Back to Journals » Patient Related Outcome Measures » Volume 6
Exploring quality of life as an intervention outcome among women with stress-related disorders participating in work rehabilitation
Authors Eklund M
Received 17 September 2014
Accepted for publication 7 November 2014
Published 13 January 2015 Volume 2015:6 Pages 1—7
DOI https://doi.org/10.2147/PROM.S74498
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Robert Howland
Mona Eklund
Department of Health Sciences, Lund University, Lund, Sweden
Background: Findings from quality of life studies are often inconclusive for reasons such as: i) estimates may address different aspects of quality of life and thus produce different outcomes; ii) quality of life is largely determined by self-factors; and iii) people with a long-term condition rate their quality of life better than those who have had their condition for a short duration. This makes quality of life a complex phenomenon to measure.
Aims: The above explanations served as hypotheses for this methodologically oriented paper, based on a longitudinal study on women with stress-related disorders receiving work rehabilitation.
Methods: Eighty-four women participating in a lifestyle intervention or care as usual were compared. Self-ratings of “general quality of life” and a summarized “satisfaction with different life domains” index (according to Manchester Short Assessment of Quality of Life) and two self-factors (self-esteem and self-mastery) were administered at admission and a 6-month follow-up. Participant age and amount of months on sick leave prior to rehabilitation were used as two proxies of duration of the condition.
Results: General quality of life distinguished between the groups, whereas satisfaction with life domains did not. Self-esteem and self-mastery were related to both quality of life aspects. Age was related to both estimates of quality of life, whereas duration of sick leave was unrelated to both.
Conclusion: General quality of life and satisfaction with life domains produced different results. Outcome studies should apply more than one operationalization of quality of life and self-factors should be considered as important determinants of quality of life. Duration of the condition needs to be acknowledged as well when interpreting levels of quality of life, although the current study could not present any clear-cut findings in this respect.
Keywords: stress, mastery, sick leave, self, occupation
Introduction
Quality of life is an important outcome of different types of interventions, including those intended to promote return to work after experiencing a minor mental disorder. There is no agreement on how quality of life should be defined, but the present study adopts the criteria stipulated by Mendlowicz and Stein,1 which include the person’s perception of the quality of his or her own life and a view of quality of life as multidimensional (covering areas such as social life, health, and functioning in daily activities and work).
Several studies of interventions supporting return to work have failed to identify any obvious effects on quality of life. This was the case, for example, for a minimal intervention conducted in primary care for people on sick leave for stress-related disorders2 and a lifestyle intervention, named Redesigning Daily Occupations (ReDO™), aimed at reorganizing the daily activities of women.3 Although other studies have yielded more promising results, for example, that psychiatric consultation added to care as usual (CAU) was effective for quality of life improvement4 and that patients who participated in a solution-focused intervention improved their quality of life more than a CAU group,5 findings regarding quality of life outcomes are inconclusive. Besides the obvious explanation that a certain intervention did not have any effect on people’s quality of life, other explications have been proposed, such as i) measures differ in scope and the measure in use may not account for relevant dimensions of quality of life;6 ii) quality of life is determined by factors pertaining to the self, such as self-esteem and self-mastery,7–11 and such factors tend to be fairly stable over time; and iii) people adjust to life circumstances and simultaneously recalibrate their inner goals and expectations.6 The latter implies that people who have had their condition for a longer period of time rate their quality of life higher than those with a shorter duration. This, in turn, makes it hard to identify true changes in quality of life.
Proceeding from these explanations, which served as a rationale and impetus for this methodologically oriented study, the following hypotheses were tested in the samples of the afore-mentioned study3 comparing the lifestyle intervention ReDO™ with CAU:
- Two variables reflecting quality of life would identify divergent results with respect to differences in quality of life increments from baseline to the 6-month follow-up between the group receiving the ReDO™ intervention and those receiving CAU.
- Self-factors may explain quality of life in the sample as a whole, and a stronger sense of self would be related to better quality of life.
- Older participants and those who had been on sick leave for a long duration would rate their quality of life better.
Methods
This was a combined cross-sectional and longitudinal intervention study with a matched-control design. It was partly based on re-analysis of previously published data3 from a project focusing on women with stress-related disorders that took place in southern Sweden. The ReDO™ intervention was conducted in one county, while the CAU group was selected in an adjacent county. The Regional Research Ethics Committee at Lund University approved the study (Nos 922/2004 and 149/2007), which was also registered as a clinical trial at ClinicalTrials.gov (identifier NCT01234961).
The ReDO™ intervention
The ReDO™ intervention was built upon knowledge about women’s everyday activities generated in research by Erlandsson and Eklund,12–14 and was also inspired by the Lifestyle Redesign® project,15 which focused on helping elderly adults to incorporate positive changes with respect to the activity repertoires of their everyday lives. The term occupation, as in daily occupations, is in the present study used to denote all of a person’s everyday activities, including paid work, household work, hobbies, socializing, etc, and is used synonymously with the term activity. The ReDO™ intervention, described in detail in Erlandsson,16 is a 16-week group-based program with three parts. In the first 5 weeks, the program focuses on analyzing hindrances for a healthy and balanced activity lifestyle, such as no time for leisure and an unequal distribution between family members regarding household work, while the subsequent 5 weeks address factors that hinder return to work, such as unclear responsibilities and a disturbing work environment. During these 10 weeks in total, the group meets twice a week, for 2.5 hours per session. The group sessions target identification of problems and working through personal strategies to solve them. Between sessions the participants practice their strategies in their home environment and try to organize their everyday activities such that they perceive a better balance. This includes a balance between different types of activities and between activity engagement and rest. Their experiences are then discussed during the subsequent sessions, and problems and solutions are renegotiated. The last 6 weeks of the program constitute a work practice period, if possible at their current workplace, otherwise at a relevant new workplace with the goal of returning to work. The group facilitators were two occupational therapists with specific training in the ReDO™ method.
CAU
CAU was composed of a broad array of interventions, ranging from follow-up visits to the Social Insurance Office (SIO), sometimes which included the employer, to more comprehensive interventions. Examples of the latter were work rehabilitation programs, supported work training at one’s ordinary job, regularly seeing a psychologist, social worker and/or physiotherapist, and mindfulness training.
Study period
The women’s project in which the ReDO™ intervention was used ran from September 2007 to May 2009, meaning that new participants were included until February 2009. This study was based on two measurement points – admission and a follow-up 6 months after completing the 16-week program. The last follow-ups were made in early 2010. The measurements in the CAU group were performed at time points that corresponded to those of the ReDO™ group and included a baseline measurement and a second measurement after 10 months (16 weeks + 6 months).
Selection of participants
Women with a diagnosis of a stress-related disorder (F32 or F34 according to the International Classification of Diseases [ICD]-10 classification),17 having been on sick leave for 2 months or longer, and having employment were eligible for the study. The SIO officer assessed if the ReDO™ intervention would be a suitable alternative, while considering these criteria and whether the woman would have the capacity to participate in the intervention. Forty-two women were offered and chose to enter the ReDO™ program, and all of them also agreed to be enrolled in the research project.
The comparison group was selected through the SIO register in the neighboring county by a matching procedure, based on the following criteria: specific diagnosis, age, family situation (marital status and number of children), profession, and duration of sick leave. Approximately 25% of the initially invited women declined to participate in the study, and new presumptive participants were approached until matched controls had been found for all the ReDO™ women. All women in the comparison group participated in regular follow-ups with the SIO officer and the employer, and received relevant medical treatment. About 50% also reported receiving one of the more comprehensive rehabilitation alternatives mentioned above during the 16-week period.
The final participants were thus 42 women in each group. This was considered to be a sufficient number according to the power calculation made, which was based on the ambition to detect an effect size of 0.6 between the groups. Effect size was defined as the mean of one group minus the mean of the other, divided by the pooled standard deviation. An effect size of 0.6 corresponds to a moderately strong effect,18 and according to the power analysis, 40 women in each group were required to detect that effect size with 80% power at P<0.05.19 Four participants withdrew from the ReDO™ group and five from the CAU group during the 16-week period. Further attrition occurred during the follow-up interval, and 37 women in the ReDO™ group and 34 in the CAU group completed the data collection during the 6-month follow-up. The study was thus under-powered with respect to the follow-up measurements. The groups appeared equivalent on socio-demographic characteristics, as shown in Table 1. They were also comparable regarding type of occupation (P=0.193). Managers and professionals formed the largest category (50% in the ReDO™ group and 36% in the CAU group). Other major occupational categories were technicians and associate professionals (14% in the ReDO™ group and 31% in the CAU group) and clerical support, service and sales workers (35% in the ReDO™ group and 31% in the CAU group).
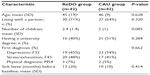  | Table 1 Baseline characteristics of the participants (N=84) |
Those who dropped out of the study (n=12) between baseline and follow-up were more likely to have a college or university education (P=0.044) and they had a longer period of sick leave before entering the rehabilitation (P=0.008) compared to those who completed the study (n=71).
Data collection and instruments
A questionnaire was devised to gather socio-demographic and clinical data (eg, age, education, marital status, number of children, any previous rehabilitation), and information regarding sick leave and work data was obtained from the SIO registers. The instruments administered at baseline and the 6-month follow-up are described below.
Two aspects of quality of life were assessed by the Swedish version20 of the Manchester Short Assessment of Quality of Life (MANSA).21 The instrument generates two estimates of quality of life, one of which is a one-item rating of general quality of life. The other is obtained by summarizing the respondent’s ratings of satisfaction within eleven equally-weighted life domains. Responses are given on a 7-point scale ranging from “could not be worse” (=1) to “could not be better” (=7). A higher score denotes better quality of life. The domains concern work, economy, friends, leisure, housing, personal safety, people one lives with (if any), sex life, relationship with family, and physical and mental health. The Swedish version has shown good psychometric properties in terms of internal consistency, ability to discriminate between people with and without known ill-health,20,22 and sensitivity to change.23 Satisfactory internal consistency (Cronbach’s alpha =0.77) was indicated for the current sample. The general quality of life rating and the composite score of satisfaction with life domains were the two quality of life estimates used for this study.
The self-factors addressed in this study were self-esteem and self-mastery. They were chosen since they have been found relevant in previous quality of life studies.7–11 The “self” is defined as a personal characteristic shaped by a combination of personality variables, the person’s life history, adjustment to circumstances and environmental influences.24 A scale developed by Rosenberg25 was employed to assess self-esteem. It is based on ten items with yes/no response alternatives with the total score indicating a balance between positive and negative self-esteem. The items target, eg, satisfaction with oneself, whether one has good qualities, whether one feels useless at times, pride of oneself, and self-respect. The score ranges from -1 (negative self-esteem) to 1 (positive self-esteem) and for negatively worded items the scoring is reversed. The instrument has satisfactory psychometric properties as shown, for example, by Sinclair et al.26 They identified a one-facture structure behind the scale and obtained a Cronbach’s alpha coefficient of 0.91. Validity was shown by correlations of -0.47 to -0.62 with scales assessing different but related phenomena including depression, anxiety, and stress.24 Cronbach’s alpha for the current sample was 0.88.
The construct of self-mastery was originally framed as a coping mechanism and was defined as one’s perceived power over the things that have important influence on one’s life situation.27 The Swedish version of the Pearlin self-mastery scale, recently found to represent a logical continuum of the measured construct and to yield valid and reliable data,28 was used. The instrument has seven items that address ability to solve problems, having control over happenings in one’s life, and ability to accomplish what one wants to achieve. The items are rated on an ordered scale with four response alternatives, from “strongly disagree” (=1) to “strongly agree” (=4). A higher score indicates a higher level of self-mastery. Since self-mastery was used as a self-factor in the current study, we only used the women’s baseline scores for the analyses. For the present sample, the Cronbach’s alpha coefficient was 0.77.
Data analysis
Data from four measurement points (baseline, after 16 weeks, and follow-ups after another 6 and 12 months) were available,3 but two measurements were considered optimal to meet the aim of this study. The baseline measurement and the 6-month follow-up were chosen as the measurements for this study. Research has shown that quality of life changes are more visible in a follow-up perspective than immediately after an intervention.29 The 6-month follow-up was regarded optimal because it allowed time for quality of life changes to have occurred but was not too distant in time. The instruments for assessing quality of life and self-mastery produced ordinal data and non-parametric statistics were used. The analyses were based on the Mann–Whitney U test to compare groups and the Spearman correlation test to estimate associations between variables. Change scores were calculated as the baseline score subtracted from the score at the 6-month follow-up. The P-value was set at <0.05 and the statistical software used was PASW statistics 18.0.
Results
The ratings of general quality of life and satisfaction with life domains at baseline and follow-up for the sample as a whole are shown in Table 2. The two quality of life estimates showed inter-correlations of P<0.001 at both baseline (rs=0.63, shared variance 40%) and the follow-up (rs=0.73, shared variance 53%). According to satisfaction with life domains, there was no difference between the groups in change of quality of life from baseline to the follow-up (P=0.251). There was a statistically significant difference with respect to change in the women’s perceptions of general quality of life (P=0.017), in favor of the ReDO™ group.
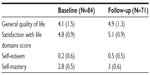  | Table 2 The participants’ mean ratings (SD) of quality of life, self-esteem, and self-mastery at baseline and the 6-month follow-up |
The participants’ rating of self-esteem and self-mastery are presented in Table 2. Both self-variables were significantly associated with the two estimates of quality of life at baseline as well as at follow-up (Table 3). Observation indicates that general quality of life and satisfaction with life domains showed relations that were similar in strength to self-esteem, particularly at baseline. The correlations in relation to self-mastery showed an analogous pattern.
  | Table 3 Associations between self-factors and quality of life (N at baseline =84; N at follow-up =71) |
The two proxies for duration of illness, ie, age and time on sick leave before baseline, were unrelated (rs=0.071, P=0.656). Age was statistically significantly associated with both general quality of life (rs=0.31; P=0.004) and satisfaction with life domains (rs=0.39; P<0.001) at baseline. Statistically significant relationships were found also at the follow-up regarding general quality of life (rs=0.25; P=0.033) and satisfaction with life domains (rs=0.24; P=0.049). The relationship between time on sick leave before baseline and quality of life was non-significant for both quality of life estimates on both occasions, coefficients ranging between, rs=-0.17 and rs=0.035 and P-values between 0.113 and 0.982 respectively.
Discussion
The first hypothesis was fully confirmed. Whereas one quality of life estimate (satisfaction with life domains) did not detect any difference between the groups regarding change from baseline to the follow-up, the other estimate (general quality of life) detected a difference. The correlation coefficients between the two instruments indicated a shared variance of 40% and 53% respectively, indicating that they measured constructs that were only partly overlapping. This gives some support to the critique proposing that quality of life is not a clear-cut and well-defined construct.30 Post et al31 discerned three operationalizations of quality of life – as health, as well-being, and as a superordinate construct, including both subjective well-being and objective life circumstances. The detailed satisfaction with life items probably made the participants reflect on their objective circumstances (work, economy, housing, etc), and might thus indicate the superordinate construct. The general quality of life estimate in the MANSA, on the other hand, may have reflected the participants’ well-being. Following this line of thought, the ReDO™ women improved more than the CAU women in terms of general well-being, but not in terms of quality of life as a superordinate construct that included objective life circumstances. The present study could not reveal which quality of life estimate was more adequate, but the findings suggest that more than one operationalization of quality of life should be reflected in outcome research, thereby also meeting the critique of inadequacy and indistinctness6,31 among quality of life instruments.
The self is shaped by a combination of basic personality variables and external situational influences24 and is thus not easily accessible for intervention and change. If associated with quality of life, it may therefore slow changes in that area. The findings indicated that two self-related factors, self-esteem and self-mastery, were both correlated with the estimates of quality of life employed in this study at baseline as well as at follow-up. This supports the second hypothesis and confirms previous findings that suggest factors pertaining to the self and personality are of importance for people’s quality of life ratings. This, has been studied among people with mood and anxiety disorders32 and severe mental illnesses,7,33 but also in a female sample from the general population34 and among young women.35 The fact that the quality of life estimates exhibited similar associations with the respective self-factors suggests than none of them was superior in capturing the essence of the quality of life construct.
Moreover, the associations between variables in this study showed that the closeness between the two quality of life estimates did not appear to be more pronounced than the association between self-mastery and quality of life. The correlations between these variables ranged between rs=0.54 and rs=0.73. A warranted reflection is then whether a general subjective factor is the general denominator in all the measures used. This discussion was raised by Priebe et al36 and may be seen as part of the complexity in delineating the quality of life construct. Finally, the third hypothesis, stating that older women and those with long sick-leave duration would rate their quality of life better, was only partly confirmed. Age showed to be positively related with quality of life, but duration of sick leave did not. The latter finding is contrary to some other studies; for example, people with mental illnesses who have had their condition for a long time tend to rate their quality of life better than those with similar conditions but for a short duration,6 and people with pain who have had their condition for a long time have been shown to cope more effectively with their situation.37 The duration of sick leave might not reflect duration of the condition, however, and if it did, the duration (about 1 year on average) may have been too short to produce an adjustment effect. Another reason for the non-finding may be that the women did not see their condition as chronic but were anticipating recovery. There could also be one or more unknown factors that influence the relationship between time on sick leave and quality of life. The proxy of age was indeed related with quality of life, at baseline as well as the follow-up, which supported the hypothesis about an adjustment effect by increasing age.
Applying the above implications to the previous ReDO™ quality of life study,3 it can be assumed that the non-findings demonstrated in that study could at least partially be explained by only one quality of life operationalization applied and self-factors and an adjustment effect influencing the quality of life ratings.
Study limitations
The sample sizes were fairly small and the study may have produced Type-II errors. In particular, the study was under-powered at follow-up, as the critical number of 40 participants in each group was not reached. True group differences on satisfaction with life domains may have gone undetected. The fact that CAU was a heterogeneous set of interventions is another limitation of the study. Effects of more successful interventions may have been leveled out by less successful ones, but the current study could not reveal if this was the case. On the other hand, this was not an effectiveness study – the main point was to address quality of life as an outcome measure – and that should make the composition of the CAU interventions less critical. Finally, two proxies were used for duration of sickness, one of which was time on sick leave. However, the participants had probably been on sick leave for too short a period of time (mean =11.5 months) to enable a true test of the hypothesis regarding recalibration of life expectations. Age as an indicator of duration of the condition, although used in respected research,38 was another proxy of unproven relevance. With these shortcomings in mind, the results of this study should be seen as tentative as further research is needed, particularly in relation to the hypothesis regarding recalibration of life expectations.
Conclusion
The findings underscore that quality of life is a complicated outcome, but also that actions can be taken to address the issue more properly. On the basis of the study findings, it is recommended that the instruments in use should be based on more than one operationalization of quality of life. Low ratings on self-factors are likely to flatten the measurable effects of an intervention aimed at increasing people’s quality of life, and the influence of self-factors should thus be carefully addressed as well. Duration of the condition also needs to be acknowledged when interpreting levels of quality of life, particularly in longitudinal studies and in the evaluation of intervention effects. The current study could not present any clear-cut findings in this respect, however, and the hypothesis regarding recalibration of life expectations needs to be addressed further.
Acknowledgments
The study was financially supported by the Swedish Research Council for Health, Working Life and Welfare. Sincere thanks to Birgitta Wästberg and Anita Bjerle-Frisk for performing parts of the data collection and to Lena-Karin Erlandsson for coordinating the project.
Disclosure
The author declares no conflicts of interest.
References
Mendlowicz MV, Stein MB. Quality of life in individuals with anxiety disorders. Am J Psychiatry. 2000;157(5):669–682. | |
Bakker IM, Terluin B, van Marwijk HW, et al. A cluster-randomised trial evaluating an intervention for patients with stress-related mental disorders and sick leave in primary care. PLoS Clin Trials. 2007;2(6):e26. | |
Eklund M, Erlandsson LK. Quality of life and client satisfaction as outcomes of the Redesigning Daily Occupations (ReDO) programme for women with stress-related disorders: A comparative study. Work. 2013;46(1):51–58. | |
van der Feltz-Cornelis CM, Hoedeman R, de Jong FJ, et al. Faster return to work after psychiatric consultation for sicklisted employees with common mental disorders compared to care as usual. A randomized clinical trial. Neuropsychiatr Dis Treat. 2010;6:375–385. | |
Nystuen P, Hagen KB. Solution-focused intervention for sick listed employees with psychological problems or muscle skeletal pain: a randomised controlled trial [ISRCTN39140363]. BMC Public Health. 2006;6:69. | |
Prince PN, Prince CR. Subjective quality of life in the evaluation of programs for people with serious and persistent mental illness. Clin Psychol Rev. 2001;21(7):1005–1036. | |
Eklund M, Bäckström M. A model of subjective quality of life for outpatients with schizophrenia and other psychoses. Qual Life Res. 2005;14(4):1157–1168. | |
Eklund M, Bäckström M, Hansson L. Personality and self-variables: important determinants of subjective quality of life in schizophrenia out-patients. Acta Psychiatr Scand. 2003;108(2):134–143. | |
Holloway F, Carson J. Quality of life in severe mental illness. Int Rev Psychiatry. 2002;14:175–184. | |
Prince PN, Gerber GJ. Subjective well-being and community integration among clients of assertive community treatment. Qual Life Res. 2005;14(1):161–169. | |
Ritsner M, Kurs R, Gibel A, Hirschmann S, Shinkarenko E, Ratner Y. Predictors of quality of life in major psychoses: a naturalistic follow-up study. J Clin Psychiatry. 2003;64(3):308–315. | |
Erlandsson LK, Eklund M. Describing patterns of daily occupations – A methodological study comparing data from four different methods. Scand J Occup Ther. 2001;8(1):31–39. | |
Erlandsson LK, Eklund M. Women’s experiences of hassles and uplifts in their everyday patterns of occupations. Occup Ther Int. 2003;10(2):95–114. | |
Erlandsson LK, Eklund M. Levels of complexity in patterns of daily occupations: relationships to women’s well-being. J Occup Sci. 2006;13(1):27–36. | |
Clark F, Azen SP, Zemke R, et al. Occupational therapy for independent-living older adults. A randomized controlled trial. JAMA. 1997;278(16):1321–1326. | |
Erlandsson LK. The Redesigning Daily Occupations (ReDO) program: Supporting women with stress-related disorders to return to work – Knowledge base, structure, and content. Occup Ther Ment Health. 2013;29(1):85–101. | |
WHO. The ICD-10 Classification of Mental and Behavioural Disorders. Geneva: World Health Organization; 1993. | |
Wampold BE. The Great Psychotherapy Debate: Models, Methods, and Findings. Mahwah, NJ: Lawrence Erlbaum Associates; 2001. | |
Altman DG. Practical Statistics for Medical Research. London: Chapman & Hall; 1993. | |
Björkman T, Svensson B. Quality of life in people with severe mental illness. Reliability and validity of the Manchester Short Assessment of Quality of Life (MANSA). Nord J Psychiatry. 2005;59(4):302–306. | |
Priebe S, Huxley P, Knight S, Evans S. Application and results of the Manchester Short Assessment of Quality of Life (MANSA). Int J Soc Psychiatry. 1999;45(1):7–12. | |
Eklund M, Sandqvist G. Psychometric properties of the Satisfaction with Daily Occupations (SDO) instrument and the Manchester Short Assessment of Quality of Life (MANSA) in women with scleroderma and without known illness. Scand J Occup Ther. 2006;13(1):23–30. | |
Priebe S, McCabe R, Junghan U, et al. Association between symptoms and quality of life in patients with schizophrenia: a pooled analysis of changes over time. Schizophr Res. 2011;133(1–3):17–21. | |
McCrae RR, Costa PT. A five-factor theory of personality. In: Pervin L, John OP, editors. Handbook of Personality: Theory and Research. New York: Guilford; 1999:139–153. | |
Rosenberg M. Society and the Adolescent Self Image. Princeton, NJ: Princeton University Press; 1965. | |
Sinclair SJ, Blais MA, Gansler DA, Sandberg E, Bistis K, LoCicero A. Psychometric properties of the Rosenberg Self-Esteem Scale: overall and across demographic groups living within the United States. Eval Health Prof. 2010;33(1):56–80. | |
Pearlin LI, Schooler C. The structure of coping. J Health Soc Behav. 1978;19(1):2–21. | |
Eklund M, Erlandsson LK, Hagell P. Psychometric properties of a Swedish version of the Pearlin Mastery Scale in people with mental illness and healthy people. Nord J Psychiatry. 2012;66(6):380–388. | |
Eklund M, Hansson L. Stability of improvement in patients receiving psychiatric occupational therapy: A 1-year follow-up. Scand J Occup Ther. 1997;4:15–22. | |
Ritsner MS, Awad AG. Quality of Life Impairment in Schizophrenia, Mood and Anxiety Disorders: New Perspectives for Research and Treatment. Dordrecht, the Netherlands: Springer; 2007. | |
Post MW, de Witte LP, Schrijvers AJ. Quality of life and the ICIDH: Towards an integrated conceptual model for rehabilitation outcomes research. Clin Rehabil. 1999;13(1):5–15. | |
van Straten A, Cuijpers P, van Zuuren FJ, Smits N, Donker M. Personality traits and health-related quality of life in patients with mood and anxiety disorders. Qual Life Res. 2007;16(1):1–8. | |
Ritsner M, Farkas H, Gibel A. Satisfaction with quality of life varies with temperament types of patients with schizophrenia. J Nerv Ment Dis. 2003;191(10):668–674. | |
Eklund M, Bäckström M, Lissner L, Björkelund C, Sonn U. Daily activities mediate the relationship between personality and quality of life in middle-aged women. Qual Life Res. 2010;19(10):1477–1486. | |
Kitamura T, Kawakami N, Sakamoto S, Tanigawa T, Ono Y, Fujihara S. Quality of life and its correlates in a community population in a Japanese rural area. Psychiatry Clin Neurosci. 2002;56(4):431–441. | |
Priebe S, Kaiser W, Huxley PJ, Röder-Wanner UU, Rudolf H. Do different subjective evaluation criteria reflect distinct constructs? J Nerv Ment Dis. 1998;186(7):385–392. | |
Persson D, Andersson I, Eklund M. Defying aches and revaluating daily doing: Occupational perspectives on adjusting to chronic pain. Scand J Occup Ther. 2011;18(3):188–197. | |
Priebe S, Reininghaus U, McCabe R, et al. Factors influencing subjective quality of life in patients with schizophrenia and other mental disorders: a pooled analysis. Schizophr Res. 2010;121(1–3):251–258. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
