more rapid symptom alleviation and fewer side effects.2 Adherence to long-term inhalation treatment is a prerequisite for managing chronic respiratory diseases effectively. The term adherence is defined as the “active, voluntary, and collaborative involvement of the patient in a mutually acceptable course of behavior to produce a therapeutic result”.3 However, the level of adherence is still undesirable for patients with asthma/COPD, and tend to be lower than in other chronic diseases.4–6 There is a lack of understanding of patient adherence to inhalation therapy in developing countries,1 such as China.7 Poor adherence might result in worse symptom control, more hospitalizations and higher spending outcomes.1 Thus factors that can facilitate patient adherence should be considered when conducting inhalation treatment.
There have been some attempts to investigate the underlying factors affecting patient adherence. Inadequate inhaler technique is considered to be one of the main factors affecting patient adherence.8,9 The most common errors while using inhalers included failure to exhale before inhaling, failure to breath hold and failure to load the dose.10 Studies have also shown that patients’ perceptions and beliefs can influence their adherent behavior.11,12 For example, the likelihood of patients adhering to treatment increases if they perceive that the disease affects their daily lives or if they realize that non-adherence may result in serious health consequences.13 And patients who feel the need to take a particular medication tend to adhere to it better, whereas patients who are concerned about overtreatment by their physician are more likely to discontinue the prescribed medication.12 Moreover, the quality of communication between patients and HCPs can also contribute.14 For example, patients can misunderstand prescriptions due to suboptimal communication with their HCPs, which could lead to accidental non-adherence.15 The researchers believe that patient adherent rate was improved when they received better communication with their HCPs.16 Other important factors preventing expected adherence include self-efficacy, comorbidities, complex regimen, cost, social support and training on the use of the inhaler.17–19
Such studies, however, may be of limited value, as they ignore inhalers as “drug-device combination product (DDCP)” presents unique “patient-device interaction” challenges.20 Despite several studies suggesting that specific inhaler attributes influence patient satisfaction and adherence to treatment,21,22 their focus is to ensure the effectiveness of the device and appropriate delivery of drugs, rather than on patients’ perception and experiences concerning their engagement with inhalation therapy and inhaler device.
Therefore, understanding patient adherence requires a systematic and comprehensive approach. To fill this gap, we conducted a qualitative study to adapt a well-regarded theoretical model from the field of human factors and ergonomics (HFE), the Systems Engineering Initiative for Patient Safety (SEIPS) model 2.0,23 which has been used by a number of HCPs, researchers and educators since its introduction and promotion in healthcare.24
The SEIPS model is an innovative HFE approach to patient safety originally described by Carayon et al in 2006.25 The updated version of the SEIPS model, ie SEIPS 2.0, clarifies the role of patients and other nonprofessionals in health-related activities, improving our understanding of the individual and collaborative works of patients, HCPs, and caregivers.23 SEIPS 2.0 presents a new HFE work system with interacting components: person(s), tasks, tools and technology, internal/external environment, and organization. An optimal fit between work system components contributes to the success of work activities, whereas a poor integration of patient work may bring about performance barriers, leading to non-adherent behavior and suboptimal health outcomes.23 The SEIPS 2.0 model has been applied broadly in healthcare to optimize healthcare workflow efficiency,26 offer guidance for evaluating health information technology implementation,27 and improve patient safety outcomes.28
Our primary objectives were to identify factors affecting Asthma/COPD patient adherence during inhalation therapy by applying a user-centered approach. The insights gained in this regard will allow us to explore the experiences of patients engaging in inhalation therapy and interacting with inhalation devices from perspectives of patients and HCPs, in order to precipitate knowledge on human factors and ergonomics facilitating or impeding the implementation of patient adherent behavior, ultimately leading to more effective adherence interventions.
Materials and Methods
Methods, Study Participants, Recruitment, and Setting
This qualitative examination of factors impacting adherence was mainly based on a semi-structured interview data, to explore the psychological underpinnings of perceptions of patients and HCPs. This semi-structured interview was guided by the SEIP model. This approach is consistent with a few existing studies. For example, Martinez et al did a qualitative study using interview based on SEIPS model to obtain a comprehensive understanding of patients’ and clinicians’ experiences with the CONDUIT-HID (CONtrolling Disease Using Inexpensive Technology—Hypertension In Diabetes) intervention.29 Wooldridge et al employed observation and interview techniques based on the SEIPS model to understand and analyze healthcare processes in a systematic manner and identify specific areas of improvement.30 Danesh et al (2020) conducted a semi-structured interview based on SEIPS model to identify factors influencing nurses’ work ability.31 Werner et al did a qualitative interview study based on SEIPS model to explore transitions experienced by older adults during the patient journey across healthcare settings surrounding an emergency department visit.32
Study participants were recruited from one large hospital system located in Ningbo, Zhejiang Province, China. Fifty participants of 62 approached agreed to be interviewed, giving a response rate of 80.1% (Figure 1). We included 35 patients and 15 HCPs in our study between May 2021 and June 2021 to understand patient adherence to inhalation therapy from various perspectives. Patients’ recruitment criteria included (a) having a physician-confirmed diagnosis of asthma or COPD; (b) using an inhaler device longer than 3 months prior to the study and being in a stable phase of their disease. HCPs recruitment criteria included more than three years of work experience in asthma/COPD treatment to provide a professional standpoint. All participants are at least 18 years old. In this study, we adhered to the principles of the Declaration of Helsinki and were approved by the ethics committee of University of Nottingham Ningbo China. The demographic information of all interviewees is summarized in Table 1 and Table 2.
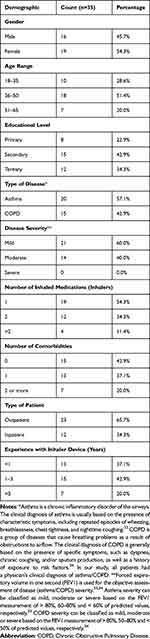 |
Table 1 Participant Demographics (Patients) |
 |
Table 2 Participant Demographics (HCPs) |
 |
Figure 1 Flow chart of participants. |
Data Collection
Based on the literature review on patient adherence to inhalation therapy and, using the SEIPS 2.023 framework as a guide, we developed a semi-structured interview protocol (see Appendix 1) with open-ended questions to explore work systems used by patients with asthma/COPD to identify factors affecting patient adherence to inhalation therapy in real life. At the beginning of each interview, each participant signed a consent form, and an investigator gave a brief introduction to the research background. Participants were then asked questions about their overall perceptions and experiences about inhalation therapy and inhaler devices, and by taking the SEIPS components into account, the answers were adequately probed. Face-to-face interviews occurred in a semiprivate area (ie a hospital room with two beds and a shared bathroom) and lasted up to an hour. All patients were selected with the consent of their respective HCPs so as not to disrupt their health care. With permission, interviews were conducted in Chinese (mandarin) and audio-recorded for English transcription.
Data Analysis
The interviews were all transcribed in Chinese by the interviewers themselves, and translated into English by the bilingual translator in our team. The research team reviewed the transcripts line-by-line for accuracy. We have separated patients’ transcribed interviews from HCPs’ transcribed interviews for comparison. The transcripts of the interviews were organized and coded using NVIVO 11 software, and the responses were coded based on SEIPS framework. A thematic analysis was conducted by two members of the research team to identify relevant codes35,36 The transcripts of interviews were read and coded by the researchers independently to develop a comprehensive code book which identifies the key concepts in the data. Interview data were analyzed concurrently with study procedures to detect theoretical saturation. After interviewing the thirty-fifth patient and the fifteenth HCPs, we concluded that the interview responses were becoming increasingly repetitive. Consequently, the sample size was determined to be fifty participants based on theoretical saturation. Coding disagreements were resolved jointly by the principal investigator and coders. The Cohen’s Kappa value for inter-rater reliability (IRR) agreement was 0.783, which indicates fair agreement between the two researchers. Consensus on preliminary and final results was reached in discussions with all authors. As a result, the themes which emerged during the analysis were broadly grouped into five categories, namely: (1) person; (2) task; (3) tool; (4) physical environment; and (5) culture and social (Table 3).
 |
Table 3 Characteristics of Patient Adherence to Inhalation Therapy |
Results
Person Related Factors
Patient Ability
Participants emphasized the importance of patient ability that impede individual patient self-efficacy during inhalation therapy, which included both physical characteristics and cognitive ability.
Physical Characteristic
The participants described two main aspects of physical characteristics. The first is caused by the loss of lung function, which is a common symptom of respiratory disease, causing the patient to not be able to use an inhaler at an adequate inhalation flow rate.
P8: I know I should take a deep breath during inhalation (therapy), but my lung condition prevented me from doing so. I cannot even breathe easily.
The second physical characteristic is the functional deterioration in manual dexterity, which is common among elderly patients and makes it difficult for them to grip the inhalation device securely.
P1: I want to hold the inhaler firmly, but my hands keep shaking. I have to spend a long time trying to control it.
The HCPs noted that a patient with physical limitations may have difficulty using an inhaler, thus trying to treat a patient with respiratory disease compounded by physical issues may not be as effective as treating the same patient without any other functional loss. The HCPs proposed that their medical staff should select the appropriate inhalation device for patients based on their individual needs and abilities. Rather than forcing patients to adapt to devices that exceed their capabilities.
H9: My prescriptions take into account the physical abilities of the patient. For example, an SMI (soft mist inhaler) is more suitable for elderly patients because it requires less inspiratory flow rate.
Cognitive Ability
Our findings suggest that there are some cognitive differences in patients’ knowledge and understanding of their treatment and HCPs’ unawareness/insensitive handling of patient-HCP communication. Some HCPs noted that insufficient knowledge of the disease and lacking awareness of the importance of ongoing attention to their treatment results in patients’ inability to abide by the inhaler regimen. According to HCPs, individual cognitive differences are considered to be one of the most significant factors affecting patient adherence.
H3: Some patients mistakenly believe that the absence of clinical symptoms means they have been cured. Chronic respiratory diseases, such as asthma, are difficult to be completely cured and must be managed with inhaled medication for a very long time.
The HCPs expressed that it is important to educate the patients to understand their disease properly and cultivate good usage habits. They described appropriate education as ensuring that a patient’s understanding of disease knowledge and the role of medication matches his/her expected results.
Some patients complained that the habitual use of specialized medical terms or vague terms by the doctor impedes their understanding of the condition and makes them hesitant to follow their doctor’s advice. They described that they are too exhausted to speak with their doctor and that the talk ends before they can fully comprehend.
P12: To be honest, I did not understand the words the doctor used, so all I could do was pay the money and get the inhaled medicine that I did not know. Would not it be nice if they explained it to me in a way I understand.
And one patient questioned the doctor’s credibility and authority because he never received a clear diagnosis.
P6: My doctor always uses ambiguous words, such as perhaps, probably, and maybe, which leaves me feeling uncertain. How can I put my trust in him, given that his diagnosis is so hazy?
Some HCPs responded that due to medical uncertainty and individual differences, they sometimes can only inform patients about the possibility of different situations but cannot give a definitive answer.
Moreover, several patients reported that memory loss may result in their forgetting to use inhalers on time or having difficulty following medication instructions correctly. There are, however, some patients who report that they set a timed alarm on their mobile phones to remind them to use their inhalers on a daily basis.
P4: I knew I had a poor memory, so I set an alarm on my phone to remind myself.
Emotional Experience
Our findings revealed that poorly patient-inhaler interactions have a significant impact on the emotional experience perceived by patients, which may create a continuous effect of burnout. Patients expressed that the noise generated while operating the inhaler device could trigger their emotional discomfort.
P17: Every time I use this inhaler, I hear the sound of the internal parts turning, which increases my anxiety and resistance.
Some patients also said that continuously and repeatedly operating the same device might trigger negative emotions.
P6: I have used the same device for over a year now, and I find it extremely boring and annoying to repeat the same operation every day like a robot.
During the interview, some HCPs expressed their understanding of the negative emotions caused by a patient’s interaction with the device. However, they emphasized that their priority is the effectiveness of inhaled medicines over the patient’s emotional experience.
H4: As doctors, we put the patient’s health first, and the patient’s feelings regarding inhalers seem to be less important.
Task Related Factors
Task Type
Collaborative Task
Some tasks in inhalation treatment involve collaboration between HCPs and patients. For example, it is essential that patients receive training in the correct use of inhalers and have their technique checked by their HCPs regularly. However, patients described that they receive only limited inhaler training, which is insufficient to develop consistently appropriate techniques. During the interview, we found that 4 in every 5 patients receive less than 10 minutes of inhaler training and 1 in 7 receive the second check of their inhaler technique.
P20: My entire face-to-face consultation lasted 10 minutes, and the doctor spent up to 1–2 minutes explaining the approximate use of an inhaler.
Some HCPs explained that time constraints in clinical practice prevent them from spending time training their patients on device operation or monitoring their ongoing use.
H11: I see dozens of patients a day, so I do not have time to explain everything about the device.
It is noted by the HCPs that some patients attempt to learn on their own by studying written instructions and watching video tutorials online, which may helpful in improving inhalation techniques. Several HCPs also suggested that using visual aids can assist them in better demonstrating the use of inhalers, thereby improving training effect during limited consultations.
H8: I have an empty inhaler available to demonstrate to the patient how to inhale the medication, so that the patient will understand my instructions more quickly and improve the effectiveness of our communication.
Independent Task
We classified some tasks that can be performed independently by the patient as independent tasks. In many of the inhalation therapy sessions, patients are expected to operate the device on their own. Some patients indicated that the lack of guidance on effective inhalation techniques increases their impediment to using inhalers. As many patients with respiratory illness (eg asthma) are treated with both inhaled reliever and inhaled maintenance therapies, this often results in “inhaler mixing” (ie, prescribing more than one type of inhaler for one patient) situations. Some patients noted that if multiple types of devices are involved, the therapy implementation becomes more difficult.
P23: It’s hard to master a single inhalation technique, and it’s even harder to master two at the same time, and I confuse these different techniques all the time.
A few patients reported that they are forced to experience “inhaler switching” (ie, switching from a familiar device to a new one) without sufficient time to adapt, thereby increasing their error rate.
P14: While the new device looks the same as the old one, the actual operation is different. At first, I followed the previous method, but the operation always failed.
Frequency and Flexibility
Our findings suggest that the frequency and flexibility of inhaler usage might influence patient adherence to inhalation therapy. Some patients indicated that the more frequently they use the device, the more likely it is that they might miss a dose.
P31: Despite setting an alarm, I sometimes forget to use my inhaler every morning and evening. It would be so much easier if I only had to use an inhaler once a day.
And one patient described that they were weary of restrictions and fetters of inhaler usage.
P7: I often have to work overtime or take business trips, so I am not flexible about treatment at all. Not to mention that I do not know when I am going to have an asthma attack, so I just try to carry the device with me 24/7. I sometimes feel like I am a pet on a leash.
While some HCPs expressed that patients may have to live with the inconvenience of inhalation therapy, given the significant advantages of inhalation therapy in treating conditions such as asthma or COPD.
H13: Pain is a part of treatment, maybe that’s the price of fighting the disease, patients always have to go through it for the sake of health.
Tool Related Factors
Type of Inhalers
Four major types of inhalers are widely used in clinical practice: pressurized metered-dose inhalers (PMDI), dry powder inhalers (DPI), soft mist inhalers (SMI), and nebulizers. According to our interviews, we found that these inhaler types present different advantages and disadvantages for use, and there is no single inhalation device that could satisfy all patients. For example, 71.4% of patients older than 51 years seem to be more resentful of PMDI because it requires coordinated driving and inhalation in comparison with other types of devices.
P5: There are times when I remember to press the button but forget to inhale, and there are times when I remember to inhale but forget to press (the button). It’s always out of sync anyway.
In contrast to female patients, male patients expressed more concern about DPIs, and the main complaint was a problem with drug agglomeration. If the device is not cleaned properly after use, a part of the drug powder will remain in the mouthpiece, causing clumping of the drug. We found that female patients are more likely to pay attention to the maintenance and cleaning of inhalers, whereas male patients are more likely to ignore these “details”.
Some HCPs illustrated that a patient’s clinical outcome may be dependent on the device type selected. They noted that the same patient may behave very differently when using different types of inhalers. Accordingly, the type of device used has a direct impact on patient adherence to inhalation therapy.
H2: He was initially a “disobedient” patient, but after changing to a different type of inhaler, he used it every time obediently.
A few HCPs also mentioned a new inhaler type – “the digital inhaler”, which has add-on/built-in sensors that detect inhaler use and measure inspiratory flow. They believed that this new technology will enable patients to obtain more benefits from inhalers, although there is currently no promotion of such devices in China.
However, the most concern of patients when discussing the possibility of the future application of the digital inhalers is the potential increase in medical expenses.
P10: Does the price of the inhaler increase as the devices become digital? If so, I do not know if it’s worth it.
Usability of Inhalers
The usability of inhalers was emphasized by participants because of the critical role of this factor in encouraging patients to stick with inhalation treatment. The patients proposed that they may not need more efficient devices but simply need devices that are: a. providing feedback; b. intuitive to use.
Providing Feedback
In our study, nearly two-thirds of patients expressed a desire to receive instant feedback on their use of the inhaler during treatment, while about three-in-seven said they would like to receive overall feedback after a period of inhaler use (eg one week or one month). During the interview, we found that approximately 88.6% of patients were concerned about whether the drug in the inhaler was truly being inhaled. The patients described that the only response they received was “a change in the numbers on the counter” (P14) and “a bitter taste in their mouths upon tasting the drugs” (P29). Some patients suggested that the inhaler should provide more real-time information about how it is being operated, as well as the speed at which it is being inhaled, to make sure they are using it properly.
P25: I am not sure if what I have done is right or wrong…I wish this device could give me more info and hints at that moment.
In addition, some patients identified that regularly reporting back on their inhaler usage may help them better review and take control of their situation.
P27: I mark my calendar after each inhalation so I know exactly how I am doing. Usually, if I notice I have missed doses in the past week, I will be extra careful to use an inhaler on time this week.
The HCPs also believed that the feedback information about inhaler usage may help patients to establish correct medication-taking routines and encourage them to better master inhalation techniques. However, about four-fifths of HCPs reported feeling overburdened with the amount of information they must handle during clinical encounters. Although getting overall feedback may help HCPs keep up with changes in a patient’s condition and make timely adjustments to treatment plans, instant feedback might be not as crucial for HCPs as it is for patients.
Intuitive to Use
The more desired feature suggested by patients was intuitive to use, which significantly reduced their cognitive load and effectively freed up mental resources for improved performance. Patients described that, with an intuitively designed inhaler, they will understand how to use it without much effort, and do not need any instruction or other help. One patient described the “intuitive inhaler” in her mind.
P4: There’s no need to consciously think about how to use the device, just opening it, inhaling it, and closing it. All of this happened so naturally!
Additionally, HCPs expected to be faced with intuitive inhalers that do not require them to spend extensive training time with patients.
H6: It also saves us time if we do not need to spend extra time teaching patients how to use the device, and the time savings can be seen with several more patients.
Physical Environment Related Factors
Home Environment
All patients identified their home setting as one in which they use their inhalers most frequently. Some of them noted the effects of home environment factors, such as temperature, humidity, and placement, on the storage of inhalers in the home. One patient described her experience of drug deterioration due to improper storage at home.
P2: Since I rinse my mouth every time I use the inhaler, I put it on the washstand in the bathroom to make it easier, but the humidity and heat in the bathroom cause the powder in the inhaler to agglomerate and denature quickly.
Similarly, another patient described the phenomenon of inhaling the wrong medicine when they mixed and placed different inhalers together.
P10: On my bedside table I kept my reliever inhaler and maintenance inhaler, and once I confused them, I used the relief inhaler as a maintenance one. That’s terrible!
Some HCPs stated that there is a lack of resources for them to manage patients’ health-related behaviors at home, which is beyond their authority and ability.
COVID-19
Some patients expressed that the usage scenarios of inhalers have been further restricted as a result of the outbreak of COVID-19. They identified that lockdowns in communities and a sweeping closure of public spaces and transportation reduce their chances of going out. Additionally, due to the fear of cross-infections and the possibility that disinfectants used in public places might induce disease, they have to stay at home.
P22: I think I am in the vulnerable group because I have poor lung function, it’s safer for me to stay at home and go out less.
Some patients also stated since they must wear masks whenever they are outdoors, it is more difficult for them to use the inhaler in public.
P30: With a mask, I cannot inhale the drug, but if I do not wear a mask and use an inhaler, I am afraid I will get infected.
Culture and Social Related Factors
Cultural Beliefs
Cultural beliefs, defined as “a set of behavioral patterns related to thoughts, manners and actions, which members of society have shared and passed on to succeeding generations”37 may influence the decision-making of patients to use their inhalers. We found that more than two-thirds of the patients showed strong beliefs in the effectiveness of Traditional Chinese Medication (TCM) and traditional Chinese health beliefs and that these patients had or are experiencing the behavior of reducing or stopping their inhaler use.
P28: There is an old Chinese saying “All medicine has du (poison) to some degree”, so as long as there are no symptoms, there is no need to use an inhaler again.
The HCPs expressed that the cultural beliefs of patients are difficult to modify, especially for older individuals, whose beliefs are deeply ingrained; however, younger patients are more amendable through sustaining counselling.
Social Stigma
Social stigma refers to the disapproval or discrimination of an individual or group based on perceivable characteristics that distinguish them from other members of society.38 In our study, we found that about one in seven patients may feel stigmatized by inhaler usage during treatment. One patient reported feeling social devaluation and discrediting to use her inhaler in public.
P32: It makes me feel ashamed and embarrassed to use the inhaler around my family or colleagues. It’s all my fault since everyone else is healthy and I have to use this (inhaler) to get well.
Another patient described that he perceived discrimination in his interactions with HCPs.
P19: When I was hospitalized, the nurses always said that I was not doing the correct steps, complaining that I could not learn it, which made her very frustrated. I know she would be more willing to take care of “smart patient” than “dumb patient” like me.
Discussion
An analysis of interviews with 35 patients and 15 HCPs identified 10 factors influencing patient adherence to inhalation therapy guided by SEIPS 2.0. This study found a large variety of person, task, tool, physical environment, culture and social factors shaping the patient adherence performance and outcomes of patients with Asthma/COPD. Privileging the participant’s voices revealed that adherence behavior in patients experiencing inhalation therapy is a dynamic process and is located in the constant negotiations between patient ability, emotional experience, task type, frequency and flexibility, type/usability of inhalers, home environment, COVID-19, cultural beliefs, social stigma and the imperfect medical encounters (see Appendix 2). Figure 2 consolidates the findings into a fully specified model of HFE factors.
 |
Figure 2 Patient adherence to inhalation therapy work system model. |
Some of these factors have been discussed in the previous literature.11–18 However, our study highlighted a few new aspects affecting the way patients performed their adherent behaviors. These factors included how negative emotional experiences made patients feel difficult to use inhaler devices; how physical environment factors (ie home environment and COVID-19) hindered and limited usage scenarios; and how traditional cultural beliefs influence patients’ decision to use their inhalers.
Our findings on the emotional experience generated by patient-device interaction affecting patient adherence to inhalation therapy were perhaps the most intriguing because most studies in the chronic illness literature focused on emotional considerations from the individual (eg depression) or interpersonal relationships (eg emotional support), and few publications highlighted them in the process of patient-device interaction. There are a number of studies that illustrate that depression and anxiety increase the likelihood of patients discontinuing treatment and decreasing the number of days they take the medication.18,19 Previous studies also discussed that patients’ adherence levels increased and their quality of life improved when their families or HCPs provided adequate emotional support.4,39 In one of the few studies providing empirical evidence for emotions arising from human-device interactions affect patient adherence, researchers found that emotional barriers may negatively affect patients’ satisfaction and confidence regarding self-injections.40 The patients’ diminishing confidence and growing dissatisfaction with the self-injection device further reduce their willingness to adhere to treatment. This is consistent with the observation made in this study. Therefore, special consideration should be given to the emotional condition of the patient during the interaction with the inhaler device. Emotional design theories such as Norman’s Emotional Design Theory,41 and Kansei Engineering42 could be implemented proactively to improve the ability to attract the attention of patients and evoke positive emotions. For example, in a study, emotional design was integrated into prosthetic devices to meet the emotional needs of users and to relate the appearance of those products to their image, which can function as a supportive product for patients and promote positive feelings.43 As a design technology, Kansei Engineering incorporates the emotional needs, psychological feelings, and cognitive habits of the users into the development of products. One study has applied Kansei Engineering method in medical nursing bed design comprised subjective evaluation, eye movement and electroencephalography (EEG) data.44 In the physical environment, the effect of the home environment was identified, including temperature, humidity and placement. One study has shown that a good physical environment in a hospital leads to a positive user experience and desired behavioral intention.45 But unlike hospital settings or pharmacy settings that are specialized in providing healthcare delivery, home settings may not offer an optimal environment for drug storage and inhalation treatment due to different lifestyle habits and living environments.46 A body of literature has assessed the patient adherence in clinical trials but rarely in the home-based environment. Since home use environments need to be considered, inhalation devices should be simulated in this environment and lay users (eg elderly patients) are encouraged to participate. We also found that the emergence of COVID-19 and changes in restrictive policies may have new implications for patient adherence to inhalation therapy. The patients constantly negotiated the challenges of restrictions on the scenarios in which patients cannot use their inhalers because of the COVID-19 outbreak. Therefore, it is very likely that some unique environmental factors that transcend clinical settings can also influence patient adherence to inhalation therapy and deserve further examination.
The results also illustrated that traditional cultural beliefs may have a direct impact on patients’ adherence via perceptions of health and medication management. The narratives affirmed that the traditional Chinese cultural concept of “All medicine has du to some degree” extends to the non-adherent behaviors in the Asthma/COPD sample, such as reduction or suspension of inhaler use. In ancient China, “du” was considered to be the defining characteristic of all drugs, which determined a medicine’s therapeutic efficiency.47 Drugs possessing “du” are effective in curing illness, but they can also cause people to become ill or die. According to traditional Chinese culture, all substances contain both Yin and Yang forces, emphasizing the dialectical relationship between all things that can be transformed into each other, resulting in the ambivalence of “du”. However, in the modern context, patients often simply suggest “du” as “duyao” (poison), lacking a corrective understanding of the paradox of “du”. As a result, patients may use the inhaled drug with excessive caution and discontinue its use once the symptoms remain stable. While many studies have shown that cultural beliefs may become potential obstacles for patients in demonstrating the desired medication adherence,48 a very small percentage of these studies addressed traditional cultural concepts and their influences in the context of inhaler adherence. It is possible that culturally and linguistically diverse populations have different health beliefs and cultural values than western medical beliefs.49 Within a group, individuals differ in their acculturation strategies (attitudes as well as actual behavior), which results in a range of behavioral repertoires.48 Thus, it is critical to place a strong emphasis on the traditional cultural meanings associated with inhaler use and address it behind inhaler adherence. Only by placing patients and culture at the center of inhaler adherence can we fundamentally understand patients’ non-adherent behaviors and develop truly effective adherence interventions.
In this study, we also explored patient adherence to inhalation therapy from both patients and HCPs. The results showed that patients’ capabilities, preferences and satisfactions with inhalation devices are causally related to their adherence, and doctors should choose the right device for the patient based on their needs and abilities.21 Some studies identified that incorporating the perspective of the patient in the treatment decision process may result in improved patient satisfaction and adherence.50,51 Although many studies support this view, patients still are rarely in a position to make that choice. In terms of rank orders, there seems to be a difference between the perceptions of HCPs and patients: HCPs are more concerned with the effectiveness of inhaled medications and the outcome of treatment than with the patient’s experience and feelings during inhalation therapy, whereas patients may hold different views about it. Similarly, Price et al52 reported that doctors and patients often perceive “well-controlled” asthma differently, and doctors often overestimate the actual usage of the patient. The HCPs also cited heavy work schedules, time constraints and a lack of resources in clinical practice for training patients’ inhaler techniques and addressing their concerns. This is consistent with what has been found in previous studies.53 Moreover, the HCPs believed that some issues are primarily relevant to the professional domains of healthcare systems, government or society. This implies we need to consider not only the requirements of individuals (eg patients, HCPs), but also different stakeholders (eg administrators, researchers, designers, and policymakers) whose decisions control and influence medical encounters and patient experiences.
As the HCPs in this study proposed, another trend in inhaler device development is introducing digital inhalers with the e-module integrated inside the device. To improve patient adherence, one of the biggest challenges is identifying those with non-adherent behaviors and the reasons behind them. Although the causes are likely to be multifactorial, the absence of effective monitoring methods has been a major cause of concern.54 When coupled with emerging technologies, the development of digital inhalers has provided an objective method of adherence monitoring, which could play a facilitative role in helping to enhance patient adherence and inhaler technique, and may have unique potential in identifying and rectifying emotional, and physical environment and cultural factors. For example, in a study, Tivatansakul et al55 proposed an emotional healthcare system that detects facial expressions and provides services aimed at resolving users’ social or mental health difficulties in daily life. The Propeller inhaler was introduced in another study, utilizing the GPS functionality of smartphones to provide localized environmental information, which can help HCPs identify correlations between asthma triggers and patient symptoms.56 Ghozali et al57 developed an asthma self-management app to help Indonesian patients improve their disease knowledge and self-efficacy by providing them with proper educational materials. It is important to note, however, that digital inhalers have an associated higher cost and may generate a vast amount of information that could increase the workload of patients and HCPs.9 Therefore, future studies should be conducted to demonstrate their economic and clinical benefits to increased costs.
Limitations
It is important to note several limitations of the study in terms of its methodology and sampling. Firstly, we conducted semi-structured interviews, where patients and HCPs are required to recall their experiences, which may introduce recall bias and inaccuracies. Secondly, this study is limited by the rather small size and a lack of diversity in participants’ cultural backgrounds. All participants were recruited from the same geographic region in China, the findings of this study should be generalized with caution. Future studies could include participants and HCPs from diverse locations/countries to address this limitation. Lastly, despite the fact that the SEIPS model provides a view of the whole system from the perspective of patient safety, some factors that are not directly related to safety issues may be overlooked. Research in the future should incorporate components of other systems-based models in order to gain a more comprehensive understanding.
Conclusion
This study revealed ten valuable HFE factors that influence patient adherence to inhalation therapy. We constructed a conceptual model of SEIPS model 2.0 by identifying new factors of emotional experience, physical environment and traditional cultural beliefs which were identified important factors to understand patient adherent behaviors. Our study also suggests that future adherence interventions should focus on the patient’s perception and experience concerning their interactions with inhaler devices. It is imperative that HCPs work on strategies to improve the quality and effectiveness of patient-HCP communication, as well as tailor device selection based on patient needs, preferences, and abilities. This study offer actionable opportunities to improve the inhalation therapy experience for patients. It may also apply to the study of patient adherence with other forms of drug-device combination products.
Acknowledgments
This work is supported by 2025 Key Technological Innovation Program of Ningbo City under Grant No.2022Z080, and the First Batch of 2021 MOE of PRC Industry-University Collaborative Education Program (Program No. 202101042006, Kingfar-CES “Human Factors and Ergonomics” Program). Written informed consent for publication of their details was obtained from the patient/study participant/parent/guardian/next of kin.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sabaté E. Adherence to Long-Term Therapies: Evidence for Action. World Health Organization; 2003.
2. Dabrowska M, Luczak-Wozniak K, Miszczuk M, et al. Impact of a single session of inhalation technique training on inhalation skills and the course of asthma and COPD. Respir Care. 2019;64(10):1250–1260. doi:10.4187/respcare.06740
3. Delamater AM. Improving patient adherence. Clin Diabetes. 2006;24(2):71–77. doi:10.2337/diaclin.24.2.71
4. DiMatteo MR. Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med Care. 2004;42(3):200–209. doi:10.1097/01.mlr.0000114908.90348.f9
5. Covvey JR, Mullen A, Ryan M, et al. A comparison of medication adherence/persistence for asthma and chronic obstructive pulmonary disease in the United Kingdom. Int J Clin Pract. 2014;68(10):1200–1208. doi:10.1111/ijcp.12451
6. Mäkelä MJ, Backer V, Hedegaard M, Larsson K. Adherence to inhaled therapies, health outcomes and costs in patients with asthma and COPD. Respir Med. 2013;107(10):1481–1490. doi:10.1016/j.rmed.2013.04.005
7. Zeng Y, Cai S, Chen Y, et al. Current status of the treatment of COPD in China: a multicenter prospective observational study. Int J Chron Obstruct Pulmon Dis. 2020;15:3227. doi:10.2147/COPD.S274024
8. Price D, Fletcher M, Van Der Molen T. Asthma control and management in 8000 European patients: the REcognise Asthma and LInk to Symptoms and Experience (REALISE) survey. NPJ Prim Care Respir Med. 2014;24(1):1–10. doi:10.1038/npjpcrm.2014.9
9. Chrystyn H, Audibert R, Keller M, Quaglia B, Vecellio L, Roche N. Real-life inhaler adherence and technique: time to get smarter! Respir Med. 2019;158:24–32.
10. Hesso I, Nabhani Gebara S, Greene G, Co Stello RW, Kayyali R. A quantitative evaluation of adherence and inhalation technique among respiratory patients: an observational study using an electronic inhaler assessment device. Int J Clin Pract. 2020;74(2):e13437. doi:10.1111/ijcp.13437
11. Leventhal H, Diefenbach M, Leventhal EA. Illness cognition: using common sense to understand treatment adherence and affect cognition interactions. Cognit Ther Res. 1992;16(2):143–163. doi:10.1007/BF01173486
12. Brandstetter S, Finger T, Fischer W, et al. Differences in medication adherence are associated with beliefs about medicines in asthma and COPD. Clin Transl Allergy. 2017;7(1):1–7. doi:10.1186/s13601-017-0175-6
13. Rapoff M, Bartlett S. Adherence in children and adults. In: Barlett SJ, editor. Clinical Care in the Rheumatic Diseases Atlanta. American College of Rheumatology; 2006:279–284.
14. Rogliani P, Ora J, Puxeddu E, Matera MG, Cazzola M. Adherence to COPD treatment: myth and reality. Respir Med. 2017;129:117–123. doi:10.1016/j.rmed.2017.06.007
15. Ulrik CS, Backer V, Søes-Petersen U, Lange P, Harving H, Plaschke PP. The patient’s perspective: adherence or non-adherence to asthma controller therapy? J Asthma. 2006;43(9):701–704. doi:10.1080/02770900600925569
16. Blais L, Bourbeau J, Sheehy O. Inhaled corticosteroids in COPD. Trends in patient’s persistence on treatment and determinants of use. Can Respir J. 2003;11:27–32. doi:10.1155/2004/289420
17. Moroni-Zentgraf P. Impact of patient needs on design and usage of an inhalation device in respiratory medicine. Respir Drug Delivery. 2013;1:141.
18. Restrepo RD, Alvarez MT, Wittnebel LD, et al. Medication adherence issues in patients treated for COPD. Int J Chron Obstruct Pulmon Dis. 2008;3(3):371. doi:10.2147/COPD.S3036
19. Sanduzzi A, Balbo P, Candoli P, et al. COPD: adherence to therapy. Multidiscip Respir Med. 2014;9(1). doi:10.4081/mrm.2014.395
20. Leiner S, Parkins D, Lastow O. Inhalation Devices and Patient Interface: Human Factors. Springer; 2015.
21. Ding B, Small M, Scheffel G, Holmgren U. Maintenance inhaler preference, attribute importance, and satisfaction in prescribing physicians and patients with asthma, COPD, or asthma–COPD overlap syndrome consulting for routine care. Int J Chron Obstruct Pulmon Dis. 2018;13:927. doi:10.2147/COPD.S154525
22. Hoy H, O’Keefe L. Choosing the right inhaler for the right patient: considerations for effective management of patients with chronic obstructive pulmonary disease or asthma. J Am Assoc Nurse Pract. 2020;32(1):89–99. doi:10.1097/JXX.0000000000000366
23. Holden RJ, Carayon P, Gurses AP, et al. SEIPS 2.0: a human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics. 2013;56(11):1669–1686. doi:10.1080/00140139.2013.838643
24. Carayon P, Karsh B-T, Gurses AP, et al. Macroergonomics in health care quality and patient safety. Rev Hum Factors Ergon. 2013;8(1):4–54. doi:10.1177/1557234X13492976
25. Carayon P. Handbook of Human Factors and Ergonomics in Health Care and Patient Safety. CRC press; 2006.
26. Bacci JL, Coley KC, McGrath K, Abraham O, Adams AJ, McGivney MS. Strategies to facilitate the implementation of collaborative practice agreements in chain community pharmacies. J Am Pharm Assoc. 2016;56(3):257–265. e252. doi:10.1016/j.japh.2016.02.014
27. Walker DM, Hefner JL, Sieck CJ, Huerta TR, McAlearney AS. Framework for evaluating and implementing inpatient portals: a multi-stakeholder perspective. J Med Syst. 2018;42(9):1–8. doi:10.1007/s10916-018-1009-3
28. Doucette WR, Vinel S, Pennathur P. Initial development of the systems approach to home medication management (SAHMM) model. Res Social Adm Pharm. 2017;13(1):39–47. doi:10.1016/j.sapharm.2015.12.013
29. Martinez VI, Marquard JL, Saver B, Garber L, Preusse P. Consumer health informatics interventions must support user workflows, be easy-to-use, and improve cognition: applying the seips 2.0 model to evaluate patients’ and clinicians’ experiences with the conduit-hid intervention. Int J Hum Comput Interact. 2017;33(4):333–343. doi:10.1080/10447318.2016.1278340
30. Wooldridge AR, Carayon P, Hundt AS, Hoonakker PL. SEIPS-based process modeling in primary care. Appl Ergon. 2017;60:240–254. doi:10.1016/j.apergo.2016.11.010
31. Danesh MK, Garosi E, Mazloumi A, Najafi S. Identifying factors influencing cardiac care nurses’ work ability within the framework of the SEIPS model. Work. 2020;66(3):569–577. doi:10.3233/WOR-203199
32. Werner NE, Rutkowski R, Graske A, et al. Exploring SEIPS 2.0 as a model for analyzing care transitions across work systems. Appl Ergon. 2020;88:103141. doi:10.1016/j.apergo.2020.103141
33. Bateman ED, Hurd SS, Barnes PJ, et al. Global strategy for asthma management and prevention: GINA executive summary. Eur Respir J. 2008;31(1):143–178. doi:10.1183/09031936.00138707
34. Vestbo J, Hurd SS, Agustí AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187(4):347–365. doi:10.1164/rccm.201204-0596PP
35. Strauss AL. Qualitative Analysis for Social Scientists. Cambridge university press; 1987.
36. Charmaz K. Constructing Grounded Theory. sage; 2014.
37. Hatah E, Lim KP, Ali AM, Shah NM, Islahudin F. The influence of cultural and religious orientations on social support and its potential impact on medication adherence. Patient Prefer Adherence. 2015;9:589. doi:10.2147/PPA.S79477
38. Latalova K, Kamaradova D, Prasko J. Perspectives on perceived stigma and self-stigma in adult male patients with depression. Neuropsychiatr Dis Treat. 2014;10:1399. doi:10.2147/NDT.S54081
39. Bonito A, Horowitz N, McCorkle R, Chagpar AB. Do healthcare professionals discuss the emotional impact of cancer with patients? Psycho Oncology. 2013;22(9):2046–2050. doi:10.1002/pon.3258
40. Rekaya N, Vicik SM, Hulesch BT, McDonald LL. Enhancement of an auto-injector device for self-administration of etanercept in patients with rheumatoid arthritis confers emotional and functional benefits. Rheumatol Ther. 2020;7(3):537–552. doi:10.1007/s40744-020-00216-5
41. Norman DA. Emotional Design: Why We Love (or Hate) Everyday Things. Civitas Books; 2004.
42. Nagamachi M. Kansei engineering. In: Handbook of Human Factors and Ergonomics Methods. CRC Press; 2004:794–799.
43. Sansoni S, Speer L, Wodehouse A, Buis A. Aesthetic of prosthetic devices: from medical equipment to a work of design. In: Emotional Engineering. Vol. 4. Springer; 2016:73–92.
44. Zhou Z, Cheng J, Wei W, Lee L. Validation of evaluation model and evaluation indicators comprised Kansei engineering and eye movement with EEG: an example of medical nursing bed. Microsyst Technol. 2021;27(4):1317–1333. doi:10.1007/s00542-018-4235-1
45. Juliá Nehme B, Torres Irribarra D, Cumsille P, Yoon SY. Waiting room physical environment and outpatient experience: the spatial user experience model as analytical tool. J Inter Des. 2021;46(4):27–48. doi:10.1111/joid.12205
46. Council NR. Health Care Comes Home: The Human Factors. Washington. DC: The National Academies Press; 2011.
47. Liu Y. Healing with Poisons: Potent Medicines in Medieval China. University of Washington Press; 2021.
48. Shahin W, Kennedy GA, Stupans I. The impact of personal and cultural beliefs on medication adherence of patients with chronic illnesses: a systematic review. Patient Prefer Adherence. 2019;13:1019. doi:10.2147/PPA.S212046
49. Eh K, McGill M, Wong J, Krass I. Cultural issues and other factors that affect self-management of type 2 diabetes mellitus (T2D) by Chinese immigrants in Australia. Diabetes Res Clin Pract. 2016;119:97–105. doi:10.1016/j.diabres.2016.07.006
50. Wilson SR, Strub P, Buist AS, et al. Shared treatment decision making improves adherence and outcomes in poorly controlled asthma. Am J Respir Crit Care Med. 2010;181(6):566–577. doi:10.1164/rccm.200906-0907OC
51. Pollard S, Bansback N, FitzGerld J, Bryan S. The burden of nonadherence among adults with asthma: a role for shared decision-making. Allergy. 2017;72(5):705–712. doi:10.1111/all.13090
52. Price D, David-Wang A, Cho SH, et al. Asthma in Asia: physician perspectives on control, inhaler use and patient communications. J Asthma. 2016;53(7):761–769. doi:10.3109/02770903.2016.1141951
53. Fink JB, Rubin BK. Problems with inhaler use: a call for improved clinician and patient education. Respir Care. 2005;50(10):1360–1375.
54. Pritchard JN, Nicholls C. Emerging technologies for electronic monitoring of adherence, inhaler competence, and true adherence. J Aerosol Med Pulm Drug Deliv. 2015;28(2):69–81. doi:10.1089/jamp.2014.1163
55. Tivatansakul S, Ohkura M, Puangpontip S, Achalakul T. Emotional healthcare system: emotion detection by facial expressions using Japanese database.
56. Kagen S, Garland A. Asthma and allergy mobile apps in 2018. Curr Allergy Asthma Rep. 2019;19(1):1–13. doi:10.1007/s11882-019-0840-z
57. Ghozali M, Satibi S, Ikawati Z, Lazuardi L. Asthma self-management app for Indonesian asthmatics: a patient-centered design. Comput Methods Programs Biomed. 2021;211:106392. doi:10.1016/j.cmpb.2021.106392
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
