Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 16
Exploration of Influencing Factors for Postoperative Recurrence in Patients with Madelung’s Disease on the Basis of Multivariate Stepwise Cox Regression Analysis
Authors Li S, Xiao Y, Wang Y, Bai M, Du F, Zhang H
Received 10 April 2022
Accepted for publication 16 December 2022
Published 15 January 2023 Volume 2023:16 Pages 103—110
DOI https://doi.org/10.2147/CCID.S368273
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jeffrey Weinberg
Shuo Li,* Yiding Xiao,* Yang Wang, Ming Bai, Fengzhou Du, Hailin Zhang
Department of Plastic Surgery, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Hailin Zhang, Email [email protected]
Purpose: Madelung’s disease (MD) is a rare condition of massive deposits of fat accumulations between superficial and deep fascia at typical locations. There is an absence of systematic studies related to MD in the Chinese cohort. Thus, the objective of the study was to investigate the clinical features of the MD cases in our institution and to explore the clinical variables associated with postoperative recurrence.
Materials and Methods: We retrospectively analyzed the clinical information of 21 individuals with MD from 2013 to 2021 enrolled in our institution. The paired t-test and χ2 test were, respectively, used to determine the difference between continuous and classified variables. The univariate Kaplan–Meier analysis by log-rank and multivariate stepwise Cox regression analysis were used to explore variables possibly associated with postoperative recurrence in MD individuals.
Results: In the current study, 90.48% of the studied patients were male with a mean age of 48.76 years old. About 61.90% exhibited type I MD. MD patients who experienced postoperative recurrence had a higher age, BMI, incidence of chronic complications, and prevalence of alcoholism than the other MD patients without recurrence (P < 0.05). The univariate Kaplan–Meier analysis by log-rank identified that age, BMI, alcoholism, and comorbidities were influencing factors related with postoperative recurrence (P < 0.05).
Conclusion: Demographic characteristics of the 21 studied Chinese cases with MD were generally in accordance with previously published data of other foreign populations. The factors possibly influencing the postoperative recurrence for patients with MD were age, BMI, alcoholism, and a combination of comorbidities. This is the first time that a summarization of clinical characteristics and postoperative recurrence variables of Chinese patients with MD has been reported.
Keywords: Madelung’s disease, MD, clinicopathological characteristics, recurrence influencing factors, Kaplan–Meier analysis, Cox proportional hazards regression
Corrigendum for this paper has been published.
Introduction
Madelung’s disease (MD) is a rare condition of numerous, progressive, symmetric, and unencapsulated deposits of fat accumulations between superficial and deep fascia at typical locations, such as the neck, face, trunk, and extremities of limbs, which is also known as Launois–Bensaude syndrome, benign symmetric lipomatosis (BSL), or multiple symmetric lipomatosis (MSL). The disorder was first reported by Benjamin Brodie in 1846.1 It was then named after the German surgeon Madelung, who described it in 1888.2
The prevalence of MD in the Mediterranean area has been approximately 1:25,000.3 However, MD was extremely rare in the Asian population.4 The pathogenesis and etiology of MD have not been elucidated yet. In most cases, people with MD present no apparent symptoms.5 For symptomatic MD patients, the most frequent complaints include cervical mobility restriction, cosmetic abnormality, respiratory distress, difficulty in swallowing, dysphonia, and psychological depression.4,6 The pathologic nature of the massively symmetric fat accumulations in patients with MD is benign, and no spontaneous regression of the nonencapsulated adipose tissue has been officially reported.7
MD can be classified into two types based on the distribution of lipomatosis.8,9 Type I, also known as horse collar lipoma, exclusively occurs in males, and adipose tissue is usually deposited in the neck, arms, upper trunk, and mediastinum. Fat deposits in these areas can result in cervical disfigurement accompanied by swallowing hypofunction, neck movement disorder, or even upper airway obstruction. Moreover, fatty tissue in uninvolved regions tends to be reduced or even absent. Type II MD can occur in males and females and is often relevant to weight gain. Deposition of lipomatous tissue in Type II MD patients is dominantly in the upper back, thighs, hips, and deltoid regions, very similar to the fat distribution pattern in females.
The mainstay therapeutic approaches for MD include surgical resection and liposuction.10 Staged and multi-modality surgical procedures are usually required to achieve acceptable therapeutic effects for patients with MD.11 It is rarely possible to obliterate the diffuse adipose masses as the deposits generally infiltrate several different planes and involve various adjacent structures, which indicates that surgical treatment is palliative instead of curative, and recurrence is common.12,13
Considering the extremely low incidence of MD in the Asian population, the clinicopathological characteristics of the 21 cases with MD in the current study were summarized and compared with those of other foreign populations. Although postoperative recurrence in MD patients is quite common, no published studies have analyzed and reported clinicopathological recurrence factors in MD individuals. Thus, the objective of the study was to investigate the clinical data of the 21 MD cases in our institution and to identify the variables possibly related to the postoperative recurrence rate for patients with MD.
Methods
We retrospectively searched patients diagnosed with MD enrolled in our institution between 2013 and 2020. Due to the low prevalence of the disease, we finally found 21 individuals with MD and retrospectively analyzed their clinical information. A detailed medical history inquiry and physical examination were conducted for each patient admitted to our institution. Thus, patients’ medical records and clinical information were safely preserved. Eleven of them underwent lipectomy or liposuction, while the other 10 did not accept complementary treatment as their lipomatous deposits did not severely influence their quality of life. The continuous variables were expressed as mean (AVG) ± standard deviation. The paired t-test and χ2 test were, respectively, used to determine the difference between continuous and classified variables. The univariate Kaplan–Meier analysis using log-rank and multivariate stepwise Cox regression analysis was used to explore variables possibly associated with postoperative recurrence in MD individuals. Statistical analysis was performed using SPSS 24.0 software (IBM, New York, USA). P≤0.05 was considered statistically significant. This study was in compliance with the guidelines of the Declaration of Helsinki. The clinical study protocol was reviewed and approved by Bioethical Committee of Peking Union Medical College Hospital. Written informed consent was obtained from all patients who participated in the study for publication and the use of their clinical data, including any accompanying images.
Results
Overall, 90.48% of patients were male. The mean age at the time of diagnosis was 48.76. 71.43% of patients fell into the overweight category (BMI≥24). According to Enzi’s classification, 61.90% of patients exhibited type I MD, while the rest had type II MD only or had features of both types I and II. Most of the studied cohort (66.67%) had multiple fatty masses over the body. The most commonly affected anatomic regions were the neck (23.29%), abdomen (10.96%), and dorsal area (8.22%). 71.43% of patients were related to alcohol abuse. MD patients are often combined with other metabolic abnormalities, while only 23.8% of cases did not present any comorbidities. No familial cases were found. 47.62% of the studied cohort experienced limited neck mobility (Figures 1 and 2), while the others were asymptomatic. Neuropathies, tongue, orbital involvement, etc., were not found in the current study cohort. Eleven of the studied 21 patients underwent surgical resection (81.82%) and liposuction (18.18%). The average follow-up duration was 4.30 years (range, 0.78–7.73 years). 45.45% of the studied MD patients who received excision or liposuction experienced postoperative recurrence. The average time when recurrence occurred after therapy was 1.84 years.
To further analyze the possible variables related to postoperative recurrence, the 11 patients who received treatment were divided into the recurrence group (n=5) and the non-recurrence group (n=6) within the average follow-up duration (4.3 years). The disparities of clinical information between the two groups are presented in Table 1. The average age of MD patients in the recurrence group (51.6± 6.39) was significantly higher than that of MD individuals in the non-recurrence group (38.7± 8.02) (P=0.017). Cases in the recurrence group also had higher BMI (27.16± 3.33) than those in the non-recurrence group (23.05± 2.06) (P=0.033). All patients in the recurrence group were combined with comorbidities, while the proportion in the non-recurrence group was only 33.3% (P=0.045). The percentage of alcoholic patients in the recurrence group was 80%, much higher than that in the non-recurrence group (16.7%) (P=0.036). Other variables, including the gender ratio, clinical classification, the percentage of MD patients with symptoms, and the percentage of MD individuals with abnormal liver function between these two groups, were not statistically different (P>0.05).
 |
Table 1 Disparities in Clinical Characteristics Between Recurrence (n=5) and Non-Recurrence Group (n=6) |
Using the diagnosis of MD disease post-operational relapse as an endpoint, the results of the univariate analysis by log-rank and multivariate stepwise Cox regression analysis are as follows: The univariate analysis by log-rank showed that variables including age (<45, ≥45), BMI (<24, ≥24), whether alcoholic, and whether combined with comorbidities were associated with recurrence (P<0.05) (Table 2). Furthermore, the Kaplan–Meier curves revealed that the postoperative recurrence rates of the two groups stratified by the above four factors were all statistically different (P<0.05) (Figure 3). However, multivariate stepwise Cox regression analysis showed that the above clinical features were not independent influencing factors for recurrence of MD (P>0.05) (Table 3).
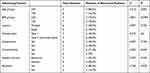 |
Table 2 The Log-Rank Univariate Analysis of Variables Related to Postoperative Recurrence of 11 MD Individuals |
 |
Table 3 Multivariate Cox Regression Analysis of Influencing Factors Related to Postoperative Recurrence of MD Disease |
Discussion
Madelung’s disease (MD) is characterized by multiple, disfiguring, abnormal fat depositions in the subcutaneous layer of different locations. According to a previous literature review, MD is more commonly seen in males in the fourth and fifth decades of life who chronically consumed alcohol, especially those in the Mediterranean or eastern European regions.3,14,15 In the current study, 90.48% of MD patients were male, similar to that in previous foreign studies. In the initial couple of years, the subcutaneous nonencapsulated fatty tissue tends to deposit in a rapid pattern, while after that, the disease usually stabilizes or progresses in a slow manner.16 There was also no spontaneous regression of MD in the current study, which is in accordance with the findings in the survey by Monika Szewc et al.4
As for disease classification, the vast majority of diagnosed patients with MD have more than one phenotype, and type I is the most frequently identified subtype.5 In the studied cohort, 61.90% of patients presented with type I MD, which is highly consistent with the findings conducted by other studies.5 Massive and symmetrical subcutaneous adipose tissue was most frequently deposited in the parotid, cervical, and posterior dorsal regions, resulting in cosmetic abnormalities. Other commonly affected areas include occipital areas, abdomen, and upper extremities. According to Enzi, nonencapsulated adipose tissue in patients with MD was usually symmetrically accumulated in the neck (83.8%), back (55%), upper segments of the arms (54%), and abdomen (35%), lower extremities (28%).15 Tongue, breasts, testis, and pubis have been rarely involved in MD patients in the literature.17
Obstructive sleep apnea syndrome (OSAS) is characterized by narrowing pharynx and airway obstruction. Theoretically speaking, massive symmetrical depositions of fat around the cervical area have the high potential to result in OSAS, although the exact pathophysiology mechanisms of OSAS are related to a series of anatomical and neuromuscular factors.18 In the studied cohort in our institution, OSAS has a much higher incidence (30%) than the literature reporting.18 Thus, OSAS should be carefully examined for each patient with MD despite the rarity reported in other literature. MD patients with OSAS should seek surgical interventions as early as possible.
Several hypotheses about the pathogenesis of MD have been proposed. Although genetic alterations existed in MD individuals, MD was not widely acknowledged as a hereditary disorder.19,20 Published literature found that most MD cases were sporadic instead of familial.19,21 For instance, in a Canadian family with many family members affected by MD, Perera et al22 demonstrated the presence of specific point mutations within mitochondrial DNA, a rare MTTK gene c.8344A>G variant. However, increasing numbers of familial accumulations have been found in a dominant inheritance pattern.23
Mutations of mitochondrial DNA resulted in mitochondrial dysfunction in adipose tissues.24–26 Some studies suggested that the etiology of MD derived from excessive proliferation of adipocytes and lipid deposition in functionally defective brown adipose tissue (BAT).27,28 Decreases in cytochrome C oxidase or modification in beta-adrenergic receptors reduced adrenergic-mediated lipolysis, which further caused hypertrophy of BAT in MD patients.17,29,30 However, in the most recent publication, Daniel Schiltz et al considered that in MD patients, the pathogenesis was ascribed to adipose tissue hyperplasia instead of hypertrophy.23 UCP1 was found to be much more highly expressed in both lipomatosis and unaffected adipose tissue in patients suffering from MD than in normal patients.23 Their influential investigation of high expression of UCP1 in patients with MD inspires other researchers to propose and implement more studies associated with this molecule.
Overall, 60–90% of the reported MD cases had chronic alcohol abuse.19,31 Despite the unknown pathogenesis of MD, it is widely acknowledged that alcohol serves as an aggravating factor in adipocyte hyperplasia by decreasing the number and activity of β-adrenergic receptors, causing premature oxidative aging of the mtDNA, and having an influence on mitochondrial metabolism.5,32 Thus, it clarifies why nonconsumers have a much lower MD prevalence such as children.33 Moreover, alcohol withdrawal has been reported to be related to a slight regression of the disease, while increased alcohol intake can lead to an acceleration of non-enveloped fat accumulations.9
In addition to the possible pathogenesis mentioned above, according to the study conducted by Daniel Schiltz and Oliver Felthaus et al in 2018,34 the etiology of MD might be related with the mTOR pathway, which is regulated in the brown adipose tissue and rapamycin was found to be able to inhibit the mTOR pathway and was considered to be a novel pharmaceutical therapy of MD.
The diagnosis of MD relies on clinical manifestations, physical examinations, and imaging studies.7,16 Auxiliary tests mainly include ultrasonography, computed tomography (CT), and magnetic resonance imaging (MRI). MD patients with an obstructed airway should perform CT or MRI to exclude malignant carcinoma of the airway or possible mediastinal extension.16 Other common differential diagnoses of MD include thyroid goiter, Cushing syndrome, morbid obesity, angiolipoma, lymphoma, encapsulated lipomas, liposarcoma, neurofibromatosis, salivary gland disorders, lipomatosis especially in human immunodeficiency patients, and so on.4,13,35
The treatment of MD mainly includes two modalities, surgical reduction and liposuction. Compared to the latter, the former has the advantage of being able to better control the noble structures including significant vessels and nerves. Being less invasive, liposuction can avoid causing extensive scars and have a shorter recovery period.13 Liposuction is also less likely to cause vascular or nervous lesions and can further reduce postoperative hematoma formation.12 Liposuction is usually applied in patients whose adipose tissue deposition tends to be diffuse and hardly be removed by surgical resection.
Due to the characteristics of this disease, the prognosis of MD is unpredictable, and the primary goal of MD is to improve cosmetic deformity and correct the laryngeal and lingual compression by the diffuse symmetrical accumulation of adipose tissue.7 According to the published studies, nearly 63% of the postoperative MD patients experienced recurrence: the recurrence rates of patients after lipectomy, liposuction, and lipectomy combined with liposuction were 51%, 95%, and 50%, respectively.4,19
Although there are several reports about the recurrence rate of MD after surgery, no studies have yet been reported to investigate the clinical risk factors associated with postoperative recurrence of MD. After searching and reviewing the published papers about MD disease among the Chinese population from the PubMed, Wanfang and CNKI (Chinese National Knowledge Infrastructure) database, the number of cases included in the current study is the largest based on the extremely low incidence of MD in the Asian population. Compared with the non-recurrence group in the current study, patients in the recurrence group had significantly higher age, BMI, incidence of chronic metabolic complications, and prevalence of alcoholism (P<0.05). According to the univariate analysis by log-rank and Kaplan–Meier curves, the variables associated with the recurrence of lipomatosis were age (<45, ≥45), BMI (<24, ≥24), alcoholism, and combination with other comorbidities (P<0.05). Bias refers to the deviation between the observed value and the true value, which is a systematic error caused by some relatively constant factors that cannot be accurately measured. The current retrospective study also holds several potential biases, including severe disease condition, a wide range of complications, and long course of disease, which are associated with characteristics of patients in superior hospitals.
By investigating the 21 Chinese cases of MD and summarizing the clinical information of other MD populations, we are fully convinced that the postoperative recurrence rate for MD patients with age≥45, BMI≥24, chronic metabolic comorbidities, or long history of alcohol consumption will be relatively higher. Thus, to some extent, MD patients with these characteristics should be informed of the higher possibility of postoperative recurrence in advance, monitor the postoperative progress more closely, improve their life modification more actively, and accept the reasonable treatment of their chronic comorbidities. These methods might be helpful to reduce the recurrence rate after surgery or delay the recurrence of the disease. However, due to the limitation of the number of cases and the length of follow-up duration in this study, further investigations in larger cohorts and longer follow-up periods are needed.
Conclusion
In conclusion, the demographic and clinical information of the studied cohort was generally in accordance with previously published data of other foreign populations. There are also some variations in the current cohort, such as lower incidence of neuropathies and higher incidence of OSAS and hepatic diseases. The factors possibly influencing the postoperative recurrence for patients with MD were age (<45, ≥45), BMI (<24, ≥24), alcoholism, and combination with other comorbidities. Advances in precision medicine emphasize the need to identify MD patients with higher recurrence possibilities. The current study significantly contributes to deepening the understanding of MD among physicians and providing better-personalized monitoring and treatment for MD patients.
Ethics Statement
Informed consent for publication of the study and associated images was obtained from the patients. This study was in compliance with the guidelines of the Declaration of Helsinki and was approved by Bioethical Committee of Peking Union Medical College Hospital.
Funding
There is no funding to report.
Disclosure
The authors have stated explicitly that there are no conflicts of interest in connection with this article.
References
1. Brodie SB. Clinical lectures on surgery delivered at St. George’s hospital. Lea Blanchard. 1846;11(22):437.
2. Madelung OW. Über den fetthals (diffuses lipom des halses). Arch Klin Chir. 1888;37(106):e130.
3. Heike Z, Gudrun UM, Frank RD, Vetter H, Walger P. Multiple benign symmetric lipomatosis—a differential diagnosis of obesity. Is there a rationale for fibrate treatment? Obes Surg. 2008;18(2):1354–1356.
4. Szewc M, Sitarz R, Moroz N, et al. Madelung’s disease – progressive, excessive, and symmetrical deposition of adipose tissue in the subcutaneous layer: case report and literature review. Diabetes Metabol Synd Obes. 2018;11:819–825. doi:10.2147/DMSO.S181154
5. Pinto CI, Carvalho PJ, Correia MM. Madelung’s disease: revision of 59 surgical cases. Aesthet Plastic Surg. 2016;41(2):1–10.
6. Gao Y, Hu J-L, Zhang -X-X, et al. Madelung’s disease: is insobriety the chief cause? Aesthet Plastic Surg. 2017;41(5):1208–1216. doi:10.1007/s00266-017-0920-1
7. da Costa JN, Gomes T, Matias J. Madelung disease affecting scrotal region. Ann Plastic Surg. 2017;78(1):73–77.
8. Enzi G. Multiple symmetric lipomatosis: an updated clinical report. Medicine. 1984;63(1):56–64. doi:10.1097/00005792-198401000-00004
9. Enzi G, Busetto L, Ceschin E, et al. Multiple symmetric lipomatosis: clinical aspects and outcome in a long-term longitudinal study. Int J Obes Related Metabol Disord. 2002;26(2):253–261. doi:10.1038/sj.ijo.0801867
10. Chen K, Wang L, Yang W, et al. Profiling of differentially expressed genes in adipose tissues of multiple symmetric lipomatosis. Mol Med Rep. 2017;16(5):6570–6579. doi:10.3892/mmr.2017.7437
11. Sharma N, Hunter-Smith DJ, Rizzitelli A, et al. A surgical view on the treatment of Madelung’s disease. Clin Obes. 2015;5(5):288–290. doi:10.1111/cob.12111
12. Samdal F, Kleppe G, Tonvang G. Benign symmetric lipomatosis of the neck treated by liposuction. Case Rep. 1991;25(3):281–284.
13. Ramos S, Pinheiro S, Diogo C, Cabral L, Cruzeiro C. Madelung disease: a not-so-rare disorder. Ann Plastic Surg. 2010;64(1):122–124.
14. Enzi GI. Multiple symmetric lipomatosis. Medicine. 2018;63(1):312–315.
15. Enzi G, Busetto L, Sergi G, et al. Multiple symmetric lipomatosis: a rare disease and its possible links to brown adipose tissue. Nutr Metabol Cardiovasc Dis. 2015;25(4):347–353. doi:10.1016/j.numecd.2015.01.010
16. Nikolić ŽS, Jeremić JV, Drčić LJ, et al. Madelung disease: a rare case associated with gynaecomastia and scrotal involvement. J Plast Surg Hand Surg. 2013;47(5):415–418.
17. Chen CY, Fang QQ, Wang XF, et al. Madelung’s disease: lipectomy or liposuction? BioMed Res Int. 2018;2018:1–8.
18. Pinto V, Morselli PG, Tassone D, Piccin O. A case of severe obstructive sleep apnoea in Madelung’s disease treated by lateral pharyngoplasty. J Laryngol Otol. 2017;131(9):1.
19. Brea-García B, Cameselle-Teijeiro J, Couto-González I, Taboada-Suárez A, González-Álvarez E. Madelung’s disease: comorbidities, fatty mass distribution, and response to treatment of 22 patients. Aesthet Plast Surg. 2013;37(2):409–416.
20. Klopstock T, Naumann M, Schalke B, et al. Multiple symmetric lipomatosis Abnormalities in complex IV and multiple deletions in mitochondrial DNA. Neurology. 1994;44(5):862–866. doi:10.1212/wnl.44.5.862
21. Chalk CH, Mills KR, Jacobs JM, et al. Familial multiple symmetric lipomatosis with peripheral neuropathy. Neurology. 1990;40(8):1246–1250. doi:10.1212/wnl.40.8.1246
22. Perera U, Kennedy BA, Hegele RA. Multiple symmetric lipomatosis (Madelung disease) in a large Canadian family with the mitochondrial MTTK c.8344A>G variant. J Investigat Med High Impact Case Rep. 2018;6:2324709618802867. doi:10.1177/2324709618802867
23. Schiltz D, Tschernitz S, Ortner C, et al. Adipose tissue in multiple symmetric lipomatosis shows features of brown/beige fat. Aesthet Plast Surg. 2020;44(3):855–861. doi:10.1007/s00266-020-01666-6
24. Verna G, Kefalas N, Boriani F, et al. Launois-Bensaude syndrome: an unusual localization of obesity disease. Obes Surg. 2008;18(10):1313. doi:10.1007/s11695-008-9502-2
25. González-García R, Rodríguez-Campo FJ, Sastre-Pérez J, et al. Benign symmetric lipomatosis (Madelung’s disease): case reports and current management. Aesthet Plast Surgery. 2004;28(2):108–112. doi:10.1007/s00266-004-3123-5
26. Grassegger A, Haeussler R, Schmalzl F. Tumescent liposuction in a patient with Launois-Bensaude syndrome and severe hepatopathy. Dermatolog Surg. 2010;33(8):982–985.
27. Vilà M, Gámez J, Solano A, et al. Uncoupling protein-1 mRNA expression in lipomas from patients bearing pathogenic mitochondrial DNA mutations. Biochem Biophys Res Commun. 2000;278(3):800–802. doi:10.1006/bbrc.2000.3828
28. Moonen MPB, Nascimento EB, van Kroonenburgh MJ, Brandjes D, van Marken Lichtenbelt WD. Absence of 18F‐fluorodeoxyglucose uptake using Positron Emission Tomography/Computed Tomography in Madelung’s disease: a case report. Clin Obes. 2019;9(3):e12302.
29. Gao H, Xin Z-Y, Yin X, et al. Madelung disease: a case report. Medicine. 2019;98(3):e14116. doi:10.1097/MD.0000000000014116
30. Dorigo P, Prosdocimi M, Carpenedo F, et al. Multiple symmetric lipomatosis: a defect in adrenergic stimulated lipolysis II. Pharmacolog Res Commun. 1980;12(7):625–638. doi:10.1016/s0031-6989(80)80100-7
31. Hirose A, Okada Y, Morita E, et al. Benign symmetric lipomatosis associated with alcoholism. Intern Med. 2006;45(17):1001. doi:10.2169/internalmedicine.45.1791
32. Ray S, Chakraborty PP, Pramanik S, et al. Bilateral breast enlargement in a chronic alcoholic: do not miss Madelung’s disease. BMJ Case Rep. 2016;2016:bcr2016215082. doi:10.1136/bcr-2016-215082
33. Nounla J, Rolle U, Gräfe G, Kräling K. Benign symmetric lipomatosis with myelomeningocele in an adolescent: an uncommon association—case report. J Pediatr Surg. 2001;36(7):E13. doi:10.1053/jpsu.2001.24776
34. Felthaus O, Schön T, Schiltz D, et al. Adipose tissue-derived stem cells from affected and unaffected areas in patients with multiple symmetric lipomatosis show differential regulation of mTOR pathway genes. Clin Hemorheol Microcirculation. 2018;69(1–2):141–151. doi:10.3233/CH-189107
35. Lee LC, Weng TH, Huang KH, et al. Application of lateral tarsoconjunctival flap to correct ocular complications of Madelung’s disease: a case report and literature review. Medicine. 2018;97(42):115.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



